Abstract
In this study, we used new technology to investigate whether a coherent pattern of enhanced expression of inflammatory and other immune activation genes in circulating monocytes is found in patients with major depression. Since a high inflammatory state of monocytes might be related to glucocorticoid resistance, we also included the genes for the two isoforms of the glucocorticoid receptor. For this study, we aimed at finding a similar coherent pattern of inflammatory and immune activation genes in monocytes of patients with MDD and recruited 47 medication-free melancholic MDD inpatients and 42 healthy controls. A quantitative-polymerase chain reaction (Q-PCR) monocyte gene expression analysis was performed using a panel of inflammatory-related genes previously identified as abnormally regulated in mood disorder patients. Selected serum cytokines/chemokines were assessed using a cytometric bead array. Depressive symptoms were analysed using Hamilton depression scores (HAMD). Thirty-four of the 47 monocyte inflammatory-related genes were significantly upregulated and 2 were significantly downregulated as compared to controls, the latter including the gene for the active GRα in particular in those with a high HAMD score. The reduced GRα expression correlated strongly to the upregulation of the inflammatory genes in monocytes. Serum levels of IL6, IL8, CCL2 and VEGF were significantly increased in patients compared to controls. Our data show the deregulation of two interrelated homoeostatic systems, that is, the immune system and the glucocorticoid system, co-occurring in major depression.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) is a biologically and genetically heterogeneous disorder. Despite advances in understanding biological correlates of MDD, specific objective hallmarks are still lacking. Defining a clear phenotype increases the chance of finding specific disturbances in neurobiology that may benefit from particular targeted treatments.
In recent years, an increasing body of evidence shows the involvement of an increased inflammatory response system in MDD1,2 and meta-analysis studies have confirmed the increase of pro-inflammatory cytokines in the circulation of patients.3,4 Several routes have been uncovered through which cytokines might enter and act in the brain, thereby, making the brain vulnerable to stress. Indeed pro-inflammatory cytokines have been found to interact with many of the pathophysiological domains that characterize psychiatric behaviour, such as with neurotransmitter metabolism, neuroendocrine function and synaptic plasticity and behaviour.5 Further, low intravenous doses of endotoxin increase the level of these cytokines and induce depressive symptoms.6 Depressive symptoms can also be induced by interferon-alpha treatment.7 In contrast, blocking these cytokines, for example, using anti–tumour necrosis factor (TNF) therapy, results in a markedly improved mood in treatment-resistant depressed patients.8
This makes cytokines prime candidates for recording immune neurobiological disturbances underpinning major mental disorders.However, one must take into account that cytokine levels in serum or plasma are strongly confounded by age, gender, socio-economic status, metabolic syndrome, visceral obesity, smoking, exercise, poor-rated self-health and medication. Cytokine levels in serum and plasma are also more deeply affected by environmental factors and present high inter-individual variation. Accordingly, we have focused our investigations not only on cytokines but also on important cellular producers of these cytokines, namely monocytes and macrophages. Supporting this approach, our group has identified a coherent pattern of enhanced expression of inflammatory and other immune activation genes in circulating monocytes of patients with mood disorders other than MDD, namely bipolar disorder and postpartum psychosis.9, 10, 11
For this study, we aimed at finding a similar coherent pattern of inflammatory and immune activation genes in monocytes of patients with MDD. We have included severely depressed inpatients, almost exclusively with melancholic features, medication free and report outcomes of a quantitative polymerase chain reaction (Q-PCR) study of monocytes in these patients tested for the genes previously found to be upregulated in bipolar disorder, schizophrenia and related endocrine autoimmune diseases.10, 11, 12, 13, 14, 15 We compared outcomes of gene expression in monocytes with circulating levels of some monocyte/macrophage related cytokines/chemokines and vascular endothelial growth factor (VEGF), an angiogenic protein and the adhesion molecule s-ICAM all of which have been implicated in major psychiatric conditions.
It has been hypothesized that the increased inflammatory response system found in severely depressed patients is responsible for the hypothalamic-pituitary-adrenal axis hyperactivity also found in some patients, possibly due to a cytokine-induced reduction of glucocorticoid receptor (GR) sensitivity.16,17 In accordance, we have previously reported that increased activation of the inflammatory system co-occurs with hyperactivity of the hypothalamic-pituitary-adrenal axis18 and with impaired GR sensitivity19 in treatment-resistant depressed patients. Glucocorticoids modulate a wide variety of immune cell functions, like cytokine and adhesion molecule expression, immune cell trafficking, maturation and differentiation. Glucocorticoids are able to shift the immune responses from a pro-inflammatory to an anti-inflammatory cytokine pattern.20,21 Glucocorticoids bind to two receptors: the GR and the mineralocorticoid receptor. The primary receptor for glucocorticoids in immune cells is the GR, which is located in the cytoplasm in an inactive multi-protein complex form. Cloning of the human GR has identified two isoforms, termed GRα and GRβ, which originate from alternative splicing of the GR primary transcript.22,23 The GRβ lacks the ability to bind glucocorticoids and seems to function as an inhibitor of GRα-mediated transcriptional activation through the formation of GRα/GRβ heterodimers.24,25 In this study, we additionally included in the Q-PCR study of the monocytes of the MDD patients both the α and β isoform of the GR receptor.
Materials and methods
Participants
This study was approved by the Medical Ethical Committee of the Erasmus MC Rotterdam (Ethics number MEC-2003-100-5). After study procedures had been fully explained, all subjects provided written informed consent.
Forty-seven (n=47) patients with MDD were recruited from the depression inpatient unit of the Department of Psychiatry of the Erasmus Medical Centre in Rotterdam, the Netherlands. All patients were diagnosed according to the DSM-IV-TR using the Structural Clinical Interview for Disease (SCID-1). Severity of depression was analysed using Hamilton depression questionnaire version 17. We used stringent exclusion criteria to avoid the possibility that medication or a physical disorder could influence gene expression. All patients had to be antidepressant medication free for at least one week before blood withdrawal. Blood was withdrawn in the morning between 0800 and 1000 hours. Benzodiazepines were allowed on the dose of 1–3 mg per day. One patient continued with haloperidol. Patients were excluded if they met the following criteria: were incapable of understanding the information and to give informed consent; unable to read or write, mental retardation (IQ<80); bipolar I or II disorder, schizophrenia or other primary psychotic disorder; if they had drug/alcohol dependence for the last 3 months, serious medical illness; women: pregnancy or possibility for pregnancy and no adequate contraceptive measures, breastfeeding.
Forty-two gender-matched healthy controls (HC) were recruited from the same community. Gender-matched HC (n=42) were recruited via enrolling laboratory staff, medical staff and medical students. The inclusion criteria for the HC were an absence of any major Axis I psychiatric disorder such as schizophrenia, psychotic disorder, mood disorder, anxiety disorder or substance related disorder according to DSM-IV criteria and no history of a severe medical illness. HC had to be in self-proclaimed good health and free of any obvious medical illness for at least two weeks prior to the blood withdrawal, including acute infections and allergic reactions. HC were also free of medications including oral contraceptives.
Blood collection and preparation
Blood was collected in clotting tubes for serum preparation (stored at –80 °C) and in sodium–heparin tubes for immune cell preparation. From the heparinized blood, peripheral blood mononuclear cell suspensions were prepared by low-density gradient centrifugation via Ficoll-Paque PLUS (GE Healthcare, Uppsala, Sweden), as described previously in detail26 within 8 h to avoid erythrophagy-related activation of the monocytes. Peripheral blood mononuclear cells were frozen in 10% dimethylsulphoxide and stored in liquid nitrogen. This enabled us to test immune cells of patients and controls concomitantly at a later stage.
Isolation of monocytes and RNA
The use of one single cell type (i.e. monocytes instead of peripheral blood mononuclear cell) reduces the ranges of factors that may lead to inconsistency in the results due to differential gene expression per cell type. CD14 positive monocytes were isolated from frozen peripheral blood mononuclear cells by magnetic cell sorting system (auto MACS Pro, MiltenyiBiotec, B.V., Bergisch Gladbach, Germany). The viability and purity of monocytes was >95% (determined by morphological screening after Trypan Blue staining and flow cytometry analysis). The average viability was 97.1±3.5 and the purity of monocytes 97±2.2%. RNA was isolated from purified monocytes using the RNAeasy minikit according to the manufacturer’s instructions (Qiagen, Hilden, Germany).27 On average, monocytes cell yield after isolation was 2.2±1.0 × 106 and quantity of RNA in monocytes 3.3 ±1.6 μg.
RT-qPCR
One μg of RNA was reversed-transcribed using the High Capacity cDNA kit (Applied Biosystems, Foster City, CA, USA). qPCR was performed using TaqMan Arrays, format 48 (Applied Biosystems), according to the manufacturer’s protocol and validated against the single RT-qPCR method. Per fill port 400 ng of cDNA (converted from total RNA) was loaded. PCR amplification was performed using an Applied Biosystems Prism 7900HT sequence detection system with TaqMan Array block.Thermal cycler conditions were 2 min at 50 °C, 10 min at 94.5 °C, 30 s at 97 °C and 1 min at 59.7 °C for 40 cycles. Expression values were calculated using the comparative threshold cycle method.
Serum cytokine/chemokine determination
Multiple serum cytokines were measured using a multiplex array approach: the Cytometric Bead Array kit (CBA, Bender MedSystems, Burlingame, CA, USA) according to the manufacturer’s protocol. Samples were analysed in a BD FACS Canto II flow cytometer (BD Biosciences, San Jose, CA, USA) with the Flowcytomix Pro 2.3 Software (eBioscience, Vienna, Austria). We determined serum cytokine levels of the monocyte/macrophage cytokines CCL2, IL-1β, IL6, IL8, VEGF, and soluble adhesion molecule (s-ICAM). The CBA was not sensitive enough to reliably detect IL-1β and IL6. Sensitivity of the kit is provided in Supplementary Table 1. For both patients and controls, samples that were below the sensitivity of the method were replaced by the lowest sensitivity of the kit. We are aware of the insensitivity of the kit for these cytokines, however, we did not have spare serum to re-analyse these cytokines separately.
Statistical analysis
Statistical analyses were performed using SPSS version 21 and graphpad prism 5. Dendogram was obtained from Pearson correlation in SPSS. Heat map was built using Treeview.28 For sample characteristics, categorical data were evaluated using Fisher’s exact test and continuous variables using a two-sample t-test. Continuous variables are expressed as the mean±standard error. The Mann–Whitney U test was used to compare levels of nonparametric parameters (serum/cytokines). For gene expression, P was tested by univariate analysis of covariance (ANCOVA) vs control subjects; age and gender are included in this model. Statistical analysis on the gene expression data in monocytes and geometric mean of the FC was performed using DataAssist version 3.0 (Applied Biosystems, Life Technologies Corporation). Correlations were determined via Spearman rank correlation coefficients. All hypotheses were tested with an alpha of 0.05 (two-sided). Multiple testing correction was applied using Simes’ correction, which is an improved version of Bonferroni.29,30
Results
Patients
Data is expressed as mean (range). HC were younger than MDD patients (HC=49 (3131–74), MDD=54 (32–82), P<0.005). There were no significant differences in gender distribution (HC=21 males (50%), MDD=20 males (43%)). MDD patients had a mean Hamilton depression rating scale (HAMD17) score of 24.4 (18–30), and on average, one previous depressive episode (range 0–4). All patients had melancholic features according to DSM-IV criteria using SCID-1. At the time of blood sampling, all MDD patients were drug-free for at least one week. After blood drawn, participants then went on to go on a clinical trial for which the results have been reported elsewhere.31
Previous medication included (in numbers): 37 SSRI/SNRI, MAOi 2, tri/tetracyclic 9, dual inhibitor 10, benzodiazepines 36, typical antipsychotics 8, atypical antipsychotics 8. Only two MDD patients previously took MAOi (n=2) and presented higher levels of IL1β (no MAOi=41.6±3.8, MAOi=18.0±5.8, P=0.001), higher PDE4B (no MAOi=12.5±2.1, MAOi=2.2±0.3, P=0.001), higher MAFF (no MAOi=1.11±0.15, MAOi=0.30±0.004, P=0.001) and higher TNF expression (no MAOi=10.9±2.2, MAOi=0.33±0.04, P=0.001) than those who have never taken MAOi (n=45). Despite the statistical significance of these findings, it might not have clinical relevance due to the low number of patients in the comparison group. Finally, MDD patients who previously took atypical antipsychotics (n=7) had lower IL1β in the serum (no atypical_AP=21.4±4.1, atypical_AP =4.2±0.001, P=0.001) compared to those who have never taken them (n=40). No other differences were found.
RT-PCR analysis of monocytes of major depression patients
We determined the monocyte gene expression of 47 genes, including the genes examined previously in patients with bipolar disorder and schizophrenia,10,11 postpartum psychosis12 and inflammatory disorders, such as diabetes,13 autoimmune thyroid disease15 and Sjögren’s disease.14 Finally, we also measured the two splice variants of the GR (GRα and GRβ).
We first performed a cluster analysis for monocyte gene expression (Figure 1b). Two main clusters were identified—a large cluster 1 and a smaller cluster 2. Cluster 1 genes included most of the well-known pro-inflammatory mediators (e.g. IL1A, IL1B, IL6, PTX3, TNF, PDE4B and PTGS2). The smaller cluster 2 genes included mainly chemotaxis (CCL2, CCL7) and metabolic (DHRS3, FABP5) genes. Notably, the gene clusters extensively overlapped with the previously identified monocyte gene expression clusters described in the monocytes of bipolar, schizophrenia and postpartum psychosis patients (Drexhage et al.10 and Bergink et al.12).
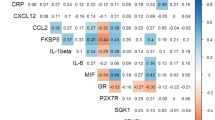
(a) Q-PCR analysis of monocytes of MDD patients (n=47) as compared to healthy control (HC) (n=42) values, set at onefold. The quantitative value obtained from Q-PCR is a cycle threshold (CT). The fold change values between different groups were determined from normalized CT values (CT gene–CT reference gene ABL), by the ΔΔCT methods (2−ΔΔCT, user Bulletin 2, Applied Biosystems, Foster City, CA, USA) as per DataAssist software. Data were standardized to the HC (thus the HC were used as the calibrator). The fold change of the HC is therefore 1. For gene expression, P was tested by univariate analysis of covariance (ANCOVA) vs control subjects; age and gender are included in this model. (b) Heat map of gene correlation, data represent Spearman’s correlation coefficients, tested on the relative mRNA expression. Significant positive correlations (P<0.05) are given by the red scale (darkest red are correlations >0.5), significant negative correlations are given by the green scale. Lighter fields are not significant. FC, fold change; MDD, major disorder. P values are shown after Simes’ correction. Bold FC are significantly upregulated.
Figure 1a additionally shows that in patients with MDD, monocyte inflammatory/immune gene expression was consistently upregulated compared to HC (apart from the GRα and HSP70 genes): 34 out of 47 (72%) immune-related genes were significantly upregulated after Simes’ correction for multiple comparisons. The upregulated genes were found mainly within cluster 1 (26/29, 90%), whereas in cluster 2, eight out of 14 (57%) of the genes were upregulated (see Figures 1a and b).
GRα and GRβ expression in monocytes and their relation with the expression of cluster 1 and cluster 2 inflammatory genes
With regard to the GRα and GRβ expression, we found a significant downregulation of the active GRα in MDD patients (F(1,86)=11.99, P=0.001), whereas there was a trend for an upregulation of the inactive GRβ, that did not reach statistical significance. To test for the relationship between the splice variants of the GR and the inflammatory gene expression, we correlated GRα and GRβ expression separately to the other tested genes (Table 1). The downregulation of GRα negatively and significantly correlated with the overexpression of a large proportion of the monocyte activation genes of cluster 1 (26/30) and of cluster 2 (8/13). GRβ overexpression positively and significantly correlated with the overexpression of 27/30 cluster 1 genes and 8/13 cluster 2 genes (Table 1).
Inflammatory cytokines/chemokines
To investigate whether the activated inflammatory response system as found via the gene activation of the circulating monocytes of MDD patients was also reflected in higher serum levels, we measured a selected panel of inflammatory cytokines/chemokines produced by monocytes IL1β, IL6, IL8, CCL2 and VEGF in the serum of the MDD patients and compared these to levels found in HC. We found evidence for increased levels of IL6 (P=0.04), IL8 (P=0.004), CCL2 (P=0.04) and VEGF (P=0.028) in the serum of MDD patients (as compared to HC), but not of IL1β after Simes’ multiple test correction (Figure 2).
Correlations between gene expression levels in circulating monocytes and serum levels of cytokines
To understand potential sources of increased serum cytokines/chemokines levels, we correlated serum cytokine/chemokine protein levels to monocyte expression levels of the corresponding genes. Interestingly there was a negative correlation between CCL2 levels in serum with CCL2 gene expression in monocytes (−0.271, P=0.047) and between serum IL1β with IL1B gene expression in monocytes (−0.259, P=0.059). There were no other significant correlations between serum protein and gene expression. This reflects a complex picture of inflammatory regulation with the possible involvement of other cell types.
We additionally investigated the relationship between the expression of the glucocorticoid receptor splice variants (GRα, GRβ) and the GRα/β expression ratio and the levels of cytokines in the serum.
Interestingly, GRα expression negatively correlated to IL8 serum levels (S=−0.389, P=0.008); GRβ expression in monocytes correlated negatively to the CCL2 serum level (S=−0.309, P=0.035), and GRα/β positively correlated to CCL2 serum levels (S=0.292, P=0.046). No other correlation was found between GR splice variants and levels of cytokines in the serum.
GRα, GRβ and inflammatory molecules in monocytes and their relation with clinical variables
In order to evaluate possible associations between GRα, GRβ and inflammatory parameters with clinical variables, we correlated gene expression levels in monocytes and the severity of depression as measured by total HAMD score. There were no associations with age and gender. As shown in Supplementary Table 2, GRα and EREG positively correlated to the severity of depression.
As anxiety is often a main symptom of severe depression, we also investigated correlations of psychic (item 10) and somatic anxiety (item 11) as assessed by the Hamilton depression scale with gene expression levels in monocytes. As shown in Tables 2A and B, the molecules EREG, CDC42, NMES1, CCL7 and AREG and GRβ positively and significantly correlated with psychic anxiety. There was no correlation between gene expression of the molecules tested and somatic anxiety.
In order to understand further the association between inflammatory molecules, GRα, GRβ gene expression levels and the GRα/β ratio in monocytes and depression severity, we conducted a linear regression model between the variables that were significantly correlated with HAMD scores in Tables 2A and B. Table 2A shows linear regression coefficients values of GRα, GRβ, and the GRα/β ratio in relation to the HAMD score. Model 1 shows the crude association; model 2 includes age and gender. As can be seen in particular, the monocyte GRα/β correlated to the HAMD score also after adjustment for age, gender and BMI.
Finally, we conducted ordinal regression models between the individual molecules EREG, CDC42, NMES1, CCL7 and AREG and GRβ as these genes correlated with psychic anxiety. As shown in Table 2B, we found the GRα and GRβ gene expression levels, the GRα/β gene expression ratio, and EREG, CDC42, CCL7, NMES1 and AREG expression individually predicting the odds of going up one level in the psychic anxiety scale. We have also conducted a multiple regression with all the molecules together to see whether it increased prediction. The only molecule that remained significantly associated was CDC42 (results are not shown).
Discussion
We have assessed an inflammatory gene expression profile in monocytes of melancholic drug-free inpatients with major depression and evaluated the relationship of this inflammatory expression pattern with the expression of the genes for the active GRα and the inactive GRβ in the monocytes. The outcomes of our study show that circulating monocytes overexpress inflammatory genes and underexpress the active GR variant (i.e. the α variant), suggesting a relative insensitivity of the monocytes for glucocorticoids. Particularly MDD patients with a high HAMD score had the lowest monocyte GRα expression. Supporting our findings, MDD patients had a high inflammatory set point of monocyte and high serum levels of pro-inflammatory cytokines and compounds, such as IL8, IL6, CCL2 and VEGF.
Our study extends and supports previous studies on gene expression profiles in peripheral blood leucocytes in patients with MDD. Spijker et al.32 used gene expression in peripheral blood after lipopolysaccharide stimulation and identified an MDD signature of seven upregulated genes of which six were related to the immune system, in particular dealing with cellular proliferation and differentiation. Segman et al.33 found in a relative small series of persistent postpartum depression patients, a gene expression signature of immune, proliferation and repair genes that was downregulated as compared to controls. Interestingly many of the immune genes found by these authors in their signature are in our list of tested genes (IFIT and EREG). Belzeaux et al.34 identified in a relatively small series of patients a considerable number of genes and microRNAs deregulated that are involved in various biological processes, most notably in nucleotide binding and chromatin assembly. They were able to select four genes that could predict treatment response. Among these four genes were TNF and IL1B, which are also in our list of tested genes. Savitz et al.35 detected a gene signature in peripheral blood of MDD patients consisting of 12 genes, among which 2 genes (ADM and TNF) were also in our list of genes. Network analysis revealed two gene networks, one clearly related to inflammation. Interestingly the inflammatory genes in the signature correlated with the grey matter volume of the caudate in magnetic resonance imaging.
Our study is congruent with these studies in identifying important inflammatory genes in circulating leucocytes being discriminative between MDD patients and HC. It also differs from these studies. First, we solely concentrated on inflammatory genes. We selected a panel of such inflammatory genes in previous studies (see before). The studies of the other investigators included genes involved in non-inflammatory processes, most notably cell proliferation and differentiation. Second, we measured gene expression not in the entire peripheral blood leucocytes population (containing around 70–80% lymphocytes), but in a discrete sub-population of peripheral blood leucocytes only, that is, in monocytes. The correlates to monocytes in the brain are the microglia, of which it is known that pro-inflammatory activation affects neuronal growth and synaptic functioning. Microglia is pro-inflammatory activated in major mental disorders.36 Third, we found overexpression of the inflammatory genes in the immune cells similar to that found in Belzeaux et al.34 and Savitz et al.35 whereas Segman et al.33 found a downregulation of genes. It must be noted that we also reported a downregulation of lymphocyte activity in postpartum psychosis, while there was strong monocyte activation. Thus, the fact that these authors used peripheral blood leucocytes instead of monocytes may explain differences found. Despite these differences, all these reported gene expression studies point to an important role of the immune and inflammatory system in MDD.
We tested the monocytes for a coherent profile of genes consisting of two mutually, strongly correlating clusters of genes, which are also upregulated in monocytes of bipolar patients, schizophrenia patients and postpartum psychosis patients. Our study thus underscores the notion already expressed by geneticists based on outcomes of GWAS studies that there must be common underlying inborn molecular vulnerabilities for the major mental disorders,37 some of which might well be inflammatory in nature.
Our upregulated gene expression profile in monocytes of melancholic drug-free inpatients with MDD is composed of a network of cytokines and pro-inflammatory molecules, many of which have previously been found upregulated when tested at the protein level in MDD patients.4 In this study, we additionally found that IL6, IL8, CCL2 and VEGF were significantly increased in the serum of our MDD patients. Interestingly there was a negative correlation between CCL2 and IL1β levels in serum with the CCL2 and IL1B gene expression in the activated monocytes. This is suggestive for the idea that the circulating pro-inflammatory activated monocytes are not the source of the elevated cytokines/chemokines in serum. However, it is also possible that the activated monocytes are the source, but the elevated cytokines downregulate the gene production in monocytes in an autocrine fashion. It is likewise possible that the cytokines are produced by other inflammatory-changed cells, such as endothelial cells or activated, migrating macrophages in the tissues and that these elevated cytokines/chemokines downregulate the gene production in monocytes in a paracrine function. Indeed our studies showed that CCL2 levels in serum correlated not only to a reduced expression of CCL2 message, but also to a reduced expression of the message for the inactivating GRβ, suggesting a generalized enhanced sensitivity of the activated monocytes to steroids due to high levels of CCL2. It is known that CCL2 is primarily produced by monocytes/macrophages shortly after having infiltrated the tissues and this phenomenon may thus represent an ongoing mild inflammatory monocyte/macrophage response in the tissues downregulating the inflammatory state of circulating monocytes to control influx. A similar phenomenon can be observed in monocytes of type 1 diabetic patients.38 The higher serum level of CCL2 found by us in MDD patients is consistent with our previous reports on higher serum levels in MDD18 and in mood disorders in general.10,12 These higher levels of CCL2 underscore the enhanced migration of monocytes into and through the tissues in major mental disorders as proposed by the immune theory.
With regard to IL8, the meta-analysis of Dowlati et al. (2009) concluded that evidence was lacking that IL8 levels were altered in MDD having evaluated four articles on IL8. IL8 is a cytokine particularly produced by macrophages when activated by IFN-γ produced by TH1 cells, the so-called M1 macrophages.39 We found IL8 clearly raised in our melancholic drug-free MDD inpatients. Severity and character of the disease may have had a role here. Serum levels of VEGF have been found largely unaltered in MDD,40 but elevations have been described in more severely ill MDD patients who are unresponsive to antidepressant treatment,18 MMD with co-morbid borderline personality disorder41 and after ECT.42 Our data also suggests a role of VEGF in MDD. VEGF is an angiogenic protein with both neuroprotection and neurotrophic actions43 and can be produced by monocytes/macrophages.44 We ourselves have previously shown an involvement of other neurotrophic factors in mood disorders.18,45,46
Our study is also the first to show that the decreased GRα/GRβ ratio in major depression occurs in the context of inflammatory activation. Our study agrees and extends that of Matsubara et al.47 who found reduced GRα mRNA in whole blood of patients with major depression. Our data also agrees with mounting evidence suggesting that inflammation itself may contribute to reduced glucocorticoid sensitivity,48 and provide a mechanism by which this maybe happening in depressed patients. We found the raised levels of IL8 in the serum of MDD patients to correlate significantly and negatively to the GRα/β ratio of gene expression in the monocytes. This can be interpreted as: the higher the production of IL8, the more reduced the glucocorticoid sensitivity of monocytes. This observation is thus compatible with the view that inflammatory cytokines can cause glucocorticoid resistance in our patients. Indeed, in conditions of chronic inflammation, pro-inflammatory cytokines can cause GR resistance49 by reducing GR affinity,16 by inhibiting GR translocation, by hormone-induced GR-mediated gene transcription,50,51 and by promoting expression of the inactive GRβ isoform of the GR.17 In addition, cytokine-mediated inflammatory processes have an important role in the development of GR resistance in the context of depression. Of particular relevance to this study, pro-inflammatory cytokines can not only induce glucocorticoid resistance in immune cells, but also in cells of the hypothalamic-pituitary-adrenal axis and therefore result in hyperactivity of the axis.51,52 In fact, studies have demonstrated that treatment with pro-inflammatory cytokines induces a decrease in GR function as evidenced by decreased sensitivity to the effects of glucocorticoids on functional endpoints and decreased GR affinity for ligand.48,53
A limitation of our approach is that we have made in our experimental design a selection of differentially expressed genes by selecting in previous whole genome analysis on monocytes of patients with major mental illnesses only the highly over- and underexpressed genes (more or less than 3.5-fold), which were clearly involved in inflammation and inflammatory processes. Although this approach proved fruitful in detecting the inflammatory signature pattern of two clusters of genes as described here and previously, we may have missed important causal genes for the inflammatory set points.
In conclusion, melancholic drug-free inpatients with major depression have an increased pro-inflammatory monocyte set point and increased levels of IL6, IL8, CCL2 and VEGF. The pro-inflammatory activation involves a decreased GRα/GRβ ratio, which is associated with the severity of the melancholic depression. Collectively, our data highlight a model for melancholic depression by which an abnormal set point of the neuro-immuno-endocrine axis leads to increased activity of the macrophage system; and suggest a mechanism by which inflammation can reduce glucocorticoid sensitivity in major depression.
References
Leonard BE . The immune system, depression and the action of antidepressants. Prog Neuropsychopharmacol Biol Psychiatry 2001; 25: 767–780.
Raison CL, Miller AH . Is depression an inflammatory disorder? Curr Psychiatry Rep 2011; 13: 467–475.
Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK et al A meta-analysis of cytokines in major depression. Biol Psychiatry 2010; 67: 446–457.
Howren MB, Lamkin DM, Suls J . Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med 2009; 71: 171–186.
Raison CL, Capuron L, Miller AH . Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol 2006; 27: 24–31.
Yirmiya R, Pollak Y, Morag M, Reichenberg A, Barak O, Avitsur R et al Illness, cytokines, and depression. Ann N Y Acad Sci 2000; 917: 478–487.
Suarez EC, Krishnan RR, Lewis JG . The relation of severity of depressive symptoms to monocyte-associated proinflammatory cytokines and chemokines in apparently healthy men. Psychosom Med 2003; 65: 362–368.
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF et al A Randomized Controlled Trial of the Tumor Necrosis Factor Antagonist Infliximab for Treatment-Resistant Depression: The Role of Baseline Inflammatory Biomarkers. JAMA Psychiatry 2013; 70: 31–41.
Bergink V, Kushner SA, Pop V, Kuijpens H, Lambregtse-van den Berg MP, Drexhage RC et al Prevalence of autoimmune thyroid dysfunction in postpartum psychosis. Br J Psychiatry 2011; 198: 264–268.
Drexhage RC, Heul-Nieuwenhuijsen L, Padmos RC, van BN, Cohen D, Versnel MA et al Inflammatory gene expression in monocytes of patients with schizophrenia: overlap and difference with bipolar disorder. A study in naturalistically treated patients. Int J Neuropsychopharmacol 2010; 13: 1369–1381.
Weigelt K, Carvalho LA, Drexhage RC, Wijkhuijs A, de WH, van Beveren NJ et al TREM-1 and DAP12 expression in monocytes of patients with severe psychiatric disorders. EGR3, ATF3 and PU.1 as important transcription factors. Brain Behav Immun 2011; 25: 1162–1169.
Bergink V, Lambregtse-van den Berg MP, Koorengevel KM, Kupka R, Kushner SA . First-onset psychosis occurring in the postpartum period: a prospective cohort study. J Clin Psychiatry 2011; 72: 1531–1537.
Beyan H, Drexhage RC, van der Heul NL, de WH, Padmos RC, Schloot NC et al Monocyte gene-expression profiles associated with childhood-onset type 1 diabetes and disease risk: a study of identical twins. Diabetes 2010; 59: 1751–1755.
Brkic Z, Maria NI, van Helden-Meeuwsen CG, van de Merwe JP, van Daele PL, Dalm VA et al Prevalence of interferon type I signature in CD14 monocytes of patients with Sjogren's syndrome and association with disease activity and BAFF gene expression. Ann Rheum Dis 2012; 72 (): 728–735.
Heul-Nieuwenhuijsen L, Padmos RC, Drexhage RC, de WH, Berghout A, Drexhage HA . An inflammatory gene-expression fingerprint in monocytes of autoimmune thyroid disease patients. J Clin Endocrinol Metab 2010; 95: 1962–1971.
Irusen E, Matthews JG, Takahashi A, Barnes PJ, Chung KF, Adcock IM . p38 mitogen-activated protein kinase-induced glucocorticoid receptor phosphorylation reduces its activity: role in steroid-insensitive asthma. J Allergy Clin Immunol 2002; 109: 649–657.
Torrego A, Pujols L, Roca-Ferrer J, Mullol J, Xaubet A, Picado C . Glucocorticoid receptor isoforms alpha and beta in in vitro cytokine-induced glucocorticoid insensitivity. Am J Respir Crit Care Med 2004; 170: 420–425.
Carvalho LA, Torre JP, Papadopoulos AS, Poon L, Juruena MF, Markopoulou K et al Lack of clinical therapeutic benefit of antidepressants is associated overall activation of the inflammatory system. J Affect Disord 2012; 148 (): 136–140.
Carvalho LA, Juruena MF, Papadopoulos AS, Poon L, Kerwin R, Cleare AJ et al Clomipramine in vitro reduces glucocorticoid receptor function in healthy subjects but not in patients with major depression. Neuropsychopharmacology 2008; 33: 3182–3189.
Besedovsky HO, del RA . Immune-neuro-endocrine interactions: facts and hypotheses. Endocr Rev 1996; 17: 64–102.
Rook GA . Glucocorticoids and immune function. Baillieres Best Pract Res Clin Endocrinol Metab 1999; 13: 567–581.
Hollenberg SM, Weinberger C, Ong ES, Cerelli G, Oro A, Lebo R et al Primary structure and expression of a functional human glucocorticoid receptor cDNA. Nature 1985; 318: 635–641.
Yudt MR, Cidlowski JA . The glucocorticoid receptor: coding a diversity of proteins and responses through a single gene. Mol Endocrinol 2002; 16: 1719–1726.
Oakley RH, Cidlowski JA . Cellular processing of the glucocorticoid receptor gene and protein: new mechanisms for generating tissue-specific actions of glucocorticoids. J Biol Chem 2011; 286: 3177–3184.
Oakley RH, Jewell CM, Yudt MR, Bofetiado DM, Cidlowski JA . The dominant negative activity of the human glucocorticoid receptor beta isoform. Specificity and mechanisms of action. J Biol Chem 1999; 274: 27857–27866.
Knijff EM, Breunis MN, van Geest MC, Kupka RW, Ruwhof C, de Wit HJ et al A relative resistance of T cells to dexamethasone in bipolar disorder. Bipolar Disord 2006; 8: 740–750.
Staal FJ, Baert MR, van Dongen JJ . Wnt target genes identified by DNA microarrays in immature CD34+ thymocytes regulate proliferation and cell adhesion. J Immunol 2004; 172: 1099–1108.
Saldanha AJ . Java Treeview--extensible visualization of microarray data. Bioinformatics 2004; 20: 3246–3248.
Rødland EA . Simes procedure is 'valid on average'. Biometrika 2006; 93: 742–746.
Simes RJ . An improved Bonferroni procedure for multiple tests of significance. Biometrika 1986; 73: 751–754.
Vermeiden M, Mulder PG, van den Broek WW, Bruijn JA, Birkenhager TK . A double-blind randomized study comparing plasma level-targeted dose imipramine and high-dose venlafaxine in depressed inpatients. J Psychiatr Res 2013; 47 (): 1337–1342.
Spijker S, Van Zanten JS, De JS, Penninx BW, van DR, Zitman FG et al Stimulated gene expression profiles as a blood marker of major depressive disorder. Biol Psychiatry 2010; 68: 179–186.
Segman RH, Goltser-Dubner T, Weiner I, Canetti L, Galili-Weisstub E, Milwidsky A et al Blood mononuclear cell gene expression signature of postpartum depression. Mol Psychiatry 2010; 15: 93–100, 2.
Belzeaux R, Bergon A, Jeanjean V, Loriod B, Formisano-Treziny C, Verrier L et al Responder and nonresponder patients exhibit different peripheral transcriptional signatures during major depressive episode. Transl Psychiatry 2012; 2: e185.
Savitz J, Frank MB, Victor T, Bebak M, Marino JH, Bellgowan PS et al Inflammation and neurological disease-related genes are differentially expressed in depressed patients with mood disorders and correlate with morphometric and functional imaging abnormalities. Brain Behav Immun 2012; 31: 161–171.
Beumer W, Gibney SM, Drexhage RC, Pont-Lezica L, Doorduin J, Klein HC et al The immune theory of psychiatric diseases: a key role for activated microglia and circulating monocytes. J Leukoc Biol 2012; 92: 959–975.
Smoller JW, Craddock N, Kendler K, Lee PH, Neale BM, Nurnberger JI et al Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 2013; 381: 1371–1379.
Bouma G, Coppens JM, Lam-Tse WK, Luini W, Sintnicolaas K, Levering WH et al An increased MRP8/14 expression and adhesion, but a decreased migration towards proinflammatory chemokines of type 1 diabetes monocytes. Clin Exp Immunol 2005; 141: 509–517.
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A . Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 2002; 23: 549–555.
Ventriglia M, Zanardini R, Pedrini L, Placentino A, Nielsen MG, Gennarelli M et al VEGF serum levels in depressed patients during SSRI antidepressant treatment. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 146–149.
Kahl KG, Bens S, Ziegler K, Rudolf S, Kordon A, Dibbelt L et al Angiogenic factors in patients with current major depressive disorder comorbid with borderline personality disorder. Psychoneuroendocrinology 2009; 34: 353–357.
Minelli A, Zanardini R, Abate M, Bortolomasi M, Gennarelli M, Bocchio-Chiavetto L . Vascular Endothelial Growth Factor (VEGF) serum concentration during electroconvulsive therapy (ECT) in treatment resistant depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35: 1322–1325.
Segi-Nishida E, Warner-Schmidt JL, Duman RS . Electroconvulsive seizure and VEGF increase the proliferation of neural stem-like cells in rat hippocampus. Proc Natl Acad Sci USA 2008; 105: 11352–11357.
Hasko G, Pacher P, Deitch EA, Vizi ES . Shaping of monocyte and macrophage function by adenosine receptors. Pharmacol Ther 2007; 113: 264–275.
Barbosa IG, Huguet RB, Sousa LP, Abreu MN, Rocha NP, Bauer ME et al Circulating levels of GDNF in bipolar disorder. Neurosci Lett 2011; 502: 103–106.
Barbosa IG, Rocha NP, Huguet RB, Ferreira RA, Salgado JV, Carvalho LA et al Executive dysfunction in euthymic bipolar disorder patients and its association with plasma biomarkers. J Affect Disord 2012; 137: 151–155.
Matsubara T, Funato H, Kobayashi A, Nobumoto M, Watanabe Y . Reduced glucocorticoid receptor alpha expression in mood disorder patients and first-degree relatives. Biol Psychiatry 2006; 59: 689–695.
Pace TW, Hu F, Miller AH . Cytokine-effects on glucocorticoid receptor function: relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun 2007; 21: 9–19.
Irwin MR, Miller AH . Depressive disorders and immunity: 20 years of progress and discovery. Brain Behav Immun 2007; 21: 374–383.
Miller AH, Pariante CM, Pearce BD . Effects of cytokines on glucocorticoid receptor expression and function. Glucocorticoid resistance and relevance to depression. Adv Exp Med Biol 1999; 461: 107–116.
Pariante CM, Pearce BD, Pisell TL, Sanchez CI, Po C, Su C et al The proinflammatory cytokine, interleukin-1alpha, reduces glucocorticoid receptor translocation and function. Endocrinology 1999; 140: 4359–4366.
Maddock C, Pariante CM . How does stress affect you? An overview of stress, immunity, depression and disease. Epidemiol Psichiatr Soc 2001; 10: 153–162.
Pariante CM, Thomas SA, Lovestone S, Makoff A, Kerwin RW . Do antidepressants regulate how cortisol affects the brain? 2003 Curt Richter Award paper. Psychoneuroendocrinology 2004; 29: 423–447.
Acknowledgements
We greatly appreciate Harm J de Wit, Angelique van Rijswijk and Annemarie Wijkhuijs for their technical help, Walter van den Broek and Esther Pluijms for their excellent clinical care, Siska Verploegh for compiling the clinical information, and Alfredo Ortigosa Aguilera for his essential database management and assistance. This study was supported in part by EU-FP7-HEALTH-F2–2008–222963 ‘MOODINFLAME’, by British Council-Partek Partnership, by the Biomedical Research Council, King’s College, London and by an ECNP Young Investigator Award to Livia Carvalho. Livia A Carvalho is also supported by the NARSAD Young Investigator Award and by the British Heart Foundation. These supporters had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Carvalho, L., Bergink, V., Sumaski, L. et al. Inflammatory activation is associated with a reduced glucocorticoid receptor alpha/beta expression ratio in monocytes of inpatients with melancholic major depressive disorder. Transl Psychiatry 4, e344 (2014). https://doi.org/10.1038/tp.2013.118
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.118
Keywords
This article is cited by
-
Associations of C-reactive protein with depressive symptoms over time after mild to moderate ischemic stroke in the PROSCIS-B cohort
Journal of Neurology (2024)
-
Evidence of innate immune dysfunction in first-episode psychosis patients with accompanying mood disorder
Journal of Neuroinflammation (2022)
-
The neuroimmunology of social-stress-induced sensitization
Nature Immunology (2022)
-
Transcriptomic signaling pathways involved in a naturalistic model of inflammation-related depression and its remission
Translational Psychiatry (2021)
-
Targeting the CCL2-CCR2 axis in depressive disorders
Pharmacological Reports (2021)