Abstract
Frailty is a well-recognized geriatric syndrome with various definitions and conceptual frameworks. This study aimed to use latent class analysis to discover potential subtypes of pre-frail and frail older people. Data from the I-Lan Longitudinal Aging Study (ILAS), a community-based cohort study was used for analysis. Latent class analysis was applied to characterize classes or subgroups with different frailty phenotypes among ILAS participants targeting older adults aged 65 and above, capable of completing a 6-meter walk, without severe major or life threatening diseases, and not institutionalized. Latent class analysis identified three distinct subgroups with different frailty phenotypes: non-mobility-type (weight loss and exhaustion), mobility-type frailty (slowness and weakness), and low physical activity. Comparing these groups with the robust group, people with mobility-type frailty had poorer body composition, worse bone health, poorer cognitive function, lower survival (hazard ratio: 6.82, p = 0.019), and poorer overall health outcomes (hazard ratio: 1.67, p = 0.040). People in the non-mobility-type group had poorer bone health and more metabolic serum abnormalities. In conclusion, mobility-type frailty was a better predictor of adverse outcomes. However, further investigation is needed to evaluate how these phenotypic subgroups may help in predicting prognosis or in developing interventions.
Similar content being viewed by others
Introduction
Frailty, a well-recognized geriatric syndrome that is characterized by loss of function and physiologic reserve, highlights the vulnerability older adults1,2. Several studies have shown that frailty may effectively predict adverse health outcomes and mortality3,4. A theoretical dynamic model that integrates biomedical and psychosocial perspectives has been proposed to evaluate frailty progression5. Though all frail elderly may share a final common pathway of functional decline due to dysregulated homeostasis of multiple organ systems6, the clinical presentations of frailty may differ greatly.
Previous studies have proposed various operational definitions and conceptual frameworks of frailty; however, despite different definitions in different study populations, the prevalence of frailty did not vary greatly2,7. Moreover, it is likely that no single operational definition of frailty will satisfy all experts, and previous studies failed to reach a consensus regarding the definition of frailty of clinical uses8. Due to the complex physiopathological process, multifaceted etiology, and diverse clinical phenotype of frailty, current studies categorize frailty into different functional domains, such as physical frailty, cognitive frailty, and social frailty9,10.
Although there are no universal criteria for assessing frailty, proper assessment of physical frailty and timely intervention may reduce subsequent disability, hospitalizations and mortality11,12. Instead of keeping creating new frailty criteria, we tried to focus on a more clearly defined and well-accepted term: “physical frailty”. Physical frailty has recently garnered extensive research interest, based on five phenotypic criteria proposed by Fried, et al. from the Cardiovascular Health Study (CHS)13: weakness; slowness; low level of physical activity; weight loss; and exhaustion. However, it was uncertain how each individual component and others were clustered. These five components may individually represent different underlying patho-etiology; however, their clustering may reveal common pathways underlying the frailty phenotype. Frailty component clusters may also suggest the existence of frailty subtypes that may help to clarify the trajectory for people with pre-frailty and frailty. Frailty subtypes may also improve the prediction of adverse outcomes and prognosis to devise effective intervention programs14. Therefore, this community-based cohort study in Taiwan employed latent class analysis (LCA), to identify distinct subgroups of subjects with different phenotype presentation(s) of pre-frail or frail status and investigated relationships between participant’s characteristics and health outcomes.
Results
Prevalence and clustering of frailty components
The prevalence of frailty and its individual components in ILAS were lower than in the CHS study population (Table 1), particularly exhaustion and slowness; however, differences in weight loss, low physical activity and weak grip strength between the ILAS and CHS cohorts were all within 5%. Table 2 summarizes the ILAS LCA results; to ascertain whether or not these components of frailty criteria aggregated into subgroups, we calculated the conditional probabilities of having each CHS frailty component within latent classes (Table 3). In two-class models, there was no evidence indicating that some components co-occurred preferentially in the specific class, whereas in three-class models, the prevalence of each component increased progressively across classes. In four-class models, excepting the expected class of clinically non-frail ILAS group as class 2, LCA showed class 1 to have very high conditional probability of low physical activity. Furthermore, class 3 had high probability of three CHS criteria including low physical activity, slowness and weakness; this class fit the CHS frailty definition best, though the prevalence differed from that obtained using CHS criteria (15.8% by LCA vs. 6.8% in ILAS). AIC favored the three-class model while BIC favored the two-class model. Results of the LCA four-class model further suggested that slowness and weakness may cluster as a unique phenotype subgroup, and that low physical activity may be another.
Mobile, non-mobile and physically inactive frailty groups
Based on the results of the LCA three-class model, we categorized participants as either mobility-type or non-mobility type frailty, or low physical activity. Table 4 shows comparisons between different groups based on LCA. Compared to robust and other frailty subtypes, the mobility group was older, had greater waist circumference, lower appendicular skeletal muscle mass, the lowest hip T-score, poorer SMAF score functional status, and lower cognitive function based on MMSE adjusted for education level. Although the mobility group had statistically greater waist circumference, there were no significant differences in BMI or total body-fat percentage between groups. On the other hand, the non-mobility group had the most depressed mood, highest risk of malnutrition, and a lower hip T-score; they also had higher levels of HbA1c and LDL-C and lower HDL-C. Compared to the robust group, mobility type frailty had higher risk for mortality and poorer composite outcomes (Table 5); this effect was more significant when low physical activity was added to mobility type frailty compared with the robust group). However survival analysis of non-mobility frailty with or without low physical activity, and low physical activity only, showed no statistically difference compared to the robust group. Figure 1 showed the Kaplan-Meier survival curves for different subgroup in ILAS participants by LCA analysis.
Adverse health outcomes
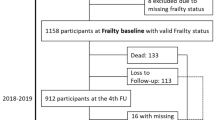
Only five participants were lost to follow-up due to changing address or being uncontactable by telephone. During average follow-up of 2.6 years, 117 outcome events were reported, including 10 emergency room visits, 57 hospitalizations, 28 falls, three long-term care facility placements, and 19 deaths.
Discussion
To the best of our knowledge, this is the first evaluation of frailty phenotypes using LCA, which suggested that components of physical frailty aggregate as a syndrome. LCA showed that four probable subgroups captured heterogeneity in the frailty definition better than two or three; however, the prevalence of these subgroups were not consistent with clinically defined pre-frail and frail groups. Interestingly, the prevalence of class 1 was similar to the non-frail group in ILAS, but the prevalence of class 2 and class 3 were discordant with the pre-frail and frail groups. In the four-class LCA model, slowness and weakness frequently aggregated together; therefore, we proposed these two criteria as mobility-type frailty. On the other hand, weight loss and exhaustion did not show such strong aggregation; hence, we grouped these components as non-mobility type frailty. Consequently, we hypothesize that frailty can be categorized into mobility type and non-mobility type.
Xue et al. proposed a cycle of frailty based on the Women’s Health and Aging Study II15, in which any frailty component could initiate the frailty cycle, and different initiators may lead to different rates of frailty progression; the most common initiator was weakness. The study also suggested that weakness, slowness, and low physical activity often co-occur and precede exhaustion and weight loss15, which could partially explain our results.
Mobility-type frailty
Lower muscle strength and/or physical performance may be attributed to loss of muscle mass or diminished muscle quality, which begin in middle-age. Various mechanisms suggested to explain these muscle changes including proteolysis, oxidative stress, dysregulation of inflammatory cytokines and hormones, physical inactivity, and undernutrition, all of which will further contribute to frailty through interactive pathways16,17. Manini et al. have attributed age-related decline in muscle strength to a combination of neurologic and muscular factors18.
Slowness (slow walking speed) and weakness (low grip strength) are frequently used to measure physical performance and muscle strength in older people19,20; however, slowness and weakness may also have a neurologic etiology. In our previous study, Huang et al. discovered that slowness and weakness with non-muscle etiology were strongly associated with cognitive impairment21. In addition, Wu et al. found that among all frailty components, slowness and weakness were the most significantly associated with cognitive impairment, and also that, rather than memory impairment, non-memory domains, such as executive dysfunction, appear early in the robust-prefrail-frail trajectory22. Accordingly, we propose that neurological degeneration may play a more important or an earlier role in physical decline than muscular degeneration itself, and that mobility-type frailty would further affect cognitive function, starting with non-memory domains. Congruently, another study reported that mobility dysfunction is often associated with cerebellar atrophy23.
In the ILAS cohort, worse mobility type frailty was associated with greater central obesity, lower appendicular skeletal muscle mass, the worst hip T-score, statistically higher comorbidity burden among all groups; this group also had poorer cognitive function, low physical performance, more people with hypertension and diabetes.
The association between aging and diminished walking speed and grip strength has been reported24,25, and both variables effectively predict poor health outcomes such as institutionalization and mortality26,27. Although there was a good correlation between the two physical measurements in frail individuals28, using either parameter alone showed a poorer prediction rate29,30.
Non-mobility-type frailty
In this study, clustering between weight loss and exhaustion was not statistically significant; this may be because weight loss and exhaustion were quantified by self-reported questionnaire, and the prevalence was low in ILAS. Besides, a previous study has suggested that weight loss and exhaustion may occur later in the cycle or trajectory of frailty, long after the mobility type phenotype manifests15. In contrast to the muscle catabolic or neurological pathway leading to mobility type frailty, the underlying mechanism of non-mobility-type frailty may be even more complicated.
Weight loss, especially among people aged 70 years and older, is a risk indicator for current health problems such as underlying diseases, and mortality31. Therefore, underlying chronic diseases, chronic inflammation, and adverse circumstances including malnutrition, loss of fat-free mass, functional decline and impaired immunity should be carefully evaluated32,33. Accordingly, screening older adults with significant weight loss for frailty has been advocated34.
Exhaustion is considered to result from energy dysregulation13. In fact, women with weight loss and exhaustion as initial presentations are more likely to get worse15. In our analysis, participants with non-mobility frailty showed no remarkable difference in body composition, besides lower hip T-score, compared to the robust group. Interestingly, they had some metabolism-related declines, including poor nutrition status, higher HbA1c, higher LDL-C and lower HDL-C serum levels. They were also the most depressed group overall. Moreover, survival analysis of the non-mobility frailty group showed no statistical difference compared to the robust group.
Low physical activity
Low physical activity may be the most ambiguous of the CHS frailty criteria. In this study (Table 3), low physical activity was isolated as one class in the four-class model. It can also combine with mobility-type phenotypes and result in a specific frailty group (class 3 in LCA four-class model). Women’s Health and Aging Study data also showed that in an LCA three-class model, concurrent weakness, slowness and low physical activity showed very high prevalence in a specific class, which they defined as frail35.
Though forming a specific LCA class, low physical activity actually broadly and strongly interacted with other frailty criteria. Slowness, weakness and skeletal muscle loss may curb older adults’ willingness to exercise, and decrease regular physical activity. Soon, diminished resting metabolism and total energy expenditure preempt undernourishment and further muscle mass loss and performance decline1,5,31. Physically inactivity also causes loss of muscle mass, by decreasing the rate of muscle synthesis or increasing muscle protein degradation36.
Furthermore, though criteria of the mobility-type subgroup and low physical activity may share similar underlying pathways, some studies have found that chronic multimorbidity and diseases strongly related to physical impairment can only explain a small part of reduced physical performance37.
Based on the Survey in Europe on Nutrition and the Elderly, Chin et al. found that unintentional weight loss was the most significant symptom associated with inactivity in frail individuals; physical inactivity alone or combined with weight loss strongly predicted less favorable health and nutritional characteristics and poorer physical functioning38. Other studies have also revealed the relationship between malnutrition, weight loss and inactivity among home-dwelling older people39. Low physical activity has been independently associated with activities of daily living and instrumental activities of daily living disability too ref.40.
Though many studies have shown that all five CHS frailty criteria have some correlation with poor clinical outcomes, we found mobility-type frailty to be more significantly associated with poor health outcomes and mortality, and the correlation was even stronger when mobility-type criteria were combined with low physical activity; however, non-mobility-type frailty did not show such a significant association with poor clinical outcomes.
Conclusion
Given the laboratory findings in this study, wasting or chronic inflammatory processes may theoretically contribute to the non-mobility phenomenon. While non-mobility-type frailty has a complicated underlying mechanism, mobility-type frailty was probably largely due to neurodegeneration; such physical frailty manifested earlier in the frailty trajectory, and was more associated with cerebellar degeneration.
The underlying mechanisms of frailty are complex, and its trajectories of clinical progression vary widely, even when we only consider physical frailty. We hypothesize that frailty can be subdivided into new phenotypic categories of mobility-type and non-mobility-type frailty. However, further investigation is needed to ascertain the additional value of these subgroups for predicting adverse outcomes or helping to develop efficient interventions.
Methods
Study subjects and design
The I-Lan Longitudinal Aging Study (ILAS) is a research cohort of community-dwelling residents aged 50 years or more from I-Lan (Yilan) County, in Northeast Taiwan. Residents were randomly sampled through the household registrations of the county government. Selected residents were invited to participate by mail or telephone invitations from the research team, and were enrolled when they had fully consented and agreed for participation. The inclusion criteria were: (i) inhabitants who then lived in I-Lan County without a plan to move in the near future; and (ii) inhabitants aged 50 years or older. Any respondents that met any one of the following conditions were excluded from the study: (i) the respondent was unable to communicate with the interviewer and grant an interview; (ii) the respondent had a poor function status, which could lead to a fail in evaluation, such as unable to complete a 6-meter timed walk within a reasonable period of time; (iii) the respondent had a limited life expectancy (in general, <6 months) because of major illnesses; (iv) currently institutionalized people. The design and participant selection have been described previously41. This substudy investigated the complex interrelationships between aging, frailty, sarcopenia, and cognitive decline; the specific aim was to identify potential subgroups of the frailty phenotype and to compare demographic characteristics and laboratory test results between subgroups. A written informed consent was obtained from every participant. The Institutional Review Board of National Yang Ming University approved the ILAS study protocol. The design and procedures of the study were carried out in accordance with the principles of the Declaration of Helsinki.
Demography, physical examinations and laboratory measurements
Study participants completed a questionnaire to elicit information on their demographic characteristics, socioeconomic status, anthropometric measurements, medical history, functional performance, and burden of chronic diseases. Comprehensive functional assessment included the Center for Epidemiologic Studies Depression Scale (CES-D) for mood status42, Mini-Mental State Examination (MMSE) for cognitive function43, Functional Autonomy Measurement System (SMAF) including activities of daily living44, and Mini-nutrition Assessment (MNA)-short form for nutritional status45. The burden of chronic diseases was evaluated using Charlson Comorbidity Index.
All participants provided an overnight, 10-hour, fasting blood sample; serum concentrations of albumin, creatinine, low-density and high-density lipoprotein cholesterol (LDL-C & HDL-C), were analyzed automatically (ADVIA 1800, Siemens, Malvern, PA, USA). Other cardiometabolic-related measurements included whole-blood glycated hemoglobin (HbA1c) and high-sensitivity C-reactive protein (hs-CRP). Hormone profiling included growth hormone, dehydroepiandrosterone sulfate (DHEA-S), insulin-like growth factor-1 (IGF-1) and 25-hydroxyvitamin D (25(OH)D).
Frailty phenotype
Modified Fried’s criteria were used to define physical frailty, which comprised exhaustion, weakness, slowness, physical inactivity, and weight loss13; the published criteria were modified by using the baseline measurements of ILAS participants – Table 1 shows the cross-validated data. Exhaustion was defined using two items of the CES-D questionnaire. Weakness was defined by low handgrip strength; slowness was defined by slow walking speed; and physical inactivity was gaged using the International Physical Activity Questionnaire46; subjects whose performance level was lower than the gender-specific lowest quintile of the study population were designated weak and/or slow and/or physically inactive according to the initial definition in the CHS study. Weight loss was defined as having either unintended weight loss exceeding 5% of body weight in the past year, or 3 kg within 3 months. Individuals fulfilling three or more CHS criteria were classified as frail, and those meeting one or two criteria were assigned pre-frail status; those negative for all five criteria were considered robust.
Body composition and bone density
All participants received a whole-body dual-energy X-ray absorptiometry (DXA) scan (Lunar Prodigy instrument, GE Healthcare, Madison, WI, USA). Total body-fat mass percentage and appendicular skeletal muscle mass (ASM), defined as the summed muscle mass of four limbs, were recorded; bone mineral density at the bilateral hip joints was measured, and the T-score was calculated.
Adverse health outcomes
Three-monthly follow-up telephone interviews were conducted to record adverse health outcomes after enrollment; these included falls, unexpected emergency department visits, hospitalizations, institutionalizations, and mortality.
Missing Data
Participants with a missing value on any of the variables were excluded from the analysis. There was no statistically difference on age, gender, and other key variables between the studied and excluded population.
Statistical analysis
LCA was used to identify distinct participant subgroups with different frailty phenotypes; LCA is a subset of structural equation modeling, which is used to detect homogeneous subgroups within a larger heterogeneous population47,48: the subtypes, termed “latent classes”, may present according the disease entities or patterns of association in the respective phenotypes. To measure co-occurrence, we tabulated frailty criteria to assess the convergent validity; LCA was then used to determine the number of classes or subgroups49. In addition, following reported recommendations, indices-of-fit of the model with different numbers of classes were compared using Pearson’s chi square50, the Akaike Information Criterion (AIC)51, and the Bayesian Information Criterion (BIC)52.
Improvements-of-fit of the models were evaluated from two up to four classes. Based on LCA results, slow and/or weak participants were statistically significantly clustered and were therefore categorized as the “mobility group”. Weight loss and/or exhaustion were also more likely to be clustered, and were categorized as the “non-mobility group”. The differences between groups of clinical characteristics and laboratory measurements were compared by one-way ANOVA with post-hoc analysis for continuous variables; comparisons between categorical data were made by χ2-test when appropriate. The Cox proportional hazard model was used to compare mortality and poor health outcomes between the mobility and non-mobility groups. Non-mobility and mobility group subjects with and without low physical activity and participants with low physical activity only, were compared to the robust group.
Statistical and LCA analysis, description of characteristics, testing differences and survival analyses were performed using SPSS 18.0 software (SPSS Inc., Chicago, IL). A two-tailed p value of ≤0.05 was considered statistically significant.
Additional Information
How to cite this article: Liu, L.-K. et al. Subtypes of physical frailty: Latent class analysis and associations with clinical characteristics and outcomes. Sci. Rep. 7, 46417; doi: 10.1038/srep46417 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Fried, L. P. et al. From bedside to bench: research agenda for frailty. Sci Aging Knowledge Environ 2005, pe24 (2005).
van Iersel, M. B. & Rikkert, M. G. Frailty criteria give heterogeneous results when applied in clinical practice. J Am Geriatr Soc 54, 728–729 (2006).
Shamliyan, T., Talley, K. M., Ramakrishnan, R. & Kane, R. L. Association of frailty with survival: a systematic literature review. Ageing Res Rev 12, 719–736 (2013).
Sternberg, S. A., Wershof Schwartz, A., Karunananthan, S., Bergman, H. & Mark Clarfield, A. The identification of frailty: a systematic literature review. J Am Geriatr Soc 59, 2129–2138 (2011).
Lang, P. O., Michel, J. P. & Zekry, D. Frailty syndrome: a transitional state in a dynamic process. Gerontology 55, 539–549 (2009).
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D. & Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 59, 255–263 (2004).
Mijnarends, D. M. et al. Instruments to Assess Sarcopenia and Physical Frailty in Older People Living in a Community (Care) Setting: Similarities and Discrepancies. J Am Med Dir Assoc (2014).
Rodriguez-Manas, L. et al. Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci 68, 62–67 (2013).
Garre-Olmo, J., Calvo-Perxas, L., Lopez-Pousa, S., de Gracia Blanco, M. & Vilalta-Franch, J. Prevalence of frailty phenotypes and risk of mortality in a community-dwelling elderly cohort. Age Ageing 42, 46–51 (2013).
Kelaiditi, E. et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging 17, 726–734 (2013).
Morley, J. E. Frailty: A time for action. European Geriatric Medicine 4, 215–216 (2013).
Lee, P. H., Lee, Y. S. & Chan, D. C. Interventions targeting geriatric frailty: A systemic review. J Clin Gerontol Geriatr 3, 47–52 (2012).
Fried, L. P. et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56, M146–156 (2001).
Chen, L. K. & Rockwood, K. Planning for frailty. J Clin Gerontol Geriatr 3, 3–4 (2012).
Xue, Q. L., Bandeen-Roche, K., Varadhan, R., Zhou, J. & Fried, L. P. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Aging Study II. J Gerontol A Biol Sci Med Sci 63, 984–990 (2008).
Fleg, J. L. & Lakatta, E. G. Role of muscle loss in the age-associated reduction in VO2 max. J Appl Physiol (1985) 65, 1147–1151 (1988).
Critchley, M. The neurology of old age: Clinical manifestation in old age. Lancet 1, 1221–1230 (1931).
Manini, T. M. & Clark, B. C. Dynapenia and aging: an update. J Gerontol A Biol Sci Med Sci 67, 28–40 (2012).
Woo, J., Ho, S. C. & Yu, A. L. Walking speed and stride length predicts 36 months dependency, mortality, and institutionalization in Chinese aged 70 and older. J Am Geriatr Soc 47, 1257–1260 (1999).
Rantanen, T. et al. Midlife hand grip strength as a predictor of old age disability. JAMA 281, 558–560 (1999).
Huang, C. Y. et al. Association of Dynapenia, Sarcopenia, and Cognitive Impairment Among Community-Dwelling Older Taiwanese. Rejuvenation Res 19, 71–78 (2016).
Wu, Y. H. et al. Cognitive Function in Individuals With Physical Frailty but Without Dementia or Cognitive Complaints: Results From the I-Lan Longitudinal Aging Study. J Am Med Dir Assoc 16, 899 e899–816 (2015).
Chen, W. T. et al. Reduced cerebellar gray matter is a neural signature of physical frailty. Hum Brain Mapp 36, 3666–3676 (2015).
Dodds, R. M. et al. Grip strength across the life course: normative data from twelve British studies. PLoS One 9, e113637 (2014).
Sampaio, R. A. C. et al. Walking speed and balance performance are associated with Short-Form 8 bodily pain domain in Brazilian older female. J Clin Gerontol Geriatr 6, 89–94 (2015).
Chen, P. J. et al. Predicting cause-specific mortality of older men living in the Veterans home by handgrip strength and walking speed: a 3-year, prospective cohort study in Taiwan. J Am Med Dir Assoc 13, 517–521 (2012).
Townsend, N. T. & Robinson, T. N. Does walking speed predict postoperative morbidity? Adv Surg 48, 53–64 (2014).
Stevens, P. J. et al. Is grip strength a good marker of physical performance among community-dwelling older people? J Nutr Health Aging 16, 769–774 (2012).
Guedes, R. C. et al. Influence of dual task and frailty on gait parameters of older community-dwelling individuals. Braz J Phys Ther 18, 445–452 (2014).
Chan, O. Y., van Houwelingen, A. H., Gussekloo, J., Blom, J. W. & den Elzen, W. P. Comparison of quadriceps strength and handgrip strength in their association with health outcomes in older adults in primary care. Age (Dordr) 36, 9714 (2014).
Morley, J. E. Weight loss in older persons: new therapeutic approaches. Curr Pharm Des 13, 3637–3647 (2007).
Roubenoff, R. et al. Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham Heart Study. Am J Med 115, 429–435 (2003).
Shilpa Amarya, K. S. & Sabharwal, Manisha . Changes during aging and their association with malnutrition. J Clin Gerontol Geriatr 6, 78–84 (2015).
Morley, J. E. et al. Frailty consensus: a call to action. J Am Med Dir Assoc 14, 392–397 (2013).
Bandeen-Roche, K. et al. Phenotype of frailty: characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci 61, 262–266 (2006).
Evans, W. J. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr 91, 1123S–1127S (2010).
Welmer, A. K., Kareholt, I., Angleman, S., Rydwik, E. & Fratiglioni, L. Can chronic multimorbidity explain the age-related differences in strength, speed and balance in older adults? Aging Clin Exp Res 24, 480–489 (2012).
Chin, A. P. M. J. et al. Inactivity and weight loss: effective criteria to identify frailty. J Nutr Health Aging 7, 55–60 (2003).
Tomstad, S. T., Soderhamn, U., Espnes, G. A. & Soderhamn, O. Living alone, receiving help, helplessness, and inactivity are strongly related to risk of undernutrition among older home-dwelling people. Int J Gen Med 5, 231–240 (2012).
Avila-Funes, J. A. et al. Cognitive impairment and low physical activity are the components of frailty more strongly associated with disability. J Nutr Health Aging 15, 683–689 (2011).
Liu, L. K. et al. Sarcopenia, and its association with cardiometabolic and functional characteristics in Taiwan: results from I-Lan Longitudinal Aging Study. Geriatr Gerontol Int 14 Suppl 1, 36–45 (2014).
Radloff, L. S. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1, 385–401 (1977).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12, 189–198 (1975).
Hebert, R., Carrier, R. & Bilodeau, A. The Functional Autonomy Measurement System (SMAF): description and validation of an instrument for the measurement of handicaps. Age Ageing 17, 293–302 (1988).
Guigoz, Y. The Mini Nutritional Assessment (MNA) review of the literature–What does it tell us? J Nutr Health Aging 10, 466–485, discussion 485–467 (2006).
Liou, Y. M., Jwo, C. J., Yao, K. G., Chiang, L. C. & Huang, L. H. Selection of appropriate Chinese terms to represent intensity and types of physical activity terms for use in the Taiwan version of IPAQ. J Nurs Res 16, 252–263 (2008).
Berlin, K. S., Williams, N. A. & Parra, G. R. An introduction to latent variable mixture modeling (part 1): overview and cross-sectional latent class and latent profile analyses. J Pediatr Psychol 39, 174–187 (2014).
Jung, T. & Wickrama, K. A. S. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass 2, 302–317 (2008).
Lazarsfeld, P. F. & Henry, N. W. Latent structure analysis. Boston: Houghton Mifflin (1968).
Goodman, L. A. Exploratory latent structure analysis using both identifiable and unidentifiable models. Biometrika 61, 215–231 (1974).
H, A. New look at statistical-model identification. IEEE Trans Automatic Control AC-19, 716–723 (1974).
Schwarz, G. Estimating the dimensions of a model. Ann Stat 6, 461–464 (1978).
Acknowledgements
We express our gratitude to the support from the Center for Geriatrics and Gerontology of Taipei Veterans General Hospital and Department of Family Medicine of Taipei Veterans General Hospital Yuanshan Branch. We also thank Dr. David Neil (PhD) of Content Ed Net (Taiwan) for provided medical writing services on behalf of Taipei Veterans General Hospital. The research was funded by Ministry of Science and Technology, R.O.C. (MOST 104-2633-B-400-001 and MOST 105-3011-B-010-001).
Author information
Authors and Affiliations
Contributions
Liu L.K. and Lee W.J. wrote the main manuscript text and responded for data collection. Guo C.Y. participated in data analysis. Chen L.K. and Liang K.Y. participated in the design of the work and drafting the article. Chen L.Y., Huang A.C., Lin M.H., and Peng L.N. provided critical reviews. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Liu, LK., Guo, CY., Lee, WJ. et al. Subtypes of physical frailty: Latent class analysis and associations with clinical characteristics and outcomes. Sci Rep 7, 46417 (2017). https://doi.org/10.1038/srep46417
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep46417
This article is cited by
-
Aging, Body Composition, and Cognitive Decline: Shared and Unique Characteristics
The Journal of nutrition, health and aging (2023)
-
The association between social activity and physical frailty among community-dwelling older adults in Japan
BMC Geriatrics (2022)
-
Sleep habits are associated with cognition decline in physically robust, but not in frail participants: a longitudinal observational study
Scientific Reports (2022)
-
Gender and physical frailty modify the association between abdominal obesity and functional disability in older adults
Aging Clinical and Experimental Research (2022)
-
Intrinsic Capacity Impairment Patterns and their Associations with Unfavorable Medication Utilization: A Nationwide Population-Based Study of 37,993 Community-Dwelling Older Adults
The Journal of nutrition, health and aging (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.