Abstract
This study investigated the incidence and risk factors of mortality in 2,476 patients with variant angina (VA) using the National Health Insurance Service–National Sample Cohort between 2004 and 2011. The risk factors of all-cause and cardiac mortality were investigated using Cox proportional hazards model. Most patients (69.5%) were less than 65 years and 42.9% were women. During the median follow-up duration of 4.9 years, there were 178 (7.2%) and 95 (3.8%) cases of all-cause and cardiac mortality, respectively. Older age, hypertension, diabetes mellitus, poor medication adherence, low household income and tertiary teaching hospitals were independent predictors for all-cause mortality, while older age, hypertension, low household income and tertiary teaching hospitals were independent predictors for cardiac mortality. In conclusion, our findings suggest that traditional risk factor control and continued medication are important to improve VA outcomes, and that household income-level factors should be considered in the assessment of risk of VA patients.
Similar content being viewed by others
Introduction
Variant angina (VA) is characterized by chest pain that is not associated with exertion, and is frequently accompanied by transient ST segment elevation on electrocardiogram1,2,3. Reversible coronary artery spasm has been established as the cause of VA4,5. Vasodilators are effective in relieving coronary artery spasm6,7,8,9,10; thus, as long as VA patients are taking vasodilators, their prognoses are better than those with atherosclerotic coronary stenosis11,12,13. However, sometimes, severe coronary spasm causes acute myocardial infarction (AMI) and fatal arrhythmia such as ventricular tachycardia, ventricular fibrillation and complete atrioventricular block, and subsequent cardiac arrest and death11,14,15. Even though some studies have investigated the outcomes and prognostic factors of patients with VA6,7,11,12,13,14,15,16,17,18,19,20,21,22, they had several weak points; first, sample sizes were relatively small and/or follow-up durations were short in most of those studies, therefore they would potentially have generalization problem; second. some of studies were performed several decades prior6,7,13,14,15, and the current VA treatment strategy using newer VA treatments such as KATP channel agonist (nicorandil)23,24, was not available for use in those studies. Therefore, investigations on VA with large subject numbers and long-term clinical follow-up duration are needed to better understand and manage this disease. Moreover, it would be helpful for such investigations to include more recent clinical practices for VA.
The purpose of this study was to determine the long-term mortality in 2,476 patients who had VA as a primary diagnosis between 2004 and 2011, and to identify the prognostic factors.
Results
Baseline characteristics of study subjects
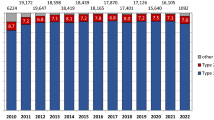
The baseline characteristics of study subjects are shown in Table 1. In all subjects (n = 2,476), most patients (69.5%) were young and middle aged (<65 years), and 42.9% were female. About two thirds of subjects had hypertension (65.2%), 21.5% diabetes mellitus, and 37.8% dyslipidemia. Approximately half (53.5%) of the subjects showed good adherence to VA medications. Most (82.6%) of the subjects were treated in tertiary teaching hospitals, and 96.8% of the subjects had health insurance. About half (45.6%) of the subjects lived in metropolitan areas. Although there were some variations in the incidence of clinical variables as well as the number of VA patients each year, no specific trends were observed from 2004 to 2011.
Mortality rates
All-cause and cardiac mortality rates are shown in Kaplan-Meyer curves (Fig. 1). During the median follow-up duration of 1,791 days (interquartile range, 1,089–2,673 days), there were 178 (7.2%) and 95 (3.8%) cases of all-cause mortality and cardiovascular mortality, respectively (Table 2). The annualized all-cause mortality and cardiovascular mortality rates of VA patients were 1.38% and 0.73%, respectively. The all-cause mortality rates were 11.2% in 2004, and 3.5% in 2011, and cardiovascular mortality rates were 4.7% in 2004 and 1.4% in 2011 with median follow-up duration of 3,431 days in 2004 and 864 days in 2011.
Mortality predictors
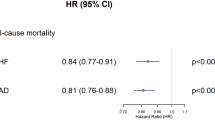
The independent predictors of all-cause and cardiovascular mortality are shown in Table 3. Older age (15–49 versus ≥65 years: hazard ratio [HR], 10.83; 95% confidence interval [CI], 5.85–20.02), hypertension (HR, 1.67; 95% CI, 1.11–2.52), diabetes mellitus (HR, 1.39; 95% CI, 1.02–1.91), poor medication adherence (HR, 1.90; 95% CI, 1.40–2.57), tertiary teaching hospitals (HR, 2.00; 95% CI, 1.25–3.22), and low household income (highest versus lowest: HR, 1.52; 95% CI, 1.00–2.30) and were independent predictors of all-cause mortality. Older age (15–49 years versus ≥65 years: HR, 6.64; 95% CI, 3.20–13.77), hypertension (HR, 1.92; 95% CI, 1.07–3.46), tertiary teaching hospitals (HR, 2.72; 95% CI, 1.30–5.66), and low household income (highest versus lowest: HR, 1.80; 95% CI, 1.04–3.11) were independent predictors of cardiovascular mortality. Poor medication adherence showed marginal statistical significance as a risk factor of cardiovascular mortality (HR, 1.50; 95% CI, 0.99–2.28).
Interactions between medication adherence and clinical variables
Interactions between poor medication adherence and mortality by age, sex, comorbidities, type of medical center, type of health security, household income, and region are shown in Table 4. There were no interaction in associations between poor medication adherences and mortality by sex, comorbidities, type of medical center, type of health security, household income, and region (P < 0.1 for each). Old age (aged ≥65 years) was the only factor having interaction with poor medication adherence in the prediction of total and cardiac mortality (P = 0.005 for each).
Factors associated with good medication adherence
Independent factors associated with good medication adherence are shown in Table 5. Older age (15–49 versus ≥65 years: OR, 1.32; 95% CI, 1.16–1.50), male sex (male versus female, OR, 0.89; 95% CI, 0.82–0.97), hypertension (OR, 1.34; 95% CI, 1.23–1.47), diabetes mellitus (OR, 1.14; 95% CI, 1.04–1.24), non-tertiary teaching hospitals (non-tertiary teaching hospital versus tertiary teaching hospital, OR, 0.72; 95% CI, 0.64–0.80), and non-metropolitan region (OR, 1.12; 95% CI, 1.03–1.21) were independent factors associated with good medication adherence.
Discussion
The results of our study of a large population of VA patients with a median follow-up of 1,791 days (=4.9 years) showed that the all-cause mortality of VA patients was 7.2% (annualized all-cause mortality rate = 1.38%) and cardiovascular mortality was 3.8% (annualized cardiovascular mortality rate = 0.73%). In VA patients, older age, hypertension, diabetes mellitus, poor medication adherence and low household income were independent risk factors of all-cause mortality, while older age, hypertension and low household income were independent risk factors of cardiovascular mortality. To the best of our knowledge, this is the largest study in the literature with a long follow-up period that shows the mortality rates and predictors in VA patients. Of additional interest, the independent association between low household income and poor VA outcomes was a meaningful and novel finding that has not been addressed in the literature to date.
The incidence of VA mortality has been reported by several studies6,7,11,12,13,14,15,16,17,18,19,20,21,22. However, those reports were limited in size and/or duration of follow-up. Bory et al.6 investigated 277 VA patients in France with a median follow-up of 7.4 years, and found all-cause and cardiac mortality rates of 7.2% and 3.6%, respectively, similar to our findings. A more recent study performed in Europe with 270 VA patients showed that 11.1% of patients died of cardiac causes after 3 years of follow-up12. The relatively high incidence of cardiac death in those patients was likely because of all the study patients had combined organic coronary stenosis. Indeed, none of the 76 VA patients without culprit coronary lesions had cardiac death in the same study12. Similarly, Figueras et al.18 reported a very low rate (7.0%) of VA-associated cardiac mortality in 273 VA patients without significant organic coronary stenosis during 12 years of follow-up. A study of Japanese nationwide registry data of 1,244 VA patients showed that the incidence of all-cause mortality and cardiac mortality during 2.7 years of follow-up was 1.3% and 0.3%, respectively25. Korean registry data including 2,129 patients with vasospasm revealed that the 2-year incidence of cardiac death was 0.9%19. Considering our study’s considerably longer follow-up duration (median 4.9 years), the rates of cardiac mortality of the previous Korean study could be expected to be similar to ours when the follow-up duration was increased about five fold. Our present study is the largest (n = 2,476) thus far with a long follow-up period (median, 4.9 years). Discrepancies among studies are mainly attributed to differences in study populations, diagnostic and management methods and length of follow-up. In general, VA prognosis has been reported to be worse in Western countries than in Asian countries24. Some previous studies that were performed several decades ago, demonstrated that annualized mortality rates of VA patients were >5%7,22, much higher than recent studies including ours.
Our results showed that VA mortality rates continuously decline from 2004 to 2011. However, this result should be interpreted cautiously because of lead-time bias. Lower mortality rates might be associated with shorter follow-up duration in patients more recently diagnosed with VA.
Several clinical parameters have been known to be risk factors of poor VA outcome. These include cigarette smoking, combined organic coronary stenosis and multi-vessel spasm20. Common cardiovascular risk factors including advanced age, hypertension and diabetes mellitus were independently associated with mortality in our study. Consistent with this finding, a previous study showed that systemic hypertension was a predictor of major coronary evens in VA patients in a multivariable analysis6. Another study also showed that more advanced age, hypertension and dyslipidemia were independent predictors of sudden cardiac death in VA patients16. However, a contradicting result indicated that traditional risk factors such as hypertension, diabetes mellitus and hypertension did not affect VA prognosis26. Further studies focused on this issue should clarify the association between classical cardiovascular risk factors and VA outcomes.
Patients’ adherence to medications is very important for the reduction of the frequency and severity of VA attacks. Abrupt cessation of medications is frequently associated with a more severe form of VA attack, as a rebound phenomenon27,28. In agreement with this finding, our study also showed that poor adherence to vasodilator therapy was independently associated with all-cause mortality in VA patients. We also showed that most of clinical variables did not have interactions with poor medication adherence in the prediction of mortality. Considering that half of patients had poor medication adherence in our study, identification of an effective medical strategy for improving medication adherence may significantly improve VA outcomes. Younger age, female sex and absence of comorbidities including hypertension and diabetes mellitus were independently associated with poor medication adherence in our study. Physicians should recognize the potential hazards of vasodilator withdrawal, and emphasize the importance of regular medications especially in young female VA patients without hypertension and diabetes mellitus to improve their outcomes as well as reduce VA attacks.
The influence of socioeconomic status on VA prognosis has not been reported. We found that lower household income was associated with an increased risk of VA mortality. The inverse relationship between socioeconomic status and other ischemic heart disease has been well described29,30. As a consistent finding, our study also showed that low household income was independently associated with increased all-cause and cardiac mortality in VA patients. Patients with lower household income may not receive appropriate prevention and management of cardiovascular disease. Risk factors are more likely to be poorly controlled, and seeking of care is delayed. Indeed, it has been shown that people with lower socioeconomic status have more unfavorable risk factors such as smoking, high blood pressure and elevated cholesterol. They also undergo fewer cardiac procedures, take fewer medications and utilize less post hospital discharge care and follow-up31. Socioeconomic status should be considered as an important factor in the assessment of risk in patients with VA, and more research is needed to further characterize this issue.
Our results showed that VA patients managed in tertiary teaching hospitals had worse prognosis than those in non-tertiary teaching hospitals. This may be due to differences in case mix, with more severe and complicated cases were transferred and managed in these hospitals.
Aside from the retrospective nature of this study, several limitations should be considered. First, errors from possible coding inaccuracy may be the main limitation of such health insurance-based database32. Serious VA-associated complications such as cardiac arrest, AMI or ventricular arrhythmia could be a primary diagnosis, and the VA diagnosis could be masked or missed. Second, methods used for VA diagnosis were not available. Third, information on other risk factors for VA outcomes such as cigarette smoking, combined atherosclerotic coronary stenosis, and multi-vessel spasm was lacking20. Additionally, information on medications other than vasodilators was lacking in our study. In particular, antiplatelets, statin and renin-angiotensin system blockers might also have an impact on patients’ survival. Fourth, the follow-up periods varied in individual patients depending on the date that VA was diagnosed, and some morality cases may not have been recorded when the patients were not being monitored. Despite these potential limitations, the present study has important clinical implications because a real-world large sample sized data from a national database was used, and without selection bias.
In conclusion, the present nationwide study showed that the annualized all-cause mortality and cardiac mortality rates of Korean VA patients were 1.38% and 0.73%, respectively. Older age, hypertension, diabetes mellitus, poor medical adherence and low socioeconomic status were associated with VA mortality. These findings provide additional evidence that traditional risk factor control and continued medication are important to improve VA outcomes. In addition, our study suggests that household income-level factors should be considered in the assessment of risk of VA patients.
Methods
Data sources
We used 2002–2013 data from the National Health Insurance Service–National Sample Cohort (NHIS-NSC), a population-based cohort established by the National Health Insurance Service (NHIS) in South Korea33. Korea has been operating the mandatory universal healthcare coverage system through the NHIS33. Every Korean citizen must be covered by the mandated universal healthcare system from birth to death, either National Health Insurance (NHI) for general populations or Medical Aid (MA) for the vulnerable, which is being managed by NHIS34. Financially, NHI is mainly funded by NHI premiums gathered from beneficiaries and receiving some government subsides, while MA is funded by taxes. MA is the only option available for the Korean populations who are unable to pay the NHI premium (e.g., low-income families), similar to Medicaid in the United States34. As of 2011, there were 50,908,646 citizens of Korea, consisting of 49,299,165 (96.8%) NHI beneficiaries and 1,609,481 (3.2%) MA recipients35. NHIS provides benefits for prevention, diagnosis, and disease and injury treatment, as well as rehabilitation, births, deaths, and health promotion. NHIS gathers, maintains, and stores all medical claims in a database consisting of diagnoses, treatments, healthcare utilization, and prescriptions33. For example, NHIS had 1.3 billion medical claims from Korean citizens in 201134. NHIS established the National Health Insurance Service–National Sample Cohort (NHIS-NSC), a population-based cohort database, whose sole purpose is to provide public health researchers and policy makers with representative and useful information regarding citizens’ healthcare utilizations and health statu33.
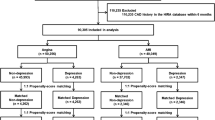
We used 2002–2013 data from NHIS-NSC, released by NHIS in 2014. This cohort data contains 1,025,340 people (as of 2002, approximately 2.2% of the entire Korean population) who were randomly selected for representing the entire Korean population33. In order to make randomized cohort samples, NHIS used probabilistic sampling to represent an individual’s total annual medical expenses within each of 1476 strata defined by age, sex, eligibility status (employed or self-employed), and income level (20 quartiles for each eligibility status and MA recipients) combinations via proportional allocation from the 46,605,433 Korean residents in 200233,36,37. In particular, NHIS-NSC was designed to be a semi-dynamically constructed cohort database; the cohort has been followed up to either the time of the participant’s disqualification from receiving health services due to death or emigration or until the end of the study period, whereas samples of newborn infants are included annually33,36,37. The database contains eligibility and demographic information regarding NHI beneficiaries as well as data on MA recipients, medical bill details, medical treatment, disease histories, and prescriptions33,36,37. NHIS-NSC data accessed in the current study included demographic information, including sex, age, residence regions, household income, and type of health security. In addition, inpatient and outpatient medical care utilization information for primary and subsidiary causes, including date of service, and drugs prescribed were included. The causes of medical care utilization or death were recorded under the International Classification of Diseases, 10th reversion (ICD-10). We included study subjects whose (1) primary cause of medical service usage was ‘I201 ’ or (2) subsidiary cause of ‘I201’ and cause of death of ‘I’, with no prior medical service usage under ‘I201’, either primary or subsidiary, before the time of inclusion in the study. For the onset of VA, we established 2002 to 2003 as the washing-out period, and excluded patients with any treatment or diagnosis history of VA during this period. To specifically detect new VA patients, we established a washing-out period from at least two years to nine years. Figure 2 shows the detailed information about how new enrollees were selected in each consecutive year from 2004 to 2011 after applying at least 2 year to maximum to 9 year washing out period. Using this model, enrollees in 2004 were the new onset VA patients with no prior diagnosis of VA during 2002–2003. (specifically, 267 enrollees in 2005 were new patients who were never diagnosed or treated for VA during 2002–2004 and 430 enrollees in 2011 were new patients with no record of VA during 2002–2010). Accordingly, patients with VA onset in 2004 would have a maximum follow up duration of nearly 10 years, and patients with VA onset in 2011 would have less follow up duration, but the duration would be >2 years. Follow-up for all VA patients was completed at the end of 2013 (Fig. 2).
Baseline clinical data
The subjects’ ages were grouped into 15–49, 50–64, and ≥65 years. Information on cardiovascular risk factors including hypertension (ICD-10 I100, I101 and I109), diabetes mellitus (ICD-10 E10–E14), and dyslipidemia (ICD-10 E78) was obtained. To assess medication adherence, all drugs administered to patients for a year after onset of VA were reviewed. In order to evaluate medication adherence, we used medication possession ratio (MPR), a ratio of total days’ supply to numbers of days of study participation per participant38,39. Good medication adherence was defined as a cumulative medication adherence of more than 80% (approximately annually 300 days) per study period among patients with VA prescribed in a given period and included data only on VA medication prescription dispensed from pharmacies40,41. In this study, VA medication refers vasodilators including diltiazem, verapamil, nitrate, nicorandil, and molsidomin. Household income was stratified into three groups according to income quintile: quintile 1–3, quintile 4–8, and quintile 9–10 groups. Metropolitan areas referred to seven major cities (Seoul, Busan, Daegu, Incheon, Gwangju, Daejeon, and Ulsan) in South Korea.
Mortality data
NHIS-NSC records were merged with certified date of death from the Statistics Korea, and the cause of death and death date were recorded. Cardiovascular death was defined as a case with circulatory cause of death (ICD-10 I00-I99). For the death date, information on only the year and month of death was obtained, and the following methods were used to calculate the follow-up duration until death: if the date of final medical care utilization was in the year and month as that of death, we set the death date by adding a nursing period (days) to the start of the date of care. In case the date of final medical care utilization was not in the same year or month as that of death, we set the death date on the middle of the year and month.
Statistical analysis
Descriptive statistics of the study population are presented as n (%) for dichotomous variables and mean ± standard deviation for continuous variables. Cox proportional hazards model was used to investigate the association of candidate risk factors with mortality. For censored cases, we set the end of the follow-up point as the last date of medical care utilization, since it was certain that these patients were alive when they utilized the medical care services. Age, sex, cardiovascular risk factors, medication adherence, type of medical center, type of health security, household income, and residence region were considered as potential confounders and were adjusted during multivariable Cox regression analysis. For the interaction analyses, we fitted cross-product terms between poor medication adherence and clinical variables in order to investigate whether the effect of poor medication adherence on mortality was changed by other clinical variables. Multiple binary logistic regression analysis was performed to investigate independent factors for good medication adherence. Age, sex, cardiovascular risk factors, type of medical center, type of health security, household income, and residence region were considered as potential confounders and were adjusted during Multiple binary logistic regression analysis. All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and P < 0.05 was regarded as statistically significant.
Ethical Statement
Ethical approval was waived in this study by the Institutional Review Board (IRB) of Boramae Medical Center (Seoul, Korea) (#IRB No. 07-2016–13). Informed consent was not obtained because patient records and information were anonymized and de-identified prior to analysis.
Additional Information
How to cite this article: Kim, H.-L. et al. Incidence and factors associated with mortality in 2,476 patients with variant angina in Korea. Sci. Rep. 7, 46031; doi: 10.1038/srep46031 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Kusama, Y. et al. Variant angina and coronary artery spasm: the clinical spectrum, pathophysiology, and management. J. Nippon. Med. Sch. 78, 4–12 (2011).
Prinzmetal, M., Kennamer, R., Merliss, R., Wada, T. & Bor, N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am. J. Med. 27, 375–388 (1959).
Yasue, H., Nakagawa, H., Itoh, T., Harada, E. & Mizuno, Y. Coronary artery spasm – clinical features, diagnosis, pathogenesis, and treatment. J. Cardiol. 51, 2–17 (2008).
Endo, M., Hirosawa, K., Kaneko, N., Hase, K. & Inoue, Y. Prinzmetal’s variant angina. Coronary arteriogram and left ventriculogram during angina attack induced by methacholine. N. Engl. J. Med. 294, 252–255 (1976).
Hillis, L. D. & Braunwald, E. Coronary-artery spasm. N. Engl. J. Med. 299, 695–702 (1978).
Bory, M. et al. Coronary artery spasm in patients with normal or near normal coronary arteries. Long-term follow-up of 277 patients. Eur. Heart. J. 17, 1015–1021 (1996).
Waters, D. D. et al. Factors influencing the long-term prognosis of treated patients with variant angina. Circulation 68, 258–265 (1983).
Kosugi, M. et al. Effect of long-term nitrate treatment on cardiac events in patients with vasospastic angina. Circ J. 75, 2196–2205 (2011).
Lombardi, M. et al. Efficacy of isosorbide-5-mononitrate versus nifedipine in preventing spontaneous and ergonovine-induced myocardial ischaemia. A double-blind, placebo-controlled study. Eur. Heart. J. 14, 845–51 (1993).
Pesola, A., Lauro, A., Gallo, R., Madeo, A. & Gosentino, G. Efficacy of diltiazem in variant angina. Results of a double-blind crossover study in CCU by Holter monitoring. The possible occurrence of a withdrawal syndrome. G. Ital. Cardiol. 17, 329–339 (1987).
Myerburg, R. J. et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N. Engl. J. Med. 326, 1451–1455 (1992).
Ong, P., Athanasiadis, A., Borgulya, G., Voehringer, M. & Sechtem, U. 3-year follow-up of patients with coronary artery spasm as cause of acute coronary syndrome: the CASPAR (Coronary Artery Spasm in Patients with Acute Coronary Syndrome) study follow-up. J. Am. Coll. Cardiol. 57, 147–152 (2011).
Yasue, H. et al. Long-term prognosis for patients with variant angina and influential factors. Circulation 78, 1–9 (1988).
Nakamura, M., Takeshita, A. & Nose, Y. Clinical characteristics associated with myocardial infarction, arrhythmias, and sudden death in patients with vasospastic angina. Circulation 75, 1110–1116 (1987).
Okumura, K. et al. Multivessel coronary spasm in patients with variant angina: a study with intracoronary injection of acetylcholine. Circulation 77, 535–542 (1988).
Ahn, J. M. et al. Prognosis of variant angina manifesting as aborted sudden cardiac death. J. Am. Coll. Cardiol. 68, 137–145 (2016).
Bugiardini, R., Manfrini, O., Pizzi, C., Fontana, F. & Morgagni, G. Endothelial function predicts future development of coronary artery disease: a study of women with chest pain and normal coronary angiograms. Circulation 109, 2518–2523 (2004).
Figueras, J., Domingo, E., Ferreira, I., Lidon, R. M. & Garcia-Dorado, D. Persistent angina pectoris, cardiac mortality and myocardial infarction during a 12 year follow-up in 273 variant angina patients without significant fixed coronary stenosis. Am. J. Cardiol. 110, 1249–1255 (2012).
Shin, D. I. et al. The 24-month prognosis of patients with positive or intermediate results in the intracoronary ergonovine provocation test. JACC. Cardiovasc. Interv. 8, 914–923 (2015).
Takagi, Y. et al. Prognostic stratification of patients with vasospastic angina: a comprehensive clinical risk score developed by the Japanese Coronary Spasm Association. J. Am. Coll. Cardiol. 62, 1144–1153 (2013).
Takahashi, J. et al. Prognostic impact of chronic nitrate therapy in patients with vasospastic angina: multicentre registry study of the Japanese Coronary Spasm Association. Eur. Heart. J. 36, 228–237 (2015).
Walling, A. et al. Long-term prognosis of patients with variant angina. Circulation 76, 990–997 (1987).
JCS joint working group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008). Cir. J. 74, 1745–1762 (2010).
Kurisu, S. et al. Usefulness of massiv eoral nicorandil in a patient with variant angina refractory to conventional treatment. Inter. Med. 42, 163–167 (2003).
Shimokawa, H. et al. Clinical characteristics and long-term prognosis of patients with variant angina. A comparative study between Western and Japanese populations. Int. J. Cardiol. 18, 331–349 (1988).
Takatsu, F. & Watarai, M. Mild stenosis makes prognosis of vasospastic angina worse. Coron. Artery. Dis. 22, 1–5 (2011).
Lette, J., Gagnon, R. M., Lemire, J. G. & Morissette, M. Rebound of vasospastic angina after cessation of long-term treatment with nifedipine. Can. Med. Assoc. J. 130, 1169–1171, 1174 (1984).
Takagi, Y. et al. Clinical characteristics and long-term prognosis of vasospastic angina patients who survived out-of-hospital cardiac arrest: multicenter registry study of the Japanese Coronary Spasm Association. Circ. Arrhythm. Electrophysiol 4, 295–302 (2011).
Gonzalez, M. A., Rodriguez Artalejo, F. & Calero, J. R. Relationship between socioeconomic status and ischaemic heart disease in cohort and case-control studies: 1960-1993. Int. J. Epidemiol 27, 350–358 (1998).
Kaplan, G. A. & Keil, J. E. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 88, 1973–1998 (1993).
Jones, C. A. et al. Cardiovascular disease risk among the poor and homeless – what we know so far. Curr. Cardiol. Rev. 5, 69–77 (2009).
Kim, H. L. et al. Incidence and risk factors associated with hospitalization for variant angina in Korea. Medicine 95, e3237 (2016).
Lee, J., Lee, J. S., Park, S. H., Shin, S. A. & Kim, K. Cohort profile: the National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol doi: 10.1093/ije/dyv319 (2016).
Park, S. B. et al. Prevalence and incidence of osteoporosis and osteoporotic vertebral fracture in Korea: Nationwide epidemiological study focusing on differences in socioeconomic status. Spine 41, 328–336 (2016).
Park, S. Y., Lee, J. Y., Lim, N. G. & Hong, Y. H. Incidence and prevalence of myasthenia gravis in Korea: A population-based study using the National Health Insurance Claims Database. J. Clin. Neurol. 12, 340–344 (2016).
Kang, Y. M., Kim, Y. J., Park, J. Y., Lee, W. J. & Jung, C. H. Mortality and causes of death in a national sample of type 2 diabetic patients in Korea from 2002 to 2013. Cardiovasc. Diabetol. 15, 131 (2016).
Kim, N. H. et al. Body Mass Index and Mortality in the General Population and in Subjects with Chronic Disease in Korea: A Nationwide Cohort Study (2002–2010). PloS. One. 10, e0139924, (2015).
Hess, L. M., Raebel, M. A., Conner, D. A. & Malone, D. C. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann. Pharmacother 40, 1280–1288 (2006).
Skaer, T. L., Sclar, D. A., Robison, L. M., Markowski, D. J. & Won, J. K. Effect of pharmaceutical formulation for diltiazem on health care expenditures for hypertension. Clin. Ther. 15, 905–911 (1993).
Ko, S. H. et al. Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002–2013: Nationwide population-based cohort study. Medicine 95, e4018 (2016).
Washington, D. L. et al. Racial variations in Department of Veterans Affairs ambulatory care use and unmet health care needs. Mil. Med. 167, 235–241 (2002).
Author information
Authors and Affiliations
Contributions
H.L.K. and J.Y.L. contributed to the idea and design of this study; J.K. and J.Y.L. prepared and checked clinical coding, undertook the data analysis; H.L.K. and J.K. wrote the draft; H.J.K. and W.H.L. contributed to data collection and analysis; and J.Y.L. revised the manuscript; all authors have seen and approved the final version of the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Kim, HL., Kim, J., Kim, H. et al. Incidence and factors associated with mortality in 2,476 patients with variant angina in Korea. Sci Rep 7, 46031 (2017). https://doi.org/10.1038/srep46031
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep46031
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.