Abstract
Catestatin was discovered as a potent inhibitor of catecholamine secretion and plays important roles in the cardiovascular system. Our previous study demonstrates a close relationship between catestatin levels and prognosis of ST-elevation myocardial infarction (STEMI). Using the same population, the goal of this study is to investigate the ability of catestatin to predict left ventricular (LV) remodeling in STEMI patients. 72 patients and 30 controls were included. Catestatin was sampled after admission to the emergency room (ER), at day3 (D3), and day7 (D7) after STEMI. Echocardiography was performed at D3 and after 65 months for evaluation of LVEDD, EF, IVS, LVPW, E, A, E’, E/A, and E/E’. The changes of these parameters from D3 to 65 months were used to reflect the changes of ventricular structure and function. We found that plasma catestatin levels at D3 were highly correlated with the changes of LVEDD, EF, E, A, E’, E/A, as well as E/E’. Patients with higher catestatin levels developed worse ventricular function during the follow-up period. Single-point catestatin was effective to predict LVEDD change. And concurrently increasing catestatin and NT-proBNP levels predicted the highest risk of LV remodeling. This study suggests an important prognostic information of catestatin on LV remodeling.
Similar content being viewed by others
Introduction
Left ventricular (LV) remodeling refers to the process by which ventricular size, structure and function are regulated by mechanical, neurohormonal, and genetic factors (refer to review1). It is driven by a combination of pathologic cardiomyocyte hypertrophy, cardiomyocyte apoptosis, myofibroblast proliferation, and interstitial fibrosis2. Following acute myocardial infarction (AMI), LV remodeling is a major predictor of morbidity and mortality3. Currently, echocardiography has been recommended as a routine examination to assess LV function in clinic4. However, it’s still not ubiquitously used because of high cost and need of specialists, especially in developing countries. In addition, when echocardiography shows positive signs, LV remodeling has already happened, which prevents its usage as an early indicator. Therefore, it’s essential to find a relatively easy and cost-effective way to identify patients with higher risk of LV remodeling at early stage after AMI, which promotes further interventions to prevent LV dilation.
In early studies, researchers demonstrated that the degree of chamber remodeling was highly associated with the extent of myocardial injury3 and factors like anterior infarct location5 and patency of the infarct-related artery6, etc. Pathologic LV remodeling is also closely linked to activation of a series of neuroendocrine, such as renin-angiotensin-aldosterone axis and the adrenergic nervous system. For clinical use, some biomarkers had been identified to predict LV remodeling, which include B-type natriuretic peptide (BNP)7, cardiac troponin I8, and serum Tenascin-C9. However, the predictive role of catestatin in LV remodeling has never been investigated.
Catestatin is a 21-amino acid peptide generated endogenously by proteolytic cleavage of its precursor chromogranin A (CHGA)10, which is co-stored and co-released with catecholamines. It has been intensively studied in cardiovascular system in recent years, which displayed potent vasodilatory effect in both rate and human11,12. In addition, catestatin exerts cardio-protective influence under Ischemia/Reperfusion condition, proved by several groups13,14. Our previous studies also indicated that catestatin had a predictive effect to detect stage B heart failure15 and was correlated to prognosis of patients with AMI16. Based on these functions in the cardiovascular system, we hypothesized that catestatin level might be useful for the diagnosis and determination of LV remodeling following AMI. So in this study, we assessed plasma catestatin concentrations with reference to LV function.
Results
Baseline characteristics
The baseline demographics, echocardiography and other laboratory findings are detailed in Table 1. In summary, 72 patients (age, 61.3 ± 14.4; sex, 81.9% male) with STEMI and 30 control subjects (age, 59.8 ± 10.4; sex, 76.7% male) were included. The baseline characteristics were compared between Control and STEMI patients. Patients with AMI had dramatically higher heart rates, Hs-CRP concentrations, as well as fasting glucose levels. For the echocardiography parameters, the EF, E, A, E’, E/E’ of AMI patients were significantly lower than those of control subjects, but other factors were comparable such as age, gender, etc.
Correlation coefficients
We have earlier reported that plasma catestatin achieved its highest level at D3 after STEMI (Supplementary Figure 1), which was an independent predictor of adverse events16. Here the correlations between catestatin concentrations at D3 and ΔLVEDD, ΔEF, ΔIVS, ΔLVPW, ΔE, ΔA, ΔE’, ΔE/A, ΔE/E’ were analyzed. As shown in Fig. 1a–i, the concentrations of catestatin were highly correlated with the changes of LVEDD (p < 0.0001), EF (p = 0.0002), E (p = 0.0003), A (p < 0.0001), E’ (p < 0.0001), E/A (p < 0.0001), as well as E/E’ (p < 0.0001). In addition, we examined the relationship between catestatin and N-terminal pro b-type natriuretic peptide (NT-proBNP), and found these two parameters were positively correlative with each other (Fig. 1j).
(a–i) Scatter plots (with Pearson or Spearman’s correlation coefficients) showing the correlation between catestatin concentrations at D3 and changes of echocardiography parameters including LVEDD, EF, IVS, LVPW, E, A, E’, E/A, and E/E’. j, Scatter plots showing the correlation between catestatin concentrations at D3 and NT-proBNP concentrations.
Comparison of catestatin levels and changes of echocardiography parameters according to different grouping methods
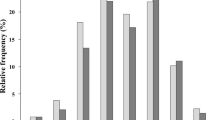
First, patients were divided into 2 groups based on the median level of catestatin at D3 (28.71 ng/ml); the changes of echocardiography parameters as well as other characteristics listed in Table 1 were compared between these 2 groups. As summarized in Table 2, the high catestatin group had increased LVEDD, decreased EF, decreased E, increased A, decreased E’, decreased E/A, as well as increased E/E’, all of which are indicative to worse LV function, but there was no difference of other characteristics except for higher diastolic blood pressure and LDL cholesterol concentration in high catestatin group. When we compared the percentage of patients who developed worse conditions (increased LVEDD, decreased EF, decreased E, increased A, decreased E’, decreased E/A, and increased E/E’) between these 2 groups, we found more patients in the high catestatin group tended to have LV remodeling (Table 3). Second, on the basis of changes of echocardiography parameters, patients were then separated into 2 sets: one was named as “Worse” (with increased LVEDD, or decreased EF, or increased IVS, or increased LVPW, or decreased E, or increased A, or decreased E’, or decreased E/A or increased E/E’, respectively); the other one was called “not Worse” (otherwise), we found that among these parameters detected, except for IVS and LVPW, patients with worse conditions had higher levels of catestatin (Fig. 2a). At last, we scored individual patient according to these 9 echocardiography parameters assessed: each parameter is 1 point, and the final score of each patient represents how many parameters became worse during the follow-up period, indicating the severity of LV remodeling (for example, if a patient only has worse LVEDD and worse EF, the score would be 2). Using this stratification strategy, we found patients with more severe outcomes tended to have higher catestatin concentrations (Fig. 2b).
(a) Histograms showing the comparison of catestatin concentrations at D3 between “Worse” group and “Not worse” group. (b) Patients were stratified according to different scores, and catestatin concentrations were compared between these groups. Whiskers denote the minimal value and max value. Error bars, SD. *p < 0.05, **p < 0.01, ***p < 0.001.
ROC analysis of catestatin level for predicting LV remodeling
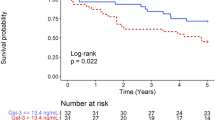
We performed ROC analysis of catestatin levels at D3 for prediction of LV remodeling, as illustrated by the following echocardiography parameters: ΔLVEDD, ΔEF, ΔE, ΔA, ΔE’, ΔE/A, ΔE/E’ (Fig. 3a–g). The AUC for prediction of ΔLVEDD was 0.9095, the highest among the analyzed variables. The best cut-off value was 32.93 ng/ml, with a sensitivity of 93.88% and specificity of 86.96%. To compare the predicting value of catestatin and NT-proBNP, we also performed ROC analysis of NT-proBNP (Supplementary Figure 2), and we found that even though comparable, the AUCs of castestatin were slightly higher than that of NT-proBNP.
Concurrently increasing catestatin and NT-proBNP levels predicted the highest risk of LV remodeling
Patients were grouped according to the catestatin and NT-proBNP median values (catestatin, 28.71 ng/ml; NT-proBNP, 472 pg/ml). Multivariate logistic regression found that concurrent increases in catestatin and NT-proBNP predicted the greatest risk [OR = 24.645 (95%CI: 2.869–211.698, p = 0.003)] (Table 4).
Discussion
In STEMI, timely reperfusion therapy can reduce infarct size, preserve left ventricular function and improve clinical outcomes. However, as one of the strongest predictors of subsequent mortality, LV remodeling occurs in an appreciable proportion of patients with AMI, even those successfully treated with pPCI. Early identification of high-risk patients allows for early intervention with targeted treatment strategies and close follow-up. But currently, a major challenge in clinic is to discriminate between patients with reversible dysfunction and those who will experience little functional recovery accompanied by LV remodeling, which necessitates the development of new strategies to predict adverse events at early stages. It has been shown that the plasma concentration of catestatin is altered during the course of AMI, and it is associated with poor prognosis such as heart failure and death16. But the role of catestatin in the pathophysiological process of AMI and its relationship with LV remodeling are largely unknown. So in this study, we aim to assess the ability of catestatin level in plasma to predict functional recovery and extent of LV remodeling.
As a follow-up of our previous study16, the current study investigated the relationship between catestatin levels at D3 and the extent of LV remodeling, determined by the changes of LVEDD, EF, E, A, E’, E/A, and E/E’. We showed that catestatin was highly correlated with the changes of these parameters. In addition, when patients were separated into two groups according to the median concentration of catestatin, we found that patients with higher levels of catestatin tended to develop worse LV function. In addition, catestatin concentrations were also positively correlated with LV remodeling severity. At last, ROC analysis suggested catestatin as a prognostic indicator with high sensitivity and specificity. When comparing prognostic value of catestatin with well-known factor NT-proBNP, catestatin had slightly stronger effects in terms of ROC curves. And patients with concurrently increasing catestatin and NT-proBNP levels had the highest risk of worse LV functions. Overall, We demonstrated that a single measurement of catestatin, obtained at D3 after interventional management, provided useful prognostic information on changes in LV volume and function. Since catestatin can be measured in plasma collected with standard equipment, stored for prolonged period, and analyzed without tedious extraction procedures, developing the clinical use of catestatin might be of great importance.
Cardiac remodeling is generally accepted as a determinant of the clinical course of heart failure (HF), which can be considered a primary target for treatment and a reliable surrogate for long-time outcomes. It is manifested clinically as changes in structure and function of the heart resulting from cardiac load or injury, such as AMI. Using noninvasive imaging like echocardiography, physicians and researchers are able to analyze the mechanisms by which biochemical and cellular events contribute to these changes during remodeling. In the current study, the myocardial functions can be assessed through the following parameters: EF for systolic function; E, A, E’, E/A, and E/E’ for diastolic function. We found that patients with higher catestatin levels at D3 developed worse systolic as well as diastolic function during the follow-up period. It has been shown that in isolated avascular frog heart, catestatin dose-dependently decreased stroke volume and stroke work, noncompetitively inhibited the positive inotropic action of isoproterenol and the positive inotropic effect of endothlin-117, suggesting its cardio-suppressive function. In addition, another group demonstrated the cardio-protective role of catestatin, which appeared mainly due to a direct reduction of post-ischemic myocardial damages and dysfunction, with infarct size reduced and left ventricular function improved18. Recently, Bassino et al. confirmed this effect using isolated adult rat cardiomyocytes undergoing simulated ischemia/reperfusion injury, and determined PI3K/NO/cGMP pathway as well as preservation of mitochondrial membrane potential were involved19. Because infarction expansion and post-ischemic reperfusion are two major factors contributing to myocardial function after AMI, it’s rationale to surmise that catestatin performed a protective role in this process.
Apart from the worsening of myocardial functions, our results also showed that catestatin levels at D3 were positively associated with the increase of LVEDD, a parameter indicating cardiac structure change. Because cardiomyocytes and extracellular matrix (ECM) are two essential components of the myocardium, the pathological alterations of them will provide insights into the remodeling process. For cardiomyocytes, the most important change after AMI is hypertrophy. Cardiomyocyte hypertrophy is characterized by an increase in cell size, enhanced protein synthesis, and heightened organization of the sarcomere20. It is a progressive response to the elevated load on the heart, which results in an increase of cardiac mass. It has been demonstrated for decades that the renin-angiotensis-aldosterone system (RAAS), regulated by catecholamine, contributes to the pathogenesis of cardiac hypertrophy21. As a peptide widely known to inhibit catecholamine release from both chromaffin cells and noradrenergic neurons10, catestatin performed a possible antihypertrophy function in cardiac tissue through the RAAS pathway. In addition, catestatin can lower the blood pressure through inducing histamine release from mast cells22, antagonizing both central neuronal nicotinic acetylcholine receptor (nAChR) and β-adrenoceptors (β-ARs) to decrease the sympathetic tone23, as well as decreasing reactive oxygen species (ROS) and increasing nitric oxide (NO). All of these suggested that catestatin exerts a protective action on hypertrophy by decreasing the pressure signal and cardiac afterload. For ECM, one of the most important pathological features of cardiac remodeling is fibrosis, and ECM degradation is closely involved in this process. Previous study showed that angiotensin II (Ang II) induced profibrogenic effects in vascular diseases24,25 and increased the expression and activity of various matrix metalloproteinase (MMPs), such as MMP-2 and MMP-925. So the inhibition of catestatin on Ang II function performed an antifibrosis role of this peptide. Furthermore, sharing several common regulating factors with hypertrophy, cardiac fibrosis is also affected by catestatin through regulating NO and ROS production26,27. Taken together, catestatin participates in the regulation of related pathways and contributes to the inhibition of cardiac remodeling.
Petersen et al. demonstrated that catecholamine activation in patients with AMI, as measured by plasma adrenaline and noradrenaline, showed an early and rapid increase in the first 3 days and was restricted to the first 5 days, with values unchanged after 1 year compared to those at discharge, at day 628. This study also suggested that the magnitude of the early catecholaminergic activation negatively correlated with left ventricular systolic performance28. As the inhibitor of catecholamine release, we speculated that the increased sympathoadrenal activities might promote negative feedback and increase the concentration of catestatin, which helps to alleviate the harmful effect of catecholamine. As mentioned before, catestatin exerts cardio-protective function through several mechanisms. Therefore, the increase of catestatin in patients with AMI may protect the myocardium. Because catestatin peaked within one week after infarction, and is relatively easy as well as cost-effective to measure, we suggest that it could be a useful and early predictive marker for LV remodeling. Furthermore, it’s not surprising that catestatin and NT-proBNP manifested a synergistic role in the prediction of LV remodeling after AMI, because NT-proBNP are substances that are produced in the heart and released in response to ventricular wall stress caused by volume and pressure overload, and it’s an established marker to evaluate the severity of heart failure. Therefore, tailoring the multifactor stratification strategy might largely increase the predictive values.
To the best of our knowledge, this is the first study presenting that catestatin might be a novel marker reflecting LV remodeling in the myocardium following AMI. In summary, we observed a positive association between catestatin concentrations at D3 and LV remodeling. However, despite the findings, there are still some limitations in the current study. First, the sample size was relative small. Second, this was a one-center study. Third, we just assessed the changes of echocardiographic parameters instead of giving a certain definition of LV remodeling, which might cause obscuration when making clinical decisions. Therefore, further large-scale investigations and careful comparisons are required to confirm the predictive ability of catestatin in LV remodeling in AMI patients.
Methods
Study population
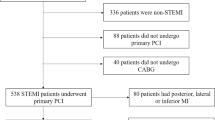
A total of 117 consecutive patients with the first AMI admitted to the Department of Cardiology, Peking University Third Hospital, from June 2008 to April 2009 were included, 17 of them were lost to follow-up. In the rest of the 100 patients, we were able to get echocardiography parameters at D3 and 65 months from 72 of them, so this study is based on the information of these 72 patients. All patients received successful primary percutaneous coronary intervention (pPCI) within 12 h from the AMI symptoms onset. The ST segment elevation myocardial infarction (STEMI) was diagnosed according to the American College of Cardiology/American Heart Association guideline in 200429. The study excluded patients with chronic obstructive pulmonary disease, significant kidney or hepatic diseases, tumor, and infectious diseases. During the same study period, 30 subjects who were admitted to the same hospital because of atypical chest pain but with normal coronary arteries confirmed by coronary angiography were included as controls, Resting blood pressure and heart rates (HRs) were measured at the same time when blood samplings were performed in triplicate in the supine position, using an oscillometric device (Philips IntelliVue MP20, Germany). This study was approved by the ethics review boards of Peking University Health Science Center. Written informed consent was obtained from the study population. All methods were performed in accordance with relevant guidelines and regulations.
Blood Sampling
At the acute phase of AMI, blood samples were obtained from an antecubital vein without stasis in all patients immediately after admission to the emergency room (ER), and in the morning of the third day (D3) and the seventh day (D7) after AMI (n = 72). In the control subjects, blood samples were obtained from the antecubital vein in the morning of the same day when angiography was performed (n = 30). The blood samples, anticoagulated with ethylenediaminetetraacetic acid (EDTA), were immediately centrifuged at 3000 rpm for 10 min at 4 °C. An aliquot of the EDTA plasma was stored at −80 °C till analysis. Repeated freeze-thaw cycles were avoided.
Assays
Plasma levels of catestatin were measured by enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s instruction (Cat. # EK-053-29, ELISA kit, Phoenix Pharmaceutical Inc., Burlingame, CA). The minimal detection limits for catestatin was 0.06 ng/ml. Serum NT-proBNP levels were measured by a two-site sandwich electrochemiluminescence immunoassay (Elecsys proBNP II, Roche Diagnostic, Mannheim, Germany). These assays were performed by an investigator blinded to the sources of the samples.
Echocardiography Procedure
All patients underwent an echocardiography examination at D3 and 65 months after AMI in our hospital. A VIVID 7 (Vingmed, GE, Horten, Norway) scanner with a 3.3-MHz multiphase array probe was used for the Doppler echocardiography studies, which was conducted under the supervision of experienced cardiologists. The study commenced with each patient lying in the left decubitus position for probe insertion. The echocardiographic techniques were performed and cardiac dimensions and volumes calculated in accordance with the guidelines of the American Society of Echocardiography30. Transmitral pulsed Doppler was recorded in the apical 4-chamber view: early (E) and atrial (A) peak velocities (m/s), peak velocity E/A ratio, and E velocity deceleration time (ms) were obtained. Pulse-wave tissue Doppler imaging was performed using the Doppler tissue imaging function of the instrument. Sample volume was located at the lateral side of the mitral annulus. Early (E’) mitral annulus velocities and the E/E’ ratio were obtained.
Statistics
Outcome measures were left ventricular end-diastolic dimension (LVEDD), ejection fraction (EF), interventricular septal end diastolic dimension (IVS), left ventricular posterior wall thickness (LVPW), E, A, E’, E/A, E/E’, and changes of them from D3 to 65 months (e.g. ΔLVEDD = LVEDD65 months-LVEDDD3). All results are expressed as the mean ± SD. Differences between groups were assessed by Student’s t-test and chi-square test. A Pearson or Spearman correlation was used to explore associations between catestatin levels and parameters. The sensitivity and specificity of catestatin concentration for predicting outcomes were determined, and receiver operating characteristics (ROC) curves were constructed. Univariate and multivariate logistic regression were performed to examine predictors of LV remodeling. p < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Zhu, D. et al. Catestatin-A Novel Predictor of Left Ventricular Remodeling After Acute Myocardial Infarction. Sci. Rep. 7, 44168; doi: 10.1038/srep44168 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Sutton, M. G. S. J. & Sharpe, N. Left ventricular remodeling after myocardial infarction pathophysiology and therapy. Circulation 101, 2981–2988 (2000).
Konstam, M. A., Kramer, D. G., Patel, A. R., Maron, M. S. & Udelson, J. E. Left ventricular remodeling in heart failure: current concepts in clinical significance and assessment. JACC: Cardiovascular Imaging 4, 98–108 (2011).
Pfeffer, M. A. & Braunwald, E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation 81, 1161–1172 (1990).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Journal of the American Society of Echocardiography 22, 107–133 (2009).
Gaudron, P., Eilles, C., Kugler, I. & Ertl, G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation 87, 755–763 (1993).
Jeremy, R. W., Hackworthy, R. A., Bautovich, G., Hutton, B. F. & Harris, P. J. Infarct artery perfusion and changes in left ventricular volume in the month after acute myocardial infarction. Journal of the American College of Cardiology 9, 989–995 (1987).
Omland, T. et al. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction comparison with plasma atrial natriuretic peptide and n-terminal proatrial natriuretic peptide. Circulation 93, 1963–1969 (1996).
Hallén, J., Jensen, J. K., Fagerland, M. W., Jaffe, A. S. & Atar, D. Cardiac troponin I for the prediction of functional recovery and left ventricular remodelling following primary percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 96, 1892–1897 (2010).
Sato, A. et al. Serum tenascin-C might be a novel predictor of left ventricular remodeling and prognosis after acute myocardial infarction. Journal of the American College of Cardiology 47, 2319–2325 (2006).
Mahata, S. K., Mahata, M., Fung, M. M. & O’Connor, D. T. Catestatin: a multifunctional peptide from chromogranin A. Regulatory peptides 162, 33–43 (2010).
Kennedy, B. P., Mahata, S. K., O’Connor, D. T. & Ziegler, M. G. Mechanism of cardiovascular actions of the chromogranin A fragment catestatin in vivo . Peptides 19, 1241–1248 (1998).
Fung, M. M. et al. Direct vasoactive effects of the chromogranin A (CHGA) peptide catestatin in humans in vivo . Clinical and experimental hypertension 32, 278–287 (2010).
Penna, C. et al. Catestatin increases the expression of anti-apoptotic and pro-angiogenetic factors in the post-ischemic hypertrophied heart of SHR. PloS one 9, e102536 (2014).
Perrelli, M.-G. et al. Catestatin reduces myocardial ischaemia/reperfusion injury: involvement of PI3K/Akt, PKCs, mitochondrial KATP channels and ROS signalling. Pflügers Archiv-European Journal of Physiology 465, 1031–1040 (2013).
Zhu, D., Wang, F., Yu, H., Mi, L. & Gao, W. Catestatin is useful in detecting patients with stage B heart failure. Biomarkers 16, 691–697 (2011).
Zhu, D. et al. Correlation of plasma catestatin level and the prognosis of patients with acute myocardial infarction. PloS one 10, e0122993 (2015).
Mazza, R. et al. Catestatin (chromogranin A344-364) is a novel cardiosuppressive agent: inhibition of isoproterenol and endothelin signaling in the frog heart. American Journal of Physiology-Heart and Circulatory Physiology 295, H113–H122 (2008).
Penna, C. et al. Catestatin improves post-ischemic left ventricular function and decreases ischemia/reperfusion injury in heart. Cellular and molecular neurobiology 30, 1171–1179 (2010).
Bassino, E. et al. Catestatin exerts direct protective effects on rat cardiomyocytes undergoing ischemia/reperfusion by stimulating PI3K-Akt-GSK3β pathway and preserving mitochondrial membrane potential. PloS one 10, e0119790 (2015).
Frey, N., Katus, H. A., Olson, E. N. & Hill, J. A. Hypertrophy of the heart a new therapeutic target? Circulation 109, 1580–1589 (2004).
Raman, V. K., Lee, Y.-A. & Lindpaintner, K. The cardiac renin—angiotensin—aldosterone system and hypertensive cardiac hypertrophy. The American journal of cardiology 76, 18D–23D (1995).
Krüger, P.-G., Mahata, S. K. & Helle, K. B. Catestatin (CgA 344–364) stimulates rat mast cell release of histamine in a manner comparable to mastoparan and other cationic charged neuropeptides. Regulatory peptides 114, 29–35 (2003).
Gaede, A. H., Lung, M. S. & Pilowsky, P. M. Catestatin attenuates the effects of intrathecal nicotine and isoproterenol. Brain research 1305, 86–95 (2009).
Rupérez, M. et al. Connective tissue growth factor is a mediator of angiotensin II–induced fibrosis. Circulation 108, 1499–1505 (2003).
Eagleton, M. J. et al. Early increased MT1-MMP expression and late MMP-2 and MMP-9 activity during angiotensin II induced aneurysm formation. Journal of Surgical Research 135, 345–351 (2006).
Souza, H. C. D. d. et al. Nitric oxide synthesis blockade increases hypertrophy and cardiac fibrosis in rats submitted to aerobic training. Arquivos brasileiros de cardiologia 89, 99–104 (2007).
Sorescu, D. & Griendling, K. K. Reactive oxygen species, mitochondria, and NAD (P) H oxidases in the development and progression of heart failure. Congestive Heart Failure 8, 132–140 (2002).
Petersen, C. L., Nielsen, J. R., Petersen, B. L. & Kjær, A. Catecholaminergic activation in acute myocardial infarction: time course and relation to left ventricular performance. Cardiology 100, 23–28 (2003).
Antman, E. M. et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Journal of the American College of Cardiology 44, 671–719 (2004).
Zoghbi, W. et al. American Society of Echocardiography: Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. European Heart Journal-Cardiovascular Imaging 4, 237–261 (2003).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81200167) and the Ph.D. Program Foundation of the Ministry of Education of China (No. 20120001120131).
Author information
Authors and Affiliations
Contributions
D.Z. and W.G. conceived and designed the experiments. D.Z., X.W., Y.L., and H.Y. performed the experiments. H.X. and D.Z. analyzed the data. D.Z. and H.X. contributed reagents/materials/analysis tools. H.X. wrote the paper. X.W. and Y.L. collected the information of patients with STEMI and helped them to know and sign the written informed consent. H.Y. contacted with patients after discharging and collected information in during the follow-up.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhu, D., Xie, H., Wang, X. et al. Catestatin-A Novel Predictor of Left Ventricular Remodeling After Acute Myocardial Infarction. Sci Rep 7, 44168 (2017). https://doi.org/10.1038/srep44168
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep44168
This article is cited by
-
Plasma catestatin levels are related to metabolic parameters in patients with essential hypertension and type 2 diabetes mellitus
Heart and Vessels (2024)
-
Chromogranin A and its derived peptides: potential regulators of cholesterol homeostasis
Cellular and Molecular Life Sciences (2023)
-
Catestatin reverses the hypertrophic effects of norepinephrine in H9c2 cardiac myoblasts by modulating the adrenergic signaling
Molecular and Cellular Biochemistry (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.