Abstract
The aim of this study was to systematically evaluate the cumulative radiation exposure and the associated lifetime-cancer-risk from diagnostic imaging in patients with Hodgkin-lymphoma-(HL) or diffuse-large-B-cell-lymphoma (DLBCL). 99 consecutive patients (53-males) diagnosed with HL or DLBCL were included in the study and followed. Based on the imaging reports, organ and effective-doses-(ED) were calculated individually for each patient and the excess lifetime risks were estimated. The average ED in the first year after diagnosis was significantly different for men (59 ± 33 mSv) and women (744 ± 33 mSv)-(p < 0.05). The mean cumulative ED in each of the following 5 years was 16 ± 16 mSv without significant differences between men and women-(p > 0.05). Over all years, more than 90% of the ED resulted from CT. The average cumulative radiation risk estimated for the first year was significantly lower for men (0.76 ± 0.41%) as compared to women (1.28 ± 0.54%)-(p < 0.05). The same was found for each of the subsequent 5-years (men-0.18 ± 0.17%; women-0.28 ± 0.25%)-(p < 0.05). In conclusion, for HL and DLBCL patients investigated in this study, a cumulative radiation risk of about 1 excess cancer per 100 patients is estimated for diagnostic imaging procedures performed during both the first year after diagnosis and a follow-up period of 5 years.
Similar content being viewed by others
Introduction
Imaging plays a pivotal role for staging, response evaluation, surveillance and prognosis in patients with malignant lymphoma1. Nowadays, computed tomography (CT) and hybrid imaging of 18F-fluorodeoxyglucose positron emission tomography and CT (18F-FDG-PET/CT) are the most widely used imaging procedures in these patients and are recommended by several guidelines1,2,3. However, CT and 18F-FDG-PET/CT lead to an exposure of patients to ionizing radiation associated with a cancer risk. Over the past decades, radiation exposure from medical imaging has significantly increased4,5. CT and nuclear imaging procedures like scintigraphy, single photon emission computed tomography (SPECT) and PET account for around half of the applied diagnostic radiation dose worldwide and for an even higher percentage in first world countries5. However, despite the still growing use of these radiation intense diagnostic procedures the awareness of health professionals regarding carcinogenesis associated with commonly performed imaging procedures is still deficient6. Although radiation exposures and risk from a single procedure is mostly negligible, the cumulative risk from multiple studies in particular in young and middle-aged cancer patients with a favorable prognosis is still a matter of concern7.
Classic Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) account together for around 3% of all cancer cases (excluding non-melanoma skin cancer) in the more developed countries8. Due to considerable therapeutic advances - as for example intensive chemotherapy, stem cell transplantation, targeted therapies and intensity-modulated radiotherapy - cure rates and survival of patients with HL and NHL have significantly improved over the past two decades. These trends impose the requirement to minimize the detriment from diagnosis and treatment in order to prevent the risk for secondary malignancies.
The aim of this study was to evaluate the cumulative radiation exposure and the associated lifetime cancer risk resulting from staging, follow-up and surveillance of patients suffering from HL and diffuse large B-cell NHL (DLBCL).
Materials and Methods
The Medical Ethics Commission II of the Medical Faculty of Mannheim approved the design of this HIPAA compliant study. Due to its retrospective nature, written informed consent was deemed not to be required.
Patient selection and study design
The patient cohort investigated in this study included all patients with an age between 18–55 years diagnosed with HL or DLBCL in our university hospital center between 01/2008 and 12/2011 that underwent at least one X-ray or nuclear medicine examination. All patients were followed-up until 12/2013. All imaging procedures leading to a radiation exposure within two months before the date of diagnosis, as they presumably contributed to the diagnosis of cancer, and two to six years after diagnosis were taken into account. This led to an observation time of between 26 and 62 month, because all patients were observed until the end of 2013 regardless of the date of their diagnosis.
For each of the study participants, the following patient information and examination-specific data for every disease-related X-ray and nuclear medicine procedure were extracted from the hospital and radiology information systems:
Patient-specific data: Identification code, date of birth, sex, date of assignment of the ICD-10 code (HL: C81.0–C81.9; DLBCL: C83.3), tumor histology, tumor stage at diagnosis, date of treatments and, if applicable, death.
Examination-specific data: Date of examination, type of procedure and available dosimetric information:
○ X-ray radiography and fluoroscopy: dose-area product  ,
,
○ CT: volume CT dose index  and dose-length product
and dose-length product  ,
,
○ nuclear medicine: radiopharmaceutical and administered activity 
Estimation of organ and effective doses
For each patient of the cohort (i = 1, …, N) and each type of procedure (P) organ doses  were estimated from the documented dose parameters
were estimated from the documented dose parameters  using tissue- (T) and sex-specific (s) dose coefficients
using tissue- (T) and sex-specific (s) dose coefficients  .
.

where the  was not documented for a radiography, the corresponding national diagnostic reference level was used. Dose coefficients for radiographies were established with the program PCXMC9 using the settings for tube voltage and collimation given in national guidelines10. For CT scans, dose coefficients were determined using the program CT-EXPO (V2.0.1; Hamburg/Hannover, Germany11) from the respective CTDIvol value and the scan length given by the ratio DLP/CTDIvol. For bone, thyroid and renal scintigraphy as well as for 18F-FDG-PET examinations, the dose coefficients provided in ICRP publication 80 were used12. Organ doses for combined 18F-FDG-PET/CT examinations were calculated separately for the CT and the PET part of the examination.
was not documented for a radiography, the corresponding national diagnostic reference level was used. Dose coefficients for radiographies were established with the program PCXMC9 using the settings for tube voltage and collimation given in national guidelines10. For CT scans, dose coefficients were determined using the program CT-EXPO (V2.0.1; Hamburg/Hannover, Germany11) from the respective CTDIvol value and the scan length given by the ratio DLP/CTDIvol. For bone, thyroid and renal scintigraphy as well as for 18F-FDG-PET examinations, the dose coefficients provided in ICRP publication 80 were used12. Organ doses for combined 18F-FDG-PET/CT examinations were calculated separately for the CT and the PET part of the examination.
For each examination, the effective dose E was calculated from the organ doses using a radiation-weighting factor of wR = 1 and the tissue-weighting factors wT given in ICRP publication 10313. Based on the estimated doses per examination, the sum  over the examination-specific organ doses
over the examination-specific organ doses  as well as the corresponding effective dose
as well as the corresponding effective dose  was computed for each patient and each year y = 1, …, 6 after diagnosis.
was computed for each patient and each year y = 1, …, 6 after diagnosis.
Estimation of lifetime attributable risks
For a person i of sex s, exposed at age e to an annual cumulative organ dose  , organ-specific lifetime attributable risk to develop cancer (cancer incidence) in the remaining life
, organ-specific lifetime attributable risk to develop cancer (cancer incidence) in the remaining life  , was estimated using the risk models developed by the BEIR VII committee14 assuming a linear non-threshold (LNT) dose-response relationship. Following the precautionary principle in medical radiation protection, and complying with the recommendation of the German Commission on Radiological Protection15, a dose and dose-rate effectiveness factor
, was estimated using the risk models developed by the BEIR VII committee14 assuming a linear non-threshold (LNT) dose-response relationship. Following the precautionary principle in medical radiation protection, and complying with the recommendation of the German Commission on Radiological Protection15, a dose and dose-rate effectiveness factor  of 1 was applied. Risk estimates were adapted to the German general population. Details of the risk estimation are described in a previous publication16. The total risk
of 1 was applied. Risk estimates were adapted to the German general population. Details of the risk estimation are described in a previous publication16. The total risk  due to imaging procedures in year y was computed for each patient by adding up the organ specific risks
due to imaging procedures in year y was computed for each patient by adding up the organ specific risks  .
.
Data processing and statistical analysis
Analysis of the anonymized patient data was performed in the EXCEL environment (Microsoft Office EXCEL 2010; Microsoft Corporation, Redmond, WA), using the embedded programming language VBA. Statistical tests were done with the program JMP (JMP11; SAS Institute Inc., Cary, NC) at a significance level of p = 0.05.
To determine to what extent the annual organ doses, effective doses and radiation risks differ over the years y = 2–6 after diagnosis, a Kruskal-Wallis ANOVA test on ranks was performed. Since no differences were found over this period of time, non-zero dose and risk estimates were averaged over the years two to six and denoted by  ,
,  , and
, and  .
.
To investigate age differences in the radiation exposure and cancer risk of patients, male and female patients were stratified into two age groups, namely ages 18–35 and 36–55 years. The significance of differences in the exposure and risk estimates between each of two specified patient groups (men vs. women, patiens with HL vs. patients with DLBCL, patients with lower tumor stage vs. patients higher tumor stage, younger vs. older patients) was evaluated by means of the Wilcoxon-Mann-Whitney-test.
Results
The study cohort comprises 99 patients (53 males, 46 females). 55 patients were diagnosed with HL and 44 with DLBCL. Differences in age at diagnosis between males and females were not significant (36.9 ± 10.0 years, range 18 to 55 years vs. 34.0 ± 11.6 years, range 18 to 55 years ). Patients with HL were significantly younger at diagnosis compared to patients with DLBCL (30.1 ± 8.9 years, range 18 to 48 years vs. 42.3 ± 9.1 years, range 18 to 55 years). Figure 1 summarizes the tumor stage according to the Ann-Arbor classification at diagnosis. With the exception of one patient who died before starting treatment, all patients were treated with either chemotherapy alone or combined radio/chemotherapy. Details are summarized in Table 1. In total, eight patients died, two of them suffered from HL, the others from DLBCL. 11 patients experienced a relapse of their disease. As already mentioned, patients in this study were not observed for the same follow-up period. The decrease in the number of patients over the years two to six for unknown reasons, death or end of the observation period (12/2013) is summarized in Fig. 2.
Number, type and distribution of imaging procedures
In the 99 patients of the study cohort, a total of 2399 imaging procedures using ionizing radiation were performed. This corresponds to an average of 24.2 (SD: 13.1, range 1 to 78) examinations per patient, not taking into account the varying follow-up periods. 71.1% of all examinations were CT scans, 23.7% radiographies and 5.2% nuclear medicine procedures. In the first year after diagnosis a mean of 16.0 (SD: 8.1, range 1 to 55) procedures per patient were carried out whereas in each of the following years on average only 3.0 (SD: 3.8, range 0 to 24) examinations were performed per patient. Table 2 provides detailed data on the examinations performed in the first and the subsequent years.
In the first year after diagnosis, the number of all CT and radiographic examinations was slightly higher for women than for men, although not significantly (CT: 11.5 ± 4.4, range 5 to 21 vs. 10.4 ± 5.1, range 0 to 26; radiographies: 4.5 ± 5.6, range 0 to 33 vs. 3.9 ± 3.6, range 0 to 14). A significant difference was found only in the number of thoracic CT examinations, which was higher for women (5.0 ± 2.3, range 2 to 14 vs. 3.6 ± 1.8, range 0 to 10).
Furthermore, the number of CTs and radiographies was significantly lower for patients diagnosed with a lower tumor stage (Ann-Arbor stages 1 and 2) than for patients with a higher tumor stage (Ann-Arbor stages 3 and 4) (CT: 12.6 ± 4.8, range 4 to 23 vs. 10.2 ± 4.4, range 0 to 26; radiographies: 5.6 ± 5.9, range 0 to 33 vs. 2.9 ± 2.9, range 0 to 13) and lower for younger (18–35 years) than for older patients (36–55 years) (CT: 9.9 ± 3.5, range 0 to 17 vs. 11.8 ± 5.5, range 1 to 26; radiographies: 3.1 ± 3.4, range 0 to 14 vs. 5.2 ± 5.3, range 0 to 33). The number of nuclear medicine procedures was significantly higher for patients with Hodgkin lymphoma than for patients with B-Cell Lymphoma (1.0 ± 0.9, range 0 to 4 vs. 0.6 ± 0.7, range 0 to 2).
In the years 2 to 6 after diagnosis no differences in the number of any procedures were found for patients of different sex, age, diagnosis and tumor stage.
The patient with the highest number of examinations was a 38-year-old woman with HL. In this patient, a total of 78 imaging studies (44 CT scans, 33 radiographic examinations, one bone scintigraphy) were performed within a follow-up period of six years, with the majority of examinations (55) performed in the first year. Analysis of the patient record revealed that the high number of examinations was necessary due to poor therapeutic response, an iatrogenic pneumothorax and various other major clinical complications.
National and international guidelines for HL and DLBCL suggest a certain number of imaging procedures in the course of the disease as summarized in Table 3, but do not take into account additional interim examinations performed due to lack of remission or clinical complications. Accordingly, considerable more imaging studies were performed in our patient cohort in particular in the first year after diagnosis than recommended by the German guidelines for initial workup and therapy monitoring (cf. Tables 2 and 3). Compared to the German guidelines, more studies than recommended were performed in the observed patient cohort in the first year. Since this guidelines recommend no diagnostic imaging using ionizing-radiation during the follow-up period at all, all investigations carried-out during this period (Table 2) are considered as additionally.
Organ dose
For both the first and the subsequent years, cumulative organ doses  and
and  did not differ significantly between patients stratified by sex, age, tumor stage and diagnosis (p > 0.05). The cumulative organ dose values
did not differ significantly between patients stratified by sex, age, tumor stage and diagnosis (p > 0.05). The cumulative organ dose values  for the first year and the average annual doses for each of the subsequent years are shown in Fig. 3. The most highly irradiated organs in the first year were the thyroid gland (143 ± 89 mSv, range 0 to 506 mSv), the bladder (86 ± 59 mSv, range 0 to 262 mSv) and the liver (85 ± 46 mSv, range 0 to 251 mSv). In the subsequent years 2–6 the average annual cumulative dose
for the first year and the average annual doses for each of the subsequent years are shown in Fig. 3. The most highly irradiated organs in the first year were the thyroid gland (143 ± 89 mSv, range 0 to 506 mSv), the bladder (86 ± 59 mSv, range 0 to 262 mSv) and the liver (85 ± 46 mSv, range 0 to 251 mSv). In the subsequent years 2–6 the average annual cumulative dose  was highest to the thyroid gland (41 ± 36 mSv, range 0 to 139 mSv), the liver (21 ± 22 mSv, range 0 to 93 mSv) and the remainder tissues (21 ± 18 mSv, range 0 to 71 mSv). Remainder tissues are: adrenals, extrathoracic region, gall bladder, heart, lymphatic nodes, muscle, oral mucosa, pancreas, small intestine, spleen and thymus. For these organs, doses are averaged, as they have a relatively low susceptibility to ionizing radiation.
was highest to the thyroid gland (41 ± 36 mSv, range 0 to 139 mSv), the liver (21 ± 22 mSv, range 0 to 93 mSv) and the remainder tissues (21 ± 18 mSv, range 0 to 71 mSv). Remainder tissues are: adrenals, extrathoracic region, gall bladder, heart, lymphatic nodes, muscle, oral mucosa, pancreas, small intestine, spleen and thymus. For these organs, doses are averaged, as they have a relatively low susceptibility to ionizing radiation.
Effective dose
The average cumulative effective dose  in the first year was significantly different for men (59 ± 33 mSv, range 0 to 153 mSv) and women (74 ± 33 mSv, range 17 to 186 mSv), whereas there were neither significant differences between patients with HL and DLBCL nor between patients in the two considered age groups or between different tumor stages. 92.7% of
in the first year was significantly different for men (59 ± 33 mSv, range 0 to 153 mSv) and women (74 ± 33 mSv, range 17 to 186 mSv), whereas there were neither significant differences between patients with HL and DLBCL nor between patients in the two considered age groups or between different tumor stages. 92.7% of  was caused by CT scans, 6.3% by nuclear medicine examinations and only 1, 0% by radiographies. In the subsequent years 2–6 no significant differences in the average annual effective dose between male and female patients, between diagnoses or tumor stages or between the two considered age groups were observed.
was caused by CT scans, 6.3% by nuclear medicine examinations and only 1, 0% by radiographies. In the subsequent years 2–6 no significant differences in the average annual effective dose between male and female patients, between diagnoses or tumor stages or between the two considered age groups were observed.
The mean cumulative effective dose per year  was 16 ± 16 mSv, range 0 to 71 mSv. Here, the relative contribution of CT scans was 97.5%. Nuclear medicine procedures and radiographies accounted for 1.7% and 0.8%, respectively. Figures 4A,B show the distribution of the annual effective dose in the first and the subsequent years stratified by sex and age group.
was 16 ± 16 mSv, range 0 to 71 mSv. Here, the relative contribution of CT scans was 97.5%. Nuclear medicine procedures and radiographies accounted for 1.7% and 0.8%, respectively. Figures 4A,B show the distribution of the annual effective dose in the first and the subsequent years stratified by sex and age group.
(A,B) Estimated average effective doses cumulated over one year in (A) the first year after diagnosis and (B) each of the following years stratified by sex and age. The horizontal line within the box represents the median value, the ends of the box the 75th and 25th percentiles. The whiskers extend from the ends of the box to the outer-most data point within the following distances: Upper Fence = upper quartile +1.5 × interquartile range, Lower Fence =lower quartile −1.5 × interquartile range, The dots represent outliers i.e. values outside this range. The confidence diamond within the box gives the mean and the upper and lower 95% confidence limits of the mean value.
The highest effective dose in the first year (186 mSv) was estimated for the above-mentioned 38-year-old female patient undergoing the highest number of examinations. She also received the highest overall cumulative effective dose (426 mSv) for the entire period of observation, in her case six years.
Lifetime attributable cancer risks
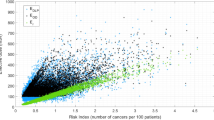
The radiation risks estimated for imaging procedures performed during the first year after diagnosis  were significantly different for men and women (0.76 ± 0.41%, range 0.0 to 1.77% vs. 1.28 ± 0.54%, range 0.18 to 2.63%) as well as for younger and older patients (18–35 years, 1.18 ± 0.55%, range 0.0 to 2,56% vs. 36–55 years, 0.85 ± 0.49%, range 0.05 to 2.63%). Estimated
were significantly different for men and women (0.76 ± 0.41%, range 0.0 to 1.77% vs. 1.28 ± 0.54%, range 0.18 to 2.63%) as well as for younger and older patients (18–35 years, 1.18 ± 0.55%, range 0.0 to 2,56% vs. 36–55 years, 0.85 ± 0.49%, range 0.05 to 2.63%). Estimated  values are summarized in Fig. 5A,B, stratified by sex and age. Between patients with DLBCL and HL there were significant differences (0.85 ± 0.56%, range 0.0 to 2.56% vs. 1.13 ± 0.49%, range 0.2 to 2.62%), primarily due to differences in the age at diagnosis between the two groups. There were no differences between tumor stages. The radiation risks associated with imaging procedures performed on average per year in the subsequent years
values are summarized in Fig. 5A,B, stratified by sex and age. Between patients with DLBCL and HL there were significant differences (0.85 ± 0.56%, range 0.0 to 2.56% vs. 1.13 ± 0.49%, range 0.2 to 2.62%), primarily due to differences in the age at diagnosis between the two groups. There were no differences between tumor stages. The radiation risks associated with imaging procedures performed on average per year in the subsequent years  are also summarized in Fig. 5A,B. Significant differences were found between men (0.18 ± 0.17%, range 0 to 0.70%) and women (0.28 ± 0.25%, range 0 to 1.01%).
are also summarized in Fig. 5A,B. Significant differences were found between men (0.18 ± 0.17%, range 0 to 0.70%) and women (0.28 ± 0.25%, range 0 to 1.01%).
(A,B) Sex- and age-specific distribution of the average lifetime attributable risk of cancer incidence cumulated over on year in (A) the first year after diagnosis and (B) each of the following years. For details of presentation see Fig. 4.
cumulated over on year in (A) the first year after diagnosis and (B) each of the following years. For details of presentation see Fig. 4.
In men, colon, bladder and lungs accounted each for more than 10% to the annual radiation risks  and
and  . In women, breast, bladder and lungs each contributed more than 10% to the mentioned risk estimates. For both male and female patients, in the first as well as in the following years, the largest proportion of the annual radiation risk originates from radiation exposure of the remainder tissues (24.5% and 26.2%, respectively).
. In women, breast, bladder and lungs each contributed more than 10% to the mentioned risk estimates. For both male and female patients, in the first as well as in the following years, the largest proportion of the annual radiation risk originates from radiation exposure of the remainder tissues (24.5% and 26.2%, respectively).
The patient with the highest overall  (summed over six years after diagnosis) was once again the 38-year-old female patient with HL who already had the most procedures and the highest cumulative effective dose. Her lifetime attributable risk of cancer incidence due to all procedures performed in the six years was estimated at 5.8%.
(summed over six years after diagnosis) was once again the 38-year-old female patient with HL who already had the most procedures and the highest cumulative effective dose. Her lifetime attributable risk of cancer incidence due to all procedures performed in the six years was estimated at 5.8%.
Discussion
The presented retrospective patient study provides a detailed analysis of the individual cumulative radiation exposure and associated cancer risk resulting from diagnostic imaging procedures using ionizing radiation carried-out in patients with HL or DLBCL over a long oberservation period of up to 6 years. In contrast to a previous study that solely investigated the cumulative effective dose of CT and 18F-FDG-PET/CT examinations in patients with lymphoma over an average surveillance period of 8 months, the long observation period of our studies makes it possible to consider the entire follow-up period currently recommended by several guidelines (cf. Table 3)17.
The second advantage of our study design is that we included all diagnostic examinations using ionizing radiation over the whole observation period. Hereby, our results clearly demonstrate that patients undergo considerably more examinations when compared to recent guidelines (cf. Tables 2 and 3). Every procedure that was done exceeding these suggested numbers was considered as additional and due to complications. This was 40.3% of procedures in the first year and 100% of procedures in the following years, as german guidelines don’t recommend imaging using ionizing radiation in the follow-up period. This has to be accounted for when comparing the results with other studies. In contrast to guidelines that do not consider clinical complications, like atypical pneumonia that frequently occur during therapy and often lead to several thoracic CT examinations, our results provide a realistic scenario without any bias concerning the number, type and radiation dose of examinations clinically performed in patients with HL and DLBCL. Therefore, the cumulative effective doses estimated for the patients of our study cohort were markedly higher compared to those in a recently published study that used a Monte Carlo simulation to investigate radiation exposure and risk of adult patients with NHL associated with the imaging protocol of the HOVON 84 international multicenter trial7.
We deliberately considered only patients with HL or DLBCL with an age between 18–55 years to address the higher radiation risk of young and middle-aged patients. Moreover, elderly patients with both HL or DLBCL have also a considerably reduced disease-related overall survival rate when compared to young and middle-aged patients and thus a considerably decreased likelihood to develop a clinically manifest secondary cancer18. Within this context, it is important to consider that the minimum latency period to develop a secondary cancer, i.e. the period of time between radiation exposure and clinical manifestation of a secondary cancer, is assumed to be two to five years for leukemia and five to ten years for solid tumors.
In the patient cohort investigated in the present study, CT contributed to 93% of the cumulative effective dose within the first year after diagnosis and on average for 98% in each of the following years. Based on the Lugano Classification, 18F-FDG-PET/CT is nowadays considered as the first-line imaging modality for the initial staging as well as follow-up of patients with FDG-avid lymphomas whereas CT is recommended for all non FDG-avid lymphomas. A more widely use of hybrid 18F-FDG-PET/CT instead of CT alone as in our study will lead to an even higher radiation exposure in patients with FDG-avid lymphomas since the Lugano Classification recommends that hybrid imaging shall include a fully diagnostic contrast-enhanced CT.
Women in our patient cohort showed a significantly higher cumulative  when compared to men in the first year after diagnosis. Since CT was the main source of ionizing radiation in this study, the higher
when compared to men in the first year after diagnosis. Since CT was the main source of ionizing radiation in this study, the higher  in women is most likely explained by a limited adaption of the individual CT scan protocol to the individual body size. Within this context, it is important to consider that over the last years several novel techniques for radiation dose reduction in CT - that were mainly not clinically available during our observation period - have been clinically implemented. Those techniques include more efficient X-ray detectors, iterative reconstruction techniques as well as automated tube current modulation and tube voltage selection based on the individual anatomy of the patient19,20. As one example out of many, a recently published study by Meyer et al. demonstrated that iterative reconstruction techniques allow for a 50% radiation dose reduction in whole-body staging examinations of patients with lymphoma20.
in women is most likely explained by a limited adaption of the individual CT scan protocol to the individual body size. Within this context, it is important to consider that over the last years several novel techniques for radiation dose reduction in CT - that were mainly not clinically available during our observation period - have been clinically implemented. Those techniques include more efficient X-ray detectors, iterative reconstruction techniques as well as automated tube current modulation and tube voltage selection based on the individual anatomy of the patient19,20. As one example out of many, a recently published study by Meyer et al. demonstrated that iterative reconstruction techniques allow for a 50% radiation dose reduction in whole-body staging examinations of patients with lymphoma20.
The interpretation of the cumulative effective dose estimated in this study has to consider that the effective dose characterizes the generic radiation risk of patients because neither the sex nor the age of the patients is considered and is thus not suitable for risk assessment of individual patients. Therefore, the ICRP stated that the effective dose should neither be used for epidemiological evaluations nor for detailed retrospective investigations of individual exposure and risks13. The effective dose was determined to be comparable to previous studies. The individual lifetime attributable risk  estimates computed in this study by using most recent organ-, sex- and age-dependent risk models yield a significantly higher cancer risk for women as compared to men. The higher risk in women can be explained by the higher radiation exposure estimated for women as compared to men as well as their higher risk coefficients for many organs and tissues, especially for breasts and lungs. The average
estimates computed in this study by using most recent organ-, sex- and age-dependent risk models yield a significantly higher cancer risk for women as compared to men. The higher risk in women can be explained by the higher radiation exposure estimated for women as compared to men as well as their higher risk coefficients for many organs and tissues, especially for breasts and lungs. The average  for men and women associated to the diagnostic imaging procedures considered in the present study corresponds to about 1 excess cancer in 100 lymphoma patients from diagnostic imaging performed in the first year after diagnosis (mean
for men and women associated to the diagnostic imaging procedures considered in the present study corresponds to about 1 excess cancer in 100 lymphoma patients from diagnostic imaging performed in the first year after diagnosis (mean  ≈ 1%), and to an additional excess cancer case for imaging procedures carried-out during a follow-up period of 5 years (
≈ 1%), and to an additional excess cancer case for imaging procedures carried-out during a follow-up period of 5 years ( ≈ 0.23% per year). Compared to the lifetime baseline cancer risk (incidence excluding non-melanoma skin cancer) of a 35-year old man or woman in Germany of about 50 and 40%, respectively21, the average imaging related additional cancer risk estimated for the HL and DLBCL patients in the present study is relatively small, but not negligible mainly due to the low age of HL (mean, 30 years) and DLBCL patients (42 years) in our study cohort. It has to be noted that the reported risk estimates overestimate the real risks to some extent since they were derived using life table data for the entire german population and not data specific for lymphoma patients with a reduced life expectancy. For individual patients, the radiation risk from diagnostic imaging procedures can be considerably high. The highest risk of nearly 6% was estimated in case of the 38-year old female patient with HL undergoing a high number of CT scans due to clinical complications.
≈ 0.23% per year). Compared to the lifetime baseline cancer risk (incidence excluding non-melanoma skin cancer) of a 35-year old man or woman in Germany of about 50 and 40%, respectively21, the average imaging related additional cancer risk estimated for the HL and DLBCL patients in the present study is relatively small, but not negligible mainly due to the low age of HL (mean, 30 years) and DLBCL patients (42 years) in our study cohort. It has to be noted that the reported risk estimates overestimate the real risks to some extent since they were derived using life table data for the entire german population and not data specific for lymphoma patients with a reduced life expectancy. For individual patients, the radiation risk from diagnostic imaging procedures can be considerably high. The highest risk of nearly 6% was estimated in case of the 38-year old female patient with HL undergoing a high number of CT scans due to clinical complications.
The estimated radiation risk of about 1% associated with diagnostic imaging procedures carried-out during a follow-up period of 5 years should be considered within the recent debate on the effectiveness of current imaging strategies to detect relapse in patients with lymphoma. One study that compared 18F-FDG-PET/CT against a combination of ultrasonography (US) and chest radiography for systematic follow-up of patients with high-risk HL found 97.5% of relapses using only US and chest radiography22. The estimated radiation dose in this study for a routine 18F-FDG-PET/CT follow-up examination was 14.5 mSv vs. 0.1 mSv for a chest radiography that was combined with US for follow-up. Thus, the authors concluded that US and chest radiography enable effective, safe, low-cost and especially low-risk routine surveillance imaging for patients at high risk of HL relapse22. Another recent study even suggested that routine, scheduled imaging might not be needed for follow-up of DLBCL, because the majority of relapses is detected outside of the planned follow-up examinations23. In this study, patient outcome did not differ between patients in which relapse was detected in routine follow-up examinations and patients with relapse outside of routine follow-up examinations23.
The present study has some potential limitations that need to be considered. First, our results are only representative for our university hospital in which mainly CT was used for staging and follow-up although 18F-FDG-PET/CT is nowadays recommended as the imaging gold-standard in case of patients with FDG-avid lymphomas. However, as already mentioned, radiation dose from hybrid 18F-FDG-PET/CT imaging comprising a fully diagnostic contrast-enhanced CT scan will lead to an even higher radiation dose when compared to CT alone. Second, this study includes solely data from the clinical and radiology information system of our university hospital center. Although most patients with HL and DLBCL receive their follow-up examinations at our institution, some patients may have received additional examinations outside of it. This may lead to a slight underestimation of the dose and risk estimates. Third, the results of this study are only representative for patients with HL and DLBCL with an age between 18–55 years. These patients were selected since their cure rate are generally good so that the risk to establish a clinically manifest secondary malignancy plays a pivotal role. The estimated radiation risks may thus not be directly transferable to elderly patients with aggressive types of lymphoma although imaging algorithms may not be different between patients with different types of lymphoma. Fourth, estimates of stochastic radiation risks are derived based on the LNT response model. Since experimental and radio-epidemiological studies do not provide conclusive evidence for the carcinogenicity of low levels of radiation (<about 50 mGy), there is a considerable controversy on the validity of the LNT model in the low-dose range24,25. Even for doses between 50 and 200 mSv, determined for the majority of the HL and DLBCL patients of our study cohort, the scientific evidence for carcinogenic radiation effects is still somewhat fuzzy24. Nevertheless, estimation of stochastic radiation risks associated with ionizing radiation by means of the LNT model is the most prudent and precautionary approach for radiation protection of patients26. All radiation risk estimates are, unquestionably, associated with uncertainties, as discussed in detail in the BEIR VII report14. In view of that, the report gives “subjective confidence intervals”. Referring to this concept, a 95% uncertainty range of a factor of 2 can be assumed for the LAR estimates given in this paper (95% CI = [0.5 * LAR; 2 * LAR]).
In conclusion, for the HL and DLBCL patients considered in the present study, a cumulative radiation risk of about 1 excess cancer per 100 patients is estimated for diagnostic imaging procedures performed during both the first year after diagnosis and a follow-up period of 5 years. Since CT is mainly responsible for the observed radiation exposure, novel CT techniques that enable significant dose reduction should be strictly implemented for imaging of patients with HL and DLBCL. Moreover, based on the results of novel studies that found most lymphoma relapses outside from routine follow-up examinations as well as a high accuracy and safety of US and chest radiography for the follow-up of patients with lymphoma, the overall usefulness of routinely performed follow-up CT or 18F-FDG-PET/CT examinations should be reevaluated in future guidelines.
Additional Information
How to cite this article: Fabritius, G. et al. Cumulative radiation exposure from imaging procedures and associated lifetime cancer risk for patients with lymphoma. Sci. Rep. 6, 35181; doi: 10.1038/srep35181 (2016).
Change history
03 May 2017
Scientific Reports 6: Article number: 35181; published online: 17 October 2016; updated: 03 May 2017. The original version of this Article contained a typographical error in the Abstract. “The average ED in the first year after diagnosis was significantly different for men (59 ± 33 mSv) and women (744 ± 33 mSv)-(p < 0.
References
Cheson, B. D. et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 32, 3059–3068 (2014).
Michael Fuchs, A. E. & Richard Greil, Ralph Naumann. Guidelines: Hodgkin lymphoma.
Ulrich Dührsen, M. A. F., Norbert Schmitz. Guidelines: Diffuse large B-cell lymphoma.
Amis, E. S. Jr. et al. American College of Radiology white paper on radiation dose in medicine. Journal of the American College of Radiology: JACR 4, 272–284 (2007).
United Nations Scientific Committee on the Effects of Atomic Radiation, U.N.S.C.o.t.E.o.A. Sources and effects of ionizing radiation - UNSCEAR 2008 . (United Nations, New York, 2010).
Puri, S. et al. Physicians’ and midlevel providers’ awareness of lifetime radiation-attributable cancer risk associated with commonly performed CT studies: relationship to practice behavior. AJR. American journal of roentgenology 199, 1328–1336 (2012).
Nievelstein, R. A. et al. Radiation exposure and mortality risk from CT and PET imaging of patients with malignant lymphoma. European radiology 22, 1946–1954 (2012).
Ferlay, J. et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International journal of cancer. Journal international du cancer 136, E359–E386 (2015).
Tapiovaara M. S.T. PCXMC-A. Monte Carlo program for calculating patient doses in medical X-ray examinations . vol. 2nd ed (STUK – Radiation and Nuclear Safety Authority, Laippatie 4, 00880 Helsinki, Finland, 2008).
Stender, H. St. Guidelines of the Bundesärztekammer for quality assurance in radiography. Dtsch Arztebl International 92, 2272–2285 (1995).
Stamm, G. & Nagel, H. D. CT-Expo - a Novel Program for Dose Evaluation in CT. Fortschr Röntgenstr 174, 1570–1576 (2002).
International Commission on Radiological Protection Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Annals of the ICRP 28, 1–126 (1998).
The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Annals of the ICRP 37, 1–332 (2007).
Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. National research council. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2 (The National Academies Press, Washington, 2006).
Strahlenschutzkommission, S. Dose and dose-rate effectiveness factor (DDREF). Recommendation by German Commission on Radiological Protection with scientific grounds (2014).
Brix, G. et al. Cumulative radiation exposure and cancer risk of patients with ischemic heart diseases from diagnostic and therapeutic imaging procedures. European journal of radiology 82, 1926–1932 (2013).
Ackerman, K. G. & Pober, B. R. Congenital diaphragmatic hernia and pulmonary hypoplasia: new insights from developmental biology and genetics. Am J Med Genet C Semin Med Genet 145C, 105–108 (2007).
Stamatoullas, A. et al. Outcome of patients older than 60 years with classical Hodgkin lymphoma treated with front line ABVD chemotherapy: frequent pulmonary events suggest limiting the use of bleomycin in the elderly. British journal of haematology 170, 179–184 (2015).
Mayer, C. et al. Potential for radiation dose savings in abdominal and chest CT using automatic tube voltage selection in combination with automatic tube current modulation. AJR. American journal of roentgenology 203, 292–299 (2014).
Meyer, M. et al. Whole-body CT for lymphoma staging: feasibility of halving radiation dose and risk by iterative image reconstruction. European journal of radiology 83, 315–321 (2014).
Robert Koch Institute and the Association of Population-based Cancer Registries in Germany, A.o.P.-B.C.R.i. Cancer in Germany 2009/2010 (2013).
Picardi, M. et al. Advanced-stage Hodgkin lymphoma: US/chest radiography for detection of relapse in patients in first complete remission–a randomized trial of routine surveillance imaging procedures. Radiology 272, 262–274 (2014).
Thompson, C. A. et al. Utility of routine post-therapy surveillance imaging in diffuse large B-cell lymphoma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 32, 3506–3512 (2014).
Shore, R. E. Radiation impacts on human health: certain, fuzzy, and unknown. Health physics 106, 196–205 (2014).
Shah, D. J., Sachs, R. K. & Wilson, D. J. Radiation-induced cancer: a modern view. The British journal of radiology 85, e1166–e1173 (2012).
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR), U.N.S.C.o.t.E.o.A.R. Biological mechanisms of radiation actions at low doses: A white paper to guide the Scientific Committee’s future programme of work. United Nations Publication V. 12-57831 (2012).
National comprehensive cancer network, R.T.H. NCCN Guidelines: Hodgkin lymphoma.
National comprehensive cancer network, A.D.Z. NCCN Guidelines: Non-Hodgkin lymphoma.
Eichenauer, D. A., Engert, A., Dreyling, M. & Group, E. G. W. Hodgkin’s lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 22 Suppl 6, vi55–vi58 (2011).
Tilly, H. et al. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology 26, v116–v125 (2015).
Acknowledgements
This research project is part of the Research Campus M2OLIE and funded by the German Federal Ministry of Education and Research (BMBF) within the Framework “Forschungscampus: public-private partnership for Innovations” under the funding code 13GW00926.
Author information
Authors and Affiliations
Contributions
Study design, measurements and statistical analysis: T.H., G.F., G.B. and E.N. Contributed to the writing of the manuscript: T.H., G.F., G.B., S.O.S., W.K.H., S.K., M.M., C.H., E.N., H.D.P., M.M. and G.G.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Fabritius, G., Brix, G., Nekolla, E. et al. Cumulative radiation exposure from imaging procedures and associated lifetime cancer risk for patients with lymphoma. Sci Rep 6, 35181 (2016). https://doi.org/10.1038/srep35181
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35181
This article is cited by
-
A Cross-Sectional Analysis of the Lung Cancer Screening Eligibility Among Cancer Survivors Who Ever Smoked
Journal of General Internal Medicine (2024)
-
Diagnostic performance of prospective same-day 18F-FDG PET/MRI and 18F-FDG PET/CT in the staging and response assessment of lymphoma
Cancer Imaging (2023)
-
Low-dose coronary calcium scoring tarnishes power of zero
Journal of Nuclear Cardiology (2023)
-
PET/MRI for staging patients with Hodgkin lymphoma: equivalent results with PET/CT in a prospective trial
Annals of Hematology (2021)
-
Reduction of operator radiation exposure using a passive robotic device during fluoroscopy-guided arterial puncture: an experimental study in a swine model
European Radiology Experimental (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.