Abstract
The purpose of the current study was to investigate the effect of topical atropine on choroidal thickness using spectral-domain optical coherence tomography. A total of 30 healthy eyes from 30 children were analyzed in this study. A single drop of 1% atropine gel was administered twice daily for a week. Choroidal thickness (CT) was measured using SD-OCT, and changes in CT before and after administration of the eye drops were analyzed at the subfovea and at 1.0-mm intervals (up to 3.0 mm) from the fovea at superior, inferior, nasal, and temporal locations. Pre- and post-cycloplegic axial length (AL) was also measured using the IOLMaster. We observed that administration of 1% atropine gel led to a significant increase in the choroidal thickness under the fovea and at all intervals from the fovea. The greatest change in CT was observed in the inferior meridian, while the nasal meridian exhibited the least change. AL did not significantly differ before and after cycloplegia, and there was no significant correlation between the changes in AL and subfoveal CT. It was concluded that administration of 1% atropine gel can significantly increase CT in the eyes of young Chinese children, albeit with different magnitude at different locations.
Similar content being viewed by others
Introduction
The ocular choroid is an extensively vascularized tissue situated between the sclera and Bruch’s membrane. The major role of the choroid is to supply oxygen and nutrients to the outer retina1. Evidence from animal studies have reported that the choroid can rapidly change its thickness in response to a variety of stimuli such as myopic or hyperopic defocus in order to move the retina towards the plane of focus.
In addition, previous studies have revealed that there is a rich autonomic vasoactive nerve supply to the choroid that involves the activation of adrenergic and muscarinic receptors2. Therefore, it is reasonable to speculate that topical adrenergic and anticholinergic agents could exert an effect on the choroid. A number of animal studies have shown that non-selective, partially selective or highly selective muscarinic antagonists (i.e., atropine, pirenzepine, himbaicine, MT3, MT7) can significantly influence choroidal thickness and ocular growth changes3,4,5.
In humans, there are some reports that highlight the effect of topical anticholinergic or adrenergic agents on choroidal thickness with varied or even contradictory findings. For example, some studies have reported absence of any influence of these agents on the choroidal thickness6,7,8, while some authors have observed an increase9 or a decrease10,11 in the choroidal thickness, even when the same drugs were used (Table 1). We speculate that such discrepancies might arise from the differences in the methods of drug instillation, race of participants, and distribution rate of mydriatic agents to the posterior.
Atropine now is considered as a most potent drug to control the progression of myopia in children, with strong supporting evidence from well-conducted clinical trials12,13. However, the exact site and mechanism of action of atropine in slowing myopia progression is still insufficiently understood14,15. In a longitudinal study, Read and associates16 reported that a significant increase in subfoveal choroidal thickness of myopic and nonmyopic children was observed over 18-month follow-up, and children showing faster axial eye growth exhibited significantly less choroidal thickening over time compared with children showing slower axial eye growth. The results suggested that there may be a potential role for the thicker choroid in the mechanisms inhibiting eye growth in childhood. In this respect, if the choroid of children is thickened by drugs (i.e. atropine), which might be a part of mechanism to slow the progression of myopia.
By far, however, there is no published evidence of the effect of topical atropine administration on the choroidal thickness of children in vivo measured by SD-OCT equipments. Therefore, in the present study, we wanted to explore the effect of a long acting anticholinergic drug i.e. atropine (1%) on the choroidal thickness in Chinese children within the age group of 5 to 10 years.
Results
In the present study we examined 30 healthy eyes of 30 subjects (including 14 boys) satisfying the inclusion criteria. The subjects were in the age group 5-10 years with a mean age of 7.47 ± 1.16 years. The mean spherical equivalent after 1-week of cycloplegia was -0.38 ± 2.16 D (from −3.50 D to +4.63 D).
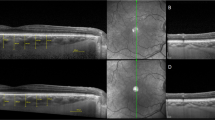
Choroidal thickness measured at the fovea and at 1.0-mm intervals (up to 3.0 mm) from the fovea at nasal, temporal, superior, and inferior locations for both groups are summarized in Table 2. Following administration of 1% atropine gel, choroid thickened significantly under the fovea (i.e. from 287.03 ± 65.76 μm to 302.52 ± 69.94 μm, P < 0.001) and at all intervals from the fovea. However, the magnitude of change in choroidal thickness varied with the location. The greatest change in choroidal thickness was observed in the inferior meridian (20.44 ± 30.21 μm, the average change of the three measurement locations in the inferior meridian, the same below), while the nasal meridian exhibited the least change (11.19 ± 15.54 μm) (P = 0.007, Fig. 1). In addition, the change of choroidal thickness in the temporal meridian (19.52 ± 24.06 μm) significantly thickened than that of in the nasal meridian (P = 0.016), and the change of choroidal thickness in the inferior meridian slightly but significantly thickened than that of in the superior meridian (13.66 ± 21.71 μm) (P = 0.048).
The changes of choroidal thickness before and after 1-week administration of 1% atropine gel.
(A) T3, 3 mm temporal to the fovea; T2, 2 mm temporal to the fovea; T1, 1 mm temporal to the fovea; SF, subfovea; N3, 3 mm nasal to the fovea; N2, 2 mm nasal to the fovea; N1, 1 mm nasal to the fovea. (B) S3, 3 mm superior to the fovea; S2, 2 mm superior to the fovea; S1, 1 mm superior to the fovea; SF, subfovea; I3, 3 mm inferior to the fovea; I2, 2 mm inferior to the fovea; I1, 1 mm inferior to the fovea.
Axial length did not differ significantly before (23.40 ± 0.98 mm) and after (23.39 ± 0.98 mm) cycloplegia with a mean difference of −8.33 ± 46.32 μm (P = 0.333). Plus, there was no significant correlation between the changes in axial length and subfoveal choroidal thickness (r = −0.186, P = 0.324).
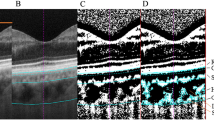
There was excellent agreement between the two independent observers, with an ICC of 0.952 and 0.955 before and after cycloplegia, respectively (Table 3). Bland-Altman plot of difference against mean choroidal thickness showed no significant change in variability for the range of choroidal thickness, and a very few observations were outside 95% limits of agreement (LOA) both before and after cycloplegia (Fig. 2). Specifically, the Bland-Altman analysis indicated that the 95% LOA between the two observers ranged from −43.09 μm to 48.31 μm (mean, 2.61 μm) and −38.11 μm to 41.71 μm (mean, 1.47 μm) for chorodial thickness of all locations of measurements before and after cycloplegia, respectively (Table 3). Plus, the inter-observer repeatability coefficients were 46.58 μm (95% confidence interval: 45.55 μm to 47.32 μm) and 40.96 μm (95% confidence interval: 39.58 μm to 41.14 μm) for chorodial thickness of all locations of measurements before and after cycloplegia, respectively (Table 3).
Bland-Altman plot analyses.
Bland-Altman plot of interobservers agreement on choroidal thickness measurements for all locations between the two observers before (A) and after 1-week administration of 1% atropine gel (B). Solid line indicates the average mean difference, whereas dotted lines delineate 95% limits of agreement (1.96 *SD). There was no specific trend to cause the difference between the two observers.
Discussion
Similar to the iris, which is also a part of the uvea, the choroid may also likely display certain changes following the use of a mydriatic agent. In the present study, we found that the use of topical 1% atropine gel administration for a week significantly increased the choroidal thickness under the fovea and at all parafoveal locations. Our findings are consistent with the results of Sander et al., wherein 2% homatropine hydrobromide was used9. Notably, we did not observe a statistically significant change in the axial length (−8.33 ± 46.32 μm) despite significant subfoveal choroidal thickness (15.48 ± 16.13 μm) as a result of atropine-induced cycloplegia. Plus, we did not discover a significant relationship between the changes in subfoveal choroidal thickness and axial length, suggesting that choroidal thickening could not significantly influence the axial length obtained by IOLMaster. We speculated that the lack of correlation between the change of axial length and subfoveal choroidal thickness may be attributed to the relatively poor resolution of IOLMaster (10 μm) when compared with SD-OCT (5 μm). It was noteworthy that the range of standard deviation of the change of the axial length was relatively wide.
In the present study, although choroidal thickness thickened significantly at all the measured locations, the magnitude of change was not identical. Maximal change in choroidal thickness was observed in the inferior meridian (20.44 ± 30.21 μm), while the location 3.0 mm nasal to the fovea exhibited the least change (4.17 ± 10.49 μm) in choroidal thickness which may be attributed to the limited space around the optic head (Fig. 1; Table 2). As the inferior conjunctival sac was in contact with the drug for the maximum time, it seems likely that the inferior part of the choroid received the highest drug concentration, thereby having the strongest effect on the choroid.
Atropine is a nonselective antagonist of the muscarinic acetylcholine receptor types M1, M2, M3, M4, and M5. Topical atropine is used as a cycloplegic, to temporarily paralyze the accommodation reflex, and also as a mydriatic agent, to dilate the pupils. There has been a relatively long time since atropine was used as an anti-myopia drug. In 1989, Yen et al.17 conducted the first randomized control trial on the use of atropine in childhood myopia, confirming that 1% atropine was effective in slowing the progression of myopia, and the effect of 1% atropine was better than that of 1% cyclopentolate. The latest study reported that 0.01% atropine now is the preferred option for controlling myopia progression than any other concentrations when considering side effects13. Unfortunately, the exact mechanism of atropine in slowing progression are still not known14,15. In the present study, the choroidal thickness at all measured locations significantly thickened after 1-week administration of 1% atropine gel, which may be a part of mechanism of preventing myopia progression in the use of atropine. Read and associates16 reported that children showing faster axial eye growth exhibited significantly less choroidal thickening over time compared with children showing slower axial eye growth. Besides, in an experimental study, Nickla and associates18 found that choroidal thickness could predict ocular growth rates in normal chick eyes: eyes with thinner choroids grew faster than those with thicker choroids. The aforementioned results further supported that there may be a potential role for the thicker choroid in the mechanisms inhibiting eye growth in childhood.
Atropine induces cycloplegia by paralyzing the ciliary muscles, whose action inhibits accommodation to allow accurate refraction in children. In China, children who are less than 10 years old are usually administered 1% atropine gel twice daily for a week or thrice daily for 3 successive days before refraction to reach cycloplegia. Compared to tropicamide (a shorter-acting cholinergic antagonist) or phenylephrine (an α-adrenergic agonist), 1% atropine gel when used twice daily for a week may be potent enough to reach and affect the choroid.
The exact mechanism underlying increased choroidal thickness following administration of topical 1% atropine, though elusive, could still be surmised from the findings of previous studies. Firstly, cycloplegia induced by atropine may be a very important factor that can increase the choroidal thickness, as some previous studies highlight an inverse relationship between accommodation and choroidal thickness19,20. It is well known that accommodation is highly efficient in children less than 10 years of age. During accommodation the force involved in the contraction of the ciliary muscle may be transmitted to the choroid, and this mechanical force can affect the choroidal thickness. Woodman et al.19 were first to observe a small amount of choroidal thinning during the accommodation task using Spectralis OCT. They postulated that the regional variation in the parafoveal thickness corresponds to the distribution of the nonvascular smooth muscle (NVSM) cells within the choroid indicating that these cells may regulate choroidal thickness during accommodation20. Chiang and associates21 found that subfoveal choroidal thickness significantly increased within 10 min of exposure to 2.00 D of monocular myopic defocus (reducing accommodation). Interestingly, Li et al.22 reported that accommodation decreased early after myopic refractive surgery with a concomitant increase in choroidal thickness, and the decrease in the amplitude of accommodation was the most significant factor associated with the increase of choroidal thickness at the fovea. Thus, in line with previous reports, blockade of accommodation by atropine may be an important mechanism underlying changes in choroidal thickness.
Secondly, antagonism of muscarinic receptors may be another possible factor affecting choroidal thickness. Alterations in the tone of nonvascular smooth muscle have been suggested to cause choroidal thickening after administration of antimuscarinic drugs in animals1. There is a rich autonomic vasoactive never supply to the choroid involving the activation of adrenergic and muscarinic receptors2. A previous study has found that electrical stimulation of the post-ganglionic axons (action of the parasympathetic innervation) from the chick ciliary ganglion leads to contraction of explant choroids, and this contraction can be blocked by atropine, showing that acetylcholine may affect contraction of at least some choroidal smooth muscle23. In addition, Nickla et al.24 have found that the choroid thickened significantly after double parasympathectomy in 4–5-week-old chicks. In another study by Nickla and associates25, it was observed that atropine inhibited the development of myopia in negative lens-wearing eyes, and also caused choroidal thickening in young chicks. It was proposed that the choroidal thickening reflected the loss of an excitatory input, probably cholinergic, to the choroidal nonvascular smooth muscle23, which may normally restrain thickening in opposition to osmotic forces that swell the lacunae26 and thicken the choroid1.
Given that the choroid contains abundant nonvascular smooth muscle, the contraction of these muscles might squeeze fluid out of the choroid, thereby thinning it and the contraction of nonvascular smooth muscle may be induced by acetylcholine25. However, because the nonvascular smooth muscle is not aligned perpendicular to the plane of the choroid, it is also possible that contraction of these muscles facilitates filling of the lacunae. Therefore, the contribution of nonvascular smooth muscle to the change in choroidal thickness is still speculative and needs further investigation.
Thirdly, considering the common molecular origin and high degree of homology between the muscarinic and adrenergic receptor families, cross-reactivity of some muscarinic antagonists with adrenergic receptors is likely27. For example, muscarinic toxin 3 (MT3, with high selectivity for the M4 receptor) has been shown to bind with high affinity to α-adrenergic receptors in mammals28. It is possible that such cross-reactivity may also be displayed by other muscarinic receptor antagonists including atropine. Further, previous studies have revealed that atropine, especially at high concentrations, had direct α-adrenoceptor blocking activity, which may account, at least in part, for the “atropine flush”29,30. In view of the above, such cross-reactivity could also affect the choroidal vasculature that is innervated by both sympathetic and parasympathetic nerves. Therefore, blockade of α-adrenoceptor in the choroidal vascular could also cause thickening of the choroid.
Finally, a non-adrenergic, non-cholinergic (NANC) dilator response which is potentiated by blockade of presynaptic muscarinic receptors may also be a plausible reason. Anticholinergic drugs such as atropine caused a vasodilation response in ocular blood vessels, potentially through their action on pre-junctional muscarinic receptors (possibly the M2 subtype), thus increasing the release of neural nitric oxide (NO) from vasodilator nerves31. In an ARVO annual meeting abstract, Carr et al.32 found that atropine could stimulate cyclic adenosine monophosphate (cAMP) synthesis in NO-ergic neurons, thereof producing abundant of NO, and NO is necessary for choroidal thickening33. Moreover, it is possible that atropine may indirectly affect the retina, by causing the release of dopamine or other neurotransmitters34, and it has been reported that dopamine can cause increase in choroidal thickness35.
To date, there are seven studies that report the effect of topical anticholinergic or adrenergic agents on the choroidal thickness. The details of these studies have been summarized in Table 1. Clearly, different results can be obtained even with the use of the same anticholinergic agents such as Mydrin-P, and tropicamide. We speculate that such discordance may be attributed to the difference in the race of participants, methods of instillation, bioactivities of anticholinergic agents36, and variations in individual responses to topical ocular eye drops. For example, the efficacy of all antimuscarinic agents is influenced by the amount of iris pigmentation. In addition, the amount of topical instillation that reaches the posterior is also an important factor that needs to be taken into account. There are three potential routes for penetration of topically applied ophthalmic drugs to the posterior segment: (1) the trans-vitreous route: trans-corneal diffusion followed by entry into vitreous and subsequent distribution to ocular tissues; (2) periocular route: diffusion around the sclera followed by trans-scleral absorption and (3) uvea-scleral route: trans-corneal diffusion followed by progression through the uvea-sclera37. Among these, the conjunctiva/scleral route is more important that it allows diffusion of drug into more posterior structures of the uveal tract. Atropine is a hydrophilic drug that can easily penetrate the sclera and reach the choroid.
It would have been ideal to study changes in different components of choroidal vasculature, similar to those reported in previous studies38,39,40,41; unfortunately, it was difficult to differentiate the various segmentations of choroidal vasculature in the present study. Therefore, we could not determine the exact reason for the thickening of choroid induced by atropine. This is a potentially interesting topic and deserves further explorations in the near future. Further, it would also be interesting to explore the proportionate change in the luminal and stromal areas of choroid before and after administration of atropine42.
The present study had some limitations that need to be considered. First, the sample size is relatively small and only children aged between 5 and 10 years were recruited. Therefore, the effect of atropine in the choroids of adults is unclear. Second, automated quantifying of choroidal thickness via software is yet not available commercially. Therefore, the choroidal thickness was manually measured using the built-in measuring tool. The wide range of 95% limitis of agreement in Fig. 2 and the large repeatability coefficients (more than 40 μm) indicated a large inter-observer variability in the present study. In order to reduce the error of the measurements, the choroidal thickness recorded by the two observers were averaged to obtain the final measurement at each point. Further research with larger sample sizes is needed to better elucidate the effect of atropine on the choroidal thickness. Third, we could not analyze retinal thickness following atropine administration as some of the children were too young to cooperate after OCT scan in the choroidal mode.
In conclusion, in the present study, we found that topical administration of 1% atropine gel can significantly increase choroidal thickness in young Chinese children, with different magnitude of change at different locations. However, the change in which segmentation of choroidal vasculature contributes to the thickening is still unclear and warrants further exploration using advanced OCT technologies.
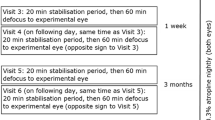
Subjects and Methods
This was a prospective comparative study. The Institutional Review Board of Nanjing Medical University Affiliated Wuxi Second Hospital approved the protocol. All participants gave their informed consent to participate in the clinical examination program, and our study was performed in accordance with the tenets of the Declaration of Helsinki.
Subjects
Thirty-five healthy children were initially recruited into this comparative study between December 2015 and March 2016. Subjects with a history of any ophthalmic disease (except for refractive errors) were excluded. All subjects were screened for the presence of ocular diseases through a complete ophthalmologic examination, including fundus examination. Autorefraction was carried out with the Topcon autorefractor (KR-8900) to obtain the refractive states of participants after cycloplegia. A mean spherical equivalent (SE) was calculated as sphere power plus half the cylindrical power. The axial length was measured with the IOLMaster 500 (software version: 7.5.3.0084, Carl Zeiss Meditec, Dublin, CA). It is well known that the IOLMaster is simple to use and ideal for axial length assessment43, even in children44. Fifty-nine eyes of 30 subjects satisfying the inclusion criteria were finally assessed in the study. A single drop of 1% atropine gel was administered twice daily for a week. Because of the potential side effects of the drug, a careful history and assessment of the anterior chamber angle was made before use.
Choroidal thickness measurement
All children underwent spectral-domain optical coherence tomography (SD-OCT) before and after one week of 1% atropine treatment that induced a continuous cycloplegia. Choroidal imaging was performed using a high-speed 840-nm-wavelength SD-OCT instrument (RTVue XR Avanti; Optovue, Inc, Fremont, California, USA). All OCT scans were performed by an operator (T.T.C) at approximately 0900 and 1100 hours both before and after cycloplegia, to avoid diurnal variations45,46. Fovea-centered, 6-mm horizontal and vertical high definition cross-line scans were taken with the chorioretinal line mode. Post-cycloplegia scans were obtained using the follow-up mode to obtain images from the previous location. All images underwent manual segmentation by two researchers in a blind-manner. RTVue manual measurement tools included calipers for delineating the boundaries of the choroid.
Choroidal thickness was determined as the perpendicular distance between the outermost edge of the hyper-reflective line of the retinal pigment epithelium and the sclerochoroidal border, as reported previously47. Choroidal thickness was measured at the subfovea and at 1.0 mm intervals (up to 3.0 mm) from the fovea at superior, inferior, nasal, and temporal locations. All parameters were measured by two independent observers. Choroidal thickness values recorded by the two observers were averaged to obtain the final measurement at each point. In case of a discrepancy in the measurement of choroidal thickness i.e. if the difference in choroidal thickness values recorded by the two observers exceeded by 20% of the mean of the two values, then the measurements were checked by another senior observer who gave the final adjudication, as reported in our previous study47.
Measurement Reproducibility
To assess reliability of measurements of choroidal thcikness, interobserver reproducibility was evaluated using intraclass correlation coefficient (ICC)48. The ICC is an index of measurement reliability that ranges from 0 to 1, with values of the ICC of 0.81–1.00 indicating almost perfect agreement. Besides, Bland-Altman plots were performed to see if there was any proportional bias between measurements49. A 95% limitis of agreement (LOA) was defined as mean ± 1.96* standard deviation. In addition, the repeatability coefficient were also calculated for the inter-observer measurements according to the methods outlined by Bland and Altman. Specifically, the repeatability coefficient was defined as the standard deviation of the difference between the two repeated measurements multiplied by 1.9649.
Statistical Analysis
All values of choroidal thickness are expressed as mean ± SD. Statistical analyses were performed using SPSS software (version 18.0, SPSS, Chicago, IL, USA). A one-sample Kolmogorov-Smirnov test was used to assess the normal distribution of continuous variables before a test of significance was applied. As a result, all of the continuous variables were normally distributed. Choroidal thickness values after a-week of topical 1% atropine gel treatment were compared to the baseline using paired Student’s t-test. The changes of choroidal thickness in the different meridian (temporal, nasal, superior and inferior) was analyzed using one way analysis of variance (ANOVA). P < 0.05 was considered statistically significant. All tests were two-tailed.
Additional Information
How to cite this article: Zhang, Z. et al. The effect of topical atropine on the choroidal thickness of healthy children. Sci. Rep. 6, 34936; doi: 10.1038/srep34936 (2016).
References
Nickla, D. L. & Wallman, J. The multifunctional choroid. Prog Retin Eye Res. 29, 144–168 (2010).
Neuhuber, W. & Schrodl, F. Autonomic control of the eye and the iris. Auton Neurosci. 165, 67–79 (2011).
Arumugam, B. & McBrien, N. A. Muscarinic antagonist control of myopia: evidence for M4 and M1 receptor-based pathways in the inhibition of experimentally-induced axial myopia in the tree shrew. Invest Ophthalmol Vis Sci. 53, 5827–5837 (2012).
Diether, S. et al. Effects of intravitreally and intraperitonally injected atropine on two types of experimental myopia in chicken. Exp Eye Res. 84, 266–274 (2007).
Luft, W. A., Ming, Y. & Stell, W. K. Variable effects of previously untested muscarinic receptor antagonists on experimental myopia. Invest Ophthalmol Vis Sci. 44, 1330–1338 (2003).
Kim, M., Kwon, H. J. & Lee, S. C. Influence of mydriatics on choroidal thickness measurement using enhanced depth imaging-OCT. Optom Vis Sci. 89, 1150–1155 (2012).
Hao, J. et al. Changes in subfoveal choroidal thickness before and after dilation in adolescents with mild and moderate myopia observed with enhanced depth imaging spectral-domain optical coherence tomography. Chin J Optom Ophthalmol Vis Sci. 15, 624–627 (2013).
Mwanza, J. C., Sayyad, F. E., Banitt, M. R. & Budenz, D. L. Effect of pupil dilation on macular choroidal thickness measured with spectral domain optical coherence tomography in normal and glaucomatous eyes. Int Ophthalmol. 33, 335–341 (2013).
Sander, B. P., Collins, M. J. & Read, S. A. The effect of topical adrenergic and anticholinergic agents on the choroidal thickness of young healthy adults. Exp Eye Res. 128, 181–189 (2014).
Kara, N. et al. Effects of two commonly used mydriatics on choroidal thickness: direct and crossover effects. J Ocul Pharmacol Th. 30, 366–370 (2014).
Yuvacı, İ. et al. An evaluation of effects of different mydriatics on choroidal thickness by examining anterior chamber parameters: the ccheimpflug imaging and enhanced depth imaging-OCT study. J Ophthalmol. 2015, 981274, 10.1155/2015/981274 (2015).
Chia, A. et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology. 119, 347–354 (2012).
Chia, A., Lu, Q. S. & Tan, D. Five-year clinical trial on atropine for the treatment of ayopia 2. Ophthalmology. 123, 391–399 (2015).
Shih, K. C. et al. Use of atropine for prevention of childhood myopia progression in clinical practice. Eye Contact Lens. 42 (2016).
Morgan, I. G. & He, M. An important step forward in myopia prevention: low-dose atropine. Ophthalmology. 123, 232–233 (2016).
Read, S. A., Alonso-Caneiro, D., Vincent, S. J. & Collins, M. J. Longitudinal changes in choroidal thickness and eye growth in childhood. Invest Ophthalmol Vis Sci. 56, 3103–3112 (2015).
Yen, M. Y., Liu, J. H., Kao, S. C. & Shiao, C. H. Comparison of the effect of atropine and cyclopentolate on myopia. Ann Ophthalmol. 21, 180–182 (1989).
Nickla, D. L. & Kristen Totonelly, M. S. Choroidal thickness predicts ocular growth in normal chicks but not in eyes with experimentally altered growth. Clin Exp Optom. 98, 564–570 (2015).
Woodman, E. C., Read, S. A. & Collins, M. J. Axial length and choroidal thickness changes accompanying prolonged accommodation in myopes and emmetropes. Vision Res. 72, 34–41 (2012).
Woodman-Pieterse, E. C., Read, S. A., Collins, M. J. & Alonso-Caneiro, D. Regional changes in choroidal thickness associated with cccommodation. Invest Ophthalmol Vis Sci. 56, 6414–6422 (2015).
Chiang, S. T., Phillips, J. R. & Backhouse, S. Effect of retinal image defocus on the thickness of the human choroid. Ophthalmic Physiol Opt. 35, 405–413 (2015).
Li, M. et al. Change in choroidal thickness and the relationship with accommodation following myopic excimer laser surgery. Eye (Lond). 30, 972–978 (2016).
Meriney, S. D. & Pilar, G. Cholinergic innervation of the smooth muscle cells in the choroid coat of the chick eye and its development. J Neurosci. 7, 3827–3839 (1987).
Nickla, D. L. & Schroedl, F. Parasympathetic influences on emmetropization in chicks: evidence for different mechanisms in form deprivation vs negative lens-induced myopia. Exp Eye Res. 102, 93–103 (2012).
Nickla, D. L., Zhu, X. & Wallman, J. Effects of muscarinic agents on chick choroids in intact eyes and eyecups: evidence for a muscarinic mechanism in choroidal thinning. Ophthalmic Physiol Opt. 33, 245–256 (2013).
Junghans, B., Crewther, S. & Crewther, D. Choroidal lympthatics: An active storage reservoir. Invest Ophthalmol Vis Sci. 39, S504 (1998).
Kerlavage, A. R., Fraser, C. M., Chung, F. Z. & Venter, J. C. Molecular structure and evolution of adrenergic and cholinergic receptors. Proteins. 1, 287–301 (1986).
Näreoja, K. et al. Adrenoceptor activity of muscarinic toxins identified from mamba venoms. Br J Pharmacol. 164, 538–550 (2011).
Chang, K. C. & Hahn, K. H. Is alpha-adrenoceptor blockade responsible for atropine flush? Eur J Pharmacol. 284, 331–334 (1995).
Kwan, C. Y., Zhang, W. B., Kwan, T. K. & Sakai, Y. In vitro relaxation of vascular smooth muscle by atropine: involvement of K+ channels and endothelium. Naunyn Schmiedebergs Arch Pharmacol. 368, 1–9 (2003).
Ayajiki, K., Tanaka, T., Okamura, T. & Toda, N. Evidence for nitroxidergic innervation in monkey ophthalmic arteries in vivo and in vitro. Am J Physiol Heart Circ Physiol. 279, H2006–2012 (2000).
Carr, B., Nathanson, N. & Stell, W. Atropine prevents myopia via a nitric oxide-mediated relay. Invest Ophthalmol Vis Sci. 54, 3677–3677 (2013).
Nickla, D. L. et al. Inhibiting the transient choroidal thickening response using the nitric oxide synthase inhibitor l-NAME prevents the ameliorative effects of visual experience on ocular growth in two different visual paradigms. Exp Eye Res. 83, 456–464 (2006).
Schwahn, H. N., Kaymak, H. & Schaeffel, F. Effects of atropine on refractive development, dopamine release, and slow retinal potentials in the chick. Vis Neurosci. 17, 165–176 (2000).
Dhillon, B., Armani, J. & Nickla, D. The ocular growth inhibition effected by dopamine agonists and atropine is associated with transient increases in choroidal thickness in chicks. Invest Ophthalmol Vis Sci. 49, 1732–1732 (2008).
Smith, S. A. Factors determining the potency of mydriatic drugs in man. Br J Clin Pharmacol. 3, 503–507 (1976).
Mizuno, K. et al. Route of penetration of topically instilled nipradilol into the ipsilateral posterior retina. Invest Ophthalmol Vis Sci. 50, 2839–2847 (2009).
Branchini, L. A. et al. Analysis of choroidal morphologic features and vasculature in healthy eyes using spectral-domain optical coherence tomography. Ophthalmology. 120, 1901–1908 (2013).
Adhi, M., Brewer, E., Waheed, N. K. & Duker, J. S. Analysis of morphological features and vascular layers of choroid in diabetic retinopathy using spectral-domain optical coherence tomography. JAMA Ophthalmol. 131, 1267–1274 (2013).
Adhi, M. et al. Analysis of the thickness and vascular layers of the choroid in eyes with geographic atrophy using spectral-domain optical coherence tomography. Retina. 34, 306–312 (2014).
Park, K. A. & Oh, S. Y. An optical coherence tomography-based analysis of choroidal morphologic features and choroidal vascular diameter in children and adults. Am J Ophthalmol. 158, 716–723 (2014).
Sonoda, S. et al. Luminal and stromal areas of choroid determined by binarization method of optical coherence tomographic images. Am J Ophthalmol. 159, 1123–1131 (2015).
Lam, A. K., Chan, R. & Pang, P. C. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt. 21, 477–483 (2001).
Carkeet, A. et al. Repeatability of IOLMaster biometry in children. Optom Vis Sci. 81, 829–834 (2004).
Brown, J. S. et al. In vivo human choroidal thickness measurements: evidence for diurnal fluctuations. Invest Ophthalmol Vis Sci. 50, 5–12 (2009).
Tan, C. S., Ouyang, Y., Ruiz, H. & Sadda, S. R. Diurnal variation of choroidal thickness in normal, healthy subjects measured by spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 53, 261–266 (2012).
Zhang, Z. et al. Changes in choroidal thickness after panretinal photocoagulation for diabetic retinopathy: a 12-week longitudinal study. Invest Ophthalmol Vis Sci. 56, 2631–2638 (2015).
McAlinden, C., Khadka, J. & Pesudovs, K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt. 31, 330–338 (2011).
Bland, Martin J. & Altman, Douglas G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1, 931–936 (1986).
Acknowledgements
This study was supported by the research project plan of Wuxi Health Bureau (Q201309).
Author information
Authors and Affiliations
Contributions
Perform experiment, data analysis, write paper, prepare figures and tables (Z.Z.), data analysis, data collection (Y.Z. and S.L.), data collection (T.C.), data analysis (Z.X. and Y.G.), experiment design, write paper (Z.W.).
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, Z., Zhou, Y., Xie, Z. et al. The effect of topical atropine on the choroidal thickness of healthy children. Sci Rep 6, 34936 (2016). https://doi.org/10.1038/srep34936
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep34936
This article is cited by
-
Short-Term Effects of Atropine 0.01% on the Structure and Vasculature of the Choroid and Retina in Myopic Chinese Children
Ophthalmology and Therapy (2022)
-
Auricular acupressure for myopia prevention and control in children and its effect on choroid and retina: a randomized controlled trial protocol
Trials (2021)
-
Changes in subfoveal choroidal thickness in myopic children with 0.01% atropine, orthokeratology, or their combination
International Ophthalmology (2021)
-
The acute effect of atropine eye drops on the human full-field electroretinogram
Documenta Ophthalmologica (2021)
-
Studies on retinal mechanisms possibly related to myopia inhibition by atropine in the chicken
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.