Abstract
Breast reconstruction with transverse rectus abdominis myocutaneous (TRAM) flap is challenging in patients with low midline abdominal scar. In this study, we aimed to investigate the clinical feasibility of immediate breast reconstruction using single-pedicle TRAM (SP-TRAM) flaps in patients with low midline abdominal scar. There were 4 strict selection criteria: 1) presence at least 3 perforators on the pedicle side; 2) perforators with regional average flow velocity of >20 cm/s; 3) upper edge of the abdominal scar at least 4 cm from the umbilicus; and 4) scar age >1 year. Eight breast cancer patients with low midline abdominal scar (scar group) and 20 without (control group) underwent immediate breast reconstruction with SP-TRAM flaps consisting of zone I and III and zone II tissues. Flap complications, donor-site complications, and cosmetic results were compared between the two groups. All flaps survived and both groups presented similar flap and donor site complications, including fat necrosis, seroma, hematoma, infection, delayed wound healing, and abdominal hernia, and patients in both groups had similar aesthetic results (p > 0.05). Thus, the study demonstrated that breast reconstruction using SP-TRAM flap was a safe approach in carefully selected patients with low midline abdominal scar.
Similar content being viewed by others
Introduction
Transverse rectus abdominis myocutaneous (TRAM) flap and its variations are considered the best available options for autologous breast reconstruction after mastectomy1,2,3,4. Abdominal scars from previous surgeries often present a challenge when TRAM flap is desired for breast reconstruction1,2,5,6,7,8. In patients with low midline abdominal scars, for instance, tissue perfusion across the midline scar is unreliable, which may lead to flap necrosis, fat necrosis, or wound breakdown at the donor site2,5,7.
Nonetheless, TRAM flaps can still be appropriate for breast reconstruction even in the presence of a low midline abdominal scar9. Various operative strategies have been suggested to improve flap survival and reduce donor-site complications in these patients. A hemi-TRAM flap can be used safely in patients with low midline abdominal scar5,9,10, but it will limit the volume of the reconstructed breast1,2,5,10. Thus, other techniques, including double-pedicle or free TRAM flaps and deep inferior epigastric perforator (DIEP) flaps, which can augment tissue perfusion across midline scars, have also been proposed5,10. However, all of these methods are complex and tedious, and furthermore, the use of complicated microsurgical techniques may not be practical in all clinical situations2,5.
In this study, we performed breast reconstruction using single-pedicle TRAM (SP-TRAM) flaps in selected patients with low midline abdominal scar. In order to guarantee sufficient flap volume at the donor site, the locations and peak systolic flow velocities of the perforators were determined by preoperative color-flow duplex scanning for each patient. We compared the outcomes of SP-TRAM breast reconstruction in patients with or without low midline abdominal scar in 8 (scar group) and 20 (control group) patients, respectively, and this small series demonstrated the safety and feasibility of SP-TRAM flaps in patients with low midline abdominal scar.
Results
Patient characteristics
There were no significant differences in age, body mass index (BMI), smoking history, diabetes mellitus, and neo-adjuvant chemotherapy or preoperative radiotherapy between the scar and control groups, and no significant difference between groups in pathological characteristics (Table 1).
All patients in both groups received SP-TRAM flaps (including zones I, III, and II) showing sufficient blood supply in zone II. During mean follow-up of 24.3 months (range, 8 to 34 months) all patients remained alive, and most remained disease-free, excepting one patient in the control group who developed brain metastasis.
Cosmetic effects
The cosmetic effects were recorded as “excellent-good” in 75.0% (6/8) and “fair-poor” in 25.0% (2/8) of patients in the scar group and as “excellent-good” in 85.0% (17/20) and “fair-poor” in 15.0% (3/20) patients in the control group (Fig. 1). The differences between groups were not significant (p = 0.61).
(A) A 37-year-old woman with invasive ductal carcinoma in the right outer quadrant close to the areola. A1: Location and peak systolic flow velocities of the perforators were assessed with pre-operative color-flow duplex ultrasound scanning. A2: The patient had a previous low midline abdominal scar and breast reconstruction with a single-pedicle transverse rectus abdominis myocutaneous (SP-TRAM) flap was planned. A3: The patient underwent mastectomy with immediate reconstruction using single-pedicle TRAM flap and was followed for 20 months. (B) A 50-year-old woman with invasive ductal carcinoma in the right central quadrant. B1: The perforator locations and peak systolic flow velocities were detected by pre-operative color-flow duplex scanning. B2: The patient had previous low midline abdominal scar and was scheduled for mastectomy with immediate SP-TRAM flap breast reconstruction. B3: The same patient at 6 months after surgery.
Flap-related complications
One patient in each group had partial flap loss. There were no instances of total flap loss. One patient (1/8; 12.5%) in the scar group and 3 patients (3/20; 15%) in the control group developed fat necrosis; the rates of partial flap loss and fat necrosis were not statistically different between the two groups (p = 1.00). No patient in either group developed seroma, hematoma, or flap-site infection, and there was no significant difference in the overall complication rates between the two groups (Table 2).
Donor-site related complications
One patient in each group (1/8, 12.5%; 1/20, 5%) developed incisional infection; the rates of fat necrosis and delayed wound healing in each group were also 1/8 (12.5%) and 1/20 (5%). One patient in the control group (1/20, 5%) developed hematoma. Abdominal hernia or bulge and seroma did not occur in either group. The overall rates of donor-sites complications were not statistically different between the two groups (p = 0.37) (Table 3).
Discussion
In most cases, abdominal scar does not preclude the use of the TRAM flap, but it may determine how much tissue is available for use in the breast reconstruction2, especially in patients with low midline abdominal scar2,7,11. Flap perfusion across the midline scar in these patients is potentially insufficient1,2,5,12, but hemi-TRAM flaps may not be sufficient for reconstruction of a large breast, while hemi-TRAM flaps with larger volumes may cause greater tension in the abdominal wound and prevent closure. Therefore, zone II tissues across the midline scar may have to be included when designing a TRAM flap.
Several alternate strategies have been developed for matching the contralateral breast in these cases, including creation of bilateral-pedicled TRAM flaps2,5,11, developing the flap higher in the abdomen, and anastomosing a contralateral deep inferior epigastric artery2. While these techniques may augment flap perfusion across the midline scar, they are technically complicated, require long operation times, and may cause hemodynamic crisis. Thus, they are not practical in all patients with low midline abdominal scar. In the present study, which included Chinese breast cancer patients with and without low midline abdominal scar, we used SP-TRAM flaps for immediate breast reconstruction after mastectomy, which simplified the surgical procedure and minimized operative injury. The results demonstrated that it is feasible to use SP-TRAM flaps in in strictly selected patients who have relatively small breasts without increasing the risk of post-operative complications.
Previous abdominal wall surgery is known to alter the vascular anatomy and architecture, specifically of the cutaneous vasculature13. According to the delay phenomenon, ischemia due to abdominal wall incision is usually compensated over time by the functional dilation of adjacent vessels7,13,14. In keeping with this phenomenon, Heller et al.2 found that perfusion across the midline scar to the contralateral side was surprisingly good, and zone II tissues were usable for breast reconstruction. Santamaria et al. reported that contrast material was detected in zone II across the midline scar in 7 patients within minutes of contrast injection into the inferior epigastric artery15. Han et al. investigated the effects of an abdominal midline incision on the survival of TRAM flaps in a rat model and found that the scars experienced changes similar to those observed during the delay phenomenon in humans, with increasing size and density of the subdermal plexus16. Thus, the delay phenomenon may also play an important role in the regenerative potential of perforators, obstructed vessels, and the subdermal vascular plexus. Recent studies have indicated that there is a significant increase in microvascular density in the subdermal layer during the repair process following injury16,17, which was sustained for up to 52 weeks after the injury. It is assumed that the older the scar, the greater the extent of neo-vascularization16,17, so the age of the scar should be at least 1 year, as in our study, to allow regeneration of transected perforators. Rand et al.18 have recommended that the donor site should have >3 perforators with flow velocities if >20 cm/s in order to support an SP-TRAM flap. Because separating the umbilicus from the flap will damage the perforators across periumbilical areas, we recommend that distance from the upper edge of the low midline abdominal scar to the umbilicus should be >4 cm. Moreover, we routinely resect zone IV tissues while preserving the zone II tissues.
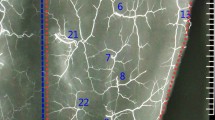
Color duplex ultrasonography, CT angiography and MR angiography methods are useful for preoperative assessment of flap perfusion in the presence of abdominal scar19,20. Intraoperative laser-assisted indocyanine green (ICG) angiography is also used to measure the perfusion of the TRAM flap before flap harvest and transfer21,22. While color duplex ultrasound can be a simple and effective modality for examining the patient’s vascular anatomy and determining the number of perforators19. In our study, this modality allowed visualization of perforators >1 mm in diameter, localization of major perforators, and determination of peak systolic flow velocities in all patients.
Rates of flap necrosis after breast reconstruction have ranged from 5.0% to 35.0%3,8 overall, and from 11.7% to 16.1% for free TRAM flap with previous abdominal scar6,8,23. In our study, strict selection of patients resulted in a rate of flap necrosis in the scar group (25.0%) that was not statistically different from that in the control group (20.0%) (p = 1.00). Anastomotic branches of superior and deep inferior gastric arteries are most abundant in the periumbilical area18. In our study, the perforators were most frequently identified in zone II which was within 4 cm below umbilicus (Tables 4 and 5). Our flaps were designed with a superior border 2.0 cm above the umbilicus and an inferior border 10 cm below the umbilicus in order to obtain a larger scar-free and vascularized area2 (Fig. 1), and the tendons of rectus abdominis were preserved to avoid injury to the perforators. These measures are key to flap survival and can potentially reduce rates of fat necrosis and flap loss. In our study, fat necrosis occurred in 1 patient (1/8; 12.5%) in the scar group and in 3 patients (3/20; 15.0%) in the control group, and the overall rates of flap-related complications were not significantly different between the two groups.
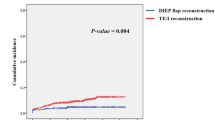
There are still controversies in terms of donor-site complications. Some have reported increased risk of abdominal complications6,24,25 while others have not1,8,11,23,26. In our study, there were no differences in the rates of incision infection (12.5% versus 5.0%, p = 0.50) or delayed wound healing (12.5% versus 5.0%, p = 0.50) between the scar group and the control groups, and there was no significant difference in the overall complication rates (37.5% versus 20.0%, p = 0.37), which indicates that SP-TRAM flaps are safe and feasible even in the presence of low midline abdominal scar. Use of a Prolene mesh repair for the abdominal defect has been associated with similar complication rates in patients undergoing SP-TRAM flap and DIEP flap breast reconstruction27. In the present study, we used mesh repair for the rectus sheath defects and there were no instances of subsequent abdominal wall hernia or bulge during the follow-up period. We continue to recommend the use of mesh to repair the abdominal wall defect in patients receiving pedicled flaps28,29.
Cosmetic effects were evaluated independently by three surgeons, excluding the operating surgeons, and were comparable in the scar group and the control group, which is consistent with previous reports7,11.
In comparison with free TRAM flaps or DIEP flaps, breast reconstruction with SP-TRAM flap allows shorter operation times and does not require microvascular anastomosing techniques. Thus, even with the development of these more complex and purportedly more beneficial techniques, the SP-TRAM flap remains a reliable alternative for breast reconstruction that yields a high degree of patient satisfaction3,30, and the good clinical results in our patients confirm that breast reconstruction with the SP-TRAM flap is feasible in patients with low midline abdominal scar.
Conclusions
In this study, 8 patients with low midline abdominal scar who met strict selection criteria underwent successful SP-TRAM flap breast reconstruction. Our clinical findings have demonstrated that in carefully selected patients, tissues across the midline scar will have a relatively sufficient blood supply and can be safely used for SP-TRAM flap breast reconstruction.
Patients and Methods
A total of 28 consecutive patients who underwent unilateral breast reconstruction with SP-TRAM flap after mastectomy from April 2013 to October 2015 at the Breast Center of the Cancer Hospital of Shantou University Medical College, 8 with previous low midline abdominal scar (scar group) and 20 without low midline abdominal scar (control group), were included in the study. In the scar group, the average length of the vertical low midline abdominal scar was 9.3 cm (range, 5 cm to 14.5 cm). The mean age of the midline abdominal scar was 13.5 years (range, 4 to 28 years). The clinico-pathological characteristics of both groups are shown in Table 1.
Preoperative blood supply was evaluated by color-flow duplex ultrasound imaging using the Philips IU-22 device, and locations and peak systolic flow velocities of major perforator vessels of the rectus abdominis muscles were identified in both groups. In the scar group the abdomen was divided into quadrants centered around the umbilicus so that perforator locations could be placed within a Cartesian grid18. As previously reported, four zones were divided with 4 cm height by designating the umbilicus as the zero position18. Locations of major perforators along the superior and inferior epigastric arteries were identified, and the peak systolic flow velocities of the perforators were measured in each zone, as shown in Tables 4 and 5. Patients with low-midline abdominal scars met the following selection criteria for breast reconstruction with SP-TRAM flap: 1) at least 3 perforators in the flap territory; 2) average peak systolic flow velocities of the perforators of >20 cm/s; 3) upper edge of the midline scar >4 cm from the umbilicus; and 4) scar age >1 year.
Surgical Technique
All 28 patients underwent breast reconstruction with SP-TRAM flap performed by the same surgical team. In 8 patients with low-midline abdominal scar, the flaps were outlined on the lower abdomen including the position of the perforators identified by color Doppler. The upper edge of the abdominal incision was 2 cm above the umbilicus, so that the more superior flap was scar-free in order to allow a larger skin bridge. The lower incision included 1/2 to 2/3 of the upper portion of the scar according to the volume of the reconstructed breast and the tension required to permit closure of the abdominal donor site. During the procedure, the skin and subcutaneous tissue of the flap were dissected to the anterior rectus sheath and the upper abdominal subcutaneous tissues were separated in order to form a tunnel to the chest wall, and the umbilicus was separated and retained on the anterior rectus sheath. The anterior wall of the rectus sheath was separated and the tendon was reserved on the muscle. The skin color and bleeding condition of the flap were observed for 15 to 20 min, with particular attention to the tissues of zone II across the midline scar, and perfusion of the flap was assessed by capillary refill. If the perfusion was deemed sufficient, flaps including zone II could be harvested and transferred for breast reconstruction with TRAM flaps, otherwise, the tissues were harvested as hemi-TRAM flaps.
The flaps were rotated through the subcutaneous tunnel to the chest defect, and the defect of the anterior wall of the rectus sheath was repaired with a mesh. The umbilicus was pulled out to the abdominal wall through a small incision and sutured, and, following drain placement, the abdominal wall closed. Finally, the flap was shaped to match the contralateral breast.
Post-operative Evaluation and Follow-up
Immediate post-reconstructive complications were recorded as flap or donor-site related. Flap-related complications were total flap loss, defined as complete necrosis of the skin and fat; partial flap loss, defined as ischemic tissue loss exceeding 25% or fat necrosis characterized by subcutaneous firmness >7.5 cm in diameter6,30; fat necrosis, defined as loss of a portion of the adipose component with subcutaneous firmness of at least 2 cm to 7.5 cm in diameter1,6,30,31; seroma formation, defined as palpable fluctuation of subcutaneous tissues requiring suction or drainage; and wound dehiscence and wound infection, defined as redness, swelling, and exudate and requiring antibiotics1,23. Donor-site complications included seroma, wound infection, fat necrosis, postoperative hematoma requiring evacuation, delayed wound healing, and abdominal wall bulge or hernia requiring operative repair24,30.
All patients had follow-up examinations every 3 months, and cosmetic effects were evaluated by using postoperative photographs obtained at 6 months after surgery. The cosmetic effects were assessed by a team of expert surgeons that excluded the operating surgeons. Four items (symmetry, volume, position of the infra-mammary fold, and ptosis) were assessed, and cosmesis was defined as excellent, good, fair, or poor according to the Lowery Scaling System32. To minimize bias in our results, the cosmetic effects were rated as either “excellent-good” or “fair-poor.”
Statistical Analysis
SPSS version 13.0 software (SPSS, Inc., Chicago, IL, USA) was used for statistical analysis, with comparison of discrete variables by Pearson chi-square or Fisher’s exact test, and comparison of means by t-test. A value of p < 0.05 was considered significant.
Ethical approval
This study was approved by the Ethics Committee of the Cancer Hospital of Shantou University Medical College and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and all subsequent revisions. All persons mentioned in the paper gave informed consent prior to their inclusion in the study.
Additional Information
How to cite this article: Wu, J.-D. et al. Breast reconstruction with single-pedicle TRAM flap in breast cancer patients with low midline abdominal scar. Sci. Rep. 6, 29580; doi: 10.1038/srep29580 (2016).
References
Di Candia, M. et al. Previous multiple abdominal surgeries: a valid contraindication to abdominal free flap breast reconstruction? Eplasty. 23, 286–303 (2012).
Heller, L. et al. Strategies and options for free TRAM flap breast reconstruction in patients with midline abdominal scars. Plast Reconstr Surg. 116, 753–759 (2005).
Christensen, B. O. et al. Long-term evaluation of postmastectomy breast reconstruction with the pedicled transverse rectusabdominis musculocutaneous flap. J Plast Surg Hand Surg. 47, 374–378 (2013).
Macadam, S. A. et al. Quality of Life and Patient-Reported Outcomes in Breast Cancer Survivors: A Multicenter Comparison of Four Abdominally Based Autologous Reconstruction Methods. Plast Reconstr Surg. 137, 758–771 (2016).
Berrino, P. et al. The “parasite” TRAM flap for autogenous tissue breast reconstruction in patients with vertical midabdominal scars. Ann Plast Surg. 43, 119–126 (1999).
Roostaeian, J. et al. The effect of prior abdominal surgery on abdominally based free flaps in breast reconstruction. Plast Reconstr Surg. 133, 247e–255e (2014).
Dragu, A. et al. Scars and perforator-based flaps in the abdominal region: a contraindication? Can J Surg. 53, 137–142 (2010).
Nykiel, M. et al. Algorithmic approach to the design and harvest of abdominal flaps for microvascular breast reconstruction in patients with abdominal scars. Ann Plast Surg. 74 Suppl 1, S33–S40 (2015).
Hamdi, M. et al. Harvesting free abdominal perforator flaps in the presence of previous upper abdominal scars. J Plast Reconstr Aesthet Surg. 67, 219–225 (2014).
Chang, C. C. A strategic approach for DIEP flap breast reconstruction in patients with a vertical midline abdominal scar. Ann Plast Surg. 73, Suppl 1, S6–11 (2014).
Hsieh, F. et al. An algorithmic approach to abdominal flap breast reconstruction in patients with pre-existing scars-results from a single surgeon’s experience. J Plast Reconstr Aesthet Surg. 62, 1650–1660 (2009).
Ohjimi, H. et al. Analyzing the vascular architecture of the free TRAM flap using intraoperative ex vivo angiography. Plast Reconstr Surg. 116, 106–113 (2005).
Rozen, W. M. et al. The effect of anterior abdominal wall scars on the vascular anatomy of the abdominal wall: A cadaveric and clinical study with clinical implications. Clin Anat. 22, 815–822 (2009).
Taylor, G. I. et al. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 89, 408–416 (1992).
Santamaria, E. Paper presented at: The Annual Meeting of the World Society of Reconstructive Microsurgery. Heidelberg, Germany. Jun, 11–14 (2003).
Han, S. et al. Effects of the abdominal midline incision on the survival of the transverse rectus abdominis musculocutaneous flap in rat model. Ann Plast Surg. 50, 171–176 (2003).
Brown, N. J. et al. Angiogenesis induction and regression in human surgical wounds. Wound Repair Regen. 10, 245–251 (2002).
Rand, R. P. et al. Color-flow duplex scanning in the preoperative assessment of TRAM flap perforators: a report of 32 consecutive patients. Plast Reconstr Surg. 93, 453–454 59 (1994).
Seidenstucker, K. et al. A prospective study using color flow duplex ultrasonography for abdominal perforator mapping in microvascular breast reconstruction. Med Sci Monit. 16, MT65–MT70 (2010).
Mathes, D. W. et al. Preoperative imaging techniques for perforator selection in abdomen-based microsurgical breast reconstruction. Clin Plast Surg. 37, 581–591 (2010).
Munabi, N. C. et al. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: a prospective trial. J Plast Reconstr Aesthet Surg. 67, 449–455 (2014).
Newman, M. I. et al. An investigation of the application of laser-assisted indocyanine green fluorescent dye angiography in pedicle transverse rectus abdominus myocutaneous breast reconstruction. Can J Plast Surg. 19, e1–e5 (2011).
Laporta, R. Tips and tricks for DIEP flap breast reconstruction in patients with previous abdominal scar. Microsurgery. 10, 1–11 (2015).
Parrett, B. M. et al. DIEP flaps in women with abdominal scars: are complication rates affected? Plast Reconstr Surg. 121, 1527–1531 (2008).
Knox, A. D. et al. Comparison of Outcomes Following Autologous Breast Reconstruction using the DIEP and Pedicled TRAM Flap Part 1:A 12 Year Clinical Retrospective Study and Literature Review. Plast Reconstr Surg. 10, 1–43 (2015).
Mennie, J. C. et al. Donor-Site Hernia Repair in Abdominal Flap Breast Reconstruction: A Population-Based Cohort Study of 7929 Patients. Plast Reconstr Surg. 136, 1–9 (2015).
Wan, D. C. et al. Inclusion of mesh in donor-site repair of free TRAM and muscle-sparing free yields rates of abdominal complications comparable to those of DIEP flap reconstruction. Plast Reconstr Surg. 126, 367–374 (2010).
Petit, J. Y. et al. Abdominal complications and sequelae after breast reconstruction with pedicled TRAM flap: is there still an indication for pedicled TRAM in the year 2003? Plast Reconstr Surg. 112, 1063–1065 (2003).
Chatterjee, A. et al. The use of mesh versus primary fascial closure of the abdominal donor site when using a transverserectus abdominis myocutaneous flap for breast reconstruction: a cost-utility analysis. Plast Reconstr Surg. 135, 682–689 (2015).
Tan, S. et al. The deep inferior epigastric perforator and pedicled transverse rectus abdominis myocutaneous flap in breast reconstruction: a comparative study. Arch Plast Surg. 40, 187–191 (2013).
Baumann, D. P. et al. Perforator number predicts fat necrosis in a prospective analysis of breast reconstruction with free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 125, 1335–1341 (2010).
Lowery, J. C. et al. Evaluations of aesthetic results in breast reconstruction: an analysis of reliability. Ann Plast Surg. 36, 601–606 (1996).
Acknowledgements
This work was partly supported by funds from the Guangdong Province Enterprise Technology Research and Development and Upgrade Project (NO. 2013B021800263) and Guangdong Provincial Key Laboratory on Breast Cancer Diagnosis and Treatment Research.
Author information
Authors and Affiliations
Contributions
J.-D.W. designed the study, collected clinical data, analyzed the data and wrote the manuscript. W.-H.H. and S.-Q.Q. collected the patients’ clinicopathological records. L.-F.H., C.-P.G. and Y.-Q.Z. collected the patients’ information and prepared the figures. F.Z. contributed to the statistical analysis. G.-J.Z. conceived of and designed the study and revised the manuscript. All authors had final approval of the submitted and published versions and are accountable for the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wu, JD., Huang, WH., Qiu, SQ. et al. Breast reconstruction with single-pedicle TRAM flap in breast cancer patients with low midline abdominal scar. Sci Rep 6, 29580 (2016). https://doi.org/10.1038/srep29580
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29580
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.