Abstract
The optimal treatment strategy for relapsed natural killer/T-cell lymphoma (NKTCL) remains largely unknown. We retrospectively reviewed the treatment modalities and prognosis of 56 relapsed NKTCL patients. Chemotherapy was the initial salvage treatment, followed by radiotherapy (RT) or autologous hematopoietic stem cell transplantation (AHSCT) as consolidative therapy, depending on the status of remission and the pattern of relapse. For patients with locoregional relapse alone, consolidative RT after salvage chemotherapy significantly improved prognosis compared with follow-up (5-year OS: 83.3 vs. 41.7%, P = 0.047). For patients with distant relapse, consolidative AHSCT after salvage chemotherapy significantly prolonged survival compared with follow-up (2-year OS: 100.0 vs. 20.0%, P = 0.004). Patients without consolidative treatment after response to salvage chemotherapy exhibited a comparable survival to those who experienced stable or progressive disease after chemotherapy. Asparaginase (ASP)-containing salvage chemotherapy failed to confer a survival advantage over ASP-absent chemotherapy (5-year OS: 44.2 vs. 39.3%, P = 0.369). In conclusion, consolidative RT or AHSCT improved prognosis in patients with relapsed NKTCL who responded to initial salvage chemotherapy, and the role of ASP in salvage chemotherapy requires further exploration in prospective studies.
Similar content being viewed by others
Introduction
Extranodal natural killer/T-cell lymphoma (NKTCL) is a distinct lymphoid malignancy in the World Health Organization (WHO) classification1,2,3,4. This disease is commonly observed in young males, diagnosed at an early stage, and exhibits a close association with Epstein–Barr virus (EBV) infection3,4. Due to its rarity, the optimal treatment strategy has yet to be established. Radiotherapy (RT) has been well accepted as the primary treatment for early-stage disease5,6,7 and is also beneficial in select cases of advanced-stage disease8. Chemotherapeutic regimens based on anthracycline agents exhibit disappointing efficacy for NKTCL9,10,11,12, probably due to the expression of a multidrug-resistant gene in tumor cells9. However, novel regimens that contain L-asparaginase (L-ASP) or pegaspargase have elicited promising responses13,14,15,16. Autologous and allogeneic hematopoietic stem cell transplantation (HSCT) have been reported as feasible consolidation therapies for high-risk, relapsed, or refractory NKTCL, but whether these approaches are associated with a definitive survival benefit remains controversial17,18,19,20,21,22.
Although approximately 70–90% of early-stage and 15–65% of advanced-stage patients achieve complete remission (CR) after primary therapy5,8,10,11,12,13,23,24,25, a proportion of them eventually experience relapse. The relapse rate of NKTCL varies from 25% to 60%, depending on the treatment modality26,27,28,29,30,31. Due to the rarity of relapsed cases, most studies report patients with relapsed disease together with those who had primary refractory disease or even newly diagnosed advanced-stage disease, which may cause inappropriate interpretation and extrapolation of treatment outcomes13,14,15,32,33,34,35. To date, very few results focusing exclusively on the treatment of relapsed NKTCL are available. Two previous studies have reported the benefits of salvage RT for recurrent NKTCL, but the roles of salvage chemotherapy and HSCT remain to be discovered36,37. In addition, the optimal management of patients with different patterns of relapse, especially those with distant recurrence, remains largely unknown. In this study, we evaluated the outcomes of salvage treatment in a relatively large cohort of patients with relapsed NKTCL, explored the effects of consolidative RT and autologous hematopoietic stem cell transplantation (AHSCT), and compared the efficacy of asparaginase (ASP)-containing and ASP-absent chemotherapy regimens.
Methods
Patient selection and evaluation
The inclusion criteria for this study were as follows: (1) pathologically confirmed NKTCL at initial diagnosis according to the WHO classification of lymphomas3,4; (2) achieved CR after primary treatment according to the International Working Group Recommendations for Response Criteria for non-Hodgkin’s lymphoma38,39; (3) pathologically or clinically diagnosed relapse; and (4) complete follow-up data. The exclusion criteria included the following: (1) experienced relapse within one month after initial CR; and (2) received best supportive care alone after relapse without anti-tumor therapy. Fifty-six patients with relapsed NKTCL between 2001 and 2013 were included in the analysis, 41 (73.2%) of whom had pathologically confirmed relapse and 15 (26.8%) of whom had clinically diagnosed relapse. Informed consent for the collection of medical information was obtained from all patients at their first visit. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the ethics committee of Sun Yat-sen University Cancer Center.
Clinical evaluations at initial presentation and relapse were performed as previously reported8,16. Clinical staging of the tumors was performed according to the Ann Arbor system. The International Prognostic Index (IPI) and the natural killer/T-cell lymphoma prognostic index (NKPI) were calculated for all patients at initial presentation28,40. The primary sites of disease were classified into the upper aerodigestive tract (UAT) and the extra-upper aerodigestive tract (EUAT) as previously reported41. Locoregional relapse (LR) was defined as tumor recurrence at the primary site and/or regional lymph nodes, and distant relapse (DR) was defined as tumor relapse at locations other than the primary site or regional lymph nodes.
Treatment and response evaluation
At initial presentation, the first-line treatment was induction chemotherapy followed by involved-field radiotherapy (IFRT) for patients with early-stage disease (Ann Arbor stage I/II), and chemotherapy alone for those with advanced stage disease (Ann Arbor stage III/IV). Chemotherapy was the initial salvage treatment after relapse. Patients who achieved CR or partial remission (PR) after initial chemotherapy could receive RT or autologous hematopoietic stem cell transplantation (AHSCT) as consolidation therapy, depending on the patient’s physical status and the pattern of recurrence (LR or DR) at the discretion of the treating physician. Chemotherapy regimens varied during the study period according to the treating physicians but were categorized as ASP-containing or ASP-absent regimens, depending on whether L-ASP or pegaspargase was incorporated. Treatment response was evaluated after every two cycles of salvage chemotherapy, before and after consolidative RT or AHSCT (if received), and at the end of salvage treatment, in accordance with the International Working Group Recommendations for Response Criteria for non-Hodgkin’s lymphoma38,39.
Statistical analysis
The duration of CR after first-line treatment was defined as the time from the documentation of an initial CR to relapse. Overall survival (OS) was measured from initial diagnosis to death due to any cause or the most recent follow-up. OS after relapse was calculated from the first recurrence to death due to any cause or the most recent follow-up. Survival data were calculated using the Kaplan-Meier method and compared using a log-rank test. Baseline characteristics and treatment response were compared using the Chi-squared test or Fisher’s exact test. A two-sided P value < 0.05 was considered statistically significant. The statistical analysis was performed using SPSS version 17.0 software (SPSS, Chicago, IL, USA).
Results
Clinical characteristics and treatment at initial presentation
The clinical characteristics at initial diagnosis and first-line treatment are presented in Table 1. Overall, the cohort exhibited low-risk clinical features. The median age of the cohort at presentation was 38 years (range 9–77 years), and 89.3% of the patients were ≤60 years old. Most of the patients presented with early-stage disease (92.9%), primary disease originating from UAT (82.1%), and a good performance status (Eastern Cooperative Oncology Group [ECOG] score of 0–1 in 91.1% of the patients). The IPI was scored as 0–1 in 87.5% of the patients, and the NKPI score was 0–1 in 69.6% of the patients.
Most of the patients (51, 91.1%) received chemotherapy plus RT as their first-line treatment, whereas four (7.1%) received chemotherapy alone, and one (1.8%) received RT alone. RT was administered at a median dose of 50.4 Gy (range 24.0–68.0 Gy), with 75.0% of the patients receiving a dose of ≥50.0 Gy. ASP-containing and ASP-absent regimens were administered as the first-line chemotherapy to 12 patients (21.8%) and 43 patients (78.2%), respectively. The median number of chemotherapy cycles was 5 (range 1–10), and 72.0% of the patients received ≥4 cycles.
Clinical characteristics at relapse
As shown in Table 2, the median duration of CR was 8.9 months (range 1.8–84.5 months). Approximately half of the patients (55.4%) experienced relapse within 12 months after the initial CR. Patterns of relapse included LR alone in 23 (41.1%) patients, DR alone in 9 (16.1%) patients, and combined LR and DR in 24 (42.9%) patients. B symptoms and an elevated LDH level were observed in 42.9% and 39.3% of the patients, respectively. Most of the patients exhibited a good performance status (ECOG score 0–1: 82.1%) at relapse.
Salvage treatment
Salvage treatment after relapse included chemotherapy alone (32 cases, 57.1%), chemotherapy followed by RT (16 cases, 28.6%), and chemotherapy followed by AHSCT (8 cases, 14.3%). As presented in Table 2, among the patients with LR alone, salvage treatment included chemotherapy alone, chemotherapy followed by RT, and chemotherapy followed by AHSCT in 9 (39.1%), 13 (56.1%), and 1 (4.3%) patients, respectively. Of the patients with DR ± LR, chemotherapy alone, chemotherapy followed by RT, and chemotherapy followed by AHSCT were administered to 23 (69.7%), 3 (9.1%), and 7 (21.2%) patients, respectively. Overall, CR, PR, stable disease (SD), and progressive disease (PD) were observed after salvage treatment in 51.8%, 12.5%, 1.8%, and 33.9% of the patients, respectively.
Salvage chemotherapeutic regimens included pegaspargase or L-ASP/gemcitabine/oxaliplatin (P-Gemox/GELOX, 13 cases, 23.2%), ifosfamide/methotrexate/etoposide (IMVP-16, 12 cases, 21.4%), etoposide/doxorubicin/vincristine/cyclophosphamide/prednisone (EPOCH, 7 cases, 12.5%), dexamethasone/ifosfamide/cisplatin/etoposide (DICE, 4 cases, 7.1%), gemcitabine/vinorelbine/doxorubicin (GND, 4 cases, 7.1%), and miscellaneous regimens (16 cases, 28.6%). ASP-containing and ASP-absent regimens were administered to 21 (37.5%) and 35 patients (62.5%), respectively. The median number of chemotherapy cycles was 4 (range 1–9).
Of the 16 patients who received RT after salvage chemotherapy, the pre-RT response was CR/PR in 15 patients and SD in one patient. All of the patients had received RT during first-line treatment. The median radiation dose was 50.0 Gy (range 36.8~60.0 Gy). The radiation field covered all sites of recurrence with adequate margins. RT techniques included conventional two-dimensional RT (9 cases), intensity-modulated RT (IMRT, 4 cases), and three-dimensional conformal RT (3D-CRT, 3 cases).
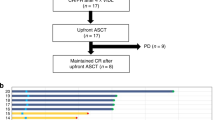
Of the 8 patients receiving AHSCT after salvage chemotherapy, the pre-transplant response was CR in 7 and PR in one patient. Salvage chemotherapy before AHSCT included IMVP-16 (2 cases), EPOCH (2 cases), SMILE, GND, GELOX, and L-ASP + vincristine + dexamethasone (1 cases for each regimen). Conditioning chemotherapy was BEAM (carmustine, etoposide, cytarabine and melphalan) in 7 patients and GemBuMel (gemcitabine, busulfan and melphalan) in one patient.
Survival and prognostic factors after relapse
The median follow-up time for the surviving patients was 74.3 months (range 17.8–146.5 months). At the time of last follow-up, 30 (53.6%) patients had died of lymphoma (n = 29) or treatment-related complications (n = 1). For the entire cohort, the 5-year OS after initial diagnosis was 50.3%, with a median survival of 61.0 months (Fig. 1a). The 5-year OS after relapse was 41.4%, with a median survival of 46.1 months (Fig. 1b).
Survival after relapse significantly differed among patients receiving different salvage treatment modalities. The 5-year OS after relapse was 100.0%, 68.2%, and 13.3% in patients who received chemotherapy followed by AHSCT, chemotherapy followed by RT, and chemotherapy alone, respectively (P < 0.001, Fig. 2). Patients who achieved CR after salvage treatment exhibited a substantially prolonged OS after relapse compared with those who failed to achieve CR (5-year OS after relapse: 74.7% vs. 7.8%, P < 0.001).
In a univariate analysis, patients with LR alone exhibited a significantly better prognosis than those with DR ± LR (60.9 vs. 27.0%, P = 0.016). A duration of CR ≥12 months was associated with a marginally better 5-year OS (50.8 vs. 32.3%, P = 0.056). Other predictors of a better 5-year OS after relapse included age ≤60 years (46.2% vs. 0.0% for age >60, P = 0.003) and ECOG score of 0–1 (50.2% vs. 10.0% for ECOG ≥2, P < 0.001). B symptoms, LDH level, number of extranodal sites, and sex had no significant impact on survival after relapse. Multivariate analysis was not performed due to the small number of events in this cohort 42.
Salvage treatment and survival of patients with locoregional relapse alone
Of the 23 patients with LR alone, one received AHSCT after exhibiting a CR to salvage chemotherapy (this patient lived without lymphoma for 63 months). The remaining 22 patients were classified into three groups: patients who achieved CR/PR after salvage chemotherapy and then received consolidative RT (group A, 12 patients) or follow-up (group B, 6 patients) and patients who experienced SD/PD after salvage chemotherapy (group C, 4 patients). Clinical characteristics at relapse, first-line treatment, and salvage chemotherapeutic regimens were comparable between patients who received consolidative RT (group A) or follow-up (group B, Table 3). Consolidative RT significantly improved 5-year OS after relapse compared with follow-up (83.3 vs. 41.7%, P = 0.047, Fig. 3a). However, survival after relapse was comparable between patients who received follow-up after CR/PR to salvage chemotherapy (group B) and patients with SD/PD to salvage chemotherapy (group C, P = 0.788, Fig. 3a).
(a) Overall survival (OS) after relapse in patients with locoregional relapse alone who received consolidative radiotherapy (RT, the black line) or follow-up (the blue line) after achieving complete or partial remission (CR/PR) after salvage chemotherapy and who exhibited stable or progressive disease (SD/PD) after salvage chemotherapy (red line). (b) OS after relapse in patients with distant relapse who received autologous hematopoietic stem cell transplantation (AHSCT, black line) or follow-up (blue line) after exhibiting CR/PR after salvage chemotherapy and those who had SD/PD after salvage chemotherapy (red line).
Salvage treatment and survival of patients with distant ± locoregional relapse
Of the 33 patients with DR ± LR, three received consolidative RT after achieving CR/PR to salvage chemotherapy, one of whom was alive without lymphoma at 14 months and two of whom died of lymphoma (at 10 and 14 months). The remaining 30 patients were classified into three groups: patients who achieved CR/PR after salvage chemotherapy and then received AHSCT as consolidative therapy (group A, seven patients) or who received follow-up (group B, six patients) and patients who experienced SD/PD after salvage chemotherapy (group C, 17 patients). As shown in Table 3, the clinical characteristics at relapse, first-line treatment, and salvage chemotherapeutic regimens were comparable between patients who received consolidative AHSCT (group A) or follow-up (group B). Marginally more patients in group A achieved CR after chemotherapy; however, this difference did not reach statistical significance (100 vs. 50%, P = 0.070). Compared with follow-up, AHSCT after response to salvage chemotherapy significantly improved 2-year OS after relapse (100.0 vs. 20.0%, P = 0.004, Fig. 3b). All patients in the AHSCT group survived without further recurrence at a median follow-up of 48.1 months. However, survival after relapse was comparable between patients who received follow-up after CR/PR to salvage chemotherapy (group B) and patients who experienced SD/PD after salvage chemotherapy (group C, P = 0.213, Fig. 3b).
Role of asparaginase in salvage treatment
After initial salvage chemotherapy, CR, PR, SD, and PD were observed in 37.5%, 25.0%, 3.6%, and 33.9% of the patients, respectively. The CR rate for ASP-containing regimens was significantly higher than that for ASP-absent regimens (66.7 vs. 20.0%, P < 0.001), but the overall response rates (ORR: CR + PR) were not significantly different (76.2 vs. 54.3%, P = 0.101). Patients who received ASP-containing or ASP-absent regimens as salvage chemotherapy exhibited comparable survival (5-year OS after relapse: 44.2 vs. 39.3%, P = 0.369, Fig. 4a). 19.0% of patients in the ASP-containing group and 23.5% of the patients in the ASP-absent group at relapse received ASP during their first-line chemotherapy (P = 0.750). Responses to chemotherapy during the first-line treatment were comparable between the ASP-containing and ASP-absent groups at relapse (CR + PR: 81.3 vs. 75.0%, P = 0.724). However, there were significantly more patients with an ECOG score ≥2 in the ASP-absent group than in the ASP-containing group (25.7 vs. 4.8%, P = 0.047, Table 4). Among those who received ASP-containing chemotherapy, response (CR + PR: 72.7 vs. 80.0%, P = 1.000) and survival (2-year OS after relapse: 70.0 vs. 46.7%, P = 0.488) were not significantly different between the patients who received L-ASP and those who received pegaspargase.
We also assessed the impact of first-line chemotherapeutic regimens on survival after relapse. During the first-line treatment, 43 (78.6%) and 12 (21.4%) patients received ASP-absent and ASP-containing regimens, respectively, as their induction chemotherapy. As shown in Table 4, no significant difference was observed in the clinical characteristics at relapse, and the first-line and salvage treatment modalities between the two groups. However, patients who received ASP-containing first-line chemotherapy exhibited a substantially worse response to salvage chemotherapy after recurrence compared with those who received ASP-absent first-line chemotherapy (CR + PR: 33.3 vs. 69.8%, P = 0.041). Accordingly, patients who received ASP-containing first-line chemotherapy exhibited significantly worse survival than those who received ASP-absent first-line chemotherapy (2-year OS after relapse: 33.3 vs. 58.6%, P = 0.015, Fig. 4b).
Discussion
In this study, we focused exclusively on the treatment modalities and prognosis of patients with relapsed NKTCL. To our knowledge, this is the largest cohort of this subgroup of patients studied to date. Our findings suggest that the overall prognosis of relapsed NKTCL remains dismal, but patients who achieved CR after salvage treatment exhibited significantly better survival after relapse. For patients with locoregional relapse alone who achieved CR/PR to salvage chemotherapy, consolidative RT substantially improved prognosis compared with follow-up. For patients with distant relapse, adding AHSCT after achieving CR/PR to salvage chemotherapy elicited a significantly better survival compared with follow-up alone. Salvage chemotherapeutic regimens incorporating ASP did not exhibit a significant survival advantage than those without ASP. However, patients who received ASP in their first-line chemotherapy exhibited a poorer response to salvage chemotherapy as well as a worse prognosis after relapse compared with those who received ASP-absent first-line chemotherapy.
The first-line treatment of NKTCL has significantly evolved during the last decade. However, the optimal treatment modality after relapse remains poorly defined to date. Due to the rarity of such cases, only retrospective data from two small cohorts are available36,37. RT has been well established as the primary treatment for early stage disease due to the high radiosensitivity of NKTCL5,6,7. Patients with relapsed disease may also benefit from RT. In two previous studies and in the present study, RT at a median dose of 40–50 Gy with or without chemotherapy yielded a 5-year OS of 62.5–83.3% in patients with localized or locoregional relapse36,37. More importantly, our and Zhao’s studies consistently demonstrated that RT with or without chemotherapy produced markedly better survival than chemotherapy alone in patients with locoregional relapse36. In addition, most of those patients receiving re-irradiation in our and Zhao’s cohorts had previously received RT in the first-line treatment, indicating that recurrent NKTCL remains radiosensitive. Considering the radiosensitivity and favorable prognosis, it is reasonable to consider RT at a median dose of 40–50 Gy as an integral part of salvage treatment in patients with locoregionally recurrent NKTCL.
Several studies have investigated the role of HSCT in newly diagnosed or relapsed/refractory NKTCL patients and have reported that AHSCT may be a feasible therapeutic option in selected patients (e.g., in CR before transplant or with advanced stage, poor prognostic index, or high EBV-DNA copy number)17,18,19,20,43. However, those studies have limitations due to their small sample sizes, inconsistent indications for AHSCT, and heterogeneous conditioning regimens. In addition, little evidence is available to demonstrate a definitive survival advantage of HSCT over follow-up after remission. In a relatively large-scale matched controlled analysis, Lee et al. revealed that AHSCT significantly improved disease-specific survival in patients who achieved CR after primary or salvage treatment or in those with a high NKPI score compared with the historical control group who did not received AHSCT17. Similar results were also observed in other smaller cohorts, as reported by Kim et al. and Au et al.19,44. However, the historically matched comparison in those studies may inevitably lead to selection bias. In the present study, the indication and conditioning regimen (CR after salvage chemotherapy and BEAM in 7 of 8 patients) for AHSCT were relatively uniform. In patients with distant relapse who achieved CR/PR after initial salvage chemotherapy, AHSCT as consolidative therapy substantially improved prognosis compared with follow-up. All of the seven patients who received AHSCT survived at a median follow-up of 48.1 months without a second relapse or treatment-related mortality, which was a very encouraging result considering the extensive relapse in those patients. A possible reason for this result is that most of these patients had attained CR before transplantation, which has been reported to be a powerful prognostic factor for better survival after HSCT in previous studies17,19,45,46,47. Additionally, due to the long study period covered in our report, the chemotherapeutic regimens showed a great variety among the patients, including those who received AHSCT. However, the heterogeneous chemotherapy received before AHSCT suggested that the excellent outcome observed in the AHSCT group might be attributed to the transplantation itself, rather than some specific induction chemotherapeutic regimens.
Overexpression of a multidrug-resistant gene was most likely the reason that NKTCL exhibits disappointing responses to anthracycline-based chemotherapeutic regimens (such as CHOP and EPOCH) as first-line treatments9,10,11,12. Asparaginase (L-asparaginase or pegaspargase) exhibits a unique antitumor mechanism via hydrolyzing serum asparagine. NKTCL cells heavily depend on exogenous asparagine and are therefore highly susceptible to asparaginase48. For relapsed or refractory patients, chemotherapeutic regimens without ASP yielded a CR rate of only 13–37% and an ORR rate of 36–52%34,36,49. In Zhang’s study, CHOP or EPOCH regimens failed to improve prognosis in patients with localized relapse and resulted in a dismal survival in disseminated recurrent cases (1-year OS was 0%)37. In contrast, ASP-containing chemotherapy yielded a CR rate of 45–61% and an ORR rate of 70–88% in patients with relapsed or refractory NKTCL13,14,15,33,34,35,50,51. In a study of 42 patients with stage IV, relapsed, or refractory NKTCL, the SMILE (L-asparaginase, methotrexate, ifosfamide, etoposide, and dexamethasone) regimen significantly improved response rates and survival compared with CHOP34. However, salvage chemotherapy with ASP-containing or ASP-absent regimens produced comparable ORR rates and survival in our cohort of relapsed patients, although the ASP-containing regimens were associated with a higher CR rate. Several explanations may account for this discrepancy. First, heterogeneity existed with respect to the chemotherapy regimens used in our cohort. Second, a relatively high proportion (42.9%) of patients in our cohort received consolidative RT or AHSCT after salvage chemotherapy, which may have attenuated the difference in efficacy between those chemotherapeutic regimens. In addition, clinical characteristics also differed between the ASP-containing and ASP-absent groups, with significantly more patients with poor physical status in the ASP-absent group. It is noteworthy that the continuous improvement of first-line chemotherapy over the study period might result in more chemoresistant relapse and confounded the comparison between the ASP-containing and ASP-absent chemotherapy at relapse. However, the first-line chemotherapeutic regimens and response were comparable between the ASP-containing and ASP-absent groups after relapse according to our data. Therefore, we consider the efficacy of first-line chemotherapy might not be a major confounding factor to the comparison between ASP-containing and ASP-absent regimens at relapse. This question remains open, and a prospective study consisting of more patients is required to assess the role of ASP in salvage treatment. Another noteworthy finding in our study was that patients who received ASP-containing chemotherapy as their first-line treatment exhibited a poorer response to salvage chemotherapy and worse prognosis after relapse compared with those who received ASP-absent first-line chemotherapy. This finding indicates that effective first-line therapy may result in more chemoresistant relapsed diseases, and more effective drugs and regimens are required for patients who experience relapse after ASP-containing first-line chemotherapy.
In the present study, chemotherapy as initial salvage treatment for relapsed NKTCL achieved an ORR of 62.5%, but patients receiving chemotherapy alone exhibited a 5-year OS of only 13.3%. Without subsequent consolidative therapy, patients, with either locoregional or distant relapse, who achieved CR/PR after salvage chemotherapy exhibited a survival comparable to those who experienced SD/PD. Therefore, chemotherapy alone is inadequate for relapsed NKTCL, and appropriate consolidative therapies according to the pattern of relapse are indispensable.
Consistent with the prior studies of Zhang et al. and Zhao et al., the overall prognosis of our relapsed cohort remained relatively poor, with a 5-year OS of 41.4% after relapse (40.0% by Zhao et al. and 37.8% by Zhang et al.)36,37. Notably, most of the patients in our study had been heavily treated in the first-line setting, with 91% receiving combined chemotherapy and RT, 72% receiving more than four cycles of chemotherapy, and 75% receiving RT of ≥50 Gy, making salvage treatment after relapse challenging. However, patients who attained CR after salvage treatment (51.8%) were nonetheless able to achieve an encouraging survival rate after relapse (5-year OS of 74.7% in our cohort, and 2-year OS of 86.0% in Zhao’s cohort)36. The plateau observed in survival curves indicated that a proportion of relapsed cases remained potentially curable with appropriate salvage treatment. Other predictors of OS observed in our cohort, including pattern of relapse (LR or DR) and duration of CR, were also been observed by Zhao et al.36.
The limitations of this study are its retrospective nature and the small sample size. Neither the role of consolidative RT in patients with distant relapse nor the role of AHSCT in patients with locoregional relapse could be determined due to the very limited number of cases. Additionally, we were unable to define whether patients who achieved PR following salvage chemotherapy could benefit from AHSCT due to the limited number of patients. Moreover, we could not perform a multivariate analysis to identify independent prognostic factors in this cohort due to the insufficient number of events.
Conclusion
The results of the present retrospective analysis indicate that patients with relapsed NKTCL who respond to initial salvage chemotherapy may benefit from consolidative RT or AHSCT, depending on their pattern of relapse. Incorporating ASP into salvage chemotherapy failed to improve survival after relapse. However, patients who received ASP during their first-line chemotherapy exhibited a poorer response to salvage chemotherapy and worse prognosis after relapse. Patients with relapsed NKTCL were potentially curable with appropriate salvage chemotherapy followed by consolidative treatment, which should be further explored in studies using prospective designs and larger sample sizes.
Additional Information
How to cite this article: Nie, M. et al. Consolidative treatment after salvage chemotherapy improves prognosis in patients with relapsed extranodal natural killer/T-cell lymphoma. Sci. Rep. 6, 23996; doi: 10.1038/srep23996 (2016).
References
Chim, C. S. et al. Primary nasal natural killer cell lymphoma: long-term treatment outcome and relationship with the International Prognostic Index. Blood 103, 216–221 (2004).
Vose, J., Armitage, J. & Weisenburger, D. International T. Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J. Clin. Oncol. 26, 4124–4130 (2008).
Chan, J., Quintanilla-Martinez, L., Ferry, J. & Peh, S. C. Extranodal NK/T-cell lymphoma, nasal type in WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (eds Swerdlow, S. H. et al.) 285–288 (IARC, 2008).
Chan, J., Jaffe, E. & Ralfkiaer, E. Extranodal NK/T-cell lymphoma, nasal type in WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (eds Jaffe, E. S., Harris, N. L., Stein, H. & Vardiman, J. W. ) 204–207 (IARC, 2001).
Li, Y. X. et al. Radiotherapy as primary treatment for stage IE and IIE nasal natural killer/T-cell lymphoma. J. Clin. Oncol. 24, 181–189 (2006).
Li, Y. X. et al. Radiotherapy alone with curative intent in patients with stage I extranodal nasal-type NK/T-cell lymphoma. Int. J. Radiat. Oncol. Biol. Phys. 82, 1809–1815 (2012).
Bi, X. W. et al. High-dose and extended-field intensity modulated radiation therapy for early-stage NK/T-cell lymphoma of Waldeyer’s ring: dosimetric analysis and clinical outcome. Int. J. Radiat. Oncol. Biol. Phys. 87, 1086–1093 (2013).
Bi, X. W. et al. Treatment outcome of patients with advanced stage natural killer/T-cell lymphoma: elucidating the effects of asparaginase and postchemotherapeutic radiotherapy. Ann. Hematol. 94, 1175–1184 (2015).
Wang, B. et al. Immunohistochemical expression and clinical significance of P-glycoprotein in previously untreated extranodal NK/T-cell lymphoma, nasal type. Am. J. Hematol. 83, 795–799 (2008).
Kim, B. S. et al. Therapeutic outcome of extranodal NK/T-cell lymphoma initially treated with chemotherapy--result of chemotherapy in NK/T-cell lymphoma. Acta Oncol. 42, 779–783 (2003).
Kim, G. E. et al. Combined chemotherapy and radiation versus radiation alone in the management of localized angiocentric lymphoma of the head and neck. Radiother. Oncol. 61, 261–269 (2001).
Wang, L., Xia, Z. J., Huang, H. Q., Lu, Y. & Zhang, Y. J. Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) in the treatment of stage IE/IIE extranodal natural killer/T cell lymphoma, nasal type: 13-year follow-up in 135 patients. Int. J. Hematol. 96, 617–623 (2012).
Yamaguchi, M. et al. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-Cell Tumor Study Group study. J. Clin. Oncol. 29, 4410–4416 (2011).
Kwong, Y. L. et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood 120, 2973–2980 (2012).
Jaccard, A. et al. Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a phase 2 study. Blood 117, 1834–1839 (2011).
Bi, X. W. et al. Radiotherapy and PGEMOX/GELOX regimen improved prognosis in elderly patients with early-stage extranodal NK/T-cell lymphoma. Ann. Hematol. 94, 1525–1533 (2015).
Lee, J. et al. Autologous hematopoietic stem cell transplantation in extranodal natural killer/T cell lymphoma: a multinational, multicenter, matched controlled study. Biol. Blood Marrow Transplant. 14, 1356–1364 (2008).
Yhim, H. Y. et al. Clinical outcomes and prognostic factors of up-front autologous stem cell transplantation in patients with extranodal natural killer/T cell lymphoma. Biol. Blood Marrow Transplant. 21, 1597–1604 (2015).
Kim, H. J. et al. High-dose chemotherapy with autologous stem cell transplantation in extranodal NK/T-cell lymphoma: a retrospective comparison with non-transplantation cases. Bone Marrow Transplant. 37, 819–824 (2006).
Fox, C. P. et al. High-dose therapy and autologous stem cell transplantation for extra-nodal NK/T lymphoma in Western patients; a study from the European Society for Blood and Marrow Transplantation. Leuk. Lymphoma 26, 1–6 (2015).
Ennishi, D. et al. Allogeneic hematopoietic stem cell transplantation for advanced extranodal natural killer/T-cell lymphoma, nasal type. Leuk. Lymphoma 52, 1255–1261 (2011).
Tse, E. et al. Allogeneic haematopoietic SCT for natural killer/T-cell lymphoma: a multicentre analysis from the Asia Lymphoma Study Group. Bone Marrow Transplant. 49, 902–906 (2014).
Koom, W. S. et al. Angiocentric T-cell and NK/T-cell lymphomas: radiotherapeutic viewpoints. Int. J. Radiat. Oncol. Biol. Phys. 59, 1127–1137 (2004).
Kim, M. et al. Ifosfamide, methotrexate, etoposide, and prednisolone (IMEP) plus L-asparaginase as a first-line therapy improves outcomes in stage III/IV NK/T cell-lymphoma, nasal type (NTCL). Ann. Hematol. 94, 437–444 (2015).
Suzuki, R. et al. Prognostic factors for mature natural killer (NK) cell neoplasms: aggressive NK cell leukemia and extranodal NK cell lymphoma, nasal type. Ann. Oncol. 21, 1032–1040 (2010).
Kim, T. M. et al. Local tumor invasiveness is more predictive of survival than International Prognostic Index in stage I(E)/II(E) extranodal NK/T-cell lymphoma, nasal type. Blood 106, 3785–3790 (2005).
Yong, W. et al. L-asparaginase-based regimen in the treatment of refractory midline nasal/nasal-type T/NK-cell lymphoma. Int. J. Hematol. 78, 163–167 (2003).
Lee, J. et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J. Clin. Oncol. 24, 612–618 (2006).
Cheung, M. M., Chan, J. K., Lau, W. H., Ngan, R. K. & Foo, W. W. Early stage nasal NK/T-cell lymphoma: clinical outcome, prognostic factors, and the effect of treatment modality. Int. J. Radiat. Oncol. Biol. Phys. 54, 182–190 (2002).
Tham, I. W., Lee, K. M., Yap, S. P. & Loong, S. L. Outcome of patients with nasal natural killer (NK)/T-cell lymphoma treated with radiotherapy, with or without chemotherapy. Head Neck 28, 126–134 (2006).
Huang, M. J. et al. Early or up-front radiotherapy improved survival of localized extranodal NK/T-cell lymphoma, nasal-type in the upper aerodigestive tract. Int. J. Radiat. Oncol. Biol. Phys. 70, 166–174 (2008).
Ahn, H. K. et al. Gemcitabine alone and/or containing chemotherapy is efficient in refractory or relapsed NK/T-cell lymphoma. Invest. New Drugs 31, 469–472 (2013).
Ji, J. et al. A study of gemcitabine, l-asparaginase, ifosfamide, dexamethasone and etoposide chemotherapy for newly diagnosed stage IV, relapsed or refractory extranodal natural killer/T-cell lymphoma, nasal type. Leuk. Lymphoma 55, 2955–2957 (2014).
Yang, L. et al. Retrospective study of modified SMILE chemotherapy for advanced-stage, relapsed, or refractory extranodal natural killer (NK)/T cell lymphoma, nasal type. Med. Oncol. 30, 720 (2013).
Yong, W. et al. L-asparaginase in the treatment of refractory and relapsed extranodal NK/T-cell lymphoma, nasal type. Ann. Hematol. 88, 647–652 (2009).
Zhao, T. et al. Survival benefit with salvage radiotherapy for patients with locoregionally recurrent extranodal NK/T cell lymphoma, nasal type. Ann. Hematol. 92, 325–332 (2013).
Zhang, X. X. et al. Salvage treatment improved survival of patients with relapsed extranodal natural killer/t-cell lymphoma, nasal type. Int. J. Radiat. Oncol. Biol. Phys. 74, 747–752 (2009).
Cheson, B. D. et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J. Clin. Oncol. 17, 1244 (1999).
Cheson, B. D. et al. Revised response criteria for malignant lymphoma. J. Clin. Oncol. 25, 579–586 (2007).
Shipp, M. A. et al. A predictive model for aggressive non-Hodgkin’s lymphoma: The International Non-Hodgkin’s Lymphoma Prognostic Factors Project. N. Engl. J. Med. 329, 987–994 (1993).
Kim, T. M. et al. Clinical heterogeneity of extranodal NK/T-cell lymphoma, nasal type: a national survey of the Korean Cancer Study Group. Ann. Oncol. 19, 1477–1484 (2008).
van Domburg, R., Hoeks, S., Kardys, I., Lenzen, M. & Boersma, E. Tools and techniques--statistics: how many variables are allowed in the logistic and Cox regression models? EuroIntervention 9, 1472–1473 (2014).
Kim, S. J. et al. Risk stratification on the basis of Deauville score on PET-CT and the presence of Epstein-Barr virus DNA after completion of primary treatment for extranodal natural killer/T-cell lymphoma, nasal type: a multicentre, retrospective analysis. Lancet Haematol. 2, e66–74 (2015).
Au, W. Y. et al. Autologous stem cell transplantation for nasal NK/T-cell lymphoma: a progress report on its value. Ann. Oncol. 14, 1673–1676 (2003).
Rodriguez, J. et al. High dose chemotherapy and autologous stem cell transplantation in patients with peripheral T-cell lymphoma not achieving complete response after induction chemotherapy. The GEL-TAMO experience. Haematologica 88, 1372–1377 (2003).
Corradini, P. et al. Long-term follow-up of patients with peripheral T-cell lymphomas treated up-front with high-dose chemotherapy followed by autologous stem cell transplantation. Leukemia 20, 1533–1538 (2006).
Chen, A. I., McMillan, A., Negrin, R. S., Horning, S. J. & Laport, G. G. Long-term results of autologous hematopoietic cell transplantation for peripheral T cell lymphoma: the Stanford experience. Biol. Blood Marrow Transplant. 14, 741–747 (2008).
Ando, M. et al. Selective apoptosis of natural killer-cell tumours by l-asparaginase. Br. J. Haematol. 130, 860–868 (2005).
Kim, B. S. et al. Effective second-line chemotherapy for extranodal NK/T-cell lymphoma consisting of etoposide, ifosfamide, methotrexate, and prednisolone. Ann. Oncol. 20, 121–128 (2009).
Ding, H. et al. High-dose methotrexate, etoposide, dexamethasone and pegaspargase (MEDA) combination chemotherapy is effective for advanced and relapsed/refractory extranodal natural killer/T cell lymphoma: a retrospective study. Int. J. Hematol. 102, 101–107 (2015).
Zhou, Z. et al. Effectiveness of gemcitabine, pegaspargase, cisplatin, and dexamethasone (DDGP) combination chemotherapy in the treatment of relapsed/refractory extranodal NK/T cell lymphoma: a retrospective study of 17 patients. Ann. Hematol. 93, 1889–1894 (2014).
Acknowledgements
This work was supported by National Natural Science Foundation of China (No. 81071950, 81301903).
Author information
Authors and Affiliations
Contributions
Z.M.L. is the guarantor of the manuscript and contributed to the concept and design. M.N., X.W.B., W.W.Z., P.S., Y.X., P.P.L., H.Q.H. and W.Q.J. performed clinical data collection and patient’s follow-up. M.N., X.W.B. & W.W.Z. contributed to analysis and interpretation of the data and the drafting and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Nie, M., Bi, Xw., Zhang, Ww. et al. Consolidative treatment after salvage chemotherapy improves prognosis in patients with relapsed extranodal natural killer/T-cell lymphoma. Sci Rep 6, 23996 (2016). https://doi.org/10.1038/srep23996
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23996
This article is cited by
-
Inhibition of extranodal NK/T-cell lymphoma by Chiauranib through an AIF-dependent pathway and its synergy with L-asparaginase
Cell Death & Disease (2023)
-
“Sandwich” protocol based on modified SMILE regimen for children with newly extranodal NK/T cell lymphoma, nasal type: a single-arm, single-center clinical study
Annals of Hematology (2023)
-
PD-L1 is upregulated by EBV-driven LMP1 through NF-κB pathway and correlates with poor prognosis in natural killer/T-cell lymphoma
Journal of Hematology & Oncology (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.