Abstract
This study was aimed to investigate the prognostic value of neutrophil-to-lymphocyte ratio (NLR) in patients with prostate cancer (PCa). A meta-analysis including 14 publications (15 cohorts) with 16,266 patients was performed to evaluate the association between NLR and overall survival (OS), progression-free survival (PFS)/recurrence-free survival (RFS) in PCa using hazard ratio (HR) and 95% confidence intervals (95% CI). The combining data showed that increased NLR predict poor OS (HR = 1.38, 95%CI: 1.22–1.56) and PFS/RFS (HR = 1.24, 95%CI 1.05–1.46) in PCa. Stratified analysis by PCa type, sample size, ethnicity and NLR cut-off value revealed that NLR showed consistent prognostic value in metastatic castration-resistant prostate cancer (mCRPC) patients and predict poor PFS/RFS in Asians, but not in Caucasians. These statistical data suggested that increased NLR could predict poor prognosis in patients with PCa.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most frequently diagnosed cancer and the second leading cause of cancer-related death among men in the western world, accounting for 220,800 new cases and 27,540 deaths in the US annually1. The incidence of prostate cancer varies remarkably in different countries and regions, which increased significantly during the past few decades due to diverse approaches diagnosing PCa. Despite different treatment methods including radical prostatectomy, hormone deprivation therapy, radiation therapy and chemotherapy were applied, most tumors relapse in 2 years to the castration-resistant state and the prognosis of PCa remains disappointing2. Given this, it is of interest for clinicians to stratify the high risk PCa patients who are prone to tumor recurrence and poor prognosis so that clinicians could further identify optimal treatment strategies3.
Accumulating evidence has shown that inflammation response is closely associated with tumorigenesis and tumor progression4,5. The interactions between tumor and inflammation were complex and involved different mechanisms. Inflammation plays an important role in every single step in carcinogenesis, involving tumor initiation, angiogenesis promotion, apoptosis inhibition and tumor metastasis6. The changes in systemic inflammatory response can be reflected by measurement of various blood-based parameters. A variety of blood-based indexes including C-reactive protein (CRP), modified Glasgow Prognostic Score (mGPS), platelets count and neutrophil-to-lymphocyte ratio (NLR) have been extensively explored to predict prognosis of cancer patients7,8,9. A large amount of studies have reported that elevation of NLR was associated with poor clinical outcomes in various malignant tumors10,11. In recent years, several studies have reported that an elevation in NLR correlated with biological tumor recurrence and poor prognosis in patients with PCa12,13,14. However, some other studies did not detect the prognostic significance of NLR in PCa patients15,16. Therefore, it is necessary to systematically clarify the prognostic significance of NLR in PCa by the approach of meta-analysis.
The current study was designed to evaluate the prognostic value of elevated NLR for overall survival (OS) and progress-free survival (PFS)/recurrence-free survival (RFS) in patients with PCa by pooling results from published data.
Results
Selection and characteristics of included eligible studies
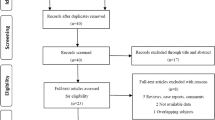
The selection process was shown in Fig. 1. Through initial searching of the database, 197 records were retrieved and screened by title and abstract. 174 records were discarded after title and abstracts screening because they were duplicate records, reviews, irrelevant studies and nonhuman studies. 23 full-text records were further evaluated for eligibility. Of them, nine studies were eliminated due to following reasons: five did not provide the survival information, three provided insufficient data to calculate HR and 95%CI, one was a comment. Soest et al.17 included two independent randomized phase III trials in their paper, we marked the cohorts as Soest1 and Soest2. Finally, 14 publications12,13,14,15,16,17,18,19,20,21,22,23,24,25 (15 cohorts) with 16,266 patients published between 2012 and 2015 were included in the meta-analysis process. The basic information of the included studies was summarized in Table 1. 11 studies (12 cohorts)12,13,14,15,16,17,19,20,21,23,24 were from western countries, 3 studies18,22,25 were from Asian countries. Of the 14 studies (15 cohorts), 10 studies (11 cohorts)12,13,14,15,16,17,18,19,21,24 investigated the prognostic role of NLR on OS, 9 studies14,18,19,20,21,22,23,24,25 investigated prognostic role of NLR on PFS/RFS.
NLR and OS in PCa
11 cohorts with 14,250 patients provided the data of NLR and OS in PCa. The pooled HR of 1.38 (95%CI: 1.22–1.56) with heterogeneity (Ph = 0.002, I2 = 64.1%) showed elevated NLR predicted shorter OS in patients with PCa (Fig. 2, Table 2).
NLR and PFS/RFS in PCa
9 cohorts with 12541 patients presented the data of pretreatment NLR and PFS/RFS in PCa. Though with heterogeneity (Ph = 0.003, I2 = 65.3%), a significant correlation between increased NLR and poor PFS/RFS (HR = 1.24, 95%CI: 1.05–1.46) was detected according to our pooled data (Fig. 3, Table 2). Interestingly, increased NLR predicted shorter RFS/PFS in Asian populations (HR = 1.42, 95%CI: 1.11–1.82), but not in Caucasian populations (HR = 1.18, 95%CI: 0.98–1.43).
Subgroup analysis and meta-regression
Subgroup analysis and meta-regression were carried out to investigate the sources of heterogeneity. With respect to the correlation between NLR and OS, subgroup analysis stratified by PCa types showed that the combined HRs were 1.44 (95%CI: 1.32–1.57) for metastatic castration-resistant prostate cancer (mCRPC) and 1.16 (95%CI: 0.98–1.36) for localized PCa. Subgroup analysis dichotomized by sample size(>400 vs. <400) and NLR cut-off value (≤3 vs. >3) did not change the results substantially(Table 2). Meta-regression showed PCa types could be the potential source of heterogeneity (p = 0.01). With regard to the correlation between NLR and PFS/RFS, subgroup analysis showed similar results with total results. Notably, the pooled HR for Asian ethnicity was 1.42 (95%CI: 1.11–1.82) without significant heterogeneity (Ph = 0.345, I2 = 6%). In addition, the pooled HR for mCRPC was 1.45 (95%CI: 1.19–1.77) with good homogeneity (Ph = 0.37, I2 = 0) (Table 2).
Sensitivity analysis
Omitting any single study by turn, sensitivity analysis demonstrated that the combined HRs for OS and PFS/RFS did not significantly alter (Fig. 4).
Publication bias
Evaluation of publication bias using Begg’s test (p < 0.05 was considered as statistical significant) demonstrated that there was no significant publication bias in OS and PFS/RFS studies (p = 0.119 and p = 0.251, respectively)(Fig. 5).
Discussion
In the present study, we aimed to explore the prognostic value of NLR in patients with PCa. A total of 14 studies (15 cohorts) containing 16,266 patients were included in this meta-analysis to calculate pooled HR. The results showed that increased pretreatment NLR was associated with poor OS(HR = 1.38, 95%CI: 1.22–1.56) and PFS/RFS (HR = 1.24, 95%CI: 1.05–1.46), though with heterogeneity. Subgroup analysis divided by ethnicity, PCa type, sample sizes and NLR cut-off value did not significantly change the main results. Of note, subgroup analysis demonstrated that pretreatment NLR had enhanced prognostic efficiency for OS and PFS/RFS in mCRPC (HR = 1.44, 95%CI: 1.32–1.57 for OS and HR = 1.45,95%CI: 1.19–1.77 for RFS/PFS) without significant heterogeneity. In addition, elevated NLR also predicted poor PFS/RFS in Asian populations, but not in Caucasian population. To our knowledge, our study is the first meta-analysis exploring the prognostic effects of increased NLR in OS and PFS/RFS in patients with PCa.
Growing evidence has indicated that inflammatory response could be heavily involved in the occurrence and development of different cancer types26,27,28. Studies revealed that inflammation-related neutrophils and immunocytes including lymphocytes were indispensable participants in tumorigenesis29. Inflammation exerts an important role in tumor formation and development through facilitating angiogenesis, proliferation and protecting tumors from apoptosis. By secreting a variety of chemokines, tumor cells could attract pro-inflammatory cells into tumor microenvironment, subsequently, an array of cytokines produced by neutrophils stimulate tumor cells growth30. Of these inflammatory parameters reflecting the systemic inflammatory response, an increased neutrophil-to-lymphocyte ratio (NLR) has been found valuable to predict clinical outcome of cancer patients31. Additionally, NLR is obtained from routine blood test, making it an easily available and reliable marker. A large amount of studies have showed the correlation between increased pretreatment NLR and poor prognosis in different malignant tumors including gastric cancer, colorectal cancer, breast cancer, prostate cancer, soft-tissue sarcoma and non-small cell lung cancer17,27,32,33,34,35.
Our results demonstrated that elevated NLR was in associated poor OS and PFS/RFS in patients with PCa, which was in accordance with the results from meta-analysis with other cancer types34,36,37. We have noted that a recently published work investigated the prognostic value of NLR in various solid tumors11. However, in that meta-analysis11, only three studies concerning patients with castration resistant prostate cancer were included. In the present work, we included patients with both localized PCa and mCRPC in an adequately sufficient data. Moreover, subgroup analysis was performed, which could provide detailed information for clinical management. More importantly, we found that NLR has adequate prognostic value for OS and PFS/RFS in mCRPC. Although chemotherapy and hormone therapy were used, mCRPC commonly occurred after the treatment after few years. Therefore, the NLR measurement could provide valuable prognostic information for mCRPC and be helpful for optimal treatment strategies selection. In addition, our results showed increased NLR predicted poor PFS/RFS in Asians, but not in Caucasians, which could be attributed to the ethnicity heterogeneity. Notably, corticosteroids were one of the palliative treatment options in patients with mCRPC for 30 years38. Intake of corticosteroids had immunosuppressive effects, which could influence the value of NLR21. The prognostic value of NLR in PCa should be evaluated after adjustment on potential confounders including use of corticosteroids. However, only one21 of the included studies provided the relevant data, thus the analysis could not be conducted in the current meta-analysis due to insufficient data. Interestingly, Lorente et al.21 found that NLR had independent prognostic value on OS regardless of corticosteroids usage using multivariable analysis. However, a recent work39 found that, in patients with melanoma, elevated NLR and corticosteroids before week 1 were associated with poorer OS in univariate analysis, however, in multivariate analysis, elevated NLR remained an independent prognostic factor whereas the prognostic efficiency of intake of corticosteroids disappeared. Since corticosteroids were widely used drugs in mCRPC treatment, further studies should take into account intake of corticosteroids when performing survival analysis. Furthermore, more large scale studies are needed to explore the effects of use of corticosteroids on survival.
Although our study was the first meta-analysis concerning NLR in PCa prognostication, there were several limitations need to be addressed. First, vast majority of included publications employed samples of Caucasian ethnicity, thus the evaluation of OS and RFS/PFS in Asians might be derived by chance because of sample insufficiency. Second, Shafique et al.16 recruited all types of PCa patients that could not be classified as any PCa types, which may contribute to heterogeneity when subgroup analysis and meta-regression were performed. Third, only publications in English were included, which could cause language bias for selection. Further investigations are needed to address the above-mentioned shortcomings.
In summary, our study demonstrated that elevated NLR predict poor OS and PFS/RFS in patients with PCa. Increased NLR showed consistent prognostic value in mCRPC patients and predict poor PFS/RFS in Asians, but not in Caucasians. The present findings could provide implications for clinical management of patients with PCa and further investigations involving large sample size and more ethnic backgrounds are needed.
Methods
Literature search
A comprehensive literature searching of Pubmed, Embase and Web of Science database was conducted. The search strategy included the combinations of the following key words: (NLR OR neutrophil-lymphocyte ratio OR neutrophil-to-lymphocyte ratio) AND (prostate cancer OR prostate carcinoma OR prostatic neoplasms OR PCa) AND (prognosis OR survival OR outcome OR recurrence). The last search was updated on October 17th, 2015. We also manually checked the reference list to identify additional publications. The published language was limited to English.
Inclusion and exclusion criteria
Inclusion criteria for publication selection were as follows: (i) the diagnosis of PCa for patients was histopathologically confirmed; (ii) the value of NLR was obtained for blood sample testing; (iii) investigated the association of NLR with PFS, RFS or OS; (iv) provided HRs and 95% CIs for NLR in OS and (or) PFS/RFS, or HRs and 95%CIs could be calculated according to the raw data provided in the article; (v) defined the cut-off value of increased NLR; (vi) published in English language.
Major exclusion criteria were as follows: (i) letters, editorials, review articles; (ii) failed to provide data of interest or insufficient data to estimate HRs and 95%CIs; (iii) failed to identify the cut-off value for elevated NLR; (iv) animal studies and irrelevant studies.
Data extraction
Two investigators (XB,G and XS,G) independently gathered information from each eligible study. The following data was extracted: surname of the first author, study country, year of publication, ethnic origin of the subjects, sample size, subtype of PCa, treatment method, cut-off value defining elevated NLR and HRs with corresponding 95% CIs for PFS/RFS and(or) OS. Discrepancies between the two investigators were settled by discussion.
Statistical analysis
The HR and the corresponding 95%CI were used to assess the prognostic efficiency of NLR on PCa. HR and 95% CI were directly extracted from each single study, if provided, or calculated according to the methods clarified by Tierney40 et al. Cochran’s Q test and Higgins I-squared statistic were applied to test the heterogeneity of pooled data. I2 > 50% and p < 0.1 indicated significant heterogeneity and random-effects model was adopted to combine the effective value. I2 < 50% and p > 0.1 were considered as no heterogeneity and a fixed-effects model was then adopted. Sources of inter-study heterogeneity were explored using subgroup analysis and meta-regression. Begg’s funnel plot was used to evaluate publication bias. Sensitivity analyses were carried out to access the robustness of the results. All p values were two-tailed and statistical significance level was set at p < 0.05. All statistical analyses were conducted using STATA 12.0 software (STATA Corporation, College Station, TX).
Additional Information
How to cite this article: Gu, X. et al. Prognostic significance of neutrophil-to-lymphocyte ratio in prostate cancer: evidence from 16,266 patients. Sci. Rep. 6, 22089; doi: 10.1038/srep22089 (2016).
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer Statistics, 2015. CA-Cancer J. Clin. 65, 5–29 (2015).
Damber, J. E. & Aus, G. Prostate cancer. Lancet. 371, 1710–1721 (2008).
Fung, C., Dale, W. & Mohile, S. G. Prostate Cancer in the Elderly Patient. J. Clin. Oncol. 32, 2523–2530 (2014).
Gregory, A. D. & Houghton, A. M. Tumor-associated neutrophils: new targets for cancer therapy. Cancer Res. 71, 2411–2416 (2011).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell. 144, 646–674 (2011).
Grivennikov, S. I., Greten, F. R. & Karin, M. Immunity, Inflammation and Cancer. Cell. 140, 883–899 (2010).
Hashimoto, K. et al. The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 103, 1856–1864 (2005).
Gu, L. et al. The association of platelet count with clinicopathological significance and prognosis in renal cell carcinoma: a systematic review and meta-analysis. PloS one 10, e0125538, 10.1371/journal.pone.0125538 (2015).
Duan, H. et al. Prognostic role of neutrophil-lymphocyte ratio in operable esophageal squamous cell carcinoma. World J Gastroenterol. 21, 5591–5597 (2015).
Cannon, N. A. et al. Neutrophil-Lymphocyte and Platelet-Lymphocyte Ratios as Prognostic Factors after Stereotactic Radiation Therapy for Early-Stage Non-Small-Cell Lung Cancer. J. Thorac. Oncol. 10, 280–285 (2015).
Templeton, A. J. et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 106, dju124, 10.1093/jnci/dju124 (2014).
Nuhn, P. et al. Association of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxel. BJU Int. 114, E11–E17 (2014).
Templeton, A. J. et al. Simple Prognostic Score for Metastatic Castration-Resistant Prostate Cancer With Incorporation of Neutrophil-to-Lymphocyte Ratio. Cancer 120, 3346–3352 (2014).
Langsenlehner, T. et al. Validation of the neutrophil-to-lymphocyte ratio as a prognostic factor in a cohort of European prostate cancer patients. World J Urol, 33, 1661–1667 (2015).
Linton, A. et al. Glasgow prognostic score as a prognostic factor in metastatic castration-resistant prostate cancer treated with docetaxel-based chemotherapy. Clin Genitourin Cancer. 11, 423–430 (2013).
Shafique, K. et al. Systemic inflammation and survival of patients with prostate cancer: evidence from the Glasgow Inflammation Outcome Study. Prostate Cancer Prostatic Dis. 15, 195–201 (2012).
van Soest, R. J. et al. Neutrophil-to-lymphocyte ratio as a prognostic biomarker for men with metastatic castration-resistant prostate cancer receiving first-line chemotherapy: data from two randomized phase III trials. Ann Oncol. 26, 743–749 (2015).
Yao, A. et al. High neutrophil-to-lymphocyte ratio predicts poor clinical outcome in patients with castration-resistant prostate cancer treated with docetaxel chemotherapy. Int J Urol. 22, 827–833 (2015).
Sharma, V. et al. The association of preoperative neutrophil to lymphocyte ratio with oncologic outcomes following radical prostatectomy for prostate cancer. J Urol. 193, e55–e56 (2015).
Poyet, C. et al. Pretreatment systemic inflamatory response parameters do not predict the outcome in men with prostate cancer undergoing radical prostatectomy. J Urol. 193, e817 (2015).
Lorente, D. et al. Baseline neutrophil-lymphocyte ratio (NLR) is associated with survival and response to treatment with second-line chemotherapy for advanced prostate cancer independent of baseline steroid use. Ann Oncol. 26, 750–755 (2015).
Lee, H. et al. High preoperative neutrophil-lymphocyte ratio predicts biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. World J Urol. 10.1007/s00345-015-1701-6 (2015).
Kwon, Y. S. et al. Neutrophil and Lymphocyte Counts as Clinical Markers for Stratifying Low-Risk Prostate Cancer. Clin Genitourin Cancer, 10.1016/j.clgc.2015.07.018 (2015).
Bahig, H. et al. Neutrophil count is associated with survival in localized prostate cancer. BMC Cancer 15, 594, 10.1186/s12885-015-1599-9 (2015).
Sumbul, A. T. et al. Neutrophil-to-lymphocyte ratio predicts PSA response, but not outcomes in patients with castration-resistant prostate cancer treated with docetaxel. Int Urol Nephrol. 46, 1531–1535 (2014).
Proctor, M. J. et al. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer 107, 695–699 (2012).
Cho, I. R. et al. Pre-treatment neutrophil to lymphocyte ratio as a prognostic marker to predict chemotherapeutic response and survival outcomes in metastatic advanced gastric cancer. Gastric Cancer. 17, 703–710 (2014).
Xiao, W. K. et al. Prognostic significance of neutrophil-lymphocyte ratio in hepatocellular carcinoma: a meta-analysis. BMC Cancer 14, 10, 10.1186/1471-2407-14-117 (2014).
Coussens, L. M. & Werb, Z. Inflammation and cancer. Nature 420, 860–867 (2002).
Koizumi, K., Hojo, S., Akashi, T., Yasumoto, K. & Saiki, I. Chemokine receptors in cancer metastasis and cancer cell-derived chemokines in host immune response. Cancer Sci. 98, 1652–1658 (2007).
Roxburgh, C. S. & McMillan, D. C. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 6, 149–163 (2010).
Koh, C. H. et al. Utility of pre-treatment neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as prognostic factors in breast cancer. Br. J. Cancer 113, 150–158 (2015).
Li, M. X. et al. Prognostic role of neutrophil- to- lymphocyte ratio in colorectal cancer: A systematic review and meta-analysis. Int J Cancer. 134, 2403–2413 (2014).
Gu, X. B., Tian, T., Tian, X. J. & Zhang, X. J. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysis. Sci Rep. 5, 12493, 10.1038/srep12493 (2015).
Szkandera, J. et al. Elevated preoperative neutrophil/lymphocyte ratio is associated with poor prognosis in soft-tissue sarcoma patients. Br J Cancer. 108, 1677–1683 (2013).
Hu, K., Lou, L., Ye, J. & Zhang, S. Prognostic role of the neutrophil-lymphocyte ratio in renal cell carcinoma: a meta-analysis. BMJ open 5, e006404, 10.1136/bmjopen-2014-006404 (2015).
Wei, Y., Jiang, Y. Z. & Qian, W. H. Prognostic role of NLR in urinary cancers: a meta-analysis. PloS one 9, e92079, 10.1371/journal.pone.0092079 (2014).
Ndibe, C., Wang, C. G. & Sonpavde, G. Corticosteroids in the Management of Prostate Cancer: A Critical Review. Curr Treat Options Oncol. 16, 6, 10.1007/s11864-014-0320-6 (2015).
Zaragoza, J. et al. Neutrophil to lymphocyte ratio measured before starting ipilimumab treatment is associated with reduced overall survival in patients with melanoma. Br J Dermatol, 10.1111/bjd.14155 (2015).
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S. & Sydes, M. R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8, 16, 10.1186/1745-6215-8-16 (2007).
Acknowledgements
This study was supported by Special fund for “Capital clinically characteristic applied research” of Beijing Municipal Science & Technology Commission (Grant No. Z141107002514160).
Author information
Authors and Affiliations
Contributions
X.B.G., X.S.G., M.W.M. and S.B.Q. defined the research theme. X.B.G., X.S.G., X.Y.L., X.Q. and H.Y. wrote and revised the main manuscript text; S.Q.S., D.Z. and W.W. prepared all the figures. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Gu, X., Gao, X., Li, X. et al. Prognostic significance of neutrophil-to-lymphocyte ratio in prostate cancer: evidence from 16,266 patients. Sci Rep 6, 22089 (2016). https://doi.org/10.1038/srep22089
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep22089
This article is cited by
-
The evolution and heterogeneity of neutrophils in cancers: origins, subsets, functions, orchestrations and clinical applications
Molecular Cancer (2023)
-
Correlation between preoperative peripheral blood NLR, PLR, LMR and prognosis of patients with head and neck squamous cell carcinoma
BMC Cancer (2023)
-
Interplay between tumor-derived factors and tumor-associated neutrophils: opportunities for therapeutic interventions in cancer
Clinical and Translational Oncology (2023)
-
The prognostic value of neutrophil-to-lymphocyte ratio in cholangiocarcinoma: a systematic review and meta-analysis
Scientific Reports (2022)
-
Neutrophils as potential therapeutic targets in hepatocellular carcinoma
Nature Reviews Gastroenterology & Hepatology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.