Abstract
The impact and management of microscopically positive margins in gastrointestinal stromal tumors (GISTs) remain unclear. The aim of this study is to estimate the prognostic value of surgical margins for disease-free survival (DFS) and overall survival (OS) in patients with primary GISTs. Twelve studies with 1985 GIST patients were included. The overall recurrence rate in R1 resection and R0 resection group was 0.364 (95% CI 0.299–0.429) and 0.296 (95% CI 0.161–0.430), respectively. Meta-analysis confirmed that a microscopically positive margin could significantly impact the disease-free survival (HR 1.596, 95% CI 1.128–2.258; I2 = 37.5%, P value = 0.091), but had no influence on overall survival (HR 1.430, 95% CI 0.608–3.363; I2 = 60.8%, P value = 0.013). Importantly, subgroup analysis revealed that adjuvant imatinib treatment could attenuate the risk of recurrence for primary GIST patients who received R1 resection. (HR 1.308, 95% CI 0.583–2.935; I2 = 53.2%, P value = 0.074). The level of evidence achieved in this study was “moderate” for DFS and “low” for OS. In conclusion, this study revealed that a microscopically positive margin is an unfavorable prognostic factor for GIST patients with R1 resection and adjuvant imatinib treatment is proved to be effective.
Similar content being viewed by others
Introduction
Gastrointestinal stromal tumors (GISTs) are the most common of the mesenchymal tumors, which probably arise from the interstitial cells of Cajal1. One of the most prominent characteristics of GISTs is the malignant potential that ranges from a benign behavior to aggressive sarcomas. To evaluate the malignant potential of GISTs, some criteria were established as determined by tumor size, location and number of mitoses, such as NIH criteria2, modified NIH criteria3 and AFIP criteria4. However, increasing evidence show that some other factors, for example sex5, genotype6,7, immune infiltrates8, as well as positive surgical margins9,10, could play an important role in the prognosis of GISTs.
It is a general consensus that surgical excision is the definitive treatment for primary GISTs without peritoneal seeding or metastasis. The goal of surgical treatment is complete gross resection with an intact pseudocapsule and negative microscopic margins (R0), according to the ESMO (European Society for Medical Oncology) and NCCN (National Comprehensive Cancer Network) guidelines11,12. Notably, apart from three central parameters (tumor size, number of mitosis and tumor location), two additional prognostic factors (surgical margins and tumor rupture) were added in the 2012 edition of ESMO guideline13. However, surgical margins were removed in the 2014 edition11, on the basis of some emerging evidence. In a prospective randomized series, the majority of patients with an R1 resection did not experience a recurrence in absence of tumor rupture and there was no statistically significant difference in recurrence rate compared with R0 resection14. Therefore, given that GISTs often abut some vital structures such as gastroesophageal junction, duodenal papilla as well as retroperitoneal vessels, R1 margins are acceptable especially for low-risk lesions when R0 resection might imply major functional sequelae11,14. However, other reports support positive microscopic margins (R1) as a main prognostic factor of tumor recurrence15,16.
These controversial results present challenges to the therapeutic strategies after R1 surgery. The management of R1 resection still remains undefined. The NCCN guideline reported no evidence of a need for re-excision, while the ESMO guideline suggested that re-excision may be an option on the condition that the original site of margins can be found and major functional sequelae are not foreseen. Therefore, it is necessary to perform a systematic and comprehensive meta-analysis to validate the prognostic value of surgical margins and the clinical impact of R1 resection.
In this study, we sought to conduct a meta-analysis to estimate the prognostic value of surgical margins for disease-free survival (DFS) and overall survival (OS) in patients with primary GISTs. In addition, we also comprehensively appraised the quality of evidence and recommended the evidence with Grading of Recommendations Assessment, Development and Evaluation (GRADE) to facilitate clinical decision-making.
Results
Study selection and characteristics
The initial and updated searches together identified 427 records. Upon further review, 19 articles evaluating the prognostic value of surgical margins in patients with primary GISTs were considered eligible. Of the 19 articles, 2 were excluded due to the insufficient reported data for the estimation of HR, 3 were excluded because they put R1 resection and R2 resection together and 2 were excluded due to the small sample size (there are only 2 cases with R1 margin in both studies)17,18. Finally, a total of 12 studies14,15,16,19,20,21,22,23,24,25,26,27 were included in this meta-analysis. Literatures screening process was shown in Fig. 1.
The characteristics of included studies are shown in Table 1. In total, 12 studies including 1985 patients were included in the pooled analysis. DFS was obtained in 11 studies and OS was obtained in 8 studies. All studies had minimum 5 years follow-up period. The rate of R1 resection ranges from 3.5–33.3% (pooled rate 11.9%, 95% CI 8.3–15.4%). Adjuvant imatinib treatment was given in 5 of the studies. The quality of study assessed by Newcastle-Ottawa quality assessment scale ranged from seven to eight, with high value indicating eligible methodology (Table S1).
Recurrence rate
The overall recurrence rate in R1 resection and R0 resection group was 0.364 (95% CI 0.299–0.429) and 0.296 (95% CI 0.161–0.430), respectively. Although the recurrence rate in R1 resection group was slightly higher than that in R0 resection group, meta-analysis revealed that R1 resection did not increase the recurrence rate of GISTs (OR by fixed-effects model 0.891, 95% CI 0.653–1.215; OR by random-effects model 1.203, 95% CI 0.632–2.287; I2 = 66.2%, P value = 0.003) (Fig. 2). To explore the source of heterogeneity, meta-regression and subgroup analysis were performed. Adjuvant imatinib treatment was not the source of heterogeneity (Table 2). Sensitivity analysis indicated that pooled ORs were not significantly influenced by omission of any single study.
Disease-free survival
Meta-analysis using a random-effects model indicated that R1 resection had an unfavorable DFS compared with R0 resection (HR 1.596, 95% CI 1.128–2.258; I2 = 37.5%, P value = 0.091), which was consistent with the results of the fixed-effects model (HR 1.567, 95% CI 1.246–1.969) (Fig. 3). To determine whether other factors had an influence on the HR of DFS, we carried out subgroup analysis and meta-regression analysis. Table 3 demonstrates the overall and stratified analysis. Notably, in the adjuvant imatinib treatment subgroup, the patients with R1 resection showed no significant difference of DFS compared with R0 resection (HR 1.308, 95% CI 0.583–2.935; I2 = 53.2%, P value = 0.074). In the subgroup without adjuvant imatinib treatment, DFS of R1 resection still remained poor (HR 1.758, 95% CI 1.338–2.310; I2 = 11.3%, P value = 0.343). These results indicate that adjuvant imatinib treatment could attenuate the risk of recurrence for primary GIST patients who received R1 resection. Sensitivity analysis indicated that pooled HR was not significantly influenced by omission of any single study.
Overall survival
Eight studies including 553 GIST patients assessed overall survival (Table 4). Although R1 resection showed a tendency of poor OS, it failed to get a statistically significant HR (HR by fixed-effects model 1.283, 95% CI 0.770–2.138; HR by random-effects model 1.430, 95% CI 0.608–3.363; I2 = 60.8%, P value = 0.013) (Fig. 4). When stratified by adjuvant imatinib treatment, there was no significant difference between R1 resection and R0 resection in adjuvant imatinib treatment subgroup (HR 1.232, 95% CI 0.185–8.204; I2 = 73.8%, P value = 0.01), or in subgroup without adjuvant treatment (HR 1.755, 95% CI 0.947–3.254; I2 = 8.4%, P value = 0.351). Sensitivity analysis indicated that pooled HR was not significantly influenced by omitting any single study.
Publication bias
No evidence of publication bias was detected by either Begg’s or Egger’s test for OR of recurrence (Begg’s P = 1.000, Egger’s P = 0.197), HR of DFS (Begg’s P = 0.891, Egger’s P = 0.986), or HR of OS (Begg’s P = 0.322, Egger’s P = 0.350). The shape of the funnel plots did not reveal obvious asymmetry (Supplementary Figure S1).
Quality of evidence
This meta-analysis contained three outcomes: recurrence rate, disease-free survival and overall survival. The GRADE system evidence for each outcome level and reasons for upgrade and downgrade are shown in Table 5.
Discussion
Due to insights in the molecular targeted therapy and improved surgical techniques, treatment of GISTs has developed rapidly. Unpredictable malignant potential and rare lymph node metastasis provided the theoretical basis for the concept of minimally invasive surgery for GISTs. Consequently, several minimally invasive surgical approaches have been introduced, such as local wedge excision, laparoscopic surgery, endoscopic enucleation and related variations of this technique. However, there is a fine balance between complete resection and minimally invasive resection. Sometimes, an R1 resection might be inescapable owing to the following reasons. First, as a neoplasm arising from the mesenchymal tissue, GIST often abuts significant vessels and other vital structures. Thus, to avoid major functional sequelae, organ-preserving surgery is acceptable with a close or microscopically positive margin. Second, DeMatteo et al.27 suggested that large GISTs that infiltrated the serosa of the bowel wall, might shed cells from anywhere along their surface into the peritoneum. This theory was also supported by the study of Crosby et al.28. Third, with increasing upper gastrointestinal examination by endoscopy, the incidence of subclinical GIST has been higher than anticipated29. These incidentally encountered GISTs are often treated by endoscopic enucleation. However, Tumor enucleation is considered insufficient, given that it may leave behind a tumor-seeded pseudocapsule with R1 resection1,30. Even though some innovative endoscopic procedures attempte to support enucleation, such as endoscopic full-thickness resection (EFTR)31, laparoscopy endoscopy cooperative surgery (LECS)32, laparoscopy-assisted endoscopic full-thickness resection (LAEFR)33 and non-exposed wall-inversion surgery (NEWS)34, the efficacy and safety of those procedures are still assessed in the clinical trials. Fourth, the surgical safe margins are not well defined for GISTs. Most reports indicated that the 1–2 cm margins including the 5 mm of microscopic distance might be adequate in GISTs35,36. But the guidelines are not conclusive.
This meta-analysis included 12 studies with 1985 surgically treated primary GIST patients. The overall recurrence rate in R1 resection and R0 resection group was 0.364 (95% CI 0.299–0.429) and 0.296 (95% CI 0.161–0.430), respectively. Although some of these studies found that macroscopic tumor-free margins are essential to a good outcome of GIST surgery, but whether the status of microscopic margins could impact the recurrence remains unclear. The pooled results from this meta-analysis confirmed that a microscopically positive margin could significantly impact the disease-free survival (HR 1.596, 95% CI 1.128–2.258; I2 = 37.5%, P value = 0.091), but had no influence on overall survival (HR 1.430, 95% CI 0.608–3.363; I2 = 60.8%, P value = 0.013). Importantly, subgroup analysis revealed that there was no significant difference of DFS between R1 resection and R0 resection in the era of adjuvant imatinib treatment (HR 1.308, 95% CI 0.583–2.935; I2 = 53.2%, P value = 0.074), however, in the subgroup without adjuvant imatinib treatment, R1 resection still remained unfavorable (HR 1.758, 95% CI 1.338–2.310; I2 = 11.3%, P value = 0.343). These results indicated that adjuvant imatinib treatment could reduce the risk of recurrence for primary GIST patients who received R1 resection, clearly indicating a need for adjuvant treatment in this group. Although there is no evidence that re-excision could benefit the patients with R1 resection, re-excision is acceptable only if the original site of lesion can be found and major functional sequelae are not foreseen11. Based on the results of this meta-analysis, adjuvant imatinib treatment is proved to be effective for GIST patients with R1 resection. Therefore, we suggest that adjuvant imatinib treatment combined with re-excision might be a standard approach for patients with R1 resection and adjuvant imatinib treatment alone could also be sufficient for patients who are not suitable to undergo re-excision. The final decision should be carefully made by the multidisciplinary care team taking into account of possible risks and benefits.
The level of evidence achieved in this meta-analysis was assessed by the GRADE approach (Table 5). The critical outcomes: the quality of DFS was “moderate” and the quality of OS was “low”. The important outcome: the quality of recurrence rate was “low”. The levels of these outcomes were confined due to the limited evidence derived from observational studies. In addition, the quality of recurrence rate and OS was degraded due to the observational studies. Therefore, the quality of evidence for R1 resection as an unfavorable prognostic factor of GISTs is acceptable.
Some limitations of this meta-analysis should be discussed. The analysis of the included studies reporting the status of surgical margins needs to account for some confounding variables. The rate of R1 resection seemed to be associated with both tumor size and recurrent risk14,37. Given that GISTs with “intermediate” or “high” risk are easier to obtain microscopically positive margins, it is difficult to distinguish whether surgical margin or tumor grade is the major factor of recurrence risk for the patients with R1 resection. It is possible that surgical margin and tumor grade have a collinear relation in the analysis of tumor recurrence. To clarify this assumption, further studies with large sample of patients who received R1 resection are needed and analysis of the relevance between status of surgical margins and tumor grade should also performed in those studies. Unfortunately, there is only one study14 reporting the risk factors associated with and R1 resection among the studies included in this meta-analysis. Besides, this study proves that adjuvant imatinib treatment is effective in reducing the recurrence rate by the analysis of all patients with R1 resection. However, whether adjuvant imatinib treatment is essential for patients with R1 resection who are “very low” or “low” grade cannot be determined from this meta-analysis.
In conclusion, this meta-analysis revealed that a microscopically positive margin could significantly impact the disease-free survival, but had no influence on overall survival. In addition, adjuvant imatinib treatment could reduce the risk of recurrence for primary GIST patients who received R1 resection. Our results validated the goal of surgery with a negative microscopic margin and determined the management of R1 resection for GISTs.
Methods
Literature search
Two investigators (XZ and BJ) performed a systematic literature search in PubMed, EMBASE, Cochrane Library and Web of Science databases (last updated on July 15, 2015), using combinations of the following terms: “gastrointestinal stromal tumors”, “GIST” and “margins”. Disagreements were resolved through consensus with a third investigator (LM). Reports in English were eligible for inclusion. The bibliographies cited in selected articles were also examined to identify other relevant studies. Conference abstracts were excluded due to the insufficient data reported. All studies were carefully evaluated to identify duplicate data.
Inclusion criteria
The following criteria were used for the study selection: (1) Participants (P): All patients were diagnosed as primary GIST using pathology and immunohistochemistry. (2) Interventions (I) and comparisons (C): Comparing the prognosis of R1 resection versus R0 resection. (3) Outcomes (O): Disease-free survival (DFS), Overall survival (OS) and microscopically positive margin rate (MPMR). (4) Study design (S): retrospective or prospective study. (5) Sufficient information allowing for estimation of hazard ratios (HRs) and 95% confidence intervals (CIs).
Qualitative assessment
Quality assessment was performed in each of the acceptable studies in duplicate by independent reviewers (XZ and BJ) using the Newcastle-Ottawa Quality Assessment Scale for cohort studies. Discrepancies were resolved by a third reviewer (LM).
Data extraction
Two reviewers (XF and JY) independently extracted the required information from all primary studies. If HRs or their 95% CIs were not directly reported in the included studies, they were estimated according to the available survival data using a method reported by Tierney et al.38. If the trial results were reported in multiple publications, we extracted the data from the article with the strictest methodology and the most complete data.
Statistical analysis
We used the PRISMA checklist39 as protocol of the meta-analysis and followed the guideline (Table S2). For the pooled analysis of the survival data, HRs and their 95% CIs were used. The point estimate of the HR was considered statistically significant at the p < 0.05 level if the 95% CI did not include the value “1”.
Heterogeneity assumption was checked by the chi-square-based Q-test. A p-value >0.10 for the Q-test indicates a lack of heterogeneity among studies. We also quantified the effect of heterogeneity using I2 test. I2 values of <25% may be considered “low,” values of about 50% may be considered “moderate” and values of >75% may be considered “high”40. Both fixed-effects (Mantel–Haenszel method) and random-effects (DerSimonian–Laird method) models were used to estimate the pooled HRs/ORs. Given the inherent between-study heterogeneity, the random-effects model was chosen. To explore the heterogeneity between studies better, meta-regression analysis and subgroup analysis were performed. To explore the dynamic trends as studies accumulated over time, cumulative meta-analysis was performed by date of publication. Sensitivity analyses were conducted to validate whether modification of inclusion criteria affected the results. Potential publication bias was estimated by the funnel plot and Egger’s linear regression test. All analyses were carried out using STATA version 10.0 (Stata Corporation, College Station, TX). Two-sided p < 0.05 was considered statistically significant.
Grading the quality of evidence
The GRADE approach was used to interpret and validate the results41. The GRADEprofiler version 3.6 was used to create the evidence profile. For each outcome, we graded the quality of the studies at four levels as “very low”, “low”, “moderate” and “high” on the basis of risk of bias, inconsistency, indirectness, imprecision and publication bias.
Additional Information
How to cite this article: Zhi, X. et al. Prognostic role of microscopically positive margins for primary gastrointestinal stromal tumors: a systematic review and meta-analysis. Sci. Rep. 6, 21541; doi: 10.1038/srep21541 (2016).
References
Joensuu, H., Hohenberger, P. & Corless, C. L. Gastrointestinal stromal tumour. Lancet, 10.1016/S0140-6736(13)60106-3 (2013).
Fletcher, C. D. et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Human pathology 33, 459–465 (2002).
Joensuu, H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Human pathology 39, 1411–1419, 10.1016/j.humpath.2008.06.025 (2008).
Miettinen, M. & Lasota, J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Seminars in diagnostic pathology 23, 70–83 (2006).
Joensuu, H. et al. Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. The lancet oncology 13, 265–274, 10.1016/S1470-2045(11)70299-6 (2012).
Joensuu, H. et al. KIT and PDGFRA mutations and the risk of GI stromal tumor recurrence. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 33, 634–642, 10.1200/JCO.2014.57.4970 (2015).
Wozniak, A. et al. Tumor genotype is an independent prognostic factor in primary gastrointestinal stromal tumors of gastric origin: a european multicenter analysis based on ConticaGIST. Clinical cancer research: an official journal of the American Association for Cancer Research 20, 6105–6116, 10.1158/1078-0432.CCR-14-1677 (2014).
Rusakiewicz, S. et al. Immune infiltrates are prognostic factors in localized gastrointestinal stromal tumors. Cancer research 73, 3499–3510, 10.1158/0008-5472.CAN-13-0371 (2013).
Unalp, H. R. et al. Gastrointestinal stromal tumours: outcomes of surgical management and analysis of prognostic variables. Canadian journal of surgery. Journal canadien de chirurgie 52, 31–38 (2009).
Keun Park, C. et al. Prognostic stratification of high-risk gastrointestinal stromal tumors in the era of targeted therapy. Annals of surgery 247, 1011–1018, 10.1097/SLA.0b013e3181724f9d (2008).
Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO25 Suppl 3, iii21-26, 10.1093/annonc/mdu255 (2014).
Demetri, G. D. et al. NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)--update of the NCCN clinical practice guidelines. Journal of the National Comprehensive Cancer Network: JNCCN 5 Suppl 2, S1–29 quiz S30 (2007).
Gastrointestinal stromal tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO23 Suppl 7, vii49-55, 10.1093/annonc/mds252 (2012).
McCarter, M. D. et al. Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. Journal of the American College of Surgeons 215, 53–59 discussion 59–60, 10.1016/j.jamcollsurg.2012.05.008 (2012).
Rutkowski, P. et al. Risk criteria and prognostic factors for predicting recurrences after resection of primary gastrointestinal stromal tumor. Annals of surgical oncology 14, 2018–2027, 10.1245/s10434-007-9377-9 (2007).
Catena, F. et al. Microscopic margins of resection influence primary gastrointestinal stromal tumor survival. Onkologie 35, 645–648, 10.1159/000343585 (2012).
Hinz, S. et al. Audit of a series of 40 gastrointestinal stromal tumour cases. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 32, 1125–1129, 10.1016/j.ejso.2006.05.018 (2006).
Langer, C. et al. Prognostic factors influencing surgical management and outcome of gastrointestinal stromal tumours. The British journal of surgery 90, 332–339, 10.1002/bjs.4046 (2003).
Cananzi, F. C. et al. Prognostic factors for primary gastrointestinal stromal tumours: are they the same in the multidisciplinary treatment era? Langenbeck’s archives of surgery / Deutsche Gesellschaft fur Chirurgie 399, 323–332, 10.1007/s00423-014-1160-3 (2014).
Jakob, J. et al. Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Annals of surgical oncology 20, 586–592, 10.1245/s10434-012-2647-1 (2013).
Kim, M. Y. et al. Predictors of recurrence after resection of small gastric gastrointestinal stromal tumors of 5 cm or less. Journal of clinical gastroenterology 46, 130–137, 10.1097/MCG.0b013e31821f8bf6 (2012).
Huang, H. et al. Surgical outcomes of gastrointestinal stromal tumors of the stomach: a single unit experience in the era of targeted drug therapy. Med Oncol 29, 941–947, 10.1007/s12032-011-9888-x (2012).
Nikfarjam, M. et al. Surgical outcomes of patients with gastrointestinal stromal tumors in the era of targeted drug therapy. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 12, 2023–2031, 10.1007/s11605-008-0561-4 (2008).
Gouveia, A. M. et al. Surgical margin status and prognosis of gastrointestinal stromal tumor. World journal of surgery 32, 2375–2382, 10.1007/s00268-008-9704-8 (2008).
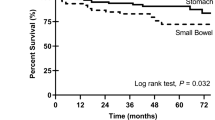
Wu, T. J. et al. Surgical treatment and prognostic analysis for gastrointestinal stromal tumors (GISTs) of the small intestine: before the era of imatinib mesylate. BMC gastroenterology 6, 29, 10.1186/1471-230X-6-29 (2006).
Pierie, J. P. et al. The effect of surgery and grade on outcome of gastrointestinal stromal tumors. Arch Surg 136, 383–389 (2001).
DeMatteo, R. P. et al. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Annals of surgery 231, 51–58 (2000).
Crosby, J. A. et al. Malignant gastrointestinal stromal tumors of the small intestine: a review of 50 cases from a prospective database. Annals of surgical oncology 8, 50–59 (2001).
Kawanowa, K. et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Human pathology 37, 1527–1535, 10.1016/j.humpath.2006.07.002 (2006).
Nishimura, J. et al. Surgical strategy for gastric gastrointestinal stromal tumors: laparoscopic vs. open resection. Surgical endoscopy 21, 875–878, 10.1007/s00464-006-9065-z (2007).
Zhou, P. H. et al. Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surgical endoscopy 25, 2926–2931, 10.1007/s00464-011-1644-y (2011).
Tsujimoto, H. et al. Successful gastric submucosal tumor resection using laparoscopic and endoscopic cooperative surgery. World journal of surgery 36, 327–330, 10.1007/s00268-011-1387-x (2012).
Hoteya, S. et al. Feasibility and safety of laparoscopic and endoscopic cooperative surgery for gastric submucosal tumors, including esophagogastric junction tumors. Digestive endoscopy: official journal of the Japan Gastroenterological Endoscopy Society 26, 538–544, 10.1111/den.12215 (2014).
Mitsui, T. et al. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric cancer: official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 17, 594–599, 10.1007/s10120-013-0291-5 (2014).
Iwahashi, M. et al. Surgical management of small gastrointestinal stromal tumors of the stomach. World journal of surgery 30, 28–35, 10.1007/s00268-005-7944-4 (2006).
Novitsky, Y. W., Kercher, K. W., Sing, R. F. & Heniford, B. T. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Annals of surgery 243, 738–745, discussion 745–737, 10.1097/01.sla.0000219739.11758.27 (2006).
Everett, M. & Gutman, H. Surgical management of gastrointestinal stromal tumors: analysis of outcome with respect to surgical margins and technique. Journal of surgical oncology 98, 588–593, 10.1002/jso.21030 (2008).
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S. & Sydes, M. R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8, 16, 10.1186/1745-6215-8-16 (2007).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS medicine 6, e1000100, 10.1371/journal.pmed.1000100 (2009).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560, 10.1136/bmj.327.7414.557 (2003).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926, 10.1136/bmj.39489.470347.AD (2008).
Acknowledgements
This work was funded by the National Natural Science Foundation of China (81503160) and the Scientific Innovation Foundation of Nantong (HS2014043).
Author information
Authors and Affiliations
Contributions
X.Z. and B.J. planned the study; X.Z., J.Y. and M.X. collected data; X.Z., J.Y., Q.N., L.S. and J.Z. drafted the manuscript. L.M. interpreted the study, O.R. and J.Q. refined language.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhi, X., Jiang, B., Yu, J. et al. Prognostic role of microscopically positive margins for primary gastrointestinal stromal tumors: a systematic review and meta-analysis. Sci Rep 6, 21541 (2016). https://doi.org/10.1038/srep21541
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep21541
This article is cited by
-
Clinical outcomes of endoscopic resection for the treatment of intermediate- or high-risk gastric small gastrointestinal stromal tumors: a multicenter retrospective study
Surgical Endoscopy (2024)
-
Survival analysis of extragastrointestinal stromal tumors based on the SEER database: a population-based study
Surgical Endoscopy (2023)
-
Prognostic value of Onodera’s nutritional index for intermediate- and high-risk gastrointestinal stromal tumors treated with or without tyrosine kinase inhibitors
World Journal of Surgical Oncology (2021)
-
Microscopic positive tumor margin does not increase the rate of recurrence in endoscopic resected gastric mesenchymal tumors compared to negative tumor margin
Surgical Endoscopy (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.