Abstract
Previous studies have demonstrated that extracellular glutathione reduces the ability of the Cystic Fibrosis pathogen Burkholderia cenocepacia to infect primary or immortalized epithelial respiratory cells. We report here that the adhesion and invasion ability of B. cenocepacia is limited also by thiol-oxidizing and disulphide-reducing agents and by protein disulfide isomerase (PDI) inhibitors. PDI inhibitors also reduce the proinflammatory response elicited by cells in response to Burkholderia. These findings indicate that a membrane-associated PDI catalyzes thiol/disulphide exchange reactions which favor bacterial infection. The combined use of selective PDI inhibitors, RNA silencing and specific antibodies identified ERp57 as a major PDI involved in the interaction between B. cenocepacia and epithelial cells. This study contributes to the elucidation of the Burkholderia pathogenic mechanisms by showing that this microorganism exploits a membrane-associated host protein to infect epithelial cells and identifies ERp57 as a putative pharmacological target for the treatment of Burkholderia lung infections.
Similar content being viewed by others
Introduction
A well known feature of Cystic Fibrosis (CF) is the marked decrease of reduced glutathione (GSH) concentration in the airway surface liquid (ASL) of patients1,2. This defect is the consequence of a reduced export of GSH through the lung epithelium and of an abnormal consumption of this antioxidant due to sustained chronic inflammation. In fact, some in vitro studies have suggested that the chloride efflux CFTR channel, which belongs to the MRP/ABC family of proteins that includes several GSH transporters, could be the direct mediator of GSH export3,4. The importance of a functional CFTR channel for GSH export is confirmed by the observation that CFTR knockout mice show comparable alterations in GSH extracellular content5 and fail to adapt GSH levels in response to cigarette smoke6. At the same time, other studies have revealed that low concentrations of GSH in the airways of young CF patients are associated to high levels of glutathionylated proteins and of glutathione sulfonamide, a specific byproduct of the reaction of GSH with the hypochlorous acid released in vivo by the abundant neutrophiles recruited in the CF lung7. Moreover, GSH7 and protein8 oxidation increases in CF children during pulmonary infections.
The role of extracellular GSH in the lung has been the object of limited investigations, but it is likely that it contributes to the control of lung inflammation by protecting the lung tissue by the damage caused by the reactive oxygen species spontaneously generated in this highly oxidizing environment or actively produced by neutrophils1,9. In addition, extracellular GSH could modulate mucus viscosity and regulate the redox state of membrane proteins containing labile disulphides10. There is also some evidence suggesting that extracellular GSH has a role in the response to bacterial lung infections. For example, GSH can reduce the toxic effects of pyocyanin11,12,13, a redox-active exotoxin released in large quantities by Pseudomonas aeruginosa during lung infections14, which significantly contributes to the pathophysiological alterations typical of the CF lung15. The concentration of GSH in the ASL significantly increases in wild type mice following P. aeruginosa infection, whereas this response is not observed in CFTR mutant mice16. Moreover, there is evidence that mycoplasma infections inhibit GSH adaptive response to oxidative stress17. We have recently demonstrated that GSH can drastically reduce the ability of the CF pathogen Burkholderia cenocepacia to adhere and invade epithelial respiratory cells, including CFTR deficient primary cells isolated from the lung of a CF patient undergoing to organ transplant18. The reduced ability of bacteria to interact with host cells is correlated with a drastic reduction of the inflammatory response and to an increase of free thiol groups on the proteins located on the external cell membrane18. This observation is suggestive of a GSH-mediated change in the redox status of membrane proteins involved in B. cenocepacia recognition. Among the membrane-associated proteins which could be affected by changes in the GSH levels outside the cells there are members of the Protein Disulphide Isomerase (PDI) family. PDIs are typically localized in the endoplasmic reticulum, where they contribute to the maturation of newly synthesized proteins by catalyzing the formation and reshuffling of disulphide bonds19. However, several studies have revealed that some PDIs may be found also in other subcellular districts (cytoplasm, nucleus, cell membrane) where they may functionally contribute to a variety of cellular activities20,21. Membrane-associated PDIs have been implicated in the attachment and entry of several viruses22,23,24,25,26, of bacteria of the Chlamydia genus27,28 of the protozoan Leishmania chagasi29, as well as in the uptake of peptides and proteins, including diphtheria and cholera toxins30,31. These studies have suggested that PDI may mediate the transient formation of disulfide bonds between a membrane receptor and a protein located on the surface of the infectious agent, thus facilitating its subsequent internalization. As high levels of extracellular GSH could affect PDI activity and/or the structure of receptor proteins, we have investigated the possibility that Burkholderia adhesion and infection are promoted by host PDIs.
Results
Thiol-modifying reagents reduce the invasive ability of B. cenocepacia LMG 16656
To test the hypothesis that extracellular GSH interferes with B. cenocepacia ability to infect epithelial respiratory cells by modifying cysteine residues of cell surface proteins18, we have carried out invasion assays in presence of the reducing agent dithiotreithol (DTT) or of the membrane-impermeant thiol oxidant 5,5′ dithio-bis (2-nitrobenzoic)acid (DTNB) which forms mixed disulfides with –SH groups32. Figure 1a shows that when 9HTEo- cells were infected for 3 hour with B. cenocepacia LMG 16656 in presence of 1 mM DTT, there was a more than 90% decrease in the number of intracellular bacteria with respect to control cells. Similarly, also the number of total B. cenocepacia LMG 16656 associated to 9HTEo- cells (including either adherent or intracellular bacteria) was markedly modified by the incubation with 1 mM DTT (Fig. 1b), indicating that DTT affects either adhesion or invasion of B. cenocepacia. At the same time, the oxidation of free thiols resulting from incubation of 9HTEo- cells with 1 mM DTNB induces a strong decrease of B. cenocepacia LMG16656 invasion (approximately 98%) and adhesion (85%), as shown in Fig. 1c,d, respectively. Incubation of 9HTEo- cells with 1 mM DTT enhanced the number of cell surface thiols to levels which are even higher to those observed after a treatment with 10 mM GSH18, whereas incubation with DTNB caused a reduction of surface-associate thiols (Fig. 1e,f).
Both DTT and DTNB reduce the ability of B. cenocepacia LMG 16656 to infect epithelial cells.
(a) Invasion of 9HTEo- cells by B. cenocepacia LMG 16656 after 3 hours of infection in presence or absence of 1 mM DTT. (b) Effect of 1 mM DTT on the total number of bacteria (adherent + intracellular) interacting with 9HTEo- epithelial cells after 3 hours of infection. (c) Invasion of 9HTEo- cells by B. cenocepacia LMG 16656 after 1 hour of infection in presence or absence of 1 mM DTNB. (d) Effect of 1 mM DTNB on the total number of bacteria (adherent + intracellular bacteria) interacting with 9HTEo- epithelial cells after 1 hour of infection. The data reported in (panels a–d) represent the mean ± SD of 3 independent experiments. Asterisks denote statistically significant results (**p < 0.001). (e,f) Cytofluorimetric analysis of surface thiols after treatment with DTT and GSH (e) and DTNB (f). Cells were incubated for 3 hours with 1 mM DTT or with 1 mM GSH (e) or for 1 hour with 1 mM DTNB (f) and then treated with 10 μM Alexa fluor C5-maleimide to label surface free thiols and then analyzed by FACScalibur system, as described in Materials and Methods. The histograms from a typical experiment are shown.
When infection experiments were carried out using bacteria pretreated with DTNB, but omitting the addition of this chemical agent during the incubation of bacteria with cells, we observed a significant increase in bacterial invasion ability, despite DTNB having a bacteriostatic effect (Fig. 2c). This observation suggests that free thiols located on the bacterial surface hinder B. cenocepacia interaction with epithelial cells.
PDI inhibitors decrease the ability of B. cenocepacia LMG 16656 to infect 9HTEo- cells.
(a,b) Effect of 0.3 mM bacitracin on. B. cenocepacia invasion (panel a) and on the total number of bacteria (adherent + intracellular) interacting with 9HTEo- cells (panel b). (c) Effect of bacitracin (open square, solid line) or DTNB (open triangle, dotted line) or the absence of treatment (filled circle, dashed line) on B. cenocepacia growth in MEM supplemented with 2 mM glutamine and 2% FBS. The inset shows the effect of bacterial pretreatment with 1 mM DTNB on B.c. LMG 16656 invasiveness into 9HTEo- cells. (d) Inhibition of B. cenocepacia 6L invasion in 9HTEo- cells in presence of 0.3 mM bacitracin. (e,f) Effect of 10 μM 16F16 on B. cenocepacia invasion (panel e) and on the total number of bacteria interacting with epithelial cells (panel f). Each panel reports the mean ± SD of, respectively, 4 (panels a,b), 5 (panel c) or 3 (panels d–f) independent experiments. Asterisks denote statistically significant results: *p < 0.05; **p < 0.001.
These experiments confirm that cysteine residues of proteins associated to the membranes of epithelial cells and, possibly, on the bacterial surface, play a role in the interaction and/or the entry of Burkholderia into host cells and suggest that infectivity of this bacterium is dependent on protein targets prone to cysteine modification either by reducing or oxidizing agents.
PDI inhibitors are able to influence B. cenocepacia ability to invade epithelial cells
Putative protein targets susceptible to both reducing and oxidizing agents include enzymes of the PDI family. To evaluate if PDIs are involved in the interaction of B. cenocepacia with 9HTEo- cells, we have used well known inhibitors of enzymes of this class. We have initially tested the effect of bacitracin which is widely used as inhibitor of PDI activity30. As shown in Fig. 2a,b, bacitracin significantly inhibits both adhesion and invasion of B. cenocepacia LMG 16656 in 9HTEo- cells. The number of intracellular and total bacteria recovered from 9HTEo- cells treated with bacitracin is approximately 90% lower than that of bacteria found in control cells. Interestingly, the extent of bacitracin-mediated inihibition of B. cenocepacia invasivity is comparable to that obtained with 10 mM extracellular GSH18 or 1 mM DTT.
It must be noted that, although bacitracin has antibacterial activity against Gram-positive bacteria33, it has no effects on Burkholderia growth (Fig. 2c). Moreover, we have observed a significant increase in the number of extracellular bacteria in the supernatants of cells treated with bacitracin (data not shown), thereby confirming that this drug affects the interaction between bacteria and epithelial respiratory cells.
The effect of bacitracin was also tested on the B. cenocepacia 6L clinical isolate, observing that also the ability of this strain to penetrate into 9HTEo- cells is reduced by bacitracin to an extent comparable to that obtained with extracellular GSH18 (Fig. 2d). This observation supports the hypothesis that PDI has a role in mediating the ability of different B. cenocepacia strains to invade epithelial cells.
To confirm the involvement of enzymes of the PDI family in B. cenocepacia interaction with epithelial cells, we have carried out infection experiments in the presence of 16F16, a compound that inhibits the PDI isoforms P4HB (also known as PDIA1) and ERp57 (also known as PDIA3)34.
The results reported in Fig. 2e,f show that when the infection was carried out in presence of 10 μM 16F16 there was a significant reduction in the number of intracellular and adherent bacteria with respect to control cells. Higher concentrations of 16F16 proved to be toxic for 9HTEo- cells and could not be tested. As in the case of bacitracin, we did not observe adverse effects of this compound as well as of all the other PDI inhibitors used in this work, except DTNB (Fig. 2c), on B. cenocepacia growth (data not shown).
A specific inhibitor of P4HB is quercetin-3-rutinoside, also known as rutin35. Infection experiments carried out in presence or in absence of 30 μM rutin failed to show an effect of this compound on the invasion or adhesion of B. cenocepacia to 9HTEo- cells (Fig. 3a). This result suggests that P4HB is not a major PDI isoform mediating the ability of this pathogen to infect epithelial cells.
B. cenocepacia invasion is specifically inhibited by PDI inhibitors targeting ERp57.
(a) Effect of 30 μM rutin on B. cenocepacia ability to adhere and invade 9HTEo- cells. (b,c). Effect of 20 and 40 μM EGCG on the invasion (panel b) or on the total number of bacteria (panel c) interacting with 9HTEo-cells. (d) Differential effects of epicathechin (EC) and epigallocatechin gallate (EGCG) on B. cenocepacia ability to adhere and invade 9HTEo- cells. (e) EGCG impairs B. cenocepacia invasivity in different epithelial cell lines. The reported data are the mean ± SD of, respectively, 3 (panels a,b,d,e) or 8 (panel c) independent experiments. Asterisks denote statistically significant results: **p < 0.001.
To evaluate the possible involvement of ERp57, we tested the effects on B. cenocepacia invasivity of EGCG, a green tea flavanol which has been shown to bind to this specific PDI isoform in vitro and modify its enzymatic activity and DNA-binding properties36. 9HTEo- cells have been pre-incubated with 0, 20 or 40 μM EGCG for 30 minutes and then infected with B. cenocepacia LMG 16656 for 3 hours in presence of the same amount of EGCG. Panels b and c of Fig. 3 show that EGCG reduces B. cenocepacia infectivity in a concentration-dependent manner. The number of total and intracellular bacteria isolated from cells treated with 40 μM EGCG decreased by 85% and by more than 90%, respectively, whereas this reduction was less marked when 9HTEo- cells were incubated with 20 μM EGCG. The reduction in bacterial infectivity obtained with 40 μM EGCG is comparable to that obtained with 10 mM GSH. No inhibition of the invasive ability of Burkholderia was observed using 40 μM epicatechin (Fig. 3d), which, lacking the galloyl moiety, binds ERp57 with low affinity and does not modify its activity36.
The effect of EGCG on B. cenocepacia LMG 16656 invasion was also tested on other cell lines, such as CFBE41o-, C38 and IB3-1. In all these cell lines we observed a consistent reduction in bacterial invasion when infections were carried out in presence of 40 μM EGCG (Fig. 3e).
These experiments show that a wide range of PDI inhibitors is able to interfere with the capability of B. cenocepacia to adhere and invade epithelial cells and suggest that ERp57 could play an important role in the infectivity of this pathogen.
Silencing or inhibition of ERp57 reduces B. cenocepacia ability to penetrate in epithelial cells
To obtain additional evidence of the involvement of ERp57 in the interaction between Burkholderia and epithelial cells, we have carried out infection experiments in 9HTEo- cells transfected with short interfering RNA (siRNA) for ERp57, P4HB or with a negative control siRNA. Figure 4 shows that cells exhibiting a decreased level of ERp57 (panel a) are less prone to B. cenocepacia invasion (panel b). The number of intracellular bacteria in cells transfected with the ERp57-specific siRNA was 45% lower than in cells transfected with an irrelevant RNA. In contrast, the silencing of P4HB caused only a modest decrease of Burkholderia entry into 9HTEo- cells with respect to control siRNA cells, which did not reach statistical significance (Fig. 4b).
Erp57 is involved in B. cenocepacia interaction with respiratory cells.
(a) Western blot analysis of ERp57 and P4HB in 9HTEo- cells transfected with different siRNAs. Lactate dehydrogenase (LDH) was used as a loading control. (b) Invasion assay of B. cenocepacia LMG 16656 in 9HTEo- cells transfected with control siRNA, P4HB siRNA and ERp57 siRNA. The reported values are means ± SD obtained by measuring B. cenocepacia LMG 16656 invasion ability in a representative experiment, including six replicates. *p < 0.05; **p < 0.001. (c) Effect of antibody-mediated PDIs blockade on the ability of B. cenocepacia to interact with 9HTEo- cells. Histograms represents the total number of bacteria (adherent + intracellular) recovered from the cell monolayer after 1 hour of infection in presence or in absence of antibodies against ERp57 or P4HB. The reported values are means ± SD from four replicates in a representative experiment. *p < 0.05. (d) Identification of a fraction of ERp57 associated to 9HTEo- cell membranes. MIPs (Maximum Intensity Projections) with orthogonal projections XZ (below of each panel) and YZ (right of each panel) from confocal system acquisition (Olympus IX 81 inverted microscope, software FV 1000) of 9HTEo- cells fixed and permeabilized (left panel) and unpermeabilized 9HTEo- cells (right panel). ERp57, detected by immunofluorescence, appears in green, whereas the nuclei, stained with Hoechst, appear in blue. Bars = 20 μm.
To further investigate the role of P4HB and ERp57 in B. cenocepacia interaction with 9HTEo-cells, we have carried out infection experiments in presence of 50 μg/ml of a function-blocking anti-P4HB antibody30 or of an anti-ERp57 antibody, after pre-treating the cells for 30 minutes with the antibodies. No difference in Burkholderia infectivity has been observed between control cells and 9HTEo- cells incubated with the P4HB antibody (Fig. 4c). In contrast, we observed a significant reduction (35%) in the number of bacteria associated to 9HTEo- cells when the infection was carried out in presence of the anti-ERp57 antibody (Fig. 4c).
Together, these experiments show that the PDI isoform ERp57 has a major role in mediating B. cenocepacia interaction with epithelial cells, whereas the PDI isoform P4HB has little or no role in this process. Immunofluorescence studies in permeabilized and unpermeabilized cells confirmed that small amounts of ERp57 can be localized on the surface of 9HTEo- cells (Fig. 4d).
PDI inhibitors reduce the inflammatory response of 9HTEo- cells to infections by B. cenocepacia LMG 16656
We have previously observed that extracellular GSH reduces the inflammatory response of epithelial cells to B. cenocepacia infections18. To evaluate the possibility that also inhibitors of PDI may reduce the inflammatory response of 9HTEo-induced by B. cenocepacia, we have analyzed by quantitative real-time RT-PCR the expression of IL-8, TNF-α and IL-1β, into tracheo-bronchial cells infected in absence and in presence of 10 mM GSH, 0.3 mM bacitracin, 10 μM 16F16, 30 μM rutin and 40 μM EGCG. With the exception of rutin, all the other PDI inhibitors proved to significantly decrease the B. cenocepacia-induced expression of the three Cytokines (Fig. 5). The capacity of EGCG to control the inflammatory response elicited by B. cenocepacia was confirmed by its ability to significantly reduce the release of IL-6 and IL-8 (Fig. 5b,c).
ERp57 inhibitors reduce the expression and release of some pro-inflammatory cytokines in response to B. cenocepacia infection.
(a) The expression of IL-8, TNF-α and IL-1β was analyzed by RT-PCR in 9HTEo- cells infected with B. cenocepacia LMG 16656 (10 CFU/cell). Infection was carried out either in cells kept in standard medium or in cells incubated with various chemical agents interfering with PDI activity, including EGCG (40 μM), GSH (10 mM), bacitracin (0,3 mM), rutin (30 μM) and 16F16 (10 μM). Data are the average +/− SD of two independent experiments and the results are shown as relative percentages of expression of each cytokine with respect to its expression in cells infected in the absence of PDI inhibitors. (b) Effect of 40 μM EGCG treatment on the IL-8 release from 9HTEo- cells incubated with or without B.c. LMG 16656 for 3 hours. Supernatants of cultures were collected and IL-8 was measured by ELISA. Values represent the mean ± SD of four individual cultures. (c) IL-6 release from 9HTEo- cells as described in b.
Discussion
CF is characterized by recurrent pulmonary infections caused by opportunistic pathogens that show a marked ability to proliferate in the lungs of patients. B. cenocepacia is a typical CF pathogen characterized by an intrinsic multidrug resistance37. Although it colonizes a relatively small number of CF patients, it is associated with a negative prognosis because it can promote a condition described as “cepacia syndrome”, which is characterized by rapid pulmonary decline and death38.
We have recently observed that extracellular GSH impairs the ability of B. cenocepacia to adhere to and penetrate within primary and immortalized epithelial respiratory cells18. As GSH is poorly able to permeate membranes, this observation suggested that this reducing agent could modulate the interaction between Burkholderia and epithelial cells by affecting the redox state of cysteines and/or disulphides of membrane-associated proteins involved in bacterial recognition. In this work we have provided further support to this hypothesis by showing that other thiol-modifying agents, such as DTT and DTNB, impair B. cenocepacia ability to infect cells (Fig. 1). DTNB, just as GSH, is unable to permeate membranes suggesting that these compounds affect B. cenocepacia infectivity by altering protein targets localized on the cell surface of epithelial cells. Moreover, either reducing (DTT and GSH) or oxidizing agents (DTNB) have similar effects on bacterial adhesion and invasion. This observation prompted us to investigate the possibility that enzymes of the PDI family, whose activity depends on highly reactive dithiol/disulfide centers, could mediate bacterial binding and internalization of B. cenocepacia. Although PDIs are primarily located in the endoplasmic reticulum to favor folding of nascent proteins, there is abundant evidence that a fraction of the enzyme localizes on the cell surface20,21.
The possibility that a host protein catalyzing the formation and breakage of disulfide bonds mediates Burkholderia infection has been initially evaluated in experiments involving the broad spectrum PDI inhibitor bacitracin, which directly interacts with cysteines in the substrate-binding domain of PDI by forming a disulphide bond with an open thiol form of the bacitracin thiazoline ring39. Bacitracin was found to inhibit bacterial attachment and entry at levels comparable with GSH18 (Fig. 2). However, as the specificity of bacitracin has been questioned by studies showing that it can bind free cysteines also in other proteins40, we have tested other structurally unrelated PDI inhibitors. We found that also 16F16 and EGCG reduce the capability of Burkholderia to adhere to or enter within 9HTEo- cells. This result is not due to effects of these compounds on the growth or survival of bacteria. It can be noted that an inhibition of B. cenocepacia invasivity comparable to that obtained incubating cells with 10 mM GSH18 was achieved using 0.3 mM bacitracin or 40 μΜ EGCG (Figs 2 and 3).
The use of multiple inhibitors, besides strengthening the hypothesis that PDI activity mediates Burkholderia infection, gives indications on the identity of the PDI isoform facilitating bacterial interaction with respiratory cells. The PDI family, indeed, includes as many as 21 different proteins41, many of which have been identified at the cell surface. Whereas bacitracin is a rather unspecific PDI inhibitor, there is evidence that compounds such as 16F16, rutin and EGCG show preferential inhibitory activity towards specific PDI isoforms34,35,36. The observation that Burkholderia invasion ability is insensitive to rutin, an inhibitor of the P4HB isoform, but is inhibited by 16F16 and EGCG, which are able to inhibit the ERp57 isoform, prompted us to further investigate the involvement of this specific enzyme in the ability of the pathogen to infect respiratory cells.
The role of ERp57 has been confirmed either by RNAi experiments or by the use of function-blocking antibodies. In fact, we have shown that ERp57-depleted epithelial cells are infected by a lower number of bacteria with respect to control cells (Fig. 4b) and that the incubation with an ERp57 antibody protects 9HTEo- cells from Burkholderia adhesion and entry (Fig. 4c). In contrast, the silencing of P4HB leads to a non-significant reduction of bacterial invasion and an anti-P4HB antibody does not modify bacterial interaction with cells. Interestingly, previous studies have shown that antibodies against P4HB impair entry of Chlamydia and of different viruses within eukaryotic cells27,42,43. On the contrary, ERp57 is involved in the entry of the rotavirus ECwt44, whereas the nairovirus nairobi sheep disease virus/ganjam virus has been recently proved to induce translocation of ERp57 and PDI to the cell membrane during the infection24. These studies suggest that distinct PDI isoforms may mediate the recognition of specific infectious agents.
Burkholderia is able to enter within mammalian cells, where it efficiently survives and replicates by its ability to interfere with the antimicrobial responses of the host cell45,46,47. The modality by which B. cenocepacia gains access into host cells is not completely understood, but a few membrane proteins involved in the host-Burkholderia recognition have been identified. It has been shown that, depending on the specific strain, Burkholderia can interact with mucin, cytokeratin 13, tumor necrosis factor receptor 1 (TNFR1), glycolipid and glycosphingolipid receptors present on epithelial cells45,46. Interestingly, most of the above mentioned putative protein receptors contain disulphide bonds which could be substrates for the activity of ERp57. For example, TNFR1 contains cysteine-rich extracellular domains which are involved in protein conformational stabilization and in control of receptor responsiveness48. Additional studies are needed to identify the cell surface receptor(s) involved in the recognition of B. cenocepacia and to directly demonstrate that ERp57 has the ability to bind bacteria and/or modulate the oxidoreductive state of thiols of receptors proteins, but our results, collectively, converge in indicating that this pathogen may efficiently penetrate within epithelial cells by exploiting membrane-associated ERp57. Although the physiological role of surface exposed ERp57 in epithelial respiratory cells is not known, it should be noted that previous studies have identified specific functions for the extracellular form of this enzyme in other cell types, including participation to sperm-egg fusion49, platelet aggregation50, the binding of 1α,25-dihydroxycholecalciferol by gut epithelial cells51 and, together with calreticulin, determination of immunogenicity of cell death52. We propose that ERp57 represents a “Trojan Horse” which facilitates Burkholderia invasion of epithelial cells through a mechanism similar to that schematized in Fig. 6. The suggestion that the target on the bacterial surface is a disulphide bond is supported by the observation that bacterial pretreatments with DTNB stimulate invasion (Fig. 2c, inset), whereas pretreatments with DTT reduce invasion (not shown) and those with GSH have no effects18.
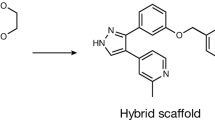
Schematic model for the ERp57-mediated disulphide exchange which favors bacterial attachment to epithelial cells.
We suggest that membrane-associated ERp57 (PDI) (panel a) catalyzes a disulphide exchange reaction between a surface exposed Burkholderia cenocepacia receptor (BcR) and a disulphide bond located on a B. cenocepacia (Bc) solvent exposed protein. We hypothesize that the formation of a transient disulphide bond between ERp57 and a BcR located on the cell membrane (panel b) promotes B. cenocepacia adhesion to the cell surface (panel c) and the subsequent internalization of the bacterium.
In this work we have also shown a correlation between inhibition of ERp57, Burkholderia infection and pro-inflammatory response of the infected epithelial cells. ERp57 inhibitors reduce the pro-inflammatory response elicited by 9HTEo- cells in response to B. cenocepacia infection. This finding confirms that strategies aimed at reducing B. cenocepacia intracellular burden might be of help in controlling the inflammatory response to this pathogen.
This work provides some clues towards possible treatments of B. cenocepacia infections in CF patients. Our observations suggest that low levels of GSH in the ASL may contribute to the ability of B. cenocepacia to colonize the lung of CF patients by influencing the activity of proteins belonging to the PDI family. Several studies have been carried out to evaluate the efficacy of therapies aimed at elevating the concentration of GSH in the lung of patients, but their effectiveness remains doubtful53. It has been suggested that poor efficacy of therapies based on GSH nebulization could be explained by the presence of high levels of the GSH degrading enzyme γ-glutamyl transferarse in the ASL of CF patients54. Our studies indicate that inhibitors of PDI activity have an ability to limit B. cenocepacia interaction with epithelial cells comparable to GSH, thereby representing a potential therapeutic alternative to favor the control of B. cenocepacia infections. It is worth nothing that EGCG, besides showing the ability to inhibit ERp57, has been reported to inhibit biofilm formation by a variety of CF pathogens55, to interfere with P. aeruginosa quorum sensing56; to limit lung colonization by Stenotrophomonas maltophilia57 and to contribute to the control of viral infections58,59,60,61. The combination of these studies and our observations mark EGCG as a potentially promising drug for the treatment of bacterial lung infections in CF and other respiratory diseases.
Methods
Reagents
GSH, bacitracin, 16F16, rutin, epigallocatechin gallate (EGCG), epicatechin (EC), dithiotreitol (DTT) and 5,5′ dithio-bis (2-nitrobenzoic)acid (DTNB) were provided from Sigma Aldrich. GSH solutions were prepared as previously described18. Bacitracin was dissolved in the infection medium. DTNB was prepared in ethanol, DTT was solubilized in distilled water, whereas 16F16, rutin, EGCG and EC were dissolved in DMSO. Antibodies against P4HB (RL90) and ERp57(sc-23886) were obtained from Thermo scientific and Santa Cruz, respectively. All these compounds were subsequently diluted in the infection medium.
Bacterial strains and growth conditions
The B. cenocepacia strain LMG 16656, corresponding to the sequenced reference strain J231562, was obtained from the Belgian Coordinate Collection of Microorganism (BCCM). The clinical isolate B. cenocepacia 6L (cblA-; BCESM+)63 was chosen for its marked difference in interaction with epithelial cells with respect to B. cenocepacia LMG 1665618. Bacteria grown on Pseudomonas Isolation Agar (PIA) plates (DifcoTM) were inoculated in chemically defined medium (CDM), containing 48 mM glucose, 7.4 mM KCl, 6 mM NaCl, 48 mM (NH4)2SO4, 0.5 mM MgSO4×7H2O, 60 mM MOPS, 3.8 mM K2HPO4×3H2O, 0.1% Casamino acid and cultivated without agitation at 37 °C, as previously described18.
Host cell lines and culture conditions
The human tracheobronchial epithelial cell line 9HTEo-64 and the cystic fibrosis human bronchial epithelial cell line CFBE41o- (ΔF508/ΔF508)65 were kindly provided by Dr. Dieter Gruenert (University of California at San Francisco). The cystic fibrosis bronchial epithelial cell line IB3−1 (ΔF508/W1282X) and the isogenic CFTR-complemented C38 cell line were obtained from ATCC.
Cells were routinely maintained in MEM (9HTEo- and CFBE41o-) or D-MEM (IB3-1 and C38) (Euroclone) supplemented with 2 mM glutamine, 100 U/ml penicillin, 0.1 mg/ml streptomycin and 10% heat-inactivated fetal bovine serum (FBS), in a humidified 5% CO2 incubator, at 37 °C. All cell lines were grown in bovine serum albumin-collagen-fibronectin coated flasks and the confluent, adherent monolayers were released from the plastic surface after treatment with trypsin (C38 and IB3-1) or polyvinyl-pirrolidone-trypsin-EDTA solution (9HTEo- and CFBE41o-), collected by centrifugation at 700 × g and resuspended in fresh medium. The effect of all treatments (bacterial infections, incubation with each chemical compound or with a combination of bacteria and compounds) on cell viability was evaluated by the trypan blue exclusion method, without observing any significant consequence on cell viability.
Invasion assays
Cell monolayers were prepared by seeding 1.5 × 105 cells/well (9HTEo- and CFBE41o-) or 1.0 × 105 cells/well (C38 and IB3-1) epithelial cells in precoated 6-well tissue culture plates, 48 hours before infection. Cells were grown at 37 °C in 5% CO2 and, prior to bacterial infection, were incubated for 2 hours in antibiotic-free medium, containing 2% FBS. In experiments involving PDIs inhibitors, epithelial cells were pretreated with the various compounds for 30 minutes before adding bacteria and maintained thorough the infection, unless otherwise stated. Bacteria were grown to mid-exponential phase (OD600 of 0.3–0.4) and then diluted in antibiotic-free medium containing 2% FBS, with or without 10 mM GSH, 1 mM DTNB, 1 mM DTT, 0.3 mM bacitracin, 10 μM 16F16, 30 μM rutin, 50 μg/ml of antibody against P4HB or ERp57, or 20 and 40 μM EGCG. The bacterial suspension was used to infect semi-confluent cell monolayers at a multiplicity of infection (MOI) of 10 bacteria/cell. Bacterial pre-treatments with 1 mM DTNB or 1 mM DTT were carried out in antibiotic free medium for 1 hour. After centrifugation, pretreated bacteria were resuspended in antibiotic-free medium to infect 9HTEo- cells for 1 hour.
Invasion assays were performed by using the ceftazidime-amikacin protection assay, as described18. Infected monolayers were incubated for 3 hours at 37 °C in 5% CO2 or 1 hour in the case of DTNB. Then, infected cells were washed twice with PBS and fresh medium containing amikacin (1 mg/ml) and ceftazidime (1 mg/ml) was added to kill extracellular bacteria. After 2 hours of incubation at 37 °C, a time sufficient to ensure the killing of all planktonic bacteria18, monolayers were washed twice with PBS, treated with trypsin for 5 minutes at 37 °C and then lysed by the addition of 1% deoxycholic acid. Intracellular bacteria were quantified by plating serial dilutions of the lysates on PIA plates. Invasion efficiency was calculated as the number of intracellular bacteria recovered after cell incubation in presence of antibiotics divided by the number of bacteria added to each well. To evaluate the number of total bacteria associated to cells (adherent + intracellular), infected monolayers were gently washed with PBS 4 times and bacteria were isolated by lysing cells with trypsin and deoxycholic acid and quantified by plating serial dilutions of the lysates on PIA plates. Each invasion assay included at least three independent replicates.
Immunofluorescence staining and microscopy
To detect the presence of ERp57 on the cell surface, cells were stained at 4 °C following a procedure that prevents the endocytosis of the antigen-antibody complex and minimizes lateral mobility of bound antibody along the plane of the plasma membrane.
After an incubation of 5 hours in antibiotic-free medium containing 2% FBS, 9HTEo- cells were washed four times with PBS and 0.1% sodium azide and incubated at 4 °C for 30 minutes in 10% FBS, 0.1% sodium azide to prevent non specific binding of antibodies. Cells were then incubated at 4 °C for 1 hour with a mouse monoclonal antibody against ERp57 (SC-23886, Santa Cruz) diluted 1:100 in PBS/0.1% sodium azide. After extensive washing with PBS/0.1% sodium azide, bound antibodies were detected by incubating slides with Alexa Fluor® 488 Anti-Mouse IgG (A21202, Life Technologies) diluted 1:500 for 1 hour at 4 °C. 9HTEo- cells were then fixed in 4% paraformaldehyde diluted in PBS/0.1% sodium azide and the nuclei were counterstained with Hoechst.
Total staining of ERp57 was obtained by fixing 9HTEo- monolayers in cold methanol for 10 minutes at −20 °C and permeabilizing cells with 0.1% Triton X-100. To prevent non-specific binding of antibodies, slides were incubated with 5% BSA (Biowest) in PBS for 1 hour at room temperature. Cells were then incubated with the mouse monoclonal antibody SC-23886 against ERp57 diluted 1:100 in 5% BSA overnight at 4 °C. Bound antibodies were detected by incubating slides with Alexa Fluor® 488 Anti-Mouse IgG (Life Technologies) diluted 1:500 for 1 hour at room temperature and the nuclei were counterstained with Hoechst.
Immunostained cells were mounted and visualized under a confocal microscope (Olympus Fluoview 1000) and excited at 488 nm with an Argon-ion laser and at 405 nm with a diode laser. Orthogonal projections XZ and YZ obtained from confocal system acquisitions were elaborated with software Imaris 7.1 (Bitplane).
Detection of external plasma membrane thiols
For detection of external plasma membrane thiols, cells were seeded in precoated 12-well tissue culture plates and grown at 37 °C in 5% CO2. After 48 hours of incubation, monolayers were incubated for 2 hours in antibiotic-free medium containing 2% FBS. After 3 hours of incubation with or without 1 mM DTT or 1 mM GSH or after 1 hour with or without 1 mM DTNB, the monolayers were washed and incubated in PBS alone or with 10 μM Alexa fluor 488 C5-maleimide (Molecular Probes) for 30 minutes at 37 °C. Subsequently, the cells were washed and scraped in PBS. Labeled thiols were detected by cytofluorimetric analysis using a BD FACScalibur.
Cytokine analysis
The amount of cytokine mRNA was determined by quantitative real-time PCR. Total RNA from cells was isolated using the High Pure RNA isolation kit (Roche, Mannheim, Germany). Reverse transcription (RT) was performed using the High Capacity cDNA Archive kit (Applied Biosystems, Foster City, CA, USA). Real-time qPCR analyses were carried out blindly by the QuantiGene Service of the Italian Cystic Fibrosis Research Foundation, using established procedures66. The levels of IL-8 (diluted 1:20) and IL-6 in supernatants were also measured by ELISA (R&D Systems, UK), according to the manufacturer’s instructions.
siRNA-mediated knockdown
siRNA were purchased from Qiagen. For each gene, four different siRNA were used: SI02662100, SI02662639, SI00018501, SI03026191 for PDIA1; SI02654771 SI02654778 SI00075656 SI00075663 for ERp57. As a control, we have used AllStars Negative Control siRNA. The siRNA knockdown experiments were carried out by plating 1.5 × 105 cells in six-well plates (3 wells for each gene silencing) and transfecting for 8 hours with 30 pmol siRNA using Lipofectamine RNAiMAX (Invitrogen) in Opti-MEM I-medium (Invitrogen) and MEM devoid of antibiotics. Medium was changed and the day after each well was split 1:4 in a 24-well plate and incubated for further 48 hours. Six wells were used for Burkholderia invasion assays and the others to verify knockdown by western blotting.
Data analysis
Statistical analysis was performed using the SigmaPlot version IV software (Systat Software, San Jose, CA). Data describing the effect of chemical compounds (GSH, DTT, DTNB, bacitracin, 16F16, rutin and EGCG) on the ability of B. cenocepacia to adhere or invade epithelial cells were analyzed using the non-parametric Kruskal–Wallis test, completed with the Dunn’s Multiple Comparison post-hoc test when required. Data from invasion experiments in cells treated with siRNAs or antibodies were analyzed using one way ANOVA and completed with the Bonferroni post-hoc test. The Student’s t-test was used to analyze the statistical significance of the variation of cytokine expression between infected cells and infected cells with each PDI inhibitor. Differences in IL-6 and IL-8 release were analyzed using a two way ANOVA test and completed with the Bonferroni post-hoc test. Data are expressed as mean ± standard deviation. p values <0.05 were considered significant. The control values in infections experiments carried out with B. cenocepacia LMG 16656 and 9HTEo- cells are the average of a large number of independent experiments (55 invasion assays and 76 measures of the total number of bacteria associated to cells). The values ± SD describing the effect of each compound on bacterial ability to infect epithelial cells are the average of a number of independent experiments, each one including replicates, reported in the legends to figures.
Additional Information
How to cite this article: Pacello, F. et al. An ERp57-mediated disulphide exchange promotes the interaction between Burkholderia cenocepacia and epithelial respiratory cells. Sci. Rep. 6, 21140; doi: 10.1038/srep21140 (2016).
References
Hudson, V. M. Rethinking cystic fibrosis pathology: the critical role of abnormal reduced glutathione (GSH) transport caused by CFTR mutation. Free Radical Biol Med 30, 1440–1461 (2001).
Cantin, A. M., North, S. L., Hubbard, R. C. & Crystal, R. G. Normal alveolar epithelial lining fluid contains high levels of glutathione. J Appl Physiol 63, 152–157 (1987).
Kogan, I. et al. CFTR directly mediates nucleotide-regulated glutathione flux. EMBO J. 22, 1981–1989 (2003).
Ballatori, N. et al. Glutathione dysregulation and the etiology and progression of human diseases. Biol Chem. 390, 191–214 (2009).
Velsor, L. W., van Heeckeren, A. & Day, B. J. Antioxidant imbalance in the lungs of cystic fibrosis transmembrane conductance regulator protein mutant mice. Am J Physiol Lung Cell Mol Physiol. 281, L31–38 (2001).
Gould, N. S., Min, E., Gauthier, S., Martin, R. J. & Day, B. J. Lung glutathione adaptive responses to cigarette smoke exposure. Resp Res. 12, 133 (2011).
Kettle, A. J. et al. Oxidation contributes to low glutathione in the airways of children with cystic fibrosis. Eur Respir J. 44, 122–129 (2014).
Sadowska-Bartosz, I., Galiniak, S., Bartosz, G. & Rachel, M. Oxidative modification of proteins in pediatric cystic fibrosis with bacterial infections. Oxid Med Cell Longev. 2014, 389629 (2014).
Kelly, F. J. Gluthathione: in defence of the lung. Food Chem Toxicol. 37, 963–966, doi: S0278-6915(99)00087-3 [pii] (1999).
Imhoff, B. R. & Hansen, J. M. Extracellular redox status regulates Nrf2 activation through mitochondrial reactive oxygen species. Biochem J. 424, 491–500 (2009).
Muller, M. Glutathione modulates the toxicity of, but is not a biologically relevant reductant for, the Pseudomonas aeruginosa redox toxin pyocyanin. Free Rad Biol Med. 50, 971–977 (2011).
Cheluvappa, R., Shimmon, R., Dawson, M., Hilmer, S. N. & Le Couteur, D. G. Reactions of Pseudomonas aeruginosa pyocyanin with reduced glutathione. Acta Biochim Pol. 55, 571–580 (2008).
Muller, M. & Merrett, N. D. Mechanism for glutathione-mediated protection against the Pseudomonas aeruginosa redox toxin, pyocyanin. Chem Biol Interact. 232, 30–37 (2015).
Lau, G. W., Hassett, D. J., Ran, H. & Kong, F. The role of pyocyanin in Pseudomonas aeruginosa infection. Trends Mol Med. 10, 599–606 (2004).
Caldwell, C. C. et al. Pseudomonas aeruginosa exotoxin pyocyanin causes cystic fibrosis airway pathogenesis. American J Pathol 175, 2473–2488 (2009).
Day, B. J., van Heeckeren, A. M., Min, E. & Velsor, L. W. Role for cystic fibrosis transmembrane conductance regulator protein in a glutathione response to bronchopulmonary pseudomonas infection. Infect Immun. 72, 2045–2051 (2004).
Kariya, C. et al. Mycoplasma pneumoniae infection and environmental tobacco smoke inhibit lung glutathione adaptive responses and increase oxidative stress. Infect Immun 76, 4455–4462 (2008).
D’Orazio, M., Pacello, F. & Battistoni, A. Extracellular glutathione decreases the ability of Burkholderia cenocepacia to penetrate into epithelial cells and to induce an inflammatory response. PloS one 7, e47550 (2012).
Freedman, R. B., Hirst, T. R. & Tuite, M. F. Protein disulphide isomerase: building bridges in protein folding. Trends Biochem Sci 19, 331–336 (1994).
Turano, C., Coppari, S., Altieri, F. & Ferraro, A. Proteins of the PDI family: unpredicted non-ER locations and functions. J Cell Physiol 193, 154–163 (2002).
Ali Khan, H. & Mutus, B. Protein disulfide isomerase a multifunctional protein with multiple physiological roles. Front Chem 2, 70 (2014).
Diwaker, D., Mishra, K. P. & Ganju, L. Potential roles of protein disulphide isomerase in viral infections. Acta Virol. 57, 293–304 (2013).
Fenouillet, E., Barbouche, R., Courageot, J. & Miquelis, R. The catalytic activity of protein disulfide isomerase is involved in human immunodeficiency virus envelope-mediated membrane fusion after CD4 cell binding. J Infect Dis 183, 744–752 (2001).
Lasecka, L. & Baron, M. D. The nairovirus nairobi sheep disease virus/ganjam virus induces the translocation of protein disulphide isomerase-like oxidoreductases from the endoplasmic reticulum to the cell surface and the extracellular space. PloS one 9, e94656 (2014).
Markovic, I. et al. Thiol/disulfide exchange is a prerequisite for CXCR4-tropic HIV-1 envelope-mediated T-cell fusion during viral entry. Blood 103, 1586–1594 (2004).
Ryser, H. J. & Fluckiger, R. Progress in targeting HIV-1 entry. Drug Discov Today 10, 1085–1094 (2005).
Abromaitis, S. & Stephens, R. S. Attachment and entry of Chlamydia have distinct requirements for host protein disulfide isomerase. PLoS Pathog. 5, e1000357 (2009).
Conant, C. G. & Stephens, R. S. Chlamydia attachment to mammalian cells requires protein disulfide isomerase. Cell Microbiol. 9, 222–232 (2007).
Santos, C. X. et al. Protein disulfide isomerase (PDI) associates with NADPH oxidase and is required for phagocytosis of Leishmania chagasi promastigotes by macrophages. J Leukoc Biol 86, 989–998 (2009).
Mandel, R., Ryser, H. J., Ghani, F., Wu, M. & Peak, D. Inhibition of a reductive function of the plasma membrane by bacitracin and antibodies against protein disulfide-isomerase. Proc Natl Acad Sci USA 90, 4112–4116 (1993).
Torres, A. G. & Gait, M. J. Exploiting cell surface thiols to enhance cellular uptake. Trends Biotechnol. 30, 185–190 (2012).
Janiszewski, M. et al. Inhibition of vascular NADH/NADPH oxidase activity by thiol reagents: lack of correlation with cellular glutathione redox status. Free Rad Biol Med 29, 889–899 (2000).
Johnson, B. A., Anker, H. & Meleney, F. L. Bacitracin: A New Antibiotic Produced by a Member of the B. Subtilis Group. Science 102, 376–377 (1945).
Hoffstrom, B. G. et al. Inhibitors of protein disulfide isomerase suppress apoptosis induced by misfolded proteins. Nat Chem Biol 6, 900–906 (2010).
Jasuja, R. et al. Protein disulfide isomerase inhibitors constitute a new class of antithrombotic agents. J Clin Invest. 122, 2104–2113, (2012).
Trnkova, L., Ricci, D., Grillo, C., Colotti, G. & Altieri, F. Green tea catechins can bind and modify ERp57/PDIA3 activity. Biochim Biophys Acta 1830, 2671–2682 (2013).
Govan, J. R. & Deretic, V. Microbial pathogenesis in cystic fibrosis: mucoid Pseudomonas aeruginosa and Burkholderia cepacia. Microbiol Rev 60, 539–574 (1996).
Isles, A. et al. Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J Pediatr 104, 206–210 (1984).
Dickerhof, N., Kleffmann, T., Jack, R. & McCormick, S. Bacitracin inhibits the reductive activity of protein disulfide isomerase by disulfide bond formation with free cysteines in the substrate-binding domain. FEBS J 278, 2034–2043 (2011).
Karala, A. R. & Ruddock, L. W. Bacitracin is not a specific inhibitor of protein disulfide isomerase. FEBS J 277, 2454–2462 (2010).
Galligan, J. J. & Petersen, D. R. The human protein disulfide isomerase gene family. Hum genomics 6, 6 (2012).
Stantchev, T. S. et al. Cell-type specific requirements for thiol/disulfide exchange during HIV-1 entry and infection. Retrovirology 9, 97, doi: 10.1186/1742-4690-9-97 (2012).
Wan, S. W. et al. Endothelial cell surface expression of protein disulfide isomerase activates beta1 and beta3 integrins and facilitates dengue virus infection. J Cell Biochem. 113, 1681–1691 (2012).
Santana, A. Y., Guerrero, C. A. & Acosta, O. Implication of Hsc70, PDI and integrin alphavbeta3 involvement during entry of the murine rotavirus ECwt into small-intestinal villi of suckling mice. Arch Virol 158, 1323–1336 (2013).
Saldias, M. S. & Valvano, M. A. Interactions of Burkholderia cenocepacia and other Burkholderia cepacia complex bacteria with epithelial and phagocytic cells. Microbiology 155, 2809–2817 (2009).
Ganesan, S. & Sajjan, U. S. Host evasion by Burkholderia cenocepacia. Front Cell Infect Microbiol 1, 25 (2011).
Amer, A. O. The many uses of autophagosomes. Autophagy 9, 633–634 (2013).
Branschadel, M. et al. Dual function of cysteine rich domain (CRD) 1 of TNF receptor type 1: conformational stabilization of CRD2 and control of receptor responsiveness. Cell Signal 22, 404–414 (2010).
Ellerman, D. A., Myles, D. G. & Primakoff, P. A role for sperm surface protein disulfide isomerase activity in gamete fusion: evidence for the participation of ERp57. Dev cell. 10, 831–837 (2006).
Holbrook, L. M. et al. The platelet-surface thiol isomerase enzyme ERp57 modulates platelet function. J thromb Haemost. 10, 278–288
Nemere, I. et al. Ribozyme knockdown functionally links a 1,25(OH)2D3 membrane binding protein (1,25D3-MARRS) and phosphate uptake in intestinal cells. Proc Natl Acad Sci USA 101, 7392–7397 (2004).
Panaretakis, T. et al. The co-translocation of ERp57 and calreticulin determines the immunogenicity of cell death. Cell Death Differ. 15, 1499–1509 (2008).
Griese, M. et al. Inhalation treatment with glutathione in patients with cystic fibrosis. A randomized clinical trial. Am J Respir Crit Care Med. 188, 83–89 (2013).
Corti, A., Pompella, A., Bergamini, G. & Melotti, P. Glutathione inhalation treatments in cystic fibrosis: the interference of airway gamma-glutamyltransferase. Am J Respir Crit Care Med. 189, 233–234 (2014).
O’May, C., Ciobanu, A., Lam, H. & Tufenkji, N. Tannin derived materials can block swarming motility and enhance biofilm formation in Pseudomonas aeruginosa. Biofouling 28, 1063–1076 (2012).
Yang, L., Liu, Y., Sternberg, C. & Molin, S. Evaluation of enoyl-acyl carrier protein reductase inhibitors as Pseudomonas aeruginosa quorum-quenching reagents. Molecules 15, 780–792 (2010).
Gordon, N. C. & Wareham, D. W. Antimicrobial activity of the green tea polyphenol (-)-epigallocatechin-3-gallate (EGCG) against clinical isolates of Stenotrophomonas maltophilia. Int J Antimicrob Agents 36, 129–131 (2010).
Liu, S. et al. (–)-Epigallocatechin-3-gallate inhibition of Epstein-Barr virus spontaneous lytic infection involves ERK1/2 and PI3-K/Akt signaling in EBV-positive cells. Carcinogenesis 34, 627–637 (2013).
Huang, H. C. et al. (–)-Epigallocatechin-3-gallate inhibits entry of hepatitis B virus into hepatocytes. Antiviral Res. 111, 100–111 (2014).
Chen, C. et al. (–)-Epigallocatechin-3-gallate inhibits the replication cycle of hepatitis C virus. Arch Virol. 157, 1301–1312 (2012).
Calland, N. et al. (–)-Epigallocatechin-3-gallate is a new inhibitor of hepatitis C virus entry. Hepatology 55, 720–729 (2012).
Holden, M. T. et al. The genome of Burkholderia cenocepacia J2315, an epidemic pathogen of cystic fibrosis patients. J Bacteriol. 191, 261–277 (2009).
Petrucca, A. Molecular characterization of Burkholderia cepacia isolates from cystic fibrosis (CF) patients in an Italian CF center. Res Microbiol 154, 491–498 (2003).
Gruenert, D. C. et al. Characterization of human tracheal epithelial cells transformed by an origin-defective simian virus 40. Proc Natl Acad Sci USA 85, 5951–5955 (1988).
Bruscia, E. et al. Isolation of CF cell lines corrected at Delta F508-CFTR locus by SFHR-mediated targeting. Gene Ther. 9, 683–685 (2002).
Nicolis, E. et al. Pyrogallol, an active compound from the medicinal plant Emblica officinalis, regulates expression of pro-inflammatory genes in bronchial epithelial cells. Int Immunopharmacol 8, 1672–1680, doi: 10.1016/j.intimp.2008.08.001 (2008).
Acknowledgements
This work was supported by the grants FFC#15/2010 (to A.B.) and FFC#13/2014 (to F.P.) from the Italian Foundation for Cystic Fibrosis Research (FFC) and by a grant from Pennsylvania Cystic Fibrosis Inc (PACFI). We also want to thank the Studio Palladio 2000, Sandrigo (VI) and the “Delegazione FFC di Roma2” for supporting the project FFC#15/2010 and the “Delegazioni di Olbia Tempio, Catania and Villa D′Almè (Bg) and Negozi Claudio Miceli” for supporting the project FFC#13/2014. Thanks are due to the FFC QuantiGene service, for carrying out the RT-PCR quantification of gene transcription. Prof Michele Scardi and Dr. Maria Chiara Mastropasqua are greatly acknowledged for their support in carrying out a revision of the statistical analysis of experimental data, whereas Dr Elena Romano and the Centre for Advanced Microscopy ‘Patrizia Albertano” are acknowledged for the help in image acquisition.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design, analysis and discussion of the research. FP and MD executed all the assays described in the work. FP and AB wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Pacello, F., D’Orazio, M. & Battistoni, A. An ERp57-mediated disulphide exchange promotes the interaction between Burkholderia cenocepacia and epithelial respiratory cells. Sci Rep 6, 21140 (2016). https://doi.org/10.1038/srep21140
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep21140
This article is cited by
-
DNA nanodevices map enzymatic activity in organelles
Nature Nanotechnology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.