Abstract
Angiotensin II (AngII) plays important roles in the regulation of cardiovascular function. Both peripheral and central actions of AngII are involved in this regulation, but mechanisms of the latter actions as a neurotransmitter/neuromodulator within the brain are still unclear. Here we show that (1) intracerebroventricularly (i.c.v.) administered AngII in urethane-anesthetized male rats elevates plasma adrenaline derived from the adrenal medulla but not noradrenaline with valsartan- (AT1 receptor blocker) sensitive brain mechanisms, (2) peripheral AT1 receptors are not involved in the AngII-induced elevation of plasma adrenaline, although AngII induces both noradrenaline and adrenaline secretion from bovine adrenal medulla cells and (3) i.c.v. administered AngII elevates blood pressure but not heart rate with the valsartan-sensitive mechanisms. From these results, i.c.v. administered AngII acts on brain AT1 receptors, thereby inducing the secretion of adrenaline and pressor responses. We propose that the central angiotensinergic system can activate central adrenomedullary outflow and modulate blood pressure.
Similar content being viewed by others
Introduction
Angiotensin II (AngII) plays a predominant role in the regulation of fluid and electrolyte balance and cardiovascular function1,2. Whilst the peripheral actions of AngII are important in this regulation, there is also evidence indicating the involvement of central AngII actions. The central actions are mediated both by circulating AngII acting via the blood-brain barrier deficient circumventricular organs3,4 and centrally generated AngII5,6 acting within the brain on cerebral regions known to influence the central regulation of fluid and electrolyte balance and cardiovascular function7,8. The responses to centrally acting AngII include the regulation of body water balance, vasopressin release, blood pressure maintenance and sympathetic nervous system activity9,10.
It is widely assumed that circulating AngII causes hypertension through its well-known direct renal and arterial actions11, but activation of angiotensinergic sympatho-excitatory pathways in the brain are also involved in the development and progression of hypertension induced by circulating AngII12. There is accumulating evidence indicating that excessive central sympathetic nerve activity plays a pathogenic role in triggering and sustaining the essential hypertensive state13. The involvement of the sympatho-adrenomedullary system in the response to stress is well known14. While the response is essential for adaptation to stress, excess or sustained exposure to stress can contribute to the development of hypertension15,16. Taken together with the involvement of the brain angiotensinergic system in response to stress17,18, it is necessary to clarify the central regulatory mechanisms of the sympatho-adrenomedullary outflow regarding centrally acting AngII for elucidating the fundamental mechanisms for the “establishment” of hypertension.
Plasma catecholamines, i.e., noradrenaline (NA) and adrenaline (Ad), are elevated by activation of the sympatho-adrenomedullary system and the concentrations can reflect global activity of the system. Plasma Ad is mainly secreted from Ad-containing cells in the adrenal medulla, while plasma NA reflects not only the release from sympathetic nerve terminals but also the secretion from NA-containing cells in the medulla19,20. Previous reports of this laboratory have shown that the influence of acute bilateral adrenalectomy on centrally administered stress-related neuropeptides that induced elevation of plasma NA and Ad was different depending on the peptides. The procedure abolished elevation of plasma Ad, but not NA, induced by corticotropin-releasing factor (CRF), while both elevations induced by bombesin or vasopressin respectively were attenuated by adrenalectomy in rats21,22. These findings suggest a possibility that sympathetic and adrenomedullary systems can be separately regulated by the central nervous system. In the present study, we examined the effects of AngII directly administered into the rat brain on both systems by measuring plasma NA and Ad, blood pressure and heart rate.
Results
Centrally administered AngII elevates plasma Ad but not NA
Treatment with vehicle [10 μl saline per animal, intracerebroventricularly (i.c.v.)] had no effect on the plasma levels of NA and Ad (Figure 1a and 1b). AngII (1 and 3 nmol per animal, i.c.v.) dose-dependently elevated plasma Ad, but AngII at a dose of 10 nmol per animal (i.c.v.) showed similar effects on plasma Ad compared with the effects of AngII at 3 nmol (Figure 1a and 1b). The Ad responses peaked at 10 min after the administration of AngII and then declined towards their basal levels (Figure 1a). On the other hand, AngII (1, 3 and 10 nmol per animal, i.c.v.) had no significant effects on plasma NA (Figure 1a and 1b). The actual values for NA and Ad at 0 min were 413 ± 21 and 253 ± 14 pg ml−1 (n = 23).
Effects of centrally administered angiotensin II (AngII) on plasma noradrenaline and adrenaline levels.
Vehicle (10 μl saline per animal) or AngII (1, 3 or 10 nmol per animal) was i.c.v. administered. (a) Increments of plasma noradrenaline and adrenaline above the basal level. ΔNoradrenaline and ΔAdrenaline: increments of noradrenaline and adrenaline above the basal level are expressed as pg ml−1. Arrow indicates the administration of vehicle or AngII. (b) The area under the curve (AUC) of the elevation of plasma noradrenaline and adrenaline above the basal level for each group is expressed as pg 2 h−1. Each point represents the mean ± s.e.m. *P < 0.05, when compared to the vehicle-treated group with the Bonferroni method.
Ad elevated by AngII is derived from adrenal medulla
In previous preliminary studies, we measured the plasma concentration of corticosterone and cortisol23. Three hours after sham-operation or adrenalectomy plus hydrocortisone, corticosterone and cortisol were 358.0 ± 21.6 and 23.3 ± 4.1 ng ml−1 in sham-operated rats (n = 3) and 28.1 ± 3.1 and 484.0 ± 151.5 ng ml−1 in adrenalectomized rats with hydrocortisone (5 mg kg−1, i.m.) (n = 3), respectively. In the present study, the basal plasma level of Ad was effectively reduced by acute bilateral adrenalectomy: the actual values for Ad at 0 min were 222 ± 64 pg ml−1 in the sham-operated group (n = 4) and 71 ± 7 pg ml−1 in the adrenalectomized group (n = 4). AngII (3 nmol per animal, i.c.v.) induced elevation of plasma Ad in the sham-operated group was abolished by the bilateral adrenalectomy (Figure 2a and 2b).
Effect of acute bilateral adrenalectomy on the centrally administered AngII-induced elevation of plasma adrenaline levels.
Acute bidirectional adrenalectomy [plus hydrocortisone (5 mg kg−1 per animal, i.m.)] or sham-operation (plus 200 μl saline per animal, i.m.) was done 3 h before the application of AngII (3 nmol per animal, i.c.v.). (a) Increments of plasma adrenaline above the basal level. Arrow indicates the administration of AngII. (b) AUC of the elevation of plasma adrenaline above the basal level for each group. *P < 0.05, when compared to the sham-operated group with an unpaired Student's t-test. Other conditions are the same as those of Figure 1.
AngII induces Ad elevation through brain AT1 receptors
Preliminary, we checked that central treatment with valsartan, an AT1 receptor blocker, or PD123319, an AT2 receptor blocker, only had no obvious effect on plasma levels of Ad (data not shown). Pretreatment with valsartan (100 nmol per animal, i.c.v.) almost abolished AngII- (3 nmol per animal, i.c.v.) induced elevation of plasma Ad (Figure 3a and 3b). On the other hand, pretreatment with PD123319 (100 nmol per animal, i.c.v.) had no significant effect on the AngII-induced response (Figure 3c and 3d). The actual values for Ad at 0 min were 303 ± 22 pg ml−1 in the vehicle-1- [3 μl of 100% N,N-dimethylformamide (DMF) per animal, i.c.v.] pretreated group (n = 5), 118 ± 21 pg ml−1 in the valsartan-pretreated group (n = 5), 184 ± 52 pg ml−1 in the vehicle-2- (5 μl saline per animal, i.c.v.) pretreated group (n = 4) and 148 ± 28 pg ml−1 in the PD123319-pretreated group (n = 6), respectively.
Effects of valsartan and PD123319 on the centrally administered AngII-induced elevation of plasma adrenaline levels.
Valsartan (Val) (AT1 receptor blocker) (100 nmol per animal), vehicle-1 (3 μl DMF per animal), PD123319 (PD) (AT2 receptor blocker) (100 nmol per animal), or vehicle-2 (5 μl saline per animal) was i.c.v. administered 30 min before the administration of AngII (3 nmol per animal, i.c.v.). (a and c) Increment of plasma adrenaline above the basal level. Arrows indicate the administration of Val (a)/PD (c)/vehicle-1/vehicle-2 and AngII. (b and d) AUC of the elevation of plasma adrenaline above the basal level for each group of (a) and (c), respectively. *P < 0.05, when compared to the vehicle-1- and AngII-treated group with an unpaired Student's t-test. The other conditions are the same as those of Figures 1 and 2.
AngII evokes NA and Ad secretion from adrenal medulla cells
In comparison with the control group, the AngII- (3.3 or 10 μM) treated group showed significant increments of spontaneous secretion of NA and Ad from the cultured bovine adrenal chromaffin cells at 60, 90 and 120 min after administration (Figure 4a and 4b). The degree of increments in Ad was larger than those in NA (Figure 4a and 4b).
Effect of AngII on secretion of noradrenaline and adrenaline from cultured bovine adrenal chromaffin cells.
Cells were incubated with (3.3 or 10 μM) or without (None) indicated concentrations of AngII for up to 120 min at 37°C. Subsequently, both noradrenaline (a) and adrenaline (b) secreted spontaneously in the incubation medium were measured by HPLC. Data represent the mean ± s.e.m. *P < 0.05, when compared to the “None” group with an unpaired Student's t-test.
Centrally acting AngII induces Ad elevation
Preliminary, we checked that peripheral treatment with valsartan only had no obvious effect on plasma levels of Ad (data not shown). In rats pretreated with vehicle (300 μl of 1% DMF per saline per animal, i.v.), centrally administered AngII- (3 nmol per animal, i.c.v.) induced elevation of plasma Ad (Figure 5a and 5b) but not NA (data not shown). Pretreatment with valsartan (100 nmol per animal, i.v.) had no significant effect on the AngII- (3 nmol per animal, i.c.v.) induced elevation of plasma Ad (Figure 5a and 5b). The actual values for Ad at 0 min were 174 ± 39 pg ml−1 in the vehicle-pretreated group (n = 5) and 271 ± 39 pg ml−1 in the valsartan-pretreated group (n = 4), respectively.
Effect of peripherally administered valsartan on the centrally administered AngII-induced elevation of plasma adrenaline levels.
Valsartan (Val) (AT1 receptor blocker) (100 nmol/animal) or vehicle (300 μl of 1% DMF in saline per animal) was i.v. administered 30 min before the administration of AngII (3 nmol per animal, i.c.v.). (a) Increments of plasma adrenaline above the basal level. Arrows indicate the administration of Val/vehicle and AngII. (b) AUC of the elevation of plasma adrenaline above the basal level for each group. Other conditions are the same as those of Figures 1–3.
Centrally acting AngII induces pressor responses
In the vehicle- (300 μl saline containing 1% DMF per animal, i.v.) pretreated group, systolic, mean and diastolic blood pressure were significantly elevated 5 min after administration of AngII (3 nmol per animal, i.c.v.) compared with the valsartan- (100 nmol per animal, i.v.) pretreated group, but no significant blood pressure changes between the two groups were observed 0 min after the administration of AngII (Table 1). On the other hand, heart rate in the vehicle-pretreated group was significantly lower than that in the valsartan-pretreated group 0 and 5 min after the administration of AngII (Table 1).
Discussion
In this study, we demonstrated that i.c.v. administered AngII elevated plasma Ad, but not NA, secreted from the rat adrenal medulla. The AngII-induced Ad secretion was inhibited by central pretreatment with valsartan, an AT1 receptor blocker, but not with PD123319, an AT2 receptor blocker. AngII stimulated the spontaneous secretion of both Ad and NA from bovine adrenal chromaffin cells, but the centrally administered AngII-induced secretion of Ad was not influenced by peripheral pretreatment with valsartan. I.c.v. administered AngII elevated systolic, mean and diastolic blood pressure but not heart rate and the elevations were abolished by valsartan. Our data suggest that centrally administered AngII acting on brain AT1 receptors induced Ad secretion from the rat adrenal medulla and pressor responses.
Studies in which AngII was administered directly into the cerebroventricles showed increases in blood pressure in many species24,25. On the other hand, acute i.c.v. administered AngII shows a different pattern of peripheral sympathetic outflow. AngII transiently inhibits renal sympathetic nerve activity, but increases splanchnic and cardiac sympathetic nerve activities26,27. These findings suggest that centrally acting AngII modulates sympathetic nerve activity in a regionally selective way. In the present study, i.c.v. administered AngII significantly elevated plasma Ad but not NA, indicating a possibility that selective activation and inhibition of sympathetic nerve activities induced by AngII counteracts significant changes in plasma NA levels. Previous reports of this laboratory showed that i.c.v. administered neuromedin U, a stress-related neuropeptide28, also elevated plasma Ad, but not NA29 and that i.c.v. administered CRF activated celiac and stellate ganglia but not superior cervical ganglia in the rat30. Taken together, central regulation of sympathetic outflow can occur in a region/organ-selective manner and sympathetic and adrenomedullary systems can be regulated separately by the central nervous system.
Plasma Ad originates exclusively from the Ad-containing cells in the adrenal medulla, however, the contribution of the extramedullary chromaffin tissues cannot be excluded. Therefore, we examined the effect of acute bilateral adrenalectomy supplemented with hydrocortisone on the i.c.v. administered AngII-induced elevation of plasma Ad. Cortisol (hydrocortisone) supplementation in adrenalectomized rats resulted in similar concentrations compared to corticosterone in sham-operated rats. Since cortisol and corticosterone have similar efficacy to corticosteroid, this supplementation can counteract the deficiency of corticosterone in adrenalectomized rats. In the present study, adrenalectomy abolished the AngII-induced elevation of plasma Ad, suggesting that centrally administered AngII activates the secretion of Ad from the rat adrenal medulla.
Typical receptors for AngII are divided into AT1 and AT2 subtypes, which are also distributed within the brain7,31. In rodents, two AT1 isoforms, AT1a and AT1b, have been identified and an overlapping localization of the isoforms is observed in the brain32; however, the ligand specificities and signal-effector coupling are virtually identical33,34. Therefore, it seems to be difficult to distinguish the two isoforms using pharmacological approaches. There is a growing consensus that the balance between AT1 and AT2 receptor signalling can determine the biological response induced by AngII. Brain AT1 receptors have been implicated in the regulation of blood pressure35, while brain AT2 receptors seem to modulate the inhibition of the sympathetic nervous system36. Actually, increasing central AT2 receptor expression attenuated the development of renovascular hypertension in the rat37. In the present study, we characterized which subtype (AT1 or AT2) in the brain is involved in the i.c.v. administered AngII-induced elevation of plasma Ad using valsartan or PD123319. Valsartan is a highly selective blocker for AT1 receptors, exhibits Ki values of 2.38 nM at AT1 and 30,000-fold higher selectivity than AT238. PD123319 is a potent and selective blocker for AT2 receptors, exhibits Ki values of 210 nM at AT2 in the rat brain39 and 1,800-fold higher selectivity than AT140. In the present study, central pretreatment with valsartan strongly attenuated the AngII-induced elevation of plasma Ad. On the other hand, PD123319 had no effect on the AngII-induced response. These results suggest that brain AT1 receptors are involved in the centrally administered AngII-induced secretion of Ad from the rat adrenal medulla.
Subsequently, we examined a possibility that AngII administered into the cerebroventricles can leak into the systemic circulation, thereby acting on the adrenal medulla directly. In the present experiment, i.c.v. administered AngII (1 and 3 nmol per animal) dose-dependently elevated plasma Ad in the rat. Considering the volume of the cerebrospinal fluid in the rat (about 300 μl41), the amount of AngII given i.c.v. in our study would result in a cerebrospinal fluid concentration of 3.3 and 10 μM, respectively. In an in vitro assay, treatment with AngII at these doses significantly induced spontaneous secretion of both NA and Ad from the bovine adrenal chromaffin cells and the degree of Ad increments was larger than that of NA ones. These results suggest that AngII has the ability to induce secretion of both catecholamines, especially Ad, from the adrenal medulla directly. On the other hand, peripheral pretreatment with valsartan, which hardly crosses the blood brain barrier, had no effect on the i.c.v. administered AngII-induced elevation of plasma Ad in the rat. Taken together, centrally administered AngII induces Ad secretion from the rat adrenal medulla through the brain, but not peripheral, AT1 receptors, whereas i.c.v. administered AngII rapidly elevated blood pressure, in accordance with previous reports24,25. Moreover, the pressor responses were abolished by peripheral pretreatment with valsartan, although the pretreatment had no effect on AngII-induced Ad secretion. This discrepancy is probably explained by a vasorelaxant effect of peripherally administered valsartan, which can counteract the vasocontractive effect of Ad secreted by the centrally administered AngII. Actually, compared with the vehicle pretreated group, tachycardia was observed in the valsartan-pretreated group, indicating a possibility that the tachycardia may be a compensatory action after peripherally administered valsartan-induced vasorelaxation.
In the brain, AT1 receptors are distributed in circumventricular organs and regions influencing the central regulation of cardiovascular function such as the nucleus tractus solitarius, the rostoral and caudal ventrolateral medulla and the hypothalamus31,42. In the hypothalamus, the paraventricular nucleus (PVN) has been considered as a regulatory centre of the central sympatho-adrenomedullary outflow43,44. Actually, microinjected AngII into the PVN increased mean blood pressure45 and specific knockdown of AT1a receptors in the PVN by infusion of interfering RNA against the receptors prevents hypertension induced by AngII treated peripherally46,47. These findings suggest a possibility that the angiotensinergic system in the PVN is critical for AngII-induced elevation of blood pressure and also for the central sympatho-adrenomedullary outflow. However, the PVN is a heterogeneous structure containing different types of output neurons including projecting neurons to brain stem autonomic centres and to sympathetic preganglionic neurons located in the spinal cord48,49. Oldfoeld et al. reported that the AT1 receptors are not expressed in the PVN neurons directly projecting to sympathetic preganglionic neurons located in the T2 level50. However, further studies are required to examine the distribution of the receptors in the PVN neurons projecting brain stem autonomic centers and other spinal cords.
In conclusion, we demonstrated here that centrally administered AngII acting on brain AT1 receptors induced Ad secretion from the rat adrenal medulla and pressor responses. These findings suggest a possibility that adrenomedullary outflow can be separately regulated by the central nervous system including brain angiotensinergic system, which can also modulate blood pressure.
Methods
Animals
All animal care and experiments were conducted in compliance with the guiding principles for the care and use of laboratory animals approved by Kochi University (No. G-5 and H-39) which are in accordance with the “Guidelines for proper conduct of animal experiments” from the Science Council of Japan. All studies involving animals are reported in accordance with the ARRIVE guidelines for reporting experiments involving animals. All efforts were made to minimize the suffering of the animals and the number of animals needed to obtain reliable results. A total of 60 animals were used in the experiments described here. Twelve-week-old male Wistar rats (Japan SLC Inc., Hamamatsu, Japan) weighing 300–350 g were housed at two per cage and were maintained in an air-conditioned room at 22–24°C under a constant day-night rhythm (14/10 h light-dark cycle, lights on at 05:00) for more than 2 weeks and given food (laboratory chow, CE-2; Clea Japan, Hamamatsu, Japan) and water ad libitum.
Experimental procedures for drug administration
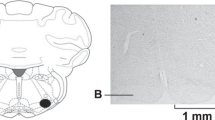
In the morning (09:00–10:00), under urethane anaesthesia (1.0 g kg−1, i.p.), the femoral vein was cannulated for saline infusion (1.2 ml h−1) and intravenous administration of drugs and the femoral artery was cannulated in order to collect blood samples. In some experiments, acute bilateral adrenalectomy [plus hydrocortisone (5 mg kg−1 per animal, i.m.)] or sham-operation (plus 200 μl saline per animal, i.m.) was done just before cannulation by an abdominal midline incision22,23. Subsequently, every rat was placed in a stereotaxic apparatus (SR-6R; Narishige, Tokyo, Japan) until the end of each experiment, as described in a published work of this laboratory51. The skull was drilled for intracerebroventricular administration of drugs using a stainless-steel cannula (outer diameter of 0.3 mm). The stereotaxic coordinates of the tip of the cannula were as follows (in mm): AP −0.8, L 1.5, V 4.0 (AP, anterior from the bregma; L, lateral from the midline; V, below the surface of the brain), according to the rat brain atlas52. Three hours were allowed to elapse before the application of drugs.
Drug administration in vivo
AngII dissolved in sterile saline was slowly administered into the right lateral ventricle at 10 μl per animal using a cannula connected to a 50-μl Hamilton syringe at a rate of 10 μl min−1 and the cannula was retained until the end of the experiment. Valsartan, an AT1 receptor blocker, or PD123319, an AT2 receptor blocker, dissolved in 3 μl of DMF or 5 μl of sterile saline, respectively, was i.c.v. administered using the cannula connected to a 10-μl Hamilton syringe at a rate of 10 μl min−1, which was retained in the ventricle for 15 min to avoid the leakage of these blockers and then removed from the ventricle. Subsequently, AngII was slowly administered as described above 30 min after the application of the blockers. When valsartan was i.v. injected, the drug dissolved in 1% DMF in saline (300 μl) was slowly injected via a cannula inserted into the femoral vein 30 min before the administration of AngII. The exact location of the cannula injected in the brain was confirmed at the end of each experiment by verifying that Cresyl Violet, injected through the cannula, had spread throughout the entire ventricular system.
Experimental groups for drug administration
The 60 rats placed in a stereotaxic apparatus were divided into 12 groups: AngII administered groups at 1 nmol per animal, i.c.v. (n = 5), at 3 nmol per animal, i.c.v. (n = 8) and 10 nmol per animal, i.c.v. (n = 5); vehicle corresponding to AngII administered group at 10 μl saline per animal, i.c.v. (n = 5); AngII (3 nmol per animal, i.c.v.) administered sham-operated group (n = 4); AngII (3 nmol per animal, i.c.v.) administered acute bilateral adrenalectomized group (n = 4); valsartan (100 nmol per animal, i.c.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 5); vehicle corresponding to valsartan (3 μl DMF per animal, i.c.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 5); PD123319 (100 nmol per animal, i.c.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 6); vehicle corresponding to PD123319 (5 μl saline per animal, i.c.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 4); valsartan (100 nmol per animal, i.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 4); vehicle corresponding to valsartan (300 μl 1% DMF in saline per animal, i.v.) and AngII (3 nmol per animal, i.c.v.) administered group (n = 5).
Measurement of plasma NA and Ad
Blood samples (250 μl) were collected through an arterial catheter at 0, 5, 10, 30, 60, 90 and 120 min after the administration of AngII or vehicle corresponding to AngII. The samples were preserved on ice during experiments. Plasma was prepared immediately after the final sampling. NA and Ad in the plasma were extracted by the method of Anton and Sayre53 with a slight modification and were assayed electrochemically with high performance liquid chromatography (HPLC)51. Briefly, after centrifugation (1500 × g for 10 min, at 4°C), the plasma (100 μl) was transferred to a centrifuge tube containing 30 mg of activated alumina, 1 ml of 0.5 M Tris buffer (pH 8.6) containing 0.03 M of disodium EDTA and 1 ng of 3,4-dihydroxybenzylamine as an internal standard. The tube was shaken for 30 min and the alumina was washed three times with 1 ml of ice-cold water deionized in a MilliQ water purification system (Millipore, Billerica, MA, USA). Then, NA and Ad adsorbed onto the alumina were eluted with 200 μl of 4% acetic acid containing 0.1 mM of disodium EDTA. A pump (EP-300: Eicom, Kyoto, Japan), a sample injector (AS-2050; JASCO, Tokyo, Japan) and an electrochemical detector (ECD-300: Eicom) equipped with a graphite electrode were used with HPLC. Analytical conditions were as follows: detector, +450 mV potential against an Ag/AgCl reference electrode; column, Eicompack CA-50DS, 2.1 mm × 150 mm (Eicom); mobile phase, 0.1 M NaH2PO4-Na2HPO4 buffer (pH 6.0) containing 50 mg l-1 disodium EDTA, 0.75 g l−1 sodium 1-octanesulfonate and 15% methanol at a flow rate of 0.5 ml min−1; injection volume, 100 μl. The amount of NA and Ad in each sample was calculated using the peak height ratio relative to that of 3,4-dihydroxybenzylamine. By this assay, coefficients of variation for the intra- and inter-assay were 3.0 and 3.7%, respectively and 0.5 pg of NA and Ad was accurately determined.
Primary culture of bovine adrenal chromaffin cells
Isolated bovine adrenal chromaffin cells were cultured (8 × l06 per dish, Falcon; 35 mm in diameter) under 5% CO2 and 95% air in a CO2 incubator in Eagle's minimum essential medium (Nissui Seiyaku, Tokyo, Japan) containing 10% calf serum and 3 μM cytosine arabinoside (Sigma-Aldrich, St. Louis, MO, USA) to suppress the proliferation of non-chromaffin cells54,55.
Measurement of secreted NA and Ad from the adrenal cells
Three days after plating, the bovine adrenal chromaffin cells were incubated with or without AngII (3.3 or 10 μM) for up to 120 min. Then, incubation medium was saved into a test tube for the NA and Ad assay by HPLC54,55.
Monitoring of blood pressure and heart rate
In rats administered valsartan intravenously, after cannulation and placement in a stereotaxic apparatus as described above, the cannula inserted into the femoral artery was connected to a pressure transducer (DX-100; Nihon Koden, Tokyo, Japan) that was connected to a carrier amplifier (AP-601G; Nihon Koden) and to a heart rate counter (AT-601G; Nihon Koden). The signals provided by the transducer were monitored by a personal computer (Macintosh G3, Apple Computer, Cupertino, CA, USA) through a multiport controller (PowerLab/8sp, AD Instruments, Castle Hill, Australia). The monitoring was started after the placement and was performed until 2 h after the administration of AngII described above. The pressure transducers were calibrated daily using a mercury manometer.
Treatment of data and statistics
All values are expressed as means ± s.e.m. Statistical differences were determined using repeated-measure (treatment × time) or one-way analysis of variance, followed by posthoc analysis with the Bonferroni method. When only two means were compared, an unpaired Student's t-test was used. P values less than 0.05 indicate statistical significance.
Drugs and chemicals
The following materials were used: synthetic AngII (Peptide Institute, Osaka, Japan); valsartan [(S)-3-methyl-2-[N-({4-[2-(2H-1,2,3,4-tetrazol-5-yl)phenyl]phenyl}methyl)pentanamido]butanoic acid] (Cayman Chemical, Ann Arbor, MI, USA); PD123319 (PD123319 ditrifluoroacetate) [(S)-1-[[4-(dimethylamino)-3-methylphenyl]methyl]-5-(diphenylacetyl)-4,5,6,7-tetrahydro-1H-imidazo[4,5-c]pyridine-6-carboxylic acid ditrifluoroacetate] (R&D Systems, Inc., Minneapolis, MN, USA). All other reagents were of the highest grade available (Nacalai Tesque, Kyoto, Japan).
References
Nishimura, H. Angiotensin receptors – evolutionary overview and perspectives. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 128, 11–30 (2001).
Fournier, D., Luft, F. C., Bader, M., Ganten, D. & Andrade-Navarro, M. A. Emergence and evolution of the renin-angiotensin-aldosterone system. J. Mol. Med. 90, 495–508 (2012).
Hendel, M. D. & Collister, J. P. Contribution of the subfornical organ to angiotensin II-induced hypertension. Am. J. Physiol. Heart Circ. Physiol. 288, H680–H685 (2005).
Stocker, S. D. & Toney, G. M. Median preoptic neurones projecting to the hypothalamic paraventricular nucleus respond to osmotic, circulating Ang II and baroreceptor input in the rat. J. Physiol. 568, 599–615 (2005).
Ganten, D., Hermann, K., Bayer, C., Unger, T. & Lang, R. E. Angiotensin synthesis in the brain and increased turnover in hypertensive rats. Science 221, 869–871 (1983).
Grobe, J. L., Xu, D. & Sigmund, C. D. An intracellular renin-angiotensin system in neurons: fact, hypothesis, or fantasy. Physiology 23, 187–193 (2008).
Song, K., Allen, A. M., Paxinos, G. & Mendelsohn, F. A. Mapping of angiotensin II receptor subtype heterogeneity in rat brain. J. Comp. Neurol. 316, 467–484 (1992).
Allen, A. M., O'Callaghan, E., Mendelsohn, F. A. & Chai, S. Y. [Intercellular Communication/Neuropeptides and neurotrophic factors/Neuronal angiotensin]. Encyclopedia of Neuroscience [Squire L. R. (ed.)] [697–702] (Oxford Academic Press, Oxford, 2009).
McKinley, M. J. et al. The brain renin-angiotensin system: location and physiological roles. Int. J. Biochem. Cell Biol. 35, 901–918 (2003).
von Bohlen und Halbach, O. & Albrecht, D. The CNS renin-angiotensin system. Cell Tissue Res. 326, 599–616 (2006).
Crowley, S. D. et al. Angiotensin II causes hypertension and cardiac hypertrophy through its receptors in the kidney. Proc. Natl. Acad. Sci. USA 103, 17985–17990 (2006).
Leenen, F. H. Actions of circulating angiotensin II and aldosterone in the brain contributing to hypertension. Am. J. Hypertens. 27, 1024–1032 (2014).
Grassi, G., Seravalle, G. & Quarti-Trevano, F. The 'neuroadrenergic hypothesis' in hypertension: current evidence. Exp. Physiol. 95, 581–586 (2010).
Ulrich-Lai, Y. M. & Herman, J. P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 10, 397–409 (2009).
McDougall, S. J., Widdop, R. E. & Lawrence, A. J. Central autonomic integration of psychological stressors: focus on cardiovascular modulation. Auton. Neurosci. 123, 1–11 (2005).
Esler, M. Heart and mind: psychogenic cardiovascular disease. J. Hypertens. 27, 692–695 (2009).
Saavedra, J. M. & Benicky, J. Brain and peripheral angiotensin II play a major role in stress. Stress 10, 185–193 (2007).
Chen, D. et al. Angiotensin type 1A receptors in C1 neurons of the rostral ventrolateral medulla modulate the pressor response to aversive stress. J. Neurosci. 32, 2051–2061 (2012).
Suzuki, T. & Kachi, T. Similarities and differences in supporting and chromaffin cells in the mammalian adrenal medullae: an immunohistochemical study. Anat. Rec. 244, 358–365 (1996).
Vollmer, R. R., Balcita, J. J., Sved, A. F. & Edwards, D. J. Adrenal epinephrine and norepinephrine release to hypoglycemia measured by microdialysis in conscious rats. Am. J. Physiol. 273, R1758–R1763 (1997).
Okada, S., Murakami, Y. & Yokotani, K. Role of brain thromboxane A2 in the release of noradrenaline and adrenaline from adrenal medulla in rats. Eur. J. Pharmacol. 467, 125–131 (2003).
Yokotani, K. et al. Brain prostanoid TP receptor-mediated adrenal noradrenaline secretion and EP3 receptor-mediated sympathetic noradrenaline release in rats. Eur. J. Pharmacol. 512, 29–35 (2005).
Shimizu, T. et al. Centrally administered histamine evokes the adrenal secretion of noradrenaline and adrenaline by brain cyclooxygenase-1- and thromboxane A2-mediated mechanisms in rats. Eur. J. Pharmacol. 541, 152–157 (2006).
Andersson, B. & Eriksson, L. Conjoint action of sodium and angiotensin on brain mechanisms controlling water and salt balances. Acta. Physiol. Scand. 81, 18–29 (1971).
May, C. N. & McAllen, R. M. Baroreceptor-independent renal nerve inhibition by intracerebroventricular angiotensin II in conscious sheep. Am. J. Physiol. 273, R560–R567 (1997).
Unger, T. et al. Differential effects of central angiotensin II and substance P on sympathetic nerve activity in conscious rats. Implications for cardiovascular adaptation to behavioral responses. Circ. Res. 56, 563–575 (1985).
Watson, A. M., Mogulkoc, R., McAllen, R. M. & May, C. N. Stimulation of cardiac sympathetic nerve activity by central angiotensinergic mechanisms in conscious sheep. Am. J. Physiol. Regul. Integr. Comp. Physiol. 286, R1051–R1056 (2004).
Mitchell, J. D., Maguire, J. J. & Davenport, A. P. Emerging pharmacology and physiology of neuromedin U and the structurally related peptide neuromedin S. Br. J. Pharmacol. 158, 87–103 (2009).
Sasaki, T., Shimizu, T., Wakiguchi, H. & Yokotani, K. Centrally administered neuromedin U elevates plasma adrenaline by brain prostanoid TP receptor-mediated mechanisms in rats. Eur. J. Pharmacol. 592, 81–86 (2008).
Usui, D. et al. Selective activation of the sympathetic ganglia by centrally administered corticotropin-releasing factor in rats. Auton. Neurosci. 146, 111–114 (2009).
Wright, J. W. & Harding, J. W. Brain renin-angiotensin–a new look at an old system. Prog. Neurobiol. 95, 49–67 (2011).
Davisson, R. L. Physiological genomic analysis of the brain renin-angiotensin system. Am. J. Physiol. Regul. Integr. Comp. Physiol. 285, R498–R511 (2003).
Sasamura, H. et al. Cloning, characterization and expression of two angiotensin receptor (AT-1) isoforms from the mouse genome. Biochem. Biophys. Res. Commun. 185, 253–259 (1992).
Burson, J. M., Aguilera, G., Gross, K. W. & Sigmund, C. D. Differential expression of angiotensin receptor 1A and 1B in mouse. Am. J. Physiol. 267, E260–E267 (1994).
Mayorov, D. N. Brain angiotensin AT1 receptors as specific regulators of cardiovascular reactivity to acute psychoemotional stress. Clin. Exp. Pharmacol. Physiol. 38, 126–135 (2011).
Gao, L. & Zucker, I. H. AT2 receptor signaling and sympathetic regulation. Curr. Opin. Pharmacol. 11, 124–130 (2011).
Blanch, G. T. et al. Increased Expression of Angiotensin II Type2 Receptors in the Solitary-Vagal Complex Blunts Renovascular Hypertension. Hypertension. 64, 777–783 (2014).
Criscione, L. et al. Pharmacological profile of valsartan: a potent, orally active, nonpeptide antagonist of the angiotensin II AT1-receptor subtype. Br. J. Pharmacol. 110, 761–771 (1993).
Blankley, C. J. et al. Synthesis and structure-activity relationships of a novel series of non-peptide angiotensin II receptor binding inhibitors specific for the AT2 subtype. J. Med. Chem. 34, 3248–3260 (1991).
Bosnyak, S. et al. Relative affinity of angiotensin peptides and novel ligands at AT1 and AT2 receptors. Clin. Sci. 121, 297–303 (2011).
Shapiro, J. S. et al. Cisterna magna cannulated repeated CSF sampling rat model–effects of a gamma-secretase inhibitor on Aβ levels. J. Neurosci. Methods. 205, 36–44 (2012).
Lenkei, Z., Palkovits, M., Corvol, P. & Llorens-Cortès, C. Expression of angiotensin type-1 (AT1) and type-2 (AT2) receptor mRNAs in the adult rat brain: a functional neuroanatomical review. Front. Neuroendocrinol. 18, 383–439 (1997).
Swanson, L. W. & Sawchenko, P. E. Paraventricular nucleus: a site for the integration of neuroendocrine and autonomic mechanisms. Neuroendocrinology 31, 410–417 (1980).
Jansen, A. S., Nguyen, X. V., Karpitskiy, V., Mettenleiter, T. C. & Loewy, A. D. Central command neurons of the sympathetic nervous system: basis of the fight-or-flight response. Science 270, 644–646 (1995).
Bains, J. S., Potyok, A. & Ferguson, A. V. Angiotensin II actions in paraventricular nucleus: functional evidence for neurotransmitter role in efferents originating in subfornical organ. Brain Res. 599, 223–229 (1992).
Northcott, C. A. et al. Adenoviral inhibition of AT1a receptors in the paraventricular nucleus inhibits acute increases in mean arterial blood pressure in the rat. Am. J. Physiol. Regul. Integr. Comp. Physiol. 299, R1202–R1211 (2010).
Chen, A., Huang, B. S., Wang, H. W., Ahmad, M. & Leenen, F. H. Knockdown of mineralocorticoid or angiotensin II type 1 receptor gene expression in the paraventricular nucleus prevents angiotensin II hypertension in rats. J. Physiol. 592, 3523–3536 (2014).
Ranson, R. N., Motawei, K., Pyner, S. & Coote, J. H. The paraventricular nucleus of the hypothalamus sends efferents to the spinal cord of the rat that closely appose sympathetic preganglionic neurones projecting to the stellate ganglion. Exp. Brain Res. 120, 164–172 (1998).
Hardy, S. G. Hypothalamic projections to cardiovascular centers of the medulla. Brain Res. 894, 233–240 (2001).
Oldfield, B. J. et al. Efferent neural projections of angiotensin receptor (AT1) expressing neurones in the hypothalamic paraventricular nucleus of the rat. J. Neuroendocrinol. 13, 139–146 (2001).
Shimizu, T., Okada, S., Yamaguchi-Shima, N. & Yokotani, K. Brain phospholipase C-diacylglycerol lipase pathway is involved in vasopressin-induced release of noradrenaline and adrenaline from adrenal medulla in rats. Eur. J. Pharmacol. 499, 99–105 (2004).
Paxinos, G. & Watson, C. The Rat Brain in Stereotaxic Coordinates [Paxinos G., & Watson C. (ed.)] (Elsevier Academic Press, Burlington, 2005).
Anton, A. H. & Sayre, D. F. A study of the factors affecting the aluminum oxide-trihydroxyindole procedure for the analysis of catecholamines. J. Pharmacol. Exp. Ther. 138, 360–375 (1962).
Yanagita, T. et al. Chronic lithium treatment up-regulates cell surface NaV1.7 sodium channels via inhibition of glycogen synthase kinase-3 in adrenal chromaffin cells: enhancement of Na+ influx, Ca2+ influx and catecholamine secretion after lithium withdrawal. Neuropharmacology 57, 311–321 (2009).
Yanagita, T. et al. Transcriptional up-regulation of cell surface NaV1.7 sodium channels by insulin-like growth factor-1 via inhibition of glycogen synthase kinase-3β in adrenal chromaffin cells: enhancement of 22Na+ influx, 45Ca2+ influx and catecholamine secretion. Neuropharmacology 61, 1265–1274 (2011).
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research (C) (No. 26460909 to T.S.) and a Grant-in-Aid for Young Scientists (B) (No. 23790744 to T.S. and No. 26861271 to S.S.) from the Japan Society for the Promotion of Science, a grant from The Smoking Research Foundation in Japan, a grant from The Japan Health Foundation and a Discretionary Grant of the President of Kochi University.
Author information
Authors and Affiliations
Contributions
T.S. and M.S. developed the concept and designed the study. K.N. and T.S. conducted experiments of measurement of rat plasma NA and Ad, blood pressures and heart rate. K.N., T.S. and M.S. conducted statistical analysis of the rat data. T. Yanagita and T.N. conducted experiments of measurement of NA and Ad secreted from the bovine adrenal chromaffin cells and statistically analysed the data obtained from the cells. T.S., K.T., S.S., F.D., T. Yawata, Y.H., T.U. and M.S. performed critical revision of the manuscript for important intellectual content. All authors contributed to the conceptual analysis and writing of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Nakamura, K., Shimizu, T., Yanagita, T. et al. Angiotensin II acting on brain AT1 receptors induces adrenaline secretion and pressor responses in the rat. Sci Rep 4, 7248 (2014). https://doi.org/10.1038/srep07248
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07248
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.