Abstract
Accurate continuous direct measurement of the blood pressure is currently available thru direct invasive methods via intravascular needles and is mostly limited to use during surgical procedures or in the intensive care unit (ICU). Non-invasive methods that are mostly based on auscultation or cuff oscillometric principles do provide relatively accurate measurement of blood pressure. However, they mostly involve physical inconveniences such as pressure or stress on the human body. Here, we introduce a new non-invasive mechanism of tissue-informative measurement, where an experimental phenomenon called subcutaneous tissue pressure equilibrium is revealed and related for application in detection of absolute blood pressure. A prototype was experimentally verified to provide an absolute blood pressure measurement by wearing a watch-type measurement module that does not cause any discomfort. This work is supposed to contribute remarkably to the advancement of continuous non-invasive mobile devices for 24-7 daily-life ambulatory blood-pressure monitoring.
Similar content being viewed by others
Introduction
Blood pressure is the pressure exerted by the circulating blood against vessel walls and is a vital sign in clinical assessments. It is used to clarify conditions of the cardiovascular system. For example, hypertension can result in strokes, heart attack, heart failure, aka ‘end-organ damage’ phenomena1 that are critical factors leading to potential lethal conditions. Conversely, hypotension can cause dizziness, fainting and endocrine or neurological disorders. Blood pressure is also crucial in other diseases such as diabetes mellitus. Lastly, blood pressure is also a useful indicator of normal cardiovascular conditions. With these considerations in mind, the continuous monitoring of blood pressure can lead to early discovery or at least immediate treatment of various cardiovascular diseases. Meanwhile, in cases of cardiovascular symptoms such as irregular heartbeat and arrhythmia, it is often difficult to discover a symptom with only a regular visit to the clinic. Moreover, at times during a clinic visit, blood pressure readings may be at variance from normal for psychological reasons, a condition known as ‘white-coat’ hypertension. As such, there is considerable interest in continuous Ambulatory Blood Pressure Monitoring (ABPM) technology2 to continuously monitor blood pressure over the full course of a day.
Currently, the most accurate continuous blood pressure measurement is an invasive method3 that is used only for limited cases with critical needs, such as during surgery. In this invasive method, direct measurement of the blood pressure is possible through the electronic pressure transducer in an intravascular cannula needle inserted into a vein. However, due to potential complications such as thrombosis, infection and bleeding3, even during a surgical procedure, the use of this invasive method is limited. As such, for daily monitoring purposes, a non-invasive ABPM method4 is much preferred over the invasive method. To date, ABPM devices are mostly based on auscultation5 or cuff oscillometry6 principles, both of which can be classified as occlusive technologies7 that use cuffs and are non-continuous and originally devised by Korotkoff. Some drawbacks of these occlusive methods include petechiae, bruising and even sleep disorders. As a result, this method is not recommended for use more than 5 to 8 times a day and would not be suitable for continuous blood pressure monitoring. Recently, semi-occlusive technologies have been developed to overcome the drawbacks of cuff-based occlusive technology. A volume clamp8 and tomometry9 are the most representative examples of these methods. These technologies, however, suffer from accuracy and reproducibility problems when tested against international standards10,11,12,13. The volume clamp method utilizes a cuff on a finger, while the tonometry approach requires sensors to have firm contact with the skin in order to touch a radial artery. These approaches continue to be insufficient for continuous ABPM functionality14,15,16.
As described above, there has been extensive research into continuous ABPM. Most previous approaches, however, came along with partial pain and non-continuity. In addition, the acquired waveform may have been proportional to the blood pressure while the methodology to acquire absolute blood pressure values was not fully developed. As such, in this paper, a new continuous blood pressure monitoring method, based on a newly discovered phenomenon and hypotheses, was proposed for continuous non-invasive ABPM (CNI-ABPM) that does not produce any discomfort or require the use of any cuffs. Through a prototype implementation and its measurement, the proposed method was verified to achieve meaningful accuracy correlation with respect to a validated commercial device.
Results
Principle of tissue-informative blood pressure detection
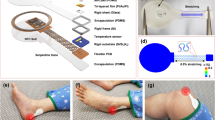
To minimize the inconvenience of existing blood-pressure measurement methods, the proposed approach tries to simplify the acquisition process of human physiological signals and devises a new signal processing algorithm that can extract absolute blood pressure values from these measured physiological data. Our experimental environment is illustrated in Fig. 1, where the acquisition process is done by locating a pressure sensor onto the wrist near the radial artery. A pressure sensor translates the radial pulse (P) into a voltage signal and a readout circuit filters out environmental noises and amplifies the desired signal, finally generating a digitized output of Y. The average value, Yavg in Fig. 1a corresponds to the average pressure delivered to the skin, which is equal to the sum of the atmosphere pressure (Patm), external pressure applied by a measurement module (Ppress) and the average blood pressure delivered from the radial artery to the skin (HST·Xavg). Y's peak-to-peak amplitude, ΔY is normally proportional to the strength of the radial pulse wave. But with these values of ΔY and Yavg, it can measure only the external applied pressure Ppress and the radial pulse wave delivered to the skin (Y), not the absolute blood pressure inside the radial artery (X).
Principle of tissue-informative blood-pressure measurement.
(a) Structural view of tissue-informative measurement in blood pressure (BP) of the radial artery. X is radial artery's pressure, P is pressure input to the pressure sensor and Y is the final digitized output of the measurement module. (b) Vertical view from the skin to the radial artery. Subcutaneous tissue is sandwiched in-between the radial artery's blood pressure and external atmospheric pressure. (c) Spring and dashpot model to mimic the BP measurement.
To address this, we found an innovative experimental phenomenon, which we call “subcutaneous tissue pressure equilibrium (STPE),” that is applicable to absolute blood pressure detection. After observing radial skin dynamics with the radial artery under the atmosphere, we hypothesized that the radial skin with a radial artery of average blood pressure would be in an equilibrium state with atmospheric pressure. In addition, we further hypothesized that the pressure equilibrium would be sustained with the pressure sensor on it even under other pressure balance changes, since the subcutaneous tissue area (HST) would be re-organized to balance the external pressure and the internal pressure from the average radial artery pressure. With these hypotheses, we tried the following experiments.
If the external applied pressure of Ppress increases, the amplitude of the detected AC signal ΔY also increases proportionally, resulting in the straight line ΔY-Ppress characteristic as shown in Fig. 2a. This is mainly due to the reduction of the propagation distance from the radial artery to the skin, i.e., a larger HST. We found an important experimental phenomenon in that the slope of the ΔY-Ppress line is proportional to the average blood pressure of the measured human, called the mean arterial pressure (Xavg). That is, a higher Xavg gives a bigger slope and a lower Xavg makes the slope smaller. This experimental proof is rearranged in Fig. 2b. This experimental result implies that if the subcutaneous tissue (HST) area between the radial artery and the skin counteracts both the radial blood pressure and the atmospheric pressure for long time as in Fig. 1b, the transfer function of the tissue tends to be adaptively changed to acquire the other pressure equilibrium. In the case of hypertensive persons with higher Xavg, their tissue has been exposed to a higher radial artery pressure and the delivering characteristic of the radial pulse tends to be more sensitive, giving bigger slope of the ΔY-Ppress line.
The STPE experimental phenomenon is theoretically analyzed by utilizing an intuitive modeling method proposed in Ref. 17. Fig. 1b shows a vertical view from the skin to the radial artery and its equivalent spring and dashpot model is presented in Fig. 1c. Springs S1 and S4 model the radial artery and the pressure sensor with spring constants k1 and k4 representing their stiffness. The wall of the radial artery and the subcutaneous tissue are modeled as parallel configuration of a spring S3 and a dashpot D2. According to its mathematical analysis whose details are given in the supplementary method section, the stiffness of the tissue and the artery wall (k3) is directly related to their transfer efficiency of the original blood pressure. If this analysis result is combined with the experimental phenomenon in Fig. 2, it concludes that higher Xavg increases the k3 value and thereby improves the transfer efficiency, which results in bigger line slope of the ΔY-Ppress characteristic.
Recursive tracking of blood pressure
Based on this tissue-informative detection principle, an average blood pressure Xavg can be found by measuring ΔY variations with respect to various Ppress values, that is, the ΔY-Ppress slope. Only if the slope and Xavg are measured, the peak-to-peak value of the absolute blood pressure (ΔX) can be detected following the calculation process shown in Fig. S1. Since the average and the peak-to-peak value are directly related with the maximum and the minimum values, the systolic pressure (Xmax) and the diastolic pressure (Xmin) are easily derived from the measured values of Xavg and ΔX. Nevertheless, human blood pressure undergoes many instant variations, called human artifacts and environmental atmospheric pressure also easily changes. Therefore, these instant variations necessitate a kind of tracking mechanism for better measurement. Fig. 3 shows the concept of a proposed real-time measurement algorithm, called “recursive tracking”.
Recursive tracking of blood-pressure measurement.
(a) Real-time slope tracking process in ΔY versus Ppress plot. The line slope is cumulatively updated by last measured value. (b) Reconstruction process of radial artery's blood pressure (i.e., systolic pressure Xmax and diastolic pressure Xmin) corresponding to updated Xavg which is calculated from ΔY-Ppress line slope.
After wearing our watch-type measurement device as shown in Fig. S2b, the average blood pressure of Xavg is cumulatively updated depending on instant small variations of Ppress and then the resulting systolic and diastolic pressures are also cumulatively adapted. Unlike existing occlusive measurement devices that add an uncomfortable physical pressure on the body, this recursive tracking method allows continuous absolute blood pressure measurements and enables most comfortable solution for the CNI-ABPM.
Continuous non-invasive ambulatory blood pressure monitoring
An overall system and its service scheme is illustrated in Fig. S2a, where the CNI-ABPM function is compactly implemented as a type of watch device and wireless technologies such as Bluetooth and cellular communications are included to maximize portability. The watch-type CNI-ABPM module acquires the radial pulse wave and its digitized information is transferred to a smart phone. Then the absolute blood pressure acquisition and recursive tracking functions are performed by utilizing a microprocessor inside the smart phone. Acquired blood pressure information, including the systolic and the diastolic pressure, is displayed on the smart phone and also can be delivered to medical institutions through a cellular network and the Internet. By transferring the processing burden of the pressure acquisition and the recursive tracking from the module to the smart phone, the CNI-ABPM module could be miniaturized and also very comfortable to wear during 24-hour monitoring. Fig. S2b shows a prototype of the CNI-ABPM module, which mainly consists of a pressure sensor, readout circuits and Bluetooth module. The pressure sensor measures the physical pressure amount and generates its corresponding voltage. This voltage signal is amplified and digitized in the readout circuits. Then this acquired digital sensor information is wirelessly transmitted to the smart phone though the Bluetooth module. A bubble cap is located between the skin and the pressure sensor to improve the transfer efficiency of the radial pulse wave and to also make wearing of the device more comfortable.
International validation standards from the British Hypertension Society18 (BHS), the Association for the Advancement of Medical Instrumentation19,20 (AAMI) and the Working Group on Blood Pressure Monitoring of the European Society of Hypertension21,22,23,24 (ESH) should follow strict procedures and also require well-trained experts for manual sphygmomanometers. Moreover, the gold standard for continuous blood pressure measurement, the invasive intravascular method requires expensive surgical actions with potential complications25. Therefore, for accuracy verification of the proposed CNI-ABPM mechanism, a brief measurement and analysis method of randomized crossover25 with an automated validated device as the reference was adopted to collect many experimental data effectively. The implemented prototype device was compared with a commercial non-invasive automated oscillometric product UA-767 from A&D Medical which is validated with protocols set by organization such as the BHS, the AAMI and the ESH. Two hundred adults are included in this crossover measurement. Measured Bland-Altman plots25 which graphically represent limits of agreements are given in Fig. 4. In case of the systolic blood pressure (SBP), its mean difference and standard deviation was 1.1 mmHg and 4.7 mmHg respectively. The diastolic blood pressure (DBP) showed mean difference of −1.9 mmHg and standard deviation of 4.4 mmHg. The recruited subjects presented the SBP range of 87–164 mmHg and the DBP range of 48–133 mmHg. Considering that the measured crossover experimental results are comparable to the AAMI accuracy criteria which are mean value of less than 5 mmHg and standard deviation of less than 8 mmHg, the crossover experiment on the accuracy in blood pressure measurement shows close correlation between the proposed device and the validated commercial product.
Discussion
Many measurement technologies to monitor radial pulse waves utilize simple contact of pressure sensors to the skin, but they do not measure absolute blood pressures. Most validated methods that provide absolute pressures correspond to occlusive technology using a cuff and they are fundamentally based on Korotkoff's sound detection or cuff oscillometry which are not appropriate for continuous ABPM. Among advanced semi-occlusive technologies that reduce the inconvenience of the cuff, volume clamp technology is supposed to be the only unsupervised method for continuous non-invasive blood pressure measurement. It is recognized now, however, that this does not fulfill the BHS nor AAMI standard criteria. Recently a watch-type measurement device using tonometry technology was announced27. This device, however, requires periodic calibrations to other cuff-based oscillometric device for accuracy compensation and may also give relatively high pressure reading or add stress on the skin during the tonometry operation. Whereas, our proposed technology does not create any inconvenience or stress and it provides comfortable blood pressure measurement to facilitate 24-hour continuous non-invasive ABPM.
The STPE phenomenon and the proposed tissue-sensitive mechanism were theoretically modeled and analyzed through the spring and dashpot model which is adopted from a radial-artery tonometry model17 thanks to their similar physical structures. The analysis result revealed that the absolute blood pressure measurement can be achieved by utilizing the STPE phenomenon while the tonometry can detect only relative blood pressure signals delivered from the radial artery. The proposed tissue-informative detection method based on this STPE phenomenon was implemented in the form of app software programming inside smart phones, which minimizes the hardware burden of the sensor module and makes very small and comfortable to wear. Another important implementation technology is a measurement tracking function. To acquire the absolute blood pressure value, our detection method utilizes external pressure from the module to the skin which varies continuously. Whereas most other products use a cuff for similar purposes, our prototype adopted a recursive-tracking algorithm that was also implemented in the app software. As such, our blood pressure module was able to eliminate the cuff and its associated inconveniences that would limit continuous ABPM.
Methods
Absolute blood pressure detection
An implemented watch-type CNI-ABPM module acquires an instant radial pulse signal through a pressure sensor and readout circuits and sends it to a smart phone. Based on this real-time measured radial pulse data, the ΔY-Ppress curve of Fig. 3 is constructed continuously. As in Fig. S1, the relationship between its slope and average blood pressure (Xavg) is given by Xavg = (Slope/HSMΔXpre − HST0)/k and the peak-to-peak value of blood pressure (ΔX) is ΔX = ΔY /(HST0 + kXavg)HSM (Ppress + Patm), where ΔXpre is previous value of ΔX in the recursive algorithm and k is a constant value experimentally determined. These detection procedures and relationships are implemented in the form of app software on a smart phone, resulting in real-time continuous measurement of absolute blood pressure.
Extraction of systolic and diastolic blood pressures
According to the proposed blood pressure measurement procedure, the average (Xavg) and the peak-to-peak value (ΔX = Xmax − Xmin) are found first. Then systolic pressure (Xmax) and diastolic pressure (Xmin) are calculated by using the relationship of Xavg = (αXmax + βXmin)/(α + β). That is, Xmax = Xavg + βΔX/(α + β) and Xmin = Xavg − αΔX/(α + β), where α = 1 and β = 2 for normal blood pressure. This calculation is also implemented inside the smart phone.
Accuracy verification
Commercial blood pressure devices are usually validated with protocols set by international standards such as the BHS, the AAMI and the ESH. Both the BHS and the ESH validates the accuracy grade of commercial devices and their grading criteria are composed of cumulative percentage of difference readings falling within 5 mmHg, 10 mmHg and 15 mmHg18,21. The AAMI suggests statistical criteria that the mean difference and its standard deviation should be less than 5 mmHg and 8 mmHg respectively19,20. Since this work pursues accuracy verification of a new detection method, not validation of commercial devices, the accuracy correlation with other validated commercial device is performed. As the correlation standard, the AAMI criteria were adopted because it is more intuitive and convenient for accuracy comparison between two different measurement devices. A prototype device based on the proposed mechanism is compared with an automated oscillometric commercial device UA-767 and their accuracy correlation is investigated whether it meets the AAMI criteria or not. This study was approved by the institutional review board at Ulsan National Institute of Science and Technology and all experiments were performed in accordance with the approved guidelines. Two hundred adults were recruited in the crossover measurement and informed consent was obtained from all subjects. Every subject is seated with legs uncrossed and arm supported at heart level and two measurements per each device are performed. If two measured values are not correlated, another measurement is made. Then, the average of two correlated measurements is recorded as the measured result. Finally, the correlation between two devices is evaluated by the mean difference and its standard deviation and graphically presented with Bland-Altman plots of the SBP and the DBP where the x-axis is the average of measured blood pressures by two devices and the y-axis is their corresponding difference26.
References
Luft, F. C. et al. Hypertension-induced end-organ damage. Hypertension 33, 212–219 (1999)
McGrath, B. P. Ambulatory blood pressure monitoring. MJA 176, 588–592 (2002).
Gupta, B. Invasive blood pressure monitoring. Update in Anaethesia 28, 37–42 (2012).
Sykes, M. K. et al. Principles of measurement and monitoring in Anaesthesia (Blackwell Science Publications, 1992).
Pickering, T. G. et al. Recommendations for blood pressure measurement in humans and experimental animals: Part1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 45, 142–161 (2005).
Ramsey, M. Blood pressure monitoring: automated oscillometric devices. J Clin Monit 7, 55–67 (1991).
Geddes, L. A. Handbook of Blood Pressure Measurement (Humana Press, 1991).
Imholz, B. P. et al. Fifteen years experience with finger arterial pressure monitoing: assessment of the technology. Cardiovasc Res 38, 605–616 (1998).
Drzewiecki, G. M. et al. Arterial tonometry: review and analysis. J Biomech 16, 141–152 (1983).
Matthys, K. & Verdonck, P. Development and modeling of arterial applanation tonometry: a review. Technol Health Care 10, 65–76 (2002).
Belani, K. et al. A new noninvasive method to measure blood pressure: results of a multicenter trial. Anesthesiology 91, 686–692 (1999).
Birch, A. A. & Morris, S. L. Do the Finapres and Colin radial artery tonometer measure the same blood pressure changes following deflation of thigh cuffs? Physiol Meas 24, 653–660 (2003).
Ristuccia, H. L. et al. Incremental bias in Finapres estimation of baseline blood pressure levels over time. Caridiovasc Res 38, 605–616 (1998).
Cua, C. L. et al. A comparison of the Vasotrac with invasive arterial blood pressure monitoring in children after pediatric cardiac surgery. Anesth Analg 100, 1289–1294 (2005).
Lindqvist, A. Beat-to-beat agreement of non-invasive finger artery and invasive radial artery blood pressure in hypertensive patients taking cardiovascular medication. Clin Physiol 15, 219–229 (1995).
Imholz, B. P. et al. Continuous finger arterial pressure: utility in the cardiovascular laboratory. Clin Auton Res 1, 43–53 (1991).
Birch, T. et al. Continuous non-invasive blood-pressure measurements. Report of 7th UK Mathematics in Medicine Study Group. http://www.maths-in-medicine.org/uk/2007/blood-pressure/report.pdf (2007). Date of access: 20/09/2014.
O'Brien, E. et al. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British hypertension society. BMJ 320, 1128–1134 (2000).
Association for the Advancement of Medical Instrumentation. American National Standard ANSI/AAMI SP10:2002. Manual, Electronic, or Automated Sphygmomanometers. AAMI: Arlington, VA (2003) [a published amendment appeared as ANSI/AAMI SP10: 2002/A1:2003].
American National Standard for Non-Invasive Sphygmomanometers-part 2: Clinical Validation of Automated Measurement Type. ANSI/AAMI/ISO 81060-2, pp. 25–256 (2009).
O'Brien, E. et al. European Society of Hypertension International Protocol revision 2010 for the validation of blood pressure measuring devices in adults. Blood Press Monit 15, 23–38 (2010).
Mancia, G. et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28, 1462–1536 (2007).
O'Brien, E. et al. Working Group on Blood Pressure Monitoring of the European Society of Hypertension International Protocol for validation of blood pressure measuring devices in adults. Blood Press Monit 7, 3–17 (2002).
O'Brien, E. et al. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ 322, 531–536 (2001).
Ribezzo, S. et al. Noninvasive techniques for blood pressure measurement are not a reliable alternative to direct measurement: a randomized crossover trial in ICU. ScientificWorldJournal 2014, Article ID 353628, 10.1155/2014/353628 (2014).
Bland, J. M. et al. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1, 307–310 (1986).
Nair, D. et al. The use of ambulatory tonometric radial arterial wave capture to measure ambulatory blood pressure: the validation of a novel wrist-bound device in adults. J Hum Hypertens 22, 220–222 (2008).
Author information
Authors and Affiliations
Contributions
S.H.W., Y.Y.C. and J.J.K. conceived and verified the concept and analyzed experimental results. Y.Y.C. and D.J.K. have contributed to development of the software. Y.Y.C., D.J.K., S.H.W., F.B. and J.J.K. have contributed to implementation of the hardware. J.J.K., F.B. and S.H.W. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Supplementary Information
Supplementary Video
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Woo, S., Choi, Y., Kim, D. et al. Tissue-Informative Mechanism for Wearable Non-invasive Continuous Blood Pressure Monitoring. Sci Rep 4, 6618 (2014). https://doi.org/10.1038/srep06618
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06618
This article is cited by
-
On the development of low power wearable devices for assessment of physiological vital parameters: a systematic review
Journal of Public Health (2023)
-
Cerebral blood volume and oxygen supply uniformly increase following various intrathoracic pressure strains
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.