Abstract
Cancer is a leading cause of death worldwide. Because the cytotoxic effects of conventional chemotherapies often harm normal tissue cells along with cancer cells, conventional chemotherapies cause many unwanted or intolerable side effects. Thus, there is an unmet medical need to establish a paradigm of chemotherapy-induced differentiation of cancer cells with tolerable side effects. Here we show that low-dose metformin or SN-38 inhibits cell growth or survival in ovarian and breast cancer cells and suppresses their tumor growth in vivo. Low-dose metformin or SN-38 increases FOXO3 nuclear localization as well as the amount of DNA damage markers and downregulates the expression of a cancer-stemness marker CD44 and other stemness markers, including Nanog, Oct-4 and c-Myc, in these cancer cells. This treatment also inhibits spheroid body-formation in 3-dimensional culture. In contrast, silencing FOXO3 diminishes all these cellular events when ovarian/breast cancer cells are treated with the mentioned drugs. These results suggest that low-dose metformin or SN-38 may reprogram these cancer cells into non-cancerous cells in a FOXO3-dependent manner and may allow patients to overcome these cancers with minimal side effects.
Similar content being viewed by others
Introduction
Cancer remains one of the most frequent causes of death (approximately 7.6 million cancer deaths in 2008) worldwide1. Conventionally, chemotherapeutic compounds treat cancers by suppressing cancer cell survival or by inducing cellular apoptosis through the compounds' cytotoxic characteristics2. Because normal tissue cells also absorb these compounds, normal tissue cells experience the cytotoxic effects, thus leading to undesirable and sometimes intolerable side effects in cancer patients. Therefore, it is necessary to develop a chemotherapeutic approach with fewer or more tolerable side effects. To address this concept, it is plausible to display such a prototype of chemotherapy not by harming or killing cancer cells and cancer stem cells (CSC)3,4 but by altering their cell fate to become non-cancerous cells or normal-like tissue stem cells (NTSC). For instance, an emerging concept in differentiation therapy has been suggested by a notable publication5, where knockdown of CD44 in breast cancer stem cells results in the cells taking on non-stem cell characteristics. Since this therapeutic approach will not harm or destroy cancer cells or normal tissue cells, this type of treatment is expected to cause fewer or tolerable side effects in patients after treatments. By using low doses of unique small-molecule drugs, we have designed a strategy to induce reprogramming of cancer cells or CSC into non-cancerous cells or NTSC.
Ovarian cancer (OvCa) is the leading cause of gynecologic cancer deaths and breast cancer (BCa) is the most common malignancy in women in the United States (U.S.)6. Many patients with advanced OvCa or BCa will eventually experience a recurrence of the cancer, which often has lost its original chemo-sensitivity, thus leading patients to succumb to the disease7,8. In spite of recent advances in the chemotherapy of OvCa or BCa, the development of a therapeutic approach with minimal side effects that potentially prevents cancer recurrence is certainly needed. For instance, metformin has recently gained widespread attention for its anticancer properties. Metformin (N',N'-dimethylbiguanide) is an anti-hyperglycaemic drug commonly used for the management of type-2 diabetes9. The glucoregulatory properties of metformin are primarily attributed to the reduction of hepatic glucose production and the augmentation of glucose uptake by peripheral tissues such as skeletal muscle9. It has been shown that the activation of adenosine monophosphate (AMP)-activated protein kinase (AMPK) is necessary for metformin's effect on suppressing glucose production by hepatocytes9,10. These results suggest that AMPK may play an essential role in regulating metformin's activity in cells.
In contrast to the widespread documentation of the mechanisms underlying metformin's therapeutic effects for diabetes, the molecular mechanisms underlying metformin's biological activities that are related to cancer treating activities have not been fully elucidated. Interestingly, two independent clinical studies have shown that metformin may reduce the risk of cancer in patients with type II diabetes11,12. This is consistent with the effect of metformin on suppressing the spontaneous development of breast tumors in HER-2/neu-transgenic mice13 as well as the induction of pancreatic cancer in the hamster models14. However, it is not clear whether the observed effects were due to the drug's direct activity on the tumor cells or if the effects resulted from the drug's regulation on insulin metabolism. It is well known that hyperinsulinemia and its associated metabolic alterations, which are corrected by metformin treatment, may play a role in the onset of some malignancies such as BCa15. The capacity of metformin to block proliferation of human BCa cells16 or cause apoptotic cell death in a mouse insulinoma cell line17 supports direct tumor suppression action, but the underlying mechanisms are not completely understood. Through the development of novel anticancer compounds, we have unexpectedly identified metformin as an anticancer agent that can induce FOXO3 activity.
FOXO3 is a key transcription factor that controls the transcription of a number of genes crucial for regulating cell cycle control18, DNA damage and stress responses19,20,21,22, aging and longevity23,24, cellular apoptosis25,26,27 and suppression of cancer28,29,30,31 in animal and human cells. Gene knockout findings reveal FOXOs' vital functions in tumor suppression32 and the maintenance of the hematopoietic stem cell pool33. While multiple mechanisms have been shown to regulate FOXO3 activity, phosphorylation inhibits FOXO3 nuclear translocation that is central for its regulation and function. This nuclear exclusion and translocation of FOXO3 into the cytoplasm inhibits FOXO3-dependent transcription. Loss of function of FOXO3 has been linked to tumorigenesis and poor patient survival in BCa28,30,31 and OvCa34 suggesting that FOXO3 is a pivotal tumor suppressor.
Previously we have identified camptothecin, a topoisomerase-1 inhibitor, as an anticancer small molecule that can potently promote FOXO3 activity in cancer cells21. Irinotecan (CPT-11), a camptothecin derivative, exerts an anticancer effect on several types of cancer35 and is recommended by national guidelines as first or second line treatment for metastatic colorectal cancer in both Europe and the U.S.36,37. Irinotecan is a prodrug that requires carboxylesterases for conversion to the active metabolite SN-38 (7-Ethyl-10-hydroxycamptothecin), which is 100- to 1000-fold more active than irinotecan38,39. However, the effect of low-dose SN-38 on OvCa and BCa cells has not been investigated and the functional role of low-dose SN-38's in the suppression of OvC and BCa development or progression has not been deciphered.
Here we show that low-dose metformin or SN-38 suppresses OvCa and BCa cell growth in vitro and in vivo as well as the formation of 3-dimensional (3D) tumor-like spheroids in 3D culture. Low-dose metformin or SN-38 also increases FOXO3 nuclear localization and reduces the expression of the stemness markers in these cancer cells in a FOXO3-dependent manner. Collectively, our results suggest that these small-molecule drugs may promote the reprogramming of OvCa/BCa cells into their perspective non-cancerous cells. The important biological and pathological significance of this mechanism in cancer therapy is discussed.
Results
Low-dose metformin or SN-38 suppresses OvCa and BCa cell growth or survival in vitro and their tumor growth in vivo
To examine the effect of metformin or SN-38 on cell growth or survival (growth/survival), we treated human OVCA429 OvCa and BT-549 BCa cells with low doses of metformin (100 μM) or SN-38 (1 nM) or DMSO (negative control) and analyzed their cell growth/survival rates using cell counting. We showed that metformin or SN-38 treatment significantly reduced the cell growth/survival rates of OVCA429 and BT-549 cells 72 hours post drug treatment (Fig. 1A).
Low-dose metformin or SN-38 suppresses OvCa and BCa cell growth or survival in vitro and their tumor growth in vivo.
(A) OVCA429 OvCa and BT549 BCa cells were grown in DMEM/F12 culture medium and treated with low doses of metformin (100 μM), SN-38 (1 nM) and the vehicle control (DMSO) for 72 hours. The growth/survival rates of cells were measured by cell counting and are shown as the percentage relative to the survival rate of the negative control. *, P < 0.01. The significant P values between the control group and the test groups treated with drugs are indicated. The number of biological replicates is three, the error bars represent SD and the statistical test is the two-sided unpaired Student's t tests. (B) OVCA429 cells were injected into female nude mice subcutaneously (n = 4/group). When palpable tumors were detected, the mice were given an intravenous injection of metformin [5 mg/kg BW], SN-38 (10 μg/kg BW), or the vehicle control (DMSO) twice per week. The tumor volumes were measured twice a week and graphed as mean values of volume with standard deviation. The significant P values (*, P < 0.05) between the control and the groups treated with metformin or SN-38 are indicated. (C) Similarly, MDA-MB-231 BCa cells were injected into female nude mice subcutaneously (n = 4/group). The tumor-bearing mice were given an intravenous injection of metformin (5 mg/kg BW) or DMSO twice per week and the tumor volumes were determined twice per week and displayed as described above.
To determine if treatment with low doses of metformin or SN-38 can suppress tumorigenesis or tumor growth in OvCa cells in vivo, we injected OVCA429 OvCa cells into the flanks of female athymic nude mice. When palpable solid tumors were detected, the tumor-bearing mice were given an intravenous (i.v.) injection (0.1 ml) of metformin [5 mg/kg body weight (BW) per mouse], SN-38 (10 μg/kg BW/mouse), or the vehicle (DMSO, negative control) three times per week at even intervals for 7 weeks. The tumor volumes were measured twice per week after the treatment. Our results show that low-dose metformin or SN-38 significantly suppressed OVCA429 ovarian tumor growth in the mouse model (Fig. 1B). Similarly, we injected MDA-MB-231 BCa cells into the flanks of female nude mice and treated the tumor-bearing mice with metformin (5 mg/kg BW/mouse). Our data suggest that low-dose metformin suppressed MDA-MB-231 breast tumor growth in the mouse model (Fig. 1C). Taken together, these results suggest that low-dose metformin or SN-38 can suppress cell proliferation and tumor growth in human OvCa and BCa cells in vivo.
Low-dose metformin or SN-38 induces FOXO3 nuclear localization and phosphorylation of DNA damage markers in OvCa and BCa cells
An important question in determining the mechanism for suppressing cell growth is how low doses of metformin or SN-38 contribute to the observed suppression of cell proliferation and tumor growth in OvCa and BCa cells. Since it is known that FOXO3 can regulate cell cycle control18 and that activation of FOXO3 can promote DNA damage repair response20,21, we sought to determine whether low-dose Metformin or SN-38 could induce FOXO3 activation as well as DNA damage response in OvCa and BCa cells. We treated OVCA429 cells with low doses of metformin or control (sterile H2O) for 24 hours and analyzed the subcellular localization of FOXO3 as well as the phosphorylation of DNA damage markers in these cells using immunofluorescence analysis. Our results indicate that low doses (such as 10 μM) of metformin promoted nuclear localization of FOXO3 (i.e., activation of FOXO3) and induced phosphorylation of the histone H2A variant H2AX (termed γ-H2AX), a hallmark of DNA damage40 and of serine (S)-15 of p53 (p53-pS15) in OvCa cells (Fig. 2). This suggests that metformin may activate FOXO3 and p53 and promote colocalization of FOXO3 and p53-pS15 to form nuclear foci. Since p53-pS15 plays an important role in regulating cell-cycle arrest in response to DNA damage41, our current findings suggest that low-dose metformin may induce cell-cycle arrest in the treated OvCa cells. In addition, low doses of metformin induced FOXO3 nuclear localization and promoted the level of γ-H2AX or the level of p53-pS15 and their co-localizations with FOXO3 in the nuclei of BCa cells. However, this occurs to a lesser extent in non-cancerous or normal-like breast cells (Supplementary Fig. 1). Similarly, our data suggest that low-dose of SN-38 (1 nM) promoted FOXO3 nuclear localization and elevated the level of γ-H2AX and their co-localizations with FOXO3 in the nuclei of OvCa and BCa cells (Supplementary Fig. 2). These results suggest that low-dose metformin or SN-38 may suppress tumor growth and development in OvCa or BCa cells via a similar or an identical molecular mechanism.
Low doses of metformin induce FOXO3 nuclear localization and phosphorylation of H2AX (γ-H2AX) and p53 (p53-pS15) and their co-localizations with FOXO3 in the nuclei of OvCa cells.
OVCA429 cells were treated with control (H2O) or metformin for 24 hours. The subcellular localizations between FOXO3 and (A) γ-H2AX or (B) p53-pS15 were detected using antibodies (Abs) against the indicated proteins and followed by an Alexa Fluor 594- or 488-conjugated secondary Ab and fluorescence microscopy. DAPI was used to show the nuclei and co-localization of proteins was shown as the merged images (orange color). (C, D) The percentages of colocalized nuclear FOXO3 and (C) γ-H2AX or (D) p53-pS15 in cells are shown in the histogram (n = 100). (E) The cytoplasmic (Cyt.) and nuclear (Nuc.) extracts were analyzed by immunoblotting (IB) with specific Abs as indicated. GAPDH and α-Tubulin represent the fractionation and loading controls of Cyt. Extracts and HMG14 and Lamin A/C indicate the fractionation and loading controls of Nuc. extracts.
Low-dose metformin or SN-38 suppresses the formation of 3D tumor-like spheroids of OvCa cells in 3D culture
To determine if the low dose of metformin or SN-38 has an inhibitory effect on the cancer cells' capacity to serially self-renew as spheroid cells in a more tissue-like microenvironment, we grew OVCA429 cells in 3D culture with extracellular matrix (ECM) gel in order for them to become spheroids. The size of spheroids was measured to see if the cells treated with low-dose metformin or SN-38 grew more slowly than the cells treated with the vehicle (negative controls). Cells that were grown in this 3D culture with low doses of metformin (10 μM) and SN-38 (1 nM) had a significantly lower median area than controls and had a lower percentage of spheres at the cutoff size than controls (Fig. 3). These results suggest that low-dose metformin or SN-38 can inhibit spheroid body-formation of OvCa cells in 3D culture.
Low doses of metformin or SN-38 suppress the formation of 3D tumor-like spheroids of OvCa cells.
OVCA429 cells were incubated for 10 days in 3D extracellular matrix gel overlay cultures under treatment with metformin (10 or 100 μM) or SN-38 (1 nM) or the vehicle control (DMSO). Cells were analyzed in a bright field microscope and the area of each sphere above a cutoff size (0.1 mm2) was measured. (A) Phase contrast/brightfield images at day 10 are shown, with all images at the same magnification, resolution and size. (B) The histogram shows the percentage of spheres that were 1×, 2× and 3× times larger than the cutoff size (mean ± SD of triplicate, n = 100). *, P < 0.05, **, P < 0.001.
Low-dose metformin or SN-38 downregulates the expression of the stemness markers in OvCa and BCa cells
To determine if the drug-mediated suppression of OvCa/BCa cells' spheroid-forming capabilities reveals the deficiency of stemness characteristics in OvCa or BCa cells, we compared the expression of a cancer-stemness marker CD444,42 in these cancer cells treated with a negative control, metformin, or SN-38. Using FACS analysis, we showed that the low-dose metformin or SN-38 treatment significantly decreased the expression of CD44 (at least 10-fold) in OVCA429 and BT-549 cells (Fig. 4A, B). However, it has been suggested that CD44 alone may not be a compelling cancer-stemness marker in breast cancer43. To confirm metformin or SN-38 treatment leads to significant downregulation of the expression of the stemness markers in these cancer cells, we performed immunoblotting experiments with total lysates of the drug-treated cells as described above. Our data demonstrate that metformin or SN-38 treatment leads to significant downregulation of the expression of several well-established stemness markers, including Nanog, Oct-4 and c-Myc, in addition to CD44 in both OVCA429 and BT-549 cells (Fig. 4C, D). Collectively, these data suggest that low-dose metformin or SN-38 may induce loss of stemness characteristics in OvCa and BCa cells and may trigger the reprogramming or the differentiation of these cancer cells into non-cancerous cells.
Low-dose metformin or SN-38 downregulates the expression of the stemness markers in OvCa and BCa cells.
(A) OVCA429 cells and (B) BT549 cells were treated with the vehicle control (DMSO) or metformin (100 μM) or SN-38 (1 nM) for 72 hours. The expression of the stemness marker CD44 in these treated cells was determined by FACS analysis using a FITC-conjugated anti-human CD44 monoclonal antibody as described in Methods. Total lysates of the drug-treated (C) OVCA429 cells and (D) BT549 cells as described above were analyzed by immunoblotting (IB) with specific Abs as indicated. β-Actin represents the loading controls.
Silencing FOXO3 decreases the metformin-mediated suppression of cell growth in OvCa cells in vitro and ovarian tumor growth in vivo
To determine whether FOXO3 is necessary for the metformin-mediated DNA damage signaling, we silenced endogenous FOXO3 in OVCA429 cells by establishing stable FOXO3-knockdown and vector control cell lines (designated OVCA429-FOXO3-shRNA and OVCA429-Control-shRNA) (Fig. 5A) as described in Methods. We treated OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines with low-dose metformin or a negative control to compare the effects of these drugs on the rate of cell proliferation and on the ovarian tumor growth in the mouse model. Our results indicate that knockdown of FOXO3 in OVCA429 significantly reduced the metformin-mediated suppression of cell growth (Fig. 5B) and ovarian tumor growth or progression in vivo in the mouse model (Fig. 5C). To verify FOXO3 knockdown in OVCA429-FOXO3-shRNA cells at the end of the drug treatment period, we performed immunoblotting experiments with total lysates of the drug-treated cells as described above. Our data indicate that the expression of FOXO3 in OVCA429-FOXO3-shRNA cells remained markedly lower than that in OVCA429-Control-shRNA cells after 72 hours of the low-dose metformin or SN-38 treatment (Fig. 5D).
Silencing FOXO3 decreases the metformin-mediated suppression of cell growth in OvCa cells in vitro and ovarian tumor growth in vivo in the mouse model.
(A) OVCA429 cells were transfected with shRNA-Control or shRNA-FOXO3 and stable cell lines were isolated. The indicated proteins were detected by immunoblotting with specific Abs against FOXO3 and β-actin (loading control). (B) The OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines were treated with low-dose metformin (100 μM) or the vehicle control (DMSO) for 72 hours. The growth/survival rates of cells were measured by cell counting and are shown as the percentage relative to the survival rate of the negative control. The P values between the control groups and the metformin-treated groups are indicated and a P value < 0.05 is considered significant. The number of biological replicates is three, the error bars represent SD and the statistical test is the two-sided unpaired Student's t tests. (C) OVCA429-Control-shRNA cells and OVCA429-FOXO3-shRNA cells were injected into female nude mice subcutaneously (n = 4/group). When palpable tumors were detected, the mice were given an intraperitoneal injection of metformin (5 mg/kg BW) or control once every three days. The tumor volumes were measured twice a week and graphed as mean values of volume with standard deviation. (D) Total lysates of the metformin- or SN38-treated OVCA429-Control-shRNA cells and OVCA429-FOXO3-shRNA cells as described in (B) were analyzed by immunoblotting (IB) with specific Abs as indicated. β-Actin represents the loading controls.
Knockdown of FOXO3 reduces the metformin-promoted phosphorylation of DNA damage markers in OvCa cells
We treated OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines with low doses of metformin and negative control for 48 hours, then analyzed the subcellular localizations of FOXO3 and γ-H2AX in these cells as described above. Notably, silencing FOXO3 significantly diminished the metformin-induced γ-H2AX in the nuclei of OVCA429 cells (Fig. 6). It is known that the protein ataxia-telangiectasia mutated (ATM) is a key enzyme for DNA damage response44. Because ATM is activated by DNA damage through autophosphorylation at Serine-1981 (designated ATM-pS1981)44, we also examined the subcellular localizations of ATM-pS1981 in these cells. Similarly, knockdown of FOXO3 significantly reduced the metformin-induced ATM-pS1981 in the nuclei of OVCA429 cells (Supplementary Fig. 3). Taken together, these results suggest that FOXO3 may play an essential role in the metformin-induced phosphorylation of DNA damage markers in OvCa cells.
Knockdown of FOXO3 reduces the metformin-promoted phosphorylation of γ-H2AX in OvCa cells.
The OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines were treated with control (DMSO) or metformin for 24 hours. The subcellular localizations between FOXO3 and γ-H2AX in (A) OVCA429-Control-shRNA or (B) OVCA429-FOXO3-shRNA cells were detected using specific Abs against the indicated proteins and followed by an Alexa Fluor 594- or 488-conjugated secondary Ab and fluorescence microscopy. DAPI was used to show the nuclei and co-localization of proteins was shown as the merged images (orange color). (C, D) The percentages of colocalized nuclear FOXO3 and γ-H2AX in (C) OVCA429-Control-shRNA and (D) OVCA429-FOXO3-shRNA cells are shown in the histogram (n = 100).
Silencing FOXO3 diminishes the metformin- or SN38-mediated suppression of spheroid body-formation in 3D culture and downregulation of the stemness markers in OvCa cells
We treated OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines with low-dose metformin, SN-38, or the negative control to compare the effects of these drugs on the different spheroid body-forming capacities in 3D culture and on the regulation of the expression of a cancer-stemness marker CD44 between these two cell lines by using FACS analysis. Our data indicate that knockdown of FOXO3 in OVCA429 significantly reduced the metformin- or SN38-mediated inhibition of the formation of tumor-like spheroids in OvCa cells in 3D culture (Fig. 7) as well as the suppression of the expression of CD44 in these cells (Fig. 8A, B).
Silencing FOXO3 in OVCA429 reduces the metformin- or SN38-mediated suppression of the formation of 3D tumor-like spheroids of OvCa cells.
The OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cell lines were incubated for 13 days in 3D extracellular matrix gel overlay cultures under treatment with the vehicle control (DMSO) or metformin (100 μM) or SN-38 (1 nM). Cells were analyzed in a bright field microscope and the area of each sphere above a cutoff size (0.1 mm2) was measured. (A) Phase contrast/brightfield images at day 13 are shown, with all images at the same magnification, resolution and size. (B) The histogram shows the percentage of spheres of OVCA429-Control-shRNA cells that were 1×, 2× and 3× times larger than the cutoff size (mean ± SD of triplicate, n = 100). *, P < 0.01, **, P < 0.001. (C) The histogram shows the percentage of spheres of OVCA429-FOXO3-shRNA cells that were 1×, 2× and 3× times larger than the cutoff size (mean ± SD of triplicate, n = 100). The P values between the control versus those of the groups treated with metformin or SN-38 are not significant.
Silencing FOXO3 in OVCA429 reduces the metformin- or SN38-mediated downregulation of the stemness markers in OvCa cells.
(A) OVCA429-Control-shRNA cells and (B) OVCA429-FOXO3-shRNA cells were treated with the vehicle control (DMSO) or metformin (100 μM) or SN-38 (1 nM) for 72 hours. The expression of a cancer-stemness marker CD44 in these treated cells was determined by FACS analysis using an FITC-conjugated anti-human CD44 monoclonal antibody as described in Methods. The unstained cell populations are shown as references (bottom panels). (C) Total lysates of the drug-treated OVCA429-Control-shRNA cells and OVCA429-FOXO3-shRNA cells as described above were analyzed by immunoblotting (IB) with specific Abs as indicated. β-Actin represents the loading controls.
To confirm that FOXO3 is essential for regulating the drug-mediated suppression of the expression of the stemness markers in OVCA429-Control-shRNA and OVCA429-FOXO3-shRNA cells, we performed immunoblotting analysis with total lysates of the drug-treated cells as described above. Our results show that the expression of CD44 in OVCA429-Control-shRNA cells was downregulated significantly after metformin or SN-38 treatment, whereas downregulation of CD44 expression was diminished in OVCA429-FOXO3-shRNA cells. These results suggest that FOXO3 may be necessary for drug-mediated suppression of CD44. In addition, our data indicate that metformin or SN-38 treatment suppresses the expression of several well-established stemness markers such as Nanog, Oct-4 and c-Myc in OVCA429-Control-shRNA cells, whereas the drug-mediated suppressive effect was abrogated in OVCA429-FOXO3-shRNA cells (Fig. 8C). These data further suggest that FOXO3 may be essential for metformin- and SN38-mediated suppression of the expression of other stemness markers. These results suggest that FOXO3 may be required for the metformin- or SN38-mediated inhibition of forming 3D tumor-like spheroids in OvCa cells and downregulation of the expression of stemness markers in OvCa cells.
Discussion
Although killing cancer cells by the conventional chemotherapeutic approach remains one of the most effective anticancer treatments for OvCa and BCa and is often applied as the front-line therapy after cytoreductive surgery, the undesirable and sometimes intolerable side effects of chemotherapies often hinder patients' willingness to accept long-term treatments with high doses chemotherapies. In fact, some cancer patients die due to intolerable side effects of high-dose chemotherapies rather than from the malignant effects of the cancer. At the very minimum, those unwanted or intolerable side effects could significantly decrease the quality of life in cancer patients undergoing chemotherapy. In this study, we show that candidate low-dose small-molecule drug such as metformin or SN-38 suppresses ovarian/breast tumor growth and may reprogram OvCa or BCa cells into their perspective non-cancerous cells in a FOXO3-dependent manner. Overall, our results strongly support the therapeutic concept of reprogramming cancer cells into non-cancerous cells in cancer patients with minimal side effects.
To decipher the functional roles of metformin and SN-38 in regulating the cellular process of reprogramming or reprogramming of OvCa/BCa cells into non-cancerous cells, we show that low-dose metformin or SN-38 promotes FOXO3 nuclear localization and induces the activation of ATM-pS1981, γ-H2AX and p53-pS15 in these cancer cells. This signaling cascade is consistent with our previous finding that FOXO3 activation triggers the activation of ATM-pS1981, which in turn phosphorylates p53-pS1545. Interestingly, it has been suggested that metformin functions as a result of the activation of AMPK in cells9,10 and AMPK activation can phosphorylate FOXO3 and induce FOXO3 activation46,47. Thus, we validate that low-dose metformin indeed induces the activation of AMPKα2 by phosphorylation of Theonine-172 residue (pT172) of AMPKα2 (designated as AMPKα2-pT172); however, SN-38 does not activate AMPKα2 phosphorylation in these cells (Supplementary Fig. 4). These results suggest that low-dose metformin may promote FOXO3 nuclear localization through AMPK activation, whereas low-dose SN-38 may activate FOXO3 nuclear localization directly.
Metformin remains one of the most commonly prescribed drugs, with nearly 120 million prescriptions filled annually worldwide48. In addition to treating diabetics, metformin is also effective in the treatment of polycystic ovary syndrome and is being explored as an anticancer agent12,13,49,50,51. In most of the previous cancer-related studies, the concentrations of metformin used in cell culture were at relatively high levels, ranging between 10,000 μM and 50,000 μM49,50. In contrast, in our current study, the concentrations of metformin used in cell culture were 10 μM or 100 μM. We have determined the IC50s for metformin and SN-38 for OVCA429 and BT-549 cells and our data indicate that the IC50s for metformin for OVCA429 and BT-549 cells are 480 μM and 1,470 μM, respectively (Supplementary Fig. 5). While the doses of metformin used in the previous in vivo studies were at relatively high levels, from 100 mg/kg to 500 mg/kg body weight (BW)49,50,51, the dose of metformin used in our in vivo tumor models was 5 mg/kg BW. Similarly, the concentrations of SN-38 used in our cell culture were 1 nM or 10 nM and the dose of SN-38 used in our in vivo studies was 10 μg/kg BW. These concentrations and doses of SN-38 used in this study were between 10- and 200-fold lower than those concentrations and doses used in previous publications (such as 1,000 nM in vitro and 2,000 μg/kg BW in vivo)52,53. Because our therapeutic approach is to apply low-dose metformin or SN-38 to promote the reprogramming of OvCa/BCa or CSC into non-cancerous cells or NTSC, this low-dose chemotherapy will not significantly harm normal tissue cells, therefore this approach may allow patients to overcome OvCa/BCa with minimal side effects.
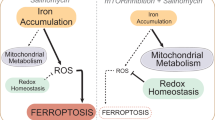
CD44 has been demonstrated to be a cancer-stemness marker for ovarian and breast CSC42,54. Notably, our results indicate that low-dose metformin or SN-38 downregulates the expression of CD44 in OvCa and BCa cells. These findings suggest that low-dose metformin or SN-38 may reduce the stemness characteristics of ovarian and breast CSC. However, it has been suggested that CD44 alone may not be a conclusive cancer-stemness marker in breast cancer progression43. Therefore, we validate that low-dose metformin or SN-38 treatment leads to significant downregulation of the expression of several well-established stemness markers, including Nanog, Oct-4 (one of the most commonly used stemness markers) and c-Myc, in addition to CD44 in both OVCA429 and BT-549 cells. Since CD117 (c-Kit) has been suggested as a biomarker for ovarian CSC in one report42, we have also tested whether the low doses of metformin or SN-38 could affect the expression of CD117 in OvCa and BCa cells. Our results suggest that OVCA429 and BT-549 cells express a very low level of CD117 and the metformin or SN-38 treatments do not appear to alter the expression of CD117 in these cells (not shown). However, we cannot rule out the possibility that the metformin or SN-38 treatment may regulate the expression of CD117 in other OvCa and BCa cells, which may express a high level of CD117. In addition, our data show that low-dose metformin or SN-38 suppresses the formation of 3D tumor-like spheroids of OvCa cells in 3D culture. Notably, our results show that silencing FOXO3 reduces the metformin- or SN38-mediated suppression of spheroid body-formation in 3D culture and downregulation of the expression of stemness markers in OvCa cells. These results suggest that FOXO3 may play an essential role in regulating the metformin- or SN38-mediated reprogramming of OvCa or BCa cells into their perspective non-cancerous cells. Collectively, these data suggest that low-dose metformin or SN-38 may induce loss of stemness characteristics in OvCa and BCa cells and may trigger the reprogramming or the differentiation of these cancer cells into non-cancerous cells. Thus, we have proposed a schematic representation of the FOXO3-dependent reprogramming of OvCa/BCa or CSC cells into their respective non-cancerous cells in response to the treatment of low-dose metformin or SN-38 (Supplementary Fig. 6).
An interesting question regarding the molecular mechanisms behind the effectiveness of low-dose metformin or SN-38 is how the activation of the FOXO3-p53 signaling pathway regulates reprogramming factors (Supplementary Fig. 6), which in turn trigger the reprogramming of cancer cells or CSC into non-cancerous cells or NTSC in response to the treatment of metformin or SN-38. The candidate reprogramming factors are yet to be identified and the mechanisms underlying the reprogramming factors-mediated reprogramming of OvCa or BCa cells into their perspective non-cancerous cells are yet to be elucidated. Remarkably, it has been demonstrated that the application of one or two small molecules can reprogram adult differentiated fibroblasts into induced pluripotent stem cells (iPSC)55. This intriguing finding suggests that one or two small molecules may be sufficient to alter the critical genetic program for the reprogramming of the cell's fate in general. Thus, this report strongly supports our findings that the application of small-molecule drugs can reprogram cancer cells or CSC into non-cancerous cells or NTSC.
Finally, this research is still at its early stage and by no means can these findings be translated into any clinical application as of now. Further investigation of this therapeutic concept of reprogramming OvCa/BCa cells into non-cancerous cells is necessary to establish novel therapeutic interventions for suppression of OvCa/BCa cancer development in patients with minimal side effects in the future.
Methods
The methods were carried out in “accordance” with the approved guidelines.
Antibodies and reagents
Metformin and SN-38 (7-ethyl-10-hydroxycamptothecin) were purchased from Fisher Scientific (Pittsburgh, PA). DMSO was purchased from Sigma (St. Louis, MO). Metformin was dissolved in sterile phosphate-buffered saline (PBS) or H2O or dimethylsulfoxide (DMSO) and SN-38 was dissolved in DMSO. Antibodies specific to FOXO3 (FKHRL1) N-16 (1:500 dilution), p53-pS15 (1:1000 dilution), p53 (DO-1, 1:1000 dilution), AMPKα2 (1:1000 dilution), phospho-H2AX Serine-139 (γ-H2AX, 1:1000 dilution), CD44 (1:1000 dilution), c-Myc (1:1000 dilution), α-Tubulin (1:2000 dilution) and Lamin A/C (1:1000 dilution) were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Antibodies against phospho-H2AX Serine-139 (1:1000 dilution) and phospho-ATM Serine-1981 (ATM-pS1981, 1:1000 dilution) were purchased from Millipore (Billerica, MA). Antibody against AMPKα2-pT172 (1:1000 dilution) was purchased from Cell Signaling Technology (Danvers, MA). Antibodies against FOXO3 (3280-1, 2071-1, 1:1000 dilution) and ATM-pS1981 (1:1000 dilution) were obtained from Epitomics (Burlingame, CA). Antibody against β-Actin (1:3000 dilution) was purchased from Sigma. Antibodies against HMG14 (high-mobility-group 14, 1:2000 dilution), Nanog (1:1000 dilution), OCT4 (1:1000 dilution) were purchased from Abcam (Cambridge, MA). Antibody against GAPDH (1:1000 dilution) was obtained from Thermo Fisher scientific (Waltham, MA). Alexa 488-, Alexa 594-, or Alexa-647-conjugated secondary antibodies (1:200 dilution) were obtained from Invitrogen-Molecular Probes (Eugene, OR). Goat anti-mouse IgG and goat anti-rabbit IgG horseradish peroxidase-conjugated secondary antibodies were purchased from Jackson ImmunoResearch (West Grove, PA).
Cell culture, cell lines and shRNA transfection
All cell lines were grown at 37°C and 5% CO2 in DMEM/F12 supplemented with L-glutamine, penicilline/streptomycin and 10% fetal bovine serum. BT549, human breast epithelial ductal carcinoma, cell line was obtained from the American Type Culture Collection and OVCA429, an established cell line derived from a patient with late-stage serous ovarian adenocarcinomas56, was kindly provided by Robert C. Bast, Jr., Division of Cancer Medicine, the University of Texas MD Anderson Cancer Center. Four HuSH 29mer shRNA constructs against human FOXO3 (NM_001455) and control HuSH shRNA cloning vector (pRS) using U6 promoter were purchased from Origene (Rockville, MD) as described previously45. OVCA429 cells were transfected with a combination of four HuSH 29mer shRNA constructs concurrently or control pRS vector by liposome using GenJet™ In Vitro DNA Tranfection Reagent (SignaGen Laboratories, Gaithersburg, MD). After puromycin selection (1 μg/ml), the OVCA429 FOXO3-knockdown pooled stable clones (designated OVCA429-FOXO3-shRNA) and the vector control stable clones (designated OVCA429-Control-shRNA) were selected.
Cell growth assays
The cell growth/survival rates were determined by cell counting. OvCa or BCa cells (1 × 105/well) were seeded into 6-well plates and treated with metformin (10 μM or 100 μM) or SN-38 (1 nM) or vehicle (negative control), DMSO, for 3 days in cell culture. Cells numbers were measured by counting in a hemocytometer using 0.4% Trypan Blue (GIBCO, Life Technologies). The relative (%) cell growth/survival rate was calculated by dividing cell number of metformin or SN-38 treatment by that of vehicle treatment.
Three-dimensional (3D) culture
For the determination of the colony size of OVCA429 cells when grown as spheres, cells were seeded in eight-well chamber slides at 5000 cells/well (Lab-TekTM II, Nunc, Thermo Scientific). The wells were first coated with 120 μl of extracellular matrix (ECM) Gel from Engelbreth-Holm-Swarm murine sarcoma (Sigma). The cells were seeded on top of the gel layer in DMEM/F12 medium for MCF10A with 2.5% ECM gel and 5 ng/ml EGF. DMSO (negative control), 10 μM metformin and 10 nM SN-38 were added to separate well plates 24 hours after initial seeding. Cells were grown for 21 days with the change of the top layer media (DMEM/F12 medium with 2.5% ECM gel and 5 ng/ml EGF and investigational drugs) every 4 days. For analysis of the sphere size, bright field images were captured with the Image-Pro Plus 7.0 software through a Leica DM IRB microscope. For each sample, 6 representative images were captured at 10× and 1392 × 1040 resolution, so all images were identically scaled. Using Image J, version 1.45 s, the number of spheres with an area above a specific cutoff value was calculated in an automated manner. The area of each sphere was also calculated in the same manner. The measurement scale was set by drawing a line that was 1 mm on a photograph to obtain a global scale of pixels/cm to be used for all sample images. Each image was converted to an 8-bit grayscale and converted to binary for detection of edges. By using the Analyze Particles function, the software displayed the area of each sphere above the cutoff value (0.1 mm2). The median area from 6 images (from 3 replicates for each sample) was calculated for each treatment. The percentage of spheres with areas above 0.1, 0.2 and 0.3 mm2 within each treatment group was also calculated.
Fluorescence-Activated Cell Sorting (FACS)
OvCa or BCa cells were trypsinized, aliquoted (1.25–2.5 × 105 cells per condition) and fixed for 10 minutes in 4% (v/v, in PBS) paraformaldehyde (Electron Microscopy Sciences) at 4°C. Afterwards, the cells were washed in PBS, centrifuged at 1200 g and re-suspended in PBS with 0.1% BSA (FACS buffer). Cells were incubated in FACS buffer containing FITC-conjugated anti-human CD44 and PE-conjugated anti-human CD117 monoclonal Abs (Fisher Scientific-Biolegend) or isotype control mouse IgG Ab. Cells were characterized by using a FACS FACScan (BD) at the Institutional shared FACS Facility and the data were analyzed by FlowJo software. Ten thousand events were collected in each run.
Immunofluorescence analysis
OvCa and BCa cells were grown separately on glass coverslips. After separate treatments of metformin (10 μM and 100 μM separately), SN-38 (1 nM) and vehicle (H2O or DMSO) for 24 hours, cells were fixed with 4% paraformaldehyde for 10 min and permeabilized with Triton X-100 (0.5%). Slide culture chambers were washed with PBS and blocked with PBS containing 2% BSA, incubated with a primary antibody (Ab) specific to FOXO3 or γ-H2AX or p53-pS15 (1:50 to 1:200 dilution), followed by Alexa 594 (red)-conjugated anti-rabbit (1:200 dilution) and Alexa 488 (green)-conjugated anti-mouse (1:200 dilution) secondary Abs (Molecular Probes, Eugene, OR). Cells were counterstained with DAPI (Sigma) to show the nuclei. Specific staining was visualized and images were captured with a Leica SP2 AOBS confocal laser scanning microscope. To analyze quantitative co-localization, we used ~100 cells images randomly captured by confocal microscopy. The volume and percentage of FOXO3 co-localized with γ-H2AX or p53-pS15 were measured using the Velocity software (ver. 6.1, Improvision, PerkinElmer). Each error bar presented is the mean of standard deviation (SD).
Immunoblotting analysis
For immunoblotting (IB) analysis, the protein samples were subjected to SDS-PAGE and transferred onto nitrocellulose membranes (Boi-Rad). Membranes were blocked for 1 hour in 3% bovine serum albumin (BSA) in Tris buffered saline containing 0.1% Tween-20 (TBST) and incubated for 1 hour with a primary antibody, as described above, diluted in TBST containing 1% BSA. After three washes with TBST, membranes were incubated for 1 hour with horseradish peroxidase-conjugated secondary antibodies (1:3000 dilution) in TBST containing 3% BSA. The immunoblots were visualized by an enhanced chemiluminescence kit obtained from Santa Cruz Biotechnology or West-Q ECL Platinum Solution obtained from GenDepot (Barker, TX).
Animal studies
To determine the tumorigenicity and to establish the ovarian and breast tumor animal models, female athymic (nu/nu) nude mice were purchased from Charles River Laboratories, Inc. (Wilmington, MA) and maintained aseptically in an athymic animal room. For tumor-cell implantation, OVCA429 or MDA-MB-231 or OVCA429-FOXO3-shRNA or OVCA429-Control-shRNA cells (in log-phase growth) were harvested, washed with PBS and re-suspended in PBS. Then cells (4 × 106 in 0.1 ml PBS with 30% ECM gel) were injected subcutaneously into the flank of each mouse as described previously28,57. When palpable solid tumors were detected (approx. 100 mm3), the one group of mice was given an intravenous (i.v.) or intraperitoneal injection (0.1 ml) of metformin (5 mg/kg BW/mouse) and another group of mice was given an i.v. injection (0.1 ml) of SN-38 (10 μg/kg BW/mouse) twice per week at even intervals for several weeks (up to 7 weeks). The vehicle (DMSO) was used as a negative control group. The tumor sizes were measured twice per week with a Vernier caliper. Data are presented as means and standard deviations (SD) of four mice in each group. Mice were weighed twice per week as a measure of overall systemic toxicity. All procedures were performed in compliance with the guidelines and regulations of the Institutional Animal Care and Use Committee (IACUC). The IACUC has approved the experiments listed in the Protocol number 21557 (Stanford's Animal Welfare Assurance Number: A3213-01).
Statistical analysis
All data are expressed as means and SD from at least three determinations. The statistical significance of difference in nuclear co-localization of proteins examined in cells (by immunofluorescence) and the percentage of cell growth/survival between two groups were analyzed with two-sided unpaired Student's t tests when the variances were equal with Grahpad PRISM (Ver.4.02) statistical software (San Diego, CA) or Excel (Microsoft Office). All statistical tests were two-sided and P values less than 0.05 were considered statistically significant.
References
Bray, F. et al. Estimates of global cancer prevalence for 27 sites in the adult population in 2008. Int. J. Cancer 132, 1133–1145 (2013).
Ricci, M. S. & Zong, W. X. Chemotherapeutic approaches for targeting cell death pathways. Oncologist 11, 342–357 (2006).
Abdullah, L. N. & Chow, E. K. Mechanisms of chemoresistance in cancer stem cells. Clin. Transl. Med. 2, 3 (2013).
Ghiaur, G., Gerber, J. & Jones, R. J. Concise review: Cancer stem cells and minimal residual disease. Stem Cells 30, 89–93 (2012).
Pham, P. V. et al. Differentiation of breast cancer stem cells by knockdown of CD44: promising differentiation therapy. J. Transl. Med. 9, 209 (2011).
Siegel, R., Naishadham, D. & Jemal, A. Cancer statistics, 2012. CA Cancer J. Clin. 62, 10–29 (2012).
McGuire, W. P. et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N. Engl. J. Med. 334, 1–6 (1996).
Ozols, R. F. et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J. Clin. Oncol. 21, 3194–3200 (2003).
Goodarzi, M. O. & Bryer-Ash, M. Metformin revisited: re-evaluation of its properties and role in the pharmacopoeia of modern antidiabetic agents. Diabetes Obes. Metab. 7, 654–665 (2005).
Zhou, G. et al. Role of AMP-activated protein kinase in mechanism of metformin action. J. Clin. Invest. 108, 1167–1174 (2001).
Evans, J. M. et al. Metformin and reduced risk of cancer in diabetic patients. BMJ 330, 1304–1305 (2005).
Bowker, S. L. et al. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care 29, 254–258 (2006).
Anisimov, V. N. et al. Effect of metformin on life span and on the development of spontaneous mammary tumors in HER-2/neu transgenic mice. Exp. Gerontol. 40, 685–693 (2005).
Schneider, M. B. et al. Prevention of pancreatic cancer induction in hamsters by metformin. Gastroenterology 120, 1263–1270 (2001).
Guastamacchia, E. et al. Evidence for a putative relationship between type 2 diabetes and neoplasia with particular reference to breast cancer: role of hormones, growth factors and specific receptors. Curr. Drug Targets Immune Endocr. Metabol. Disord. 4, 59–66 (2004).
Zakikhani, M. et al. Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res. 66, 10269–10273 (2006).
Kefas, B. A. et al. Metformin-induced stimulation of AMP-activated protein kinase in beta-cells impairs their glucose responsiveness and can lead to apoptosis. Biochem. Pharmacol. 68, 409–416 (2004).
Alvarez, B. et al. Forkhead transcription factors contribute to execution of the mitotic programme in mammals. Nature 413, 744–747 (2001).
Nemoto, S., Fergusson, M. M. & Finkel, T. Nutrient availability regulates SIRT1 through a forkhead-dependent pathway. Science 306, 2105–2108 (2004).
Tran, H. et al. DNA repair pathway stimulated by the forkhead transcription factor FOXO3a through the Gadd45 protein. Science 296, 530–534 (2002).
Tsai, W. B. et al. Functional interaction between FOXO3 and ATM regulates DNA damage response. Nat. Cell Biol. 10, 460–467 (2008).
Furukawa-Hibi, Y. et al. FOXO transcription factors in cell-cycle regulation and the response to oxidative stress. Antioxid. Redox Signal 7, 752–760 (2005).
Greer, E. L. & Brunet, A. FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene 24, 7410–7425 (2005).
Willcox, B. J. et al. FOXO3A genotype is strongly associated with human longevity. Proc. Natl Acad. Sci. USA 105, 13987–13992 (2008).
Brunet, A. et al. Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor. Cell 96, 857–868 (1999).
Sunters, A. et al. FOXO3 transcriptional regulation of Bim controls apoptosis in paclitaxel-treated breast cancer cell lines. J. Biol. Chem. 278, 49795–49805 (2003).
Yang, J. Y. et al. Induction of FOXO3a and Bim expression in response to ionizing radiation. Int. J. Oncol. 29, 643–648 (2006).
Hu, M. C. et al. IκB kinase promotes tumourigenesis through inhibition of Forkhead FOXO3. Cell 117, 225–237 (2004).
Seoane, J. et al. Integration of Smad and forkhead pathways in the control of neuroepithelial and glioblastoma cell proliferation. Cell 117, 211–223 (2004).
Habashy, H. O. et al. FOXO3a nuclear localisation is associated with good prognosis in luminal-like breast cancer. Breast Cancer Res. Treat. 129, 11–21 (2011).
Jiang, Y. et al. Foxo3a expression is a prognostic marker in breast cancer. PLoS One 8, e70746 (2013).
Paik, J. H. et al. FoxOs are lineage-restricted redundant tumor suppressors and regulate endothelial cell homeostasis. Cell 128, 309–323 (2007).
Miyamoto, K. et al. FOXO3 is essential for maintenance of the hematopoietic stem cell pool. Cell Stem Cell 1, 101–112 (2007).
Fei, M. et al. Low expression of Foxo3a is associated with poor prognosis in ovarian cancer patients. Cancer Invest. 27, 52–59 (2009).
Zamboni, W. C. et al. Studies of the efficacy and pharmacology of irinotecan against human colon tumor xenograft models. Clin. Cancer Res. 4, 743–753 (1998).
Benson, A. B. et al. Metastatic colon cancer, version 3.2013: featured updates to the NCCN Guidelines. J. Natl. Compr. Canc. Netw. 11, 141–152 (2013).
Schmoll, H. J. et al. ESMO Consensus Guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann. Oncol. 23, 2479–2516 (2012).
Hertzberg, R. P. et al. Modification of the hydroxy lactone ring of camptothecin: inhibition of mammalian topoisomerase I and biological activity. J. Med. Chem. 32, 715–720 (1989).
Kawato, Y. et al. Intracellular roles of SN-38, a metabolite of the camptothecin derivative CPT-11, in the antitumor effect of CPT-11. Cancer Res. 51, 4187–4191 (1991).
Hein, J. et al. Simian virus 40 large T antigen disrupts genome integrity and activates a DNA damage response via Bub1 binding. J. Virol. 83, 117–127 (2009).
Rodier, F. et al. DNA-SCARS: distinct nuclear structures that sustain damage-induced senescence growth arrest and inflammatory cytokine secretion. J. Cell Sci. 124, 68–81 (2011).
Zhang, S. et al. Identification and characterization of ovarian cancer-initiating cells from primary human tumors. Cancer Res. 68, 4311–4320 (2008).
Louderbough, J. M. & Schroeder, J. A. Understanding the dual nature of CD44 in breast cancer progression. Mol. Cancer Res. 9, 1573–1586 (2011).
Bakkenist, C. J. & Kastan, M. B. Initiating cellular stress responses. Cell 118, 9–17 (2004).
Chung, Y. M. et al. FOXO3 signalling links ATM to the p53 apoptotic pathway following DNA damage. Nat. Commun. 3, 1000 (2012).
Greer, E. L. et al. The energy sensor AMP activated protein kinase directly regulates the mammalian FOXO3 transcription factor. J. Biol. Chem. 282, 30107–30119 (2007).
Banko, M. R. et al. Chemical genetic screen for AMPKα2 substrates uncovers a network of proteins involved in mitosis. Mol. Cell 44, 878–892 (2011).
Ben Sahra, I., Le Marchand-Brustel, Y., Tanti, J. F. & Bost, F. Metformin in cancer therapy: a new perspective for an old antidiabetic drug? Mol. Cancer Ther. 9, 1092–1099 (2010).
Garofalo, C. et al. Metformin as an adjuvant drug against pediatric sarcomas: hypoxia limits therapeutic effects of the drug. PLoS One 8, e83832 (2013).
Fendt, S. M. et al. Metformin decreases glucose oxidation and increases the dependency of prostate cancer cells on reductive glutamine metabolism. Cancer Res. 73, 4429–4438 (2013).
Rattan, R. et al. Metformin suppresses ovarian cancer growth and metastasis with enhancement of cisplatin cytotoxicity in vivo. Neoplasia 13, 483–491 (2011).
Maurya, D. K. et al. Topoisomerase I inhibitor SN-38 effectively attenuates growth of human non-small cell lung cancer cell lines in vitro and in vivo. J. Environ. Pathol. Toxicol. Oncol. 30, 1–10 (2011).
Wallin, A. et al. Anticancer effect of SN-38 on colon cancer cell lines with different metastatic potential. Oncol. Rep. 19, 1493–1498 (2008).
Croker, A. K. et al. High aldehyde dehydrogenase and expression of cancer stem cell markers selects for breast cancer cells with enhanced malignant and metastatic ability. J. Cell Mol. Med. 13, 2236–2252 (2009).
Lyssiotis, C. A. et al. Reprogramming of murine fibroblasts to induced pluripotent stem cells with chemical complementation of Klf4. Proc. Natl. Acad. Sci. USA 106, 8912–8917 (2009).
Bast, R. C., Jr et al. Reactivity of a monoclonal antibody with human ovarian carcinoma. J. Clin. Invest. 68, 1331–1337 (1981).
Tsai, W. B. et al. Inhibition of FOXO3 tumor suppressor function by βTrCP1 through ubiquitin-mediated degradation in a tumor mouse model. PLoS ONE 5, e11171 (2010).
Acknowledgements
We thank R.C. Bast, Jr. for generously providing OvCa cell lines and the Freidenrich Center for Translational Research for generously providing support. This work was supported in part by R01 grant CA113859 (to M.C.T.H.) from the National Cancer Institute, National Institutes of Health; the 2012 Developmental Cancer Research Award from Stanford Cancer Institute (to M.C.T.H.), a grant 02-2013-051 from the Avon Foundation for Women (to M.C.T.H.) and the 2012 Ann Schreiber Research Award from the Ovarian Cancer Research Fund (to Y.M.C.). The sponsors had no role in the design, conduct, or reporting of the study.
Author information
Authors and Affiliations
Contributions
The experiments were conceived and designed by M.C.T.H., T.H., Y.M.C. and J.M.; experiments were performed by T.H., Y.M.C., M.G., M.M., J.M. and M.C.T.H; data were analyzed by T.H., Y.M.C., M.G., M.M., J.M. and M.C.T.H; essential resources and reagents were provided by J.S.B. and M.C.T.H. The paper was written by M.C.T.H. and T.H.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Hu, T., Chung, Y., Guan, M. et al. Reprogramming ovarian and breast cancer cells into non-cancerous cells by low-dose metformin or SN-38 through FOXO3 activation. Sci Rep 4, 5810 (2014). https://doi.org/10.1038/srep05810
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05810
This article is cited by
-
Neoadjuvant metformin added to conventional chemotherapy synergizes anti-proliferative effects in ovarian cancer
Journal of Ovarian Research (2020)
-
MiR-629 promotes human pancreatic cancer progression by targeting FOXO3
Cell Death & Disease (2017)
-
BRCA1 positively regulates FOXO3 expression by restricting FOXO3 gene methylation and epigenetic silencing through targeting EZH2 in breast cancer
Oncogenesis (2016)
-
Inhibitory effects of metformin at low concentration on epithelial–mesenchymal transition of CD44+CD117+ ovarian cancer stem cells
Stem Cell Research & Therapy (2015)
-
Differentiation of human neuroblastoma cells toward the osteogenic lineage by mTOR inhibitor
Cell Death & Disease (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.