Abstract
This study aimed to determine the performance and long-term outcomes of therapeutic ERCP in very old patients. Patients aged or over 90 (Group A, n = 78) and consecutive sex-matched controls (Group B, n = 312) under 65 selected were compared. More patients in Group A had chronic concomitant diseases, but the success and complication rates were comparable. The follow-up of 61 patients (78.2%) in Group A were done, with a mean period of 27.5 (3–54) months. Seven patients survived; the main causes of death for the other patients were concomitant diseases (n = 43) and primary diseases (n = 11). In patients with choledocholithiasis, cases with complete extractions of stones in bile ducts survived longer than those without (30 vs. 24 months, P < 0.001). Therapeutic ERCP in patients aged 90 years or older is effective and safe. In patients with choledocholithiasis, complete clearance of stones is associated with longer survival time.
Similar content being viewed by others
Introduction
Life expectancy is increasing all over the world1. The proportion of the elderly in the population increases2, which challenges the gastroenterologists, as ASA (American Society of Anesthesiologists) scores are poor in this old population, meaning that the mortality rate due to surgery becomes relatively higher3. As an alternative to open surgery, therapeutic endoscopic retrograde cholangiopancreatography (ERCP) is currently the first method of choice to diagnose and treat biliary and pancreatic diseases, especially for elderly patients with high operative risks, which generally correlates with the perioperative mortality rate4.
So far, there have only been a few studies evaluating the performance and safety of therapeutic ERCP in patients aged 90 years or older5,6,7. However, these studies were conducted either in a small selected samples, or without strict control groups. In 2004, Hui et al focused on the evaluation of outcomes of emergency ERCP application in very old patients. In 2000, Sugiyama et al solely studied old patients with choledocholithiasis who underwent ERCP. In addition, none of the studies followed the patients for a long period of time. Therefore, we carried out the present study to compare the performance and safety of therapeutic ERCP in patients aged or over 90 years and control patients under 65 years old and to investigate the long-term outcomes of the very elderly patients.
Results
Baseline and clinical characteristics
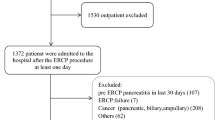
Over a period of 15 years, 17893 therapeutic ERCP procedures were performed in our endoscopy center. A total of 88 patients aged 90 years or older who underwent 109 ERCP procedures were reviewed with a percentage of 0.6% (109/17893). Ten patients referred from other hospitals (i.e. therapeutic ERCP was performed in our department but both pre-ERCP preparation and post-ERCP monitoring were conducted at other hospitals) were excluded. Thus, 78 patients aged over 90 years (mean age 91.8 ± 1.7 years; range 90–97 years) with 97 ERCP procedures were included in Group A. Of these 78 patients, four (5.1%) underwent emergency therapeutic ERCP. Accordingly, 312 sex- matched consecutive patients under 65 years old (mean age 50.3 ± 10.8 years; range 16–64 years) with 312 ERCP procedures were included in Group B (Table 1).
The presence of nausea or vomiting, fever and poor appetite proved to be more frequent in Group A than in Group B (all P < 0.05). There was no significant difference in other presenting symptoms between the two groups. Chronic concomitant diseases including hypertension, cardiac arrhythmias and pulmonary diseases (all P < 0.001), coronary heart disease (P = 0.001), diabetic mellitus (P = 0.010) and stroke (P = 0.004) were generally more frequently observed in Group A than in Group B. Besides, more patients with ASA score of 2 and 3 were found in Group A than in Group B (P < 0.001) (Table 1).
Diagnoses, difficulty, outcomes and complications of ERCP
The spectra of post-ERCP diagnosis were different. Sixty-one patients in Group A and 218 patients in Group B were diagnosed as choledocholithiasis which was the most common post-ERCP diagnosis. The proportions of patients with other post-procedure diagnosis were different in the two groups (P < 0.001, Table 2). Patients with chronic pancreatitis and benign biliary stenosis were only seen in Group B.
More periampullary diverticula and papilla in diverticula were detected during ERCP in Group A (30.8% vs. 7.7%, P < 0.001) and only one case with biliary fistula was seen in Group A.
There was a higher grade of difficulty for first procedures in Group A than in Group B (P = 0.030, Table 2). The ERCP success rate of all patients was 91.0% (71/78) in Group A and 96.2% (300/312) in Group B (P = 0.060, Table 2). The papilla was reached in all procedures. In two cases in Group A, the procedure had to be discontinued prematurely because the patients were at life-threatening risk, with one having a decreasing heart rate and another with hypoxemia due to dyspnea. There were no serious complications (Table 2). Post-ERCP complications occurred in six (7.7%) in Group A and in 23 (7.4%) in Group B (P > 0.05).
Long-term Follow-up
Of the 78 patients, 17 (21.8%) patients were lost to follow-up and these patients were excluded from further analysis. Thus, follow-up data were available for 61 patients in Group A, composed of 50 cases with benign diseases (choledocholithiasis only) and 11 with malignant disorders, which were included in the analysis to determine the outcomes of the therapeutic ERCP. And all the 11 patients with malignant tumors accepted ERCP because of intolerance to the high risk for surgery and/or unresectable tumor. The mean follow-up period of time was 27.5 (ranging from 3 to 54) months, during which 19 subsequent ERCP procedures were performed. Five patients had repetitive ERCP procedures (range: 2–5 times) during the follow-up period. All these 5 patients were diagnosed with choledocholithiasis and incomplete clearance of stones and thus endoscopic biliary stents placement and exchange were conducted.
Of the 61 patients, seven patients were alive at the final follow-up in February 2013 (Table 3). Thus, 54 patients died during the period of follow-up; 43 (41 with choledocholithiasis and 2 with cancers as primary diseases, respectively) died of concomitant diseases and 11 (2 with choledocholithiasis and 9 with cancers) died of primary diseases. The two patients with choledocholithiasis died of infection and septic shock (Table 3).
Survival analysis showed that patients with choledocholithiasis gained longer survival time than with cancers (median survival time: 27 months vs. 13 months, P < 0.001, Fig. 1A).
Based on the latest medical records of 50 patients with choledocholithiasis, 29 patients had complete extractions of bile duct stones and 21 patients did not. Further analysis showed that patients with complete extraction of stones further extended their living time, compared with those with incomplete extraction (median survival time: 30 months vs. 24 months, P < 0.001, Fig. 1B). However, no significant differences were found in the ages, ASA scores and concomitant diseases between the two groups (all P > 0.05).
Discussion
Aging has become the main trend of the whole population in both developing countries and developed countries. As the total number of old population increases, the number of senior patients with indications for ERCP mainly referring to pancreatobiliary diseases has accordingly ascended. ERCP has been proved to provide substantial benefits in old patients when compared with surgery13,14,15,16. However, little experience has accumulated so far5,17,18,19. Our study is the first to demonstrate the clinical characteristics and long-term outcomes of very old patients undergoing ERCP in China.
In recent years, the number of very old patients undergoing ERCP in our endoscopy center has been increasing. China is the largest developing country and has a vast aging population, which can explain this increase. However, the percentage of ERCP done on old people was still less than that reported in developed countries (0.6% vs. 2.9–3.1%)7,27. This may be related to the different proportions and life expectancies of aged populations in various countries. In Japan, the USA, UK and Spain, the life expectancy is 82.6, 78.2, 80.5 and 80.9 years old, respectively, while the life expectancy in China is 73.0 years old, according to the UN reports on a survey of 2005–2012 (Table 4)1. In addition, only 5.1% (4/78) of patients underwent emergency ERCP over 15 years, which is much lower than that of other regions. In Hong Kong, Hui et al. even reported that 64 patients aged 90 years and above with severe acute cholangitis underwent emergent biliary decompression with ERCP in a six-year period5.
In the present study, abdominal pain was less felt by patients aged 90 years and over. The probable explanation is that the elderly have a decreased ability to experience sensations such as pain, or there is interference such as drugs or concomitant diseases that can reduce the sensitivity to pain20. As expected, more patients with chronic concomitant diseases were seen in Group A.
In addition, the complication rate after therapeutic ERCP in the present study was 7.7% in Group A, which is within the range (2.5% to 13.0%) reported by others (Table 4). There was no difference in the complication rate between the two groups. These findings are in accordance with those observed in previous studies7,21. However, particular attention should be paid to the happening of the complications in the elderly particularly with chronic concomitant diseases, because such senior patients are more likely to be associated with delayed recovery and subsequent multiple organ dysfunctions14,15.
We observed different spectra of post-ERCP diagnosis (primary diseases) in two groups. The existence of different prevalence of diseases among different age groups may explain the different spectra. Periampullary diverticula and papilla in diverticula were more frequently observed in Group A than in Group B (P < 0.001). This observation further confirms that the prevalence of periampullary diverticula increases with age6,22,23.
The long-term outcomes of the 61 patients in Group A were available. Only seven of them were alive at the final follow-up. The main causes for death were concomitant diseases leading to multiple organ failures including cardiopulmonary system. As expected, patients with malignant diseases died earlier than those with choledocholithiasis with a median survival time of 13 vs. 27 months, respectively. These results were similar to those of previous studies. Sugiyama et al. in Japan reported that of 22 patients over 90 years old who underwent endoscopic sphincterotomy for choledocholithiasis, six were still alive (mean follow-up period 30.8 months) and the remaining 16 patients died of non-biliary diseases (mean survival time, 33.6 months)7. Rodriguez-Gonzdlez et al. found that 38 of 99 patients died of causes unrelated to ERCP procedures or the indications for the procedure with a mean survival of 22.5 months27. These findings indicate that ERCP may only be a tool to alleviate the discomfort/symptoms for very old patients with appropriate indications, but it was inferred that ERCP per se may not have significant impact on the life expectancy in general; however, studies directly comparing the survival between very elderly patients with ERCP and those without are required to further assess the impact of ERCP on the improvement of symptoms and survival. Interestingly, we note that in the present study, complete extraction of bile duct stones was associated with prolonged survival, compared with incomplete extraction in patients with choledocholithiasis. The main reason may be associated with the fact that incomplete extractions were always involved in much difficult complex situation or the patients could not tolerate. This finding is encouraging and suggests that great efforts should be made on clearance of all stones in the bile duct as completely as possible during ERCP.
There are a few limitations in the present study. First, the retrospective design may lead to bias. Second, this study focused on data from a single center. ERCP-related complications have been known to be associated with endoscopists' experience24,25. Third, 17 patients in Group A were lost during follow-up, which may have some effect on the final results.
In conclusion, therapeutic ERCP in elderly patients aged 90 years or over is comparable to young patients in efficacy and safety. The number of old patients aged 90 years or over undergoing therapeutic ERCP has increased in China, but the percentage of ERCP, especially emergency ERCP for these patients are still relatively low. Most cases die of severe concomitant diseases during the long-term follow-up. In patients with choledocholithiasis, complete clearance of bile duct stones is associated with longer survival time.
Methods
Patients
Consecutive patients with therapeutic ERCPs performed between January 1996 and December 2010 in Changhai Hospital were reviewed. Patients aged 90 years or older who were eligible for study were recruited and defined as Group A. All these patients' first ERCP procedures at or over the age 90 years old were analyzed. Then, four consecutive patients matching one index patient in Group A were included as controls and defined as Group B. The matching patients were recruited if they were <65 years old and of the same sex as the index patient in Group A. Indication for ERCP was failure of biliary drainage caused by various causes including unresectable biliary tumors, choledocolithiasis and stenosis, etc. Patients who were known to be more suitable or required for surgeries, such as those with resectable malignancy, or who had a poor general physical status (i.e. ASA ≥ 5) and thus may not tolerate ERCPs, were excluded.
Data collected included age, sex, clinical symptoms at admission, important chronic concomitant diseases and ASA scores (supplementary Table S1)8. Chronic concomitant diseases were mainly classified as follows: cardiovascular (hypertension, ischemic heart disease, heart failure, cardiac arrhythmia), neurologic (previous stroke), pulmonary diseases (chronic obstructive pulmonary disease, asthma bronchiale), diabetes mellitus, renal diseases and liver cirrhosis. Primary diseases were defined as post-ERCP diagnoses.
This study was approved by the Ethics Committee of Changhai Hospital, Second Military Medical University, Shanghai, China according to the Treaty of Helsinki. Written informed consent was obtained from all participating patients. All the methods were carried out in accordance with the approved guidelines.
Therapeutic ERCP procedures
For the therapeutic ERCP, the endoscopic procedure was performed under conscious sedation with intravenously administered diazepam 2.5–5.0 mg and pethidine 25–50 mg. In our hospital, only when pediatric patients cannot tolerate ERCP, general anesthesia was given9. No ERCP was performed with the patient under general anesthesia in this study. All ERCP procedures were performed by experienced endoscopists. The procedures were performed with standard endoscopes (Olympus duodenoscope JF-240/JF260V/TJF240/TJF260). Endoscopic sphincterotomy was performed if necessary. For bile duct stone removal, the standard techniques (i.e. dormia basket, or extraction balloon or both) were used. Tannenbaum endoprostheses, double-pigtail and metallic stents were used as appropriate for duct drainage. Nasobiliary or nasopancreatic catheters were inserted for temporary drainage if necessary. In the postprocedure recovery period, electrocardiogram monitoring, continuous pulse oximetry, blood pressure monitoring and clinical observation of the patient was done by an endoscopy nurse.
The degree of the procedural difficulty was classified into 5 categories according to Schutz et al10. Post-ERCP complications and their severity were defined according to Cotton's criteria (supplementary Table S2)11,12. Complications were defined as those that occurred within 30 days from ERCP. Procedure-interrupting events such as hypoxia (decrease in oxygen saturation below 90% for almost 2 minutes), hypotension (decrease in systolic blood pressure below 90 mmHg for 2 minutes), etc. were defined as ERCP intolerance.
For all patients, success was defined as when the biliary ducts were successfully drained and failure was defined as unsuccessful cannulation and drainage. Considering choledocholithiasis, extraction of bile duct stones was categorized into complete (defined as when all bile duct stones were extracted) and incomplete (defined as when there were still residual stones).
Follow-up
All patients were followed up yearly, with the last follow-up being conducted in February 2013. A questionnaire was created by the authors and answered through personal telephone interviews to patients and/or their relatives. All follow-up data were collected and analyzed. Parameters recorded in the questionnaire included were follow-up time, general health, subsequent endotherapy of primary diseases and, if the patient died, the cause of death. Survival analysis was compared between patients with malignant primary diseases and patients with choledocholithiasis. Besides, for patients with choledocholithiasis, whether the bile duct stones were completely cleared during the ERCP was determined by the latest medical records of the patients. The differences in ages, ASA scores, concomitant diseases and survival between patients with and those without complete clearance were determined.
Statistical analyses
Continuous variables are expressed as means ± standard deviation or median (range) and categorical data as percentages. Differences in categorical variables between the two groups were determined by the Chi-squared test with the Yates' correction or the Fisher exact probability test, whenever applicable. Kaplan-Meier survival curves were checked by log-rank test. A P value (2-tailed) of less than 0.05 was considered as statistically significant.
References
World Health Organization. World Health Report 2003: shaping the future. Geneva: World Health Organization (2003).
Ross, S. O. & Forsmark, C. E. Pancreatic and biliary disorders in the elderly. Gastroenterol Clin North Am 30, 531–545 (2001).
Mönkemüller, K., Fry, L. C., Malfertheiner, P. & Schuckardt, W. Gastrointestinal endoscopy in the elderly: current issues. Best Pract Res Clin Gastroenterol 23, 821–827 (2009).
Clarke, G. A., Jacobson, B. C., Hammett, R. J. & Carr-Locke, D. L. The indications, utilization and safety of gastrointestinal endoscopy in an extremely elderly patient cohort. Endoscopy 33, 580–584 (2001).
Hui, C. K. et al. Outcome of emergency ERCP for acute cholangitis in patients 90 years of age and older. Aliment Pharmacol Ther 19, 1153–1158 (2004).
Katsinelos, P. et al. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc 63, 417–423 (2006).
Sugiyama, M. & Atomi, Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc 52, 187–191 (2000).
Owens, W. D., Felts, J. A. & Spitznagel, E. L. Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49, 239–243 (1978).
Li, Z. S. et al. A long-term follow-up study on endoscopic management of children and adolescents with chronic pancreatitis. Am J Gastroenterol 105, 1884–1892 (2010).
Schutz, S. M. & Abbott, R. M. Grading ERCPs by degree of difficulty: a new concept to produce more meaningful outcome data. Gastrointest Endosc 51, 535–539 (2000).
Cotton, P. B. et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37, 383–393 (1991).
Liao, Z. et al. China ERCP Live Demonstration and Education Study Group. How safe and successful are live demonstrations of therapeutic ERCP? A large multicenter study. Am J Gastroenterol 104, 47–52 (2009).
Ganzalez, J. J. et al. Biliary lithiasis in the elderly patient: morbidity and mortality due to biliary surgery. Hepatogastroenterology 44, 1565–1568 (1997).
Lei, W. Y., Chang, W. H. Endoscopic retrograde cholangiopancreatography in elderly patients. Int J Gerontol 1, 83–88 (2007).
Cohen, J. R., Johnson, H., Eaton, S., Sterman, H. & Wise, L. Surgical procedures in patients during the tenth decade of life. Surgery 104, 646–651 (1988).
Salminen, P. & Grönroos, J. M. Anesthesiologist assistance in endoscopic retrograde cholangiopancreatography procedures in the elderly: is it worthwhile? J Laparoendosc Adv Surg Tech A 21, 517–519 (2011).
Smith, A. C., Dowsett, J. F., Russell, R. C., Hatfield, A. R. & Cotton, P. B. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bile duct obstruction. Lancet 344, 1655–1660 (1994).
Ashton, C. E., McNabb, W. R., Wilkinson, M. L. & Lewis, R. R. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing 27, 683–688 (1998).
Mac Mahon, M., Walsh, T. N., Brennan, P., Osborne, H. & Courtney, M. G. Endoscopic retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology 39, 28–32 (1993).
Sorkin, B. A., Rudy, T. E., Hanlon, R. B., Turk, D. C. & Stieg, R. L. Chronic pain in old and young patients: differences appear less important than similarities. J Gerontol 45, 64–68 (1990).
Freeman, M. L. Complications of endoscopic biliary sphincterotomy: a review. Endoscopy. 29, 288–297 (1997).
Lobo, D. N., Balfour, T. W. & Iftikhar, S. Y. Periampullary diverticula: consequences of failed ERCP. Ann R Coll Surg Engl 80, 326–331 (1998).
Tyagi, P., Sharma, P., Sharma, B. C. & Puri, A. S. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surg Endosc 23, 1342–1345 (2009).
Loperfido, S. et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48, 1–10 (1998).
American Society for Gastrointestinal Endoscopy. Complications of ERCP. Gastrointest Endosc 57, 633–638 (2003).
Mitchell, R. M., O'Connor, F. & Dickey, W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol 36, 72–74 (2003).
Rodríguez-González, F. J. et al. ERCP in patients 90 years of age and older. Gastrointest Endosc 58, 220–225 (2003).
Author information
Authors and Affiliations
Contributions
L.H., X.S. and J.H.: Provision of study material, collection, assembly, analysis and interpretation of data, manuscript writing. T.X., M.L., L.X., T.S., M.L. (Muyun Liu), W.Z., B.Y.: Collection of clinical data and follow-up records. F.L., D.W. and N.C.: Diagnosis of patients and endoscopic interventions. Z.L. and Z.L. (Zhaoshen Li): Conception, design and reviewed the paper. All the authors reviewed and approved the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Table S1, Supplementary Table S2
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Hu, L., Sun, X., Hao, J. et al. Long-term Follow-up of Therapeutic ERCP in 78 Patients Aged 90 Years or Older. Sci Rep 4, 4918 (2014). https://doi.org/10.1038/srep04918
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep04918
This article is cited by
-
Safety and Efficacy of Endoscopic Retrograde Cholangiopancreatography in Nonagenarians: A Systematic Review and Meta-Analysis
Digestive Diseases and Sciences (2022)
-
Safety and Efficacy of Endoscopic Retrograde Cholangiopancreatography in Patients with Performance Status 4
Digestive Diseases and Sciences (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.