Abstract
Spirooxindoles are a class of compounds with diverse biological activity. Previously, we identified a series of spirooxindole-pyranopyrimidine compounds that exhibited broad-spectrum anti-cancer activity. In this study, we evaluated one of these compounds, JP-8g, on mouse models and found that it showed potent in vivo anti-inflammatory activity. Further investigation suggested that JP-8g may execute its anti-inflammatory activity through nitric oxide synthase signaling pathways. Our results suggest that these spirooxindole-pyranopyrimidine class compounds have potential for not only cancer treatment but also inflammation therapy.
Similar content being viewed by others
Introduction
Nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications for relief of inflammatory conditions1. In the United States, over 40 distinct compounds have been approved by Food and Drug Administration (FDA), with almost 1,000 brands, formulations and doses available2.
Despite all kinds of NSAIDs available, it have been found that administration of NSAIDs is usually associated with gastrointestinal complications1. Recent studies have also warned the potential increased risks of cardiovascular3 and renal4 events with the use of NSAIDs. Although efforts have been taken to develop new NSAIDs, adverse effects of NSAIDs remain a major concern in many patients, particularly the elderly with long-term use of NSAIDs1. Further improvement on treatment of inflammation requires more detailed understanding of inflammatory biology, careful consideration of treatment for different patient population and perhaps development of new anti-inflammatory drugs with high efficacy yet low side effects.
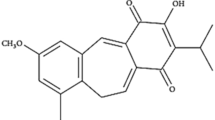
Chiral spiroindoles are increasingly important lead compounds for a wide range of biologically active molecules5,6,7. In a previous study, we reported a novel approach to synthesize spirooxindole-type pyranopyrimidines with both high yield and enantioselectivity8,9. Importantly, one such compound, namely JP-8g (Figure 1), exhibited broad spectrum of anti-cancer activity9. This feature indicates that JP-8g may involve in a major signaling pathway of tumor progression and, perhaps, mediate other physiological processes as well. In this study, we evaluated JP-8g on three different mouse models and show that it also acts as an anti-inflammatiory small molecule. Further studies suggest that JP-8g may execute anti-inflammatory activities via nitric oxide synthase (NOS) signaling pathway.
Results
JP-8g is not toxic at concentrations of 10 μM and below
We first evaluated the cytotoxicity of JP-8g on mouse primary peritoneal macrophages. While JP-8g resulted in reduced cell viability at high concentration (50 μM), it showed very little toxicity at low concentrations (10 μM or below) (Figure 2). This is consistent with our previous observation that normal cells were relatively tolerant to JP-8g9. Therefore, JP-8g were used at concentrations no more than 10 μM for all the following in vitro experiments.
Cytotoxicity of JP-8g on mouse primary peritoneal macrophages.
Macrophages were treated with JP-8g of various concentrations for 24, 48 and 72 h. LPS (1 μg/mL) was included as a control. Cell viability was determined by MTT assay. All data are normalized to those of vehicle under corresponding incubation time. Data are expressed as mean ± s.e.m. (n = 5). Statistical analysis was performed by two-way ANOVA, followed by Tukey's post-test. (*, p < 0.01; **, p < 0.001).
Evaluation of anti-inflammatory activity of JP-8g by mouse ear edema model
The anti-inflammatory activity of JP-8g was first evaluated on xylene-induced ear edema model. As shown in Figure 3A, intraperitoneal (i.p.) injection of JP-8g efficiently inhibited the exudative process caused by xylene. Notably, 50 mg/kg (96 μmol/kg) of JP-8g inhibited edema by at least 50% whereas indomethacin required 100 mg/kg (140 μmol/kg) dosing to achieve the same inhibition. The anti-edematous activity of JP-8g was further verified by oral administration (p.o.). In this case, JP-8g efficiently prevented ear edema at doses of as low as 10 mg/kg (14 μmol/kg), similar to the efficacy of indomethacin (Figure 3B).
Anti-inflammatory activity of JP-8g on xylene-induced ear inflammation model.
JP-8g of varying doses was i.p. (A) or p.o. (B) administrated. A reference NSAID drug indomethacin (IND) was also included. Data are presented as mean ± s.e.m. (n = 10). Statistical analysis was performed by one-way ANOVA, followed by Tukey's post-test (**, p < 0.01; ***, p < 0.001).
Evaluation of anti-inflammatory activity of JP-8g by paw inflammation model
We next assessed the anti-inflammatory activity of JP-8g by paw inflammation model where carrageenan was administrated by subcutaneous (s.c.) injection to induce a developing swelling of the paws in mice10. The vehicle control indicated that paw inflammation reached maximum at 4–6 h period after carrageenan injection (Figure 4). Progression of inflammation was significantly inhibited during 4–6 h period even with low dose (12.5 mg/kg) of JP-8g. Higher JP-8g doses (25 and 50 mg/kg) showed remarkable anti-inflammatory activity and prevented progression of inflammation for extended time. Most surprisingly, JP-8g (25 and 50 mg/kg) showed similar efficacy to a steroidal anti-inflammatory drug dexamethasone (DEX, 5 mg/kg).
Anti-inflammatory activity of JP-8g evaluated by carrageenan-induced paw inflammation model.
A steroidal anti-inflammatory drug dexamethasone (DEX) was used as a reference compound. Data are shown as mean ± s.e.m. (n = 7) and significant difference between vehicle and JP-8g was analyzed by ANOVA, followed by Tukey's post-test (*, p < 0.05; **, p < 0.01; ***, p < 0.001).
Evaluation of anti-inflammatory activity of JP-8g by neuroinflammation model
To induce acute neuroinflammation, LPS was intracerebroventricular (i.c.v.) injected in the third ventricle of mice. This induced an increase in body temperature during a period of 3–5 h, with a peak at 4 h (Figure 5, LPS). Co-injection of JP-8g efficiently reduced LPS-stimulated increase of body temperature over the entire examined period. Notably, JP-8g with very dose (50 pg/kg) could still efficiently relieve acute neuroinflammation.
Evaluation of the anti-inflammatory activity of JP-8g on LPS-induced acute neuroinflammation model.
Data are shown as mean ± s.e.m. (n = 7). Significant difference between JP-8g samples and LPS was calculated by two-way ANOVA, followed by Tukey's post-tests, (*, p < 0.05; **, p < 0.01; ***, p < 0.001).
Nitric oxide synthase signaling pathway is involved in the anti-inflammatory activity of JP-8g
To understand the mechanism of action of JP-8g, we examined the effect of JP-8g on NO release of mouse primary peritoneal macrophages. As shown in Figure 6, JP-8g attenuated LPS-induced NO production in a dose-dependent manner. Furthermore, administration of the inducible NOS (iNOS) inhibitor SMT11 and endothelial NOS (eNOS) antagonist L-NAME significantly reduced the anti-inflammatory activity of JP-8g (Figure 7) whereas and the neuronal NOS (nNOS) antagonist spermidine12 did not have significant impact on JP-8g (Figure S1). Overall, these results suggested that NOS signaling pathway may be involved in the JP-8g-mediated anti-inflammatory process.
iNOS inhibitor SMT and eNOS inhibitor L-NAME inhibited the in vivo anti-inflammatory activity of JP-8g.
Results are shown as means ± s.e.m. (n = 7). Significant difference between JP-8g administration in the absence and presence of inhibitors during 4–6 h period was analyzed by two-way ANOVA followed by Tukey's post-tests (*, p < 0.05; **, p < 0.01; ***, p < 0.001).
Discussion
NSAIDs are a group of compounds with chemically distinct structures. NSAIDs alleviate inflammation by inhibiting cyclooxygenase (COX)13,14. Most of the non-selective cyclooxygenase (COX) inhibitors are one- or two-ringed compounds, while COX-2 selective inhibitors usually contain three rings with a bulky side chain. JP-8g structure is relatively larger than NSAIDs but is tightly packaged into compact space. We have shown in this study that spirooxindole pyranopyrimidine molecule JP-8g exhibits potent in vivo anti-inflammatory activities. To the best of our knowledge, JP-8g represents a novel scaffold that has not been reported before.
To understand the signaling pathways that may be involved in the anti-inflammatory activity of JP-8g, we first sought to study the effect of JP-8g on LPS-stimulated nuclear translocation of p65 in primary macrophages. We found that pre-incubation of JP-8g with primary macrophages had no significant effect on LPS-induced nuclear translocation of p65 (Figure S2). More importantly, administration of NF-κB pathway inhibitors pyrrolidine dithiocarbamate (PDTC)15 and BAY 11-708216 did not result in significant reduction of the in vivo anti-inflammatory activity of JP-8g (Figure S3). Taken together, these data suggested that the NF-κB signaling pathway is not involved in the anti-inflammatory activity of JP-8g. This feature can be an advantage of JP-8g because recent studies have highlighted the beneficial sides of NF-κB17,18.
Therefore, we intended to explore other signaling pathways that may be involved in the anti-inflammatory activity of JP-8g. Nitric oxide (NO) is an important signal transducer of the inflammation process, mediating a wide variety of physiological processes in pain signaling and immune response. NO plays an important role in the function execution of macrophages, which are key immune response cells during inflammation processes19. In this study, we show that JP-8g can attenuate LPS-induced NO production in macrophages in a dose-dependent manner. In vivo inhibition studies also supported that NOS is involved in the anti-inflammatory activity of JP-8g (Figure 7).
In conclusion, JP-8g is a bifunctional molecule that exerts both anti-cancer and anti-inflammatory activities. Although the detailed mechanisms of the dual activities of JP-8g are yet to be elucidated, our study shed the light on that spirooxindole-pyranopyrimidine class compounds have great potential for not only cancer treatment but also inflammation therapy.
Methods
Ethics statement
All animal experiments were performed in accordance with the guidelines of China Council on Animal Care and Use. All animal procedures carried out in this study were reviewed, approved and supervised by the Institutional Animal Care and Use Committee of the Ethics Committee of Lanzhou University, China.
Cell viability assay
Cytotoxicity of JP-8g was assessed on mouse primary peritoneal macrophages. Primary peritoneal macrophages were isolated as described in Supporting Information. Macrophages were maintained in RPMI 1640 medium (Life Technologies, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS) (Life Technologies) throughout the experiments. Cytotoxicity was assessed by standard MTT assay. Briefly, 5 × 103 cells were seeded on to each well in 96-well plates. At 24 h after seeding, JP-8g of concentrations ranging from 3.2 nM to 50 μM was added to corresponding wells with a final volume of 100 μL. Lipopolysaccharide (LPS, serotype 0111:B4 from Escherichia coli) was used as a control. Cells were kept at 37°C for 24, 48 or 72 h and then thiazolyl blue tetrazolium bromide (MTT) (Sigma-Aldrich Corp., St. Louis, MO, USA) was added to each well to a final concentration of 0.5 mg/mL. After 4 h of incubation at 37°C, the medium was removed and then the dye crystals were removed by DMSO (Sigma) wash. The absorbance at 490 nm was obtained using BioRad ELISA plate reader 680 (BioRad, Hercules, CA, USA).
Animal experiments
The in vivo evaluation of anti-inflammatory activity of JP-8g was performed in male C57B/J mice. All animals were kept and the experiments were performed in accordance with the European Community guidelines for the use of experimental animals (86/609/EEC). All the protocols in this study were executed under the guideline of the Ethics Committee of Lanzhou University, China. Male C57B/J mice (18–22 g) were housed at 20–23°C with relative humidity of 65–75% for 1 week before the experiments, provided with a settled 12 h light/darkness cycle and access to food and water ad libitum. Animals received human care and all efforts were undertaken to minimize animal suffering before and during experiments.
Xylene-induced ear edema model
Topical application of xylene caused acute inflammation characterized by edema and granulocytic cell infiltration into the skin. Experiments were executed as described previously20. Briefly, mice were intraperitoneally (i.p.) or orally (p.o.) administrated with vehicle, JP-8g and a traditional NSAID indomethacin as a reference. At 30 min after drug administration, 10 μL of 2.5% (v/v) xylene dissolved in acetone solution was applied to the anterior and posterior surface of the right ear. The left ear remained untreated. Control animals received only the irritant, while the test mice received both the irritant and drugs. At the time of maximum inflammatory response (~3 h after xylene treatment), mice were sacrificed by cervical dislocation and a tissue disk of 6 mm diameter was cut from each ear lobe. Edema was calculated by the difference in weight between the samples from right treated and left untreated ears.
Carrageenan-induced paw inflammation model
Acute paw inflammation was induced by intraplantar (i.pl.) injection of carrageenan into the right hind paws of mice10. In this experiment, 35 mice were divided into five groups with seven mice in each group. Mice in group 1 received an i.pl. treatment of 60 μL vehicle (5% DMSO, 5% Cremophor EL and 90% saline, v/v). At 30 min after treatment, 25 μL of saline containing 5% (v/v) DMSO, 5% (v/v) Cremophor EL (Sigma) and 1% (w/v) carrageenan (Sigma) was applied to the right footpad by subcutaneous (s.c.) injection and 25 μL saline was applied to the left footpad. In group 2–4, mice were i.pl. injected with 300 μL JP-8g of varying doses (12.5 mg/kg, 25 mg/kg and 50 mg/kg), followed by s.c. injection of carrageenan at 30 min after drug pre-treatment. Group 5 was i.pl. treated with 300 μL of 5 mg/kg DEX as a reference drug and carrageenan was s.c. injected at 30 min after DEX injection. For the in vivo inhibition experiments, mice were i.pl. administrated with 25 mg/kg of JP-8g in the absence or presence of NOS inhibitors S-methylisothiourea (SMT), Nω-nitro-L-arginine methyl ester (L-NAME) and spermidine trihydrochloride (all purchased from Sigma). The thickness of left and right footpads was measured using a caliper at 1, 2, 3, 4, 5, 6, 24 and 48 h post dosing. The difference in the thickness of left untreated and right treated footpads was calculated and presented to indicate the effects of anti-inflammatory drugs and inhibitors. This study was executed in a blinded manner.
LPS-induced acute neuroinflammation model
In this experiment, 35 mice were divided into five groups with seven mice in each group. The mice were fixed in specially designed restraining device21. A thermistor probe (Beijing No.1 Machine Tool (Gaobeidian) Forging Corporation, Beijing, China) was inserted into the rectum (to a depth of 2.5 cm) and the rectal temperature was recorded by a connected a BL-420E+ recorder (Taimeng Technology Corporation, Chengdu, Sichuan, China). LPS (5 ng/kg) or LPS mixed with JP-8g (50, 250 and 500 pg/kg) were prepared in solutions in 4 μL final volume and then i.c.v. injected in the third ventricle of mice as described before8,22. Rectal temperature was recorded at different time points as an indicator for neuroinflammation. All experiments were performed between 9 and 10 AM to minimize the effect of circadian variation of animals.
Nitrite assay for estimation of NO production
Primary peritoneal macrophages (1 × 104/well) were plated in 96-well plates with MEM media, supplemented with 10% heat-inactivated FBS (Life Technologies). Cells were pre-treated with JP-8g of various concentrations for 24, 48 and 72 h, respectively. Thereafter, cells were changed into fresh medium containing 1 μg/mL of LPS and then incubated for 24, 48 or 72 h. After LPS treatment, 100 μL supernatant was transferred into new wells and 100 μL Griess reagent (Sigma) was added to each well as described23. The reaction was incubated at room temperature for 15 min and the absorbance at 550 nm was determined using Tecan infinite M200 (Tecan Group, Männedorf, Switzerland). NO production was calculated according to a standard curve of sodium nitrite of known concentrations.
References
Roth, S. H. Coming to terms with nonsteroidal anti-inflammatory drug gastropathy. Drugs 72, 873–879 (2012).
Grosser, T., Yu, Y. & Fitzgerald, G. A. Emotion recollected in tranquility: lessons learned from the COX-2 saga. Annu Rev Med 61, 17–33 (2010).
Fosbol, E. L. et al. Cause-specific cardiovascular risk associated with nonsteroidal antiinflammatory drugs among healthy individuals. Circ. Cardiovasc. Qual. Outcomes 3, 395–405 (2010).
Whelton, A. Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Am. J. Med. 106, 13S–24S (1999).
Ding, K. et al. Structure-based design of potent non-peptide MDM2 inhibitors. J. Am. Chem. Soc. 127, 10130–10131 (2005).
Rottmann, M. et al. Spiroindolones, a potent compound class for the treatment of malaria. Science 329, 1175–1180 (2010).
Vintonyak, V. V. et al. Identification of thiazolidinones spiro-fused to indolin-2-ones as potent and selective inhibitors of the Mycobacterium tuberculosis protein tyrosine phosphatase B. Angew. Chem. Int. Ed. Engl. 49, 5902–5905 (2010).
Jiang, X. et al. A unique approach to the concise synthesis of highly optically active spirooxazolines and the discovery of a more potent oxindole-type phytoalexin analogue. J. Am. Chem. Soc. 132, 15328–15333 (2010).
Jiang, X. et al. Core Scaffold-Inspired Concise Synthesis of Chiral Spirooxindole-Pyranopyrimidines with Broad-Spectrum Anticancer Potency. Adv. Synth. Catal. 354, 917–925 (2012).
Henriques, M. G. et al. Mouse paw edema. A new model for inflammation? Braz. J. Med. Biol. Res. 20, 243–249 (1987).
Szabo, C., Southan, G. J. & Thiemermann, C. Beneficial effects and improved survival in rodent models of septic shock with S-methylisothiourea sulfate, a potent and selective inhibitor of inducible nitric oxide synthase. Proc. Natl. Acad. Sci. U. S. A. 91, 12472–12476 (1994).
Maragos, C. M. et al. Complexes of .NO with nucleophiles as agents for the controlled biological release of nitric oxide. Vasorelaxant effects. J. Med. Chem. 34, 3242–3247 (1991).
DeWitt, D. L. & Smith, W. L. Primary structure of prostaglandin G/H synthase from sheep vesicular gland determined from the complementary DNA sequence. Proc. Natl. Acad. Sci. U. S. A. 85, 1412–1416 (1988).
Smith, W. L. & Dewitt, D. L. Prostaglandin endoperoxide H synthases-1 and -2. Adv. Immunol. 62, 167–215 (1996).
Bessho, R. et al. Pyrrolidine dithiocarbamate, a potent inhibitor of nuclear factor kappa B (NF-kappa B) activation, prevents apoptosis in human promyelocytic leukemia HL-60 cells and thymocytes. Biochem. Pharmacol. 48, 1883–1889 (1994).
Mori, N. et al. Bay 11-7082 inhibits transcription factor NF-kappaB and induces apoptosis of HTLV-I-infected T-cell lines and primary adult T-cell leukemia cells. Blood 100, 1828–1834 (2002).
Chien, Y. et al. Control of the senescence-associated secretory phenotype by NF-kappaB promotes senescence and enhances chemosensitivity. Genes Dev. 25, 2125–2136 (2011).
Jing, H. et al. Opposing roles of NF-kappaB in anti-cancer treatment outcome unveiled by cross-species investigations. Genes Dev. 25, 2137–2146 (2011).
Schmidtko, A., Tegeder, I. & Geisslinger, G. No NO, no pain? The role of nitric oxide and cGMP in spinal pain processing. Trends Neurosci. 32, 339–346 (2009).
Rotelli, A. E., Guardia, T., Juarez, A. O., de la Rocha, N. E. & Pelzer, L. E. Comparative study of flavonoids in experimental models of inflammation. Pharmacol. Res. 48, 601–606 (2003).
Rosow, C. E., Miller, J. M., Pelikan, E. W. & Cochin, J. Opiates and thermoregulation in mice. I. Agonists. J. Pharmacol. Exp. Ther. 213, 273–283 (1980).
Frances, B., Lahlou, H. & Zajac, J. M. Cholera and pertussis toxins inhibit differently hypothermic and anti-opioid effects of neuropeptide FF. Regul. Pept. 98, 13–18 (2001).
Ding, A. H., Nathan, C. F. & Stuehr, D. J. Release of reactive nitrogen intermediates and reactive oxygen intermediates from mouse peritoneal macrophages. Comparison of activating cytokines and evidence for independent production. J. Immunol. 141, 2407–2412 (1988).
Acknowledgements
This study was supported by the National Natural Science Foundation of China (Nos. 91213302, 20932003 and 21272102), the Key National S&T Program “Major New Drug Development” of the Ministry of Science and Technology of China (2012ZX09504001-003) and the Program for Changjiang Scholars and Innovative Research Team in University (PCSIRT:IRT1137).
Author information
Authors and Affiliations
Contributions
Y.S., J.L., X.J. and R.W. designed and advised the experiments and wrote the manuscript. J.L. and Y.S. analyzed the data. T.S., X.Z. and Y.S. performed the animal experiments. J.Y. and M.K. carried out the cell viability and biochemical examination. X.J. synthesized the JP-8g.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Anti-cancer small molecule JP-8g exhibits potent in vivo anti-inflammatory activity
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Sun, Y., Liu, J., Sun, T. et al. Anti-cancer small molecule JP-8g exhibits potent in vivo anti-inflammatory activity. Sci Rep 4, 4372 (2014). https://doi.org/10.1038/srep04372
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep04372
This article is cited by
-
Azomethine ylide cycloaddition: a versatile tool for preparing novel pyrrolizidino-spiro-oxindolo hybrids of the doubly conjugated alkamide piperine
Molecular Diversity (2020)
-
Cerium oxide-catalyzed multicomponent condensation approach to spirooxindoles in water
Molecular Diversity (2016)
-
One-Step Synthesis of Chiral Oxindole-type Analogues with Potent Anti-inflammatory and Analgesic Activities
Scientific Reports (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.