Key Points
-
Bulimia nervosa is a psychological disorder which has serious implications for oral health.
-
Points out that, given the relatively high prevalence of this disorder among young people, dental practitioners are likely to encounter individuals with bulimia nervosa.
-
Discusses the likely oral manifestations of the disorder, which will enable the practitioner to plan comprehensive treatment.
Abstract
Eating disorders are a potentially life-threatening group of mental disorders, which affect a patient's relationship with food and their body. This manifests itself through chaotic and disordered eating habits. One such eating disorder is bulimia nervosa, which has a lifetime prevalence of 1%. While there is consensus that bulimic behaviour directly causes dental erosion due to vomiting and acidic food choices, there is less clear evidence for a direct link between bulimia nervosa and dental caries, although there does still appear to be an association. Reduced salivary flow rate is a common feature among bulimics, but this is often due to anti-depressant medication rather than dietary habits or vomiting, and the effects are largely limited to unstimulated whole salivary flow rate and don't affect stimulated whole salivary flow rate. Parotid enlargement is present in a number of cases but this tends to be a minority. Further research is required given the limitations of current studies, especially gender imbalances among the populations studied and a lack of clear focus on bulimia nervosa.
Similar content being viewed by others
Introduction
The Eating Disorders are a group of mental disorders that manifest themselves in chaotic or distorted eating due to the poor relationship that patients have with food and their body.1 The three main types of eating disorders are anorexia nervosa (anorexia), bulimia nervosa (bulimia) and binge eating disorder.2 This review will focus primarily on bulimia nervosa. The diagnostic criteria for bulimia nervosa according to DSM V are outlined in Box 1.
Bulimia in the literature
Prevalence of bulimia nervosa
According to the World Health Organisation (WHO) World Mental Health Surveys, which surveyed a total of 24,124 people across 14 different countries, average estimates for lifetime prevalence of bulimia nervosa are 1%.3 The incidence of new cases of bulimia nervosa is reported to be at least 12 per 100,000 per year.4 The mean age of onset of bulimia in the WHO mental health survey was found to be 20.6 years.3
There is very strong evidence for a disparity between the number of male sufferers of eating disorders and the number of female sufferers, with the former being far fewer. It is not clear whether this specifically relates to bulimia although it is likely that prevalence is similar in all eating disorder subtypes. However, there is some disagreement over the exact disparity. For example, the adult psychiatric morbidity survey in 2007 suggested that male sufferers made up to 25% of those with eating disorders.5 In contrast to this, statistics on admitted patients in 2012–13 showed that 9.2% of those admitted to hospital with eating disorders are male.6 It is possible that women are more likely to be hospitalised as a result of their eating disorder, offering an explanation for the discrepancy between these two statistics. Nonetheless, this latter statistic does support previous research that the lifetime prevalence of bulimia is 1.1% among women and 0.1% among men.7
Relevance of bulimia to oral health
In order to identify relevant articles for this review, the MEDLINE database was searched from 1993 to present. This gave the most recent 25 years of studies, which the authors felt would focus on the most up-to-date information while incorporating findings from studies before the search period. The following search terms were used:
-
1
Bulimia/or bulimia nervosa which yielded 8,159 results
-
2
Oral which yielded 565,317 results
-
3
Dent* which yielded 503,330 results
-
4
2 or 3 which yielded 998,702 results
-
5
1 and 4 which yielded 298 results.
Abstracts for the 298 results from the literature search were reviewed and relevant manuscripts were identified. Only studies that collected empirical data on oral health were included. The following review is based primarily on the findings of ten papers. Table 1 summarises the findings of the studies identified in the search.
The symptoms of poor oral health that occur most commonly among vomiting bulimics are dental erosion, dental caries and reduced salivary secretions that lead to xerostomia.8 The dietary choices of many bulimics, whether they are vomiting or non-vomiting type, will also have an effect on oral health. For example, it is well documented that binge eating often involves highly sugary foods which may increase dental caries.9 Furthermore, many bulimics drink acidic sports drinks during physical activity which can lead to dental erosion.1
The fact that bulimia can have such far-reaching effects on the oral cavity puts oral health care professionals in a prime position to screen for bulimics early on10,11 and, thus, makes it crucial to add bulimia and its oral signs to the dental curriculum.12
Reduced salivary flow rate
Saliva plays an essential role in maintenance of oral health, and reduced salivary flow can result in a clinically significant oral imbalance. Reduced salivary flow rate is a common symptom of bulimia (see Table 1). There are a number of explanations for this in addition to vomiting, including dehydration due to excessive exercise,13 and xerostomia due to medication such as anti-depressants.14 Six of the ten included studies provided information about salivary flow rate.9,14,15,16,17,18 In three studies9,14,15 the mean salivary flow rates were provided while in four studies9,16,17,18 the percentage of subjects with hyposalivation was reported.
Dynesen et al.14 conducted one of the principal studies to examine the salivary changes that occur in bulimia nervosa. In their study of 20 bulimics and 20 case controls, the bulimics had a significantly reduced unstimulated whole saliva (UWS) flow rate (p = 0.06) but no significant difference in stimulated whole saliva (SWS) flow rate (p = 0.168). Furthermore, they were able to demonstrate that medication played a large role in this difference. Nonetheless, there was still a difference between non-medicated bulimics and the control group, with the former displaying a mean UWS flow rate of 0.23 ml/min and the latter a mean UWS flow rate of 0.29 ml/min, implying that dehydration resulting from self-induced vomiting is also likely to play a part.
There is increasing evidence for the role that pharmacotherapy might play in treating bulimia. According to NICE guidelines on treatment for bulimia: 'Selective 5-hydroxytryptamine reuptake inhibitors (SSRIs) (specifically fluoxetine) are the drugs of first choice for the treatment of bulimia nervosa in terms of acceptability, tolerability and reduction of symptoms'.19 Many of the published papers in this area do not specify how many bulimics are taking medication. However, in the few papers that do list this data, medication does appear to play a role. This can be clearly demonstrated by Dynessen et al.14 as discussed above (see Table 1 for exact figures). Given that SSRI's can cause xerostomia, it is important for dentists to find out a patient's medication history before treating them, in order to be aware of potential reasons behind certain dental problems, such as caries and erosion.
An individual with lower salivary flow rates is less protected against dental erosion than someone with higher flow rates as a result, in part, of the neutralising effect of saliva,9 but also as a result of the contribution of saliva to the acquired pellicle, which acts as a diffusion barrier against acid erosion.20 Patients with a salivary flow rate of ≤1 ml/min are five times more likely to develop dental erosions than those with higher flow rates.21
Dental erosion
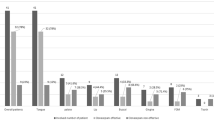
Dental erosion is defined as, 'the irreversible loss of dental hard tissues by a chemical process (acid attack) not involving bacteria'.22 The acids can be of both extrinsic and intrinsic origin. Extrinsic acids are essentially those from the diet, such as fruit juices and carbonated drinks, while intrinsic acids include those from gastro-oesophageal reflux disease and voluntary vomiting as seen in bulimia nervosa.23 Nine of the ten studies included findings on dental erosion.9,14,15,16,17,18,24,25,26
Dental erosion is a frequent oral finding among bulimics.27 Johansson et al.18 reported that patients who self-induced vomiting were 5.5 times more likely to experience dental erosion than healthy controls. This is most likely due to the fact that gastric acid, which has a mean pH of 2.9, affects tooth surfaces severely,9,28 as it is far below the critical pH of 5.5, generally considered necessary to dissolve dental enamel.29,30 Uhlen et al.26 showed that, irrespective of the duration of self-induced vomiting, lesions, be they enamel or dentine lesions, were found predominantly on palatal surfaces of bulimics (46%) followed by occlusal surfaces (36.6%) and buccal surfaces (21.8%). However, the distribution is slightly different if just analysing the lesions into dentine. In this case, severe lesions appear more frequently on the occlusal surfaces of the lower first molars followed by palatal surfaces of anterior incisors.26 A similar pattern is found for erosion of a non-bulimic origin.13 The authors also demonstrated that the duration of self-induced vomiting was directly correlated to the number of lesions present on the palatal surfaces of the front teeth and the lateral segments.26
The primary factor leading to erosion among bulimics is frequent vomiting,9 but extrinsic acid effects due to bulimic's food choices also have an impact on dental erosion. Rytomaa et al. demonstrated that bulimics were more likely to consume herb tea, soft drinks and apple vinegar than healthy controls.9 These types of drinks have been shown to cause dental erosion in a number of studies.31,32 Carbonated drinks were also frequently consumed, often to decrease the reflex stimulus for hunger.33 In a study of 20 bulimics compared with 20 controls, 13 of the bulimics drank fizzy drinks more than four times a week, compared with only four of the controls.14 A study looking at aetiological risk factors linked to tooth wear in 14-year-old children concluded that tooth wear is likely to be linked to frequent consumption of carbonated beverages.32 Many bulimics also frequently consumed acidic sports drinks during exercise,1 which further increases the risk of erosion.
Despite most of the studies reviewed here demonstrating a clear link between bulimia and dental erosion (see Table 1), it must be noted that within these individual studies, not all bulimics demonstrated this pattern.9,16 There can be a number of explanations for these discrepancies, although it is difficult to know exactly which one applies, due to the number of extraneous factors. One explanation could be that some bulimics are aware that refraining from brushing their teeth immediately after self-induced vomiting reduces the risk of erosion,16 while others do not adhere to this recommendation. Alternatively, host factors, such as differences in salivary flow rates, could affect an individual's susceptibility to dental erosion.
Parotid enlargement
Self-induced vomiting may result in enlarged salivary glands, particularly the parotid glands.14 Parotid gland enlargement among bulimics was reported in five studies.14,15,17,18,34 Prevalence estimates ranged between 0 and 80% of bulimia sufferers, but never in control subjects. However, this finding must be treated with caution, given the relatively few studies, and a total patient cohort evaluated of only 53 bulimics.
Price et al.35 used MRI and palpation to demonstrate changes in the size of parotid glands in five purging bulimic in-patients who subsequently stopped vomiting. Two patients showed a decrease of 25.6% and 18.5% in parotid gland volume between the first MRI, two weeks after being admitted, and the second MRI, two months later after a period of vomiting cessation. Furthermore, the palpation at the second check showed reduction in parotid enlargement for three of the five patients. This data backs up the correlation, although it is not overwhelming evidence due to the small number of participants and the small time period between the two scans meaning long-term gland changes were not examined.35
Although commonly associated with vomiting, the precise causes of enlarged parotid glands among bulimics are unclear.36 However, there is much agreement that its effect is to cause a reduced salivary flow rate.14,36 It is important to note, however, that significant vomiting behaviour can still be present even if salivary glands are not enlarged.35 Therefore, it is crucial that clinicians understand that a lack of parotid enlargement does not preclude bulimia.
Dental caries
Seven of the ten analysed studies included data on dental caries,9,15,16,17,18,25,34 with the majority opting to use DMFT to score their findings. Data concerning the relationship between bulimia nervosa and caries experience are equivocal.15 Vomiting may have an effect on the risk of caries, both directly and as a result of reduced salivary flow rate. In addition, the food choices made by bulimics during a binge, which are largely carbohydrate based, will increase caries risk. During binges, bulimics will often eat food that they deny themselves under normal circumstances.37 This tends to involve high energy and sugary foods.9 The Australian National Dietary Survey of Adults released data reporting that bulimics consume 21% more carbohydrates than the national average.38 Dietary carbohydrates are required for the carious process to occur. Thus, a binge, often consisting of a high-sugar diet, is likely to provide the cariogenic microbes with a source of nourishment39 and will, thus, stimulate the carious process.
In the studies reviewed, not all bulimics display a higher DMFT/S than controls.15,18 While there could be a number of explanations for this, including better oral hygiene than controls, there is some evidence to suggest that S. mutans are unable to metabolise below pH values of 4.2 and, due to the lower oral pH as a result of vomiting, bulimics may demonstrate lower caries incidence.40 Furthermore, high fat foods eaten during binges may be protective against caries.41,42
There are many studies, however, that contradict this finding, and show that most bulimics display higher caries levels, not lower.16,21,25 In addition to the explanation of increased access to fermentable carbohydrate during binges, this could be explained by the finding that S. mutans are able to adapt and, thus, still remain active at a pH as low as 3.14, directly challenging the previous findings.43 Young demonstrated that those suffering from eating disorders have much higher than normal counts of S. mutans and a much higher caries frequency.44 Ohrn et al.,16 who also demonstrated higher levels of S. mutans and DMFS among bulimics, support these results. However, neither of these latter two papers discusses the reasons behind the disparity in S. mutans count between eating disorder sufferers and controls. Given both papers were studying eating disorders in general and not just bulimia, one cannot assume that this disparity is due to the effects of vomiting.
Despite evidence to suggest higher and lower levels of S. mutans among bulimics, there are contradictory findings that suggest that there is, in fact, no difference between bulimics and controls. For example, Touyz et al. found no difference in S. mutans levels between the anorexic, bulimic and control groups. This study also concluded that there was no significant difference in the DMFT between the three groups.15 One could, therefore, use this study to argue that levels of S. mutans plays an important role in caries risk as, when levels of the bacteria are normal, DMFT levels are also normal.
To conclude, vomiting may indirectly cause increased risk of caries due to reduced salivary flow rate, and may also directly increase the risk due to higher levels of S.mutans. However, the fact that some studies have not found a difference in DMFT between bulimics and control groups means this conclusion needs to be treated with caution and further research is required, with specific focus on bulimic patients to isolate the effects of vomiting. It would also be useful to analyse oral hygiene behaviours between bulimic and control groups to identify if this could play a role in differences in DMFT, or lack thereof.
Oral-health-related behaviours
While the majority of the dietary differences between bulimics and controls tend to have a negative impact on the oral cavity, chewing gum activity, which is often increased in those with eating disorders, might have a protective effect on the oral cavity. In a case control study of 79 patients with eating disorders (EDs) compared to 48 patients without, the prevalence of intensive gum chewing (more than 3 hours/day) among those with EDs involving vomiting was 77.1% vs 17.9% of the control group (p <0.01).24 While the study doesn't differentiate between vomiting bulimics and vomiting patients with other types of EDs, given bulimia is the main eating disorder type associated with vomiting, it is highly likely these statistics correlate with the bulimic population. Furthermore, the study does not demonstrate whether chewing gum was the cause of vomiting (unlikely) or as a response to it (more likely). Nevertheless, there is evidence to suggest that salivary flow can be increased by chewing gum due to mastication. The salivary flow can elevate plaque pH due to increased concentration of bicarbonate and improved acid-buffering capacity, thus having a protective effect on the oral cavity. However, this effect is only the case if sucrose-free chewing gum is used.45 The studies that mention increased chewing gum frequency among bulimics don't mention whether the gum is sugar free or not and, thus, one can't automatically assume that there is a protective effect. Further questioning of the patients would be required to ascertain this. This might be a useful area to explore in future studies.
Critique of research
Eight out of the ten studies identified for this review adopted a case control methodology14,15,16,18,21,24,25,34 with five of the eight being sex and age matched.9,14,15,18,24 Case controls allow researchers to explore the association between aspects of oral disease and the presence of bulimia nervosa. They are also useful where cases are relatively rare, since the use of matching with controls allows researchers to rule out the effect of other variables on the outcome of interest. Despite this, they do not provide information on the long-term impact of a condition – this would be better determined by longitudinal study designs. Such a design is recommended for future research.
Although half the studies are age- and gender-matched controlled,9,14,15,18,24 more conclusive evidence might be produced if more of the studies matched for other potential confounding variables, such as height and weight, which could affect things such as parotid gland size for example, irrespective of eating disorder effects. Rytomaa et al.9 also made sure that participants were education matched. It would be useful for this to have been the case in more studies, as well as variables such as socio-economic status and ethnicity, which can both have their own impact on oral health, again irrespective of eating disordered behaviour. One way of eliminating this problem would be to adopt the technique carried out by Rytomaa et al., in which there was a ratio of 3:1 controls:bulimics.9 This increases the accuracy of the statistical tests and enhances the validity of the results by reducing the number of variables between the controls and bulimics. This accuracy and validity would be increased even further if a higher ratio was used, although this is obviously much more expensive and time-consuming. Despite the fact that this technique was not widely adopted, on the whole one could still see overall trends between the ten papers, indicating that the lack of these additional controls didn't impact the data to the degree that one would not be able to establish clear links between bulimia and oral health.
There was a lack of diagnostic homogeneity. Only two of the studies9,14 focused solely on bulimia. The other eight also discussed the effects of other eating disorders and, therefore, results will be distorted by results unrelated to bulimic behaviour. Nonetheless, two of these eight studies specifically discussed individual results for those with bulimia as separate to the other eating disorders,15,17 and a further study focused on bulimia in relation to parotid gland enlargement, even if not the other effects.18 Thus, results from these studies can be conclusive with regards to bulimia, even though other eating disorders are investigated. Another of the eight studies focused solely on those who self-induced vomiting.26 While this can also include anorexics and people with eating disorders not otherwise specified (EDNOS), the impact of vomiting, which is a defining feature of bulimia can still be successfully studied. The biggest problem are the two studies that don't differentiate findings between bulimics, anorexics and EDNOS16,24 and the other two that only study those deemed to be at risk of or suspected to have eating disorders, rather than officially diagnosed.25,34 The findings from these studies must be treated with caution, as they could be as a result of eating disorder elements not relevant to bulimia, such as starvation or low weight, as evident in anorexia.
While the majority of bulimia sufferers are women, at least 10% are men. This is clearly a minority, but it is still a significant enough proportion to warrant studies into men. Despite this, only three of the studies actually include men16,18,26 and, even then, the men represent less than 10% of the sample size. Therefore, more studies into the effects of bulimia on oral health in the male population are required, as findings might be different and it can't simply be assumed that results for the female population can be translated into results for the male population.
As specified in DSM V, in order to obtain a diagnosis of bulimia, compensatory methods post-binge need to be present.2 All of the studies in Table 1 and most of the other literature focus on vomiting bulimics. However, it is important to be aware that not all bulimics will vomit as a compensatory method. Some will use laxatives, some will fast and some will over-exercise. It is highly likely that each of these compensatory methods could have their own effect on the oral cavity as separate to the effects of vomiting. However, the research on this is very limited.
A final limitation is the method of collecting data on the behaviours of bulimic subjects. Most studies were self-reported, using questionnaires to ask bulimics about their eating disorder behaviour in order to ascertain things such as frequency of vomiting. It is commonly reported that bulimics feel ashamed of their behaviour and, as a result, while the anonymity of the study design encourages honesty, one has to bear in mind that the actual statistics for things like frequency of vomiting and bingeing may be higher than the bulimic patients admit to. It would be quite difficult, however, to produce a study design which avoided this problem as it is impossible to force patients to disclose information they are not comfortable disclosing.
In summary, in addition to limitations of study design, lack of proportional gender representation, variable matching, sufficient bulimic-specific studies and symptom-specific studies, combined with problems associated with self-reporting, limit the conclusions that can be drawn from the current literature. This leaves scope for further research in this area in the future.
Conclusion
This review has demonstrated that dental erosion, parotid enlargement, reduced salivary flow rate and dental caries are common oral manifestations in patients with bulimia. While a lot of the literature focuses on the effects of vomiting, this review has shown that binge eating and other dietary habits, as well as anti-depressant medication, can also have an effect on a bulimics oral health. Dental health practitioners are often the first to spot signs of bulimia, and, as such, the findings in this review emphasise the importance of incorporating bulimia signs and symptoms into the dental curriculum. Dentists are in a prime position to advise bulimic patients to limit their intake of acidic food and drink, and to advise them on optimal oral hygiene post-vomiting, such as rinsing the mouth with water, chewing gum and avoiding brushing teeth immediately afterwards. These should all help limit the damaging oral effects that unmanaged bulimia can eventually lead to. Research in this area is limited in both quantity and quality and, given the prevalence of the problem, more high quality research is urgently required.
References
Lo Russo L, Campisi G, Di Fede O, Di Liberto C, Panzarella V, Lo Muzio L . Oral manifestations of eating disorders: A critical review. Oral Dis 2008; 14: 479–484.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM5®). Washington D.C: American Psychiatric Publishing, 2013.
Kessler R C, Berglund P A, Chiu W T et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry 2013; 73: 904–914.
Hoek H W, Van Hoeken D . Review of the prevalence and incidence of eating disorders. Int J Eat Disord 2003; 34: 383–396.
McManus S, Meltzer H, Brugha T T, Bebbington P P, Jenkins R . Adult psychiatric morbidity in England, 2007 Results of a household survey. 2009. Available online at http://discovery.ucl.ac.uk/164862/ (accessed September 2017).
Health and Social Care Information Centre. Hospital episode statistics, admitted patient care, England 2012–2013. 2013. Available online at http://www.hscic.gov.uk/catalogue/PUB12566 (accessed September 2017).
Garfinkel P, Lin E, Goering P et al. Bulimia nervosa in a Canadian community sample: prevalence and comparison of subgroups. Am J Psychiatry 1995; 152: 1052–1058.
Kisely S, Baghaie H, Lalloo R, Johnson N W . Association between poor oral health and eating disorders: systematic review and meta-analysis. Br J Psychiatry 2015; 207: 299–305.
Rytomaa I, Jarvinen V, Kanerva R, Heinonen O P . Bulimia and tooth erosion. Acta Odontol Scand 1998; 56: 36–40.
Hague A L . Eating disorders – screening in the dental office. J Am Dent Assoc 2010; 141: 675–678.
Fonteini P, Kamposiora P, Papavisiliou G . A multidisciplinary approach to the functional and esthetic rehabilitation of a patient with bulimia nervosa: A clinical report. Int J Dent Oral Sci 2015; 2: 53–58.
DeBate R D, Tedesco L A, Kerschbaum W E . Knowledge of oral and physical manifestations of anorexia and bulimia nervosa among dentists and dental hygienists. J Dent Educ 2005; 69: 346–354.
Mulic A, Tveit A B, Songe D, Sivertsen H, Skaare A B . Dental erosive wear and salivary flow rate in physically active young adults. BMC Oral Health 2012; 12: 10.1186/1472-6831-12-8.
Dynesen A W, Bardow A, Petersson B, Nielsen L R, Nauntofte B . Salivary changes and dental erosion in bulimia nervosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 696–707.
Touyz S W, Liew V P, Tseng P, Frisken K, Williams H, Beumont P J . Oral and dental complications in dieting disorders. Int J Eat Disord 1993; 14: 341–347.
Öhrn R, Enzell K, Angmar-Månsson B. Oral status of 81 subjects with eating disorders. Eur J Oral Sci 1999; 107: 157–163.
Oliva C L, Jornet P L, Alonso F C, Salinas J E . Study of oral changes in patients with eating disorders. Int J Dent Hyg 2008; 6: 119–122.
Johansson AK, Norring C, Unell L, Johansson A . Eating disorders and oral health: a matched case-control study. Eur J Oral Sci 2012; 120: 61–68.
Health NCC for M. Eating disorders: Core interventions in the treatment and management of eating disorders. NICE Guidelines 2009; 32: 809–819.
Zero D T, Lussi A . Erosion – Chemical and biological factors of importance to the dental practitioner. Int Dent J 2005; 55: 285–290.
Jarvinen V, II R, Heinonen O . Risk factors in dental erosion. J Dent Res 1991; 70: 942–947.
Banerjee A, Watson T . Pickard's Guide to Minimally Invasive Operative Dentistry. 10th ed. Oxford University Press, 2015.
Yan-Fang R . Dental erosion: Etiology, diagnosis and prevention. Regist Dent Hyg Publication date: April 2011.
Emodi-Perlman A, Tal Y, Rosenberg N, Eli I, Alter Z, Wincour E . Prevalence of psychologic, dental, and temporomandibular signs and symptoms among chronic eating disorders patients: A comparative control study. J Orofac Pain 2008; 22: 201–208.
Hermont A P, Pordeus I A, Paiva S M, Abreu M H N G, Auad S M . Eating disorder risk behaviour and dental implications among adolescents. Int J Eat Disord 2013; 46: 677–683.
Uhlen M M, Tveit A B, Stenhagen K R, Mulic A . Self-induced vomiting and dental erosiona clinical study. BMC Oral Health 2014; 14: 92.
Milosevic A, Brodie D A, Slade P D . Dental erosion, oral hygiene, and nutrition in eating disorders. Int J Eat Disord 1997; 21: 195–199.
Bartlett D W, Coward P Y . Comparison of the erosive potential of gastric juice and a carbonated drink in vitro. J Oral Rehabil 2001; 28: 1045–1047.
Barron R P . Dental erosion in gastroesophageal reflux disease. J Can Dent Assoc 2003; 69: 1–6.
Dawes C . What is the critical pH and why does a tooth dissolve in acid? J Can Dent Assoc 2003; 69: 722–724.
Lussi A, Jaeggi T, Jaeggi-Scharer S. Prediction of the erosive potential of some beverages. Caries Res 1995; 29: 349–354.
Al-Dlaigan, Y H ; Shaw L, Smith A . Dental erosion in a group of British Part II: Influence of dietary intake. Br Dent J 2001; 190: 258–261.
Gokul G . Eating disorders and its effect toward the oral cavity: A review. Asian J Pharm Clin Res 2016; 9: 40–42.
Jugale P V, Pramila M, Murthy A K, Rangath S . Oral manifestations of suspected eating disorders among women of 20–25 years in Bangalore City, India. J Heal Popul Nutr 2014; 32: 46–50.
Price C, Schmidt M A, Adam E J, Lacey H . Parotid gland enlargement in eating disorders: An insensitive sign? Eat Weight Disord 2008; 13: e79–e83.
Riad M, Barton J R, Wilson J A, Freeman C P, Maran A G . Parotid salivary secretory pattern in bulimia nervosa. Acta Otolaryngol 1991; 111: 392–395.
Abraham S F, Beumont P J . How patients describe bulimia or binge eating. Psychol Med 1982; 12: 625–635.
Lester I H, Ian H . Australia's Food & Nutrition. 1994.
Romanos G E, Javed F, Romanos E B, Williams R C . Oro-facial manifestations in patients with eating disorders. Appetite 2012; 59: 499–504.
Frydrych A M, Davies G R, McDermott B M . Eating disorders and oral health: a review of the literature. Aust Dent J 2005; 50: 6–15; quiz 56.
Harper D S, Osborn J C, Clayton R, Hefferren J . Modification of food cariogenicity in rats by mineral-rich concentrates from milk. J Dent Res 1987; 66: 42–45.
Silva M D, Burgess R C, Sandham H J, Jenkins G N . Effects of water-soluble components of cheese on experimental caries in humans. J Dent Res 1987; 66: 38–41.
Belli W A, Marquis R E . Adaptation of Streptococcus mutans and Enterococcus hirae to acid stress in continuous culture. Appl Environ Microbiol 1991; 57: 1134–1138.
Young W . The oral medicine of tooth wear. Aust Dent J 2001; 46: 236–250; quiz 306.
Ly K A, Milgrom P, Rothen M . The potential of dental-protective chewing gum in oral health interventions. J Am Dent Assoc 2008; 139: 553–563.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Rosten, A., Newton, T. The impact of bulimia nervosa on oral health: A review of the literature. Br Dent J 223, 533–539 (2017). https://doi.org/10.1038/sj.bdj.2017.837
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.837
This article is cited by
-
Acidic food choice among adolescents with bulimic symptomatology: a major risk factor for erosive tooth wear?
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2021)