Key Points
-
Describes the effect of denture loss in hospital on patients.
-
Highlights the extent of denture loss in hospital and the financial burden to NHS trusts.
-
Key recommendations are outlined that may help to reduce denture loss in hospitals.
Abstract
Background The loss of dentures for inpatients can have a detrimental effect on their well-being. Self-respect and dignity become compromised along with their ability to eat meals and communicate clearly, and long-term recovery.
Aim This investigation aimed to identify the reported number of dentures lost in hospitals and the financial reimbursements given by trusts to replace them.
Method Information on reported denture loss and reimbursement was collected in 12 trusts throughout Kent, Surrey and Sussex.
Results Eleven out of 12 trusts returned data about how many dentures were lost in their hospitals, between them 695 dentures were reported lost over five years (2011–16). Seven trusts reported financial reimbursements for dentures losses; results showed £357,672 was reimbursed over six years (2010–16), the highest amount reimbursed for a single denture was £2,200.
Conclusion The results indicate that denture loss is a problem in hospitals that contributes to the financial burden for the NHS. Consideration needs to be given by hospitals to find ways to reduce the number of dentures lost every year.
Similar content being viewed by others
Introduction
Losing a denture while in hospital can be exceptionally distressing to an individual, and can have a detrimental effect on their nutrition, ability to communicate and well-being. In most cases, patients will need to wait until they have been discharged from hospital before they can access a dentist to remake their dentures, this process can take up to several months if not longer. Furthermore, reimbursement for denture loss is a significant financial burden on the NHS.
Edentulism is declining in most industrialised countries,1 with the UK being part of this trend. The first Adult Dental Health Survey (ADHS) in 1968 showed that 37% of adults in England and Wales had no natural teeth, whereas the latest ADHS in 2009 showed the percentage had declined to just 6%.2
Studies have found that a small but varied group of people will continue to become edentulous, and that adults who are partially dentate will commonly choose to replace their missing teeth with partial dentures for the foreseeable future.3
Wearing dentures has a significant positive impact on an individual. A study in Sweden found patients perceived losing teeth and being provided with dentures as more important, in terms of adjustment, than events such as 'marriage' and 'retirement'.4 Missing teeth can have negative consequences on self-image, social interaction and psychological health.1 For an individual, the loss of their denture will therefore have a negative impact. Self-respect and dignity may become compromised along with function and the ability to eat and communicate. Many patients will have worn their dentures for many years and may not easily adapt to new replacements.5 Considering all these factors, for an inpatient losing a denture may impact on their overall recovery.
There is limited research available on the incidence, financial costs and impact on a patient when their denture is lost in hospital. An 8-month study carried out in Tower Hamlets Primary Care Trust (UK), showed that out of 26 people who reported to have lost their denture in this time, 21 had lost them in hospital.5 A different study of 430 elderly inpatients in hospital who required dental treatment between 1981 and 1987 found that 20.4% required new dentures and for a third of these patients the loss occurred in hospital. This study concluded that the high percentage of dentures lost in hospital was important, indicating a need for better supervision and care of dentures by nursing staff.6
Aim
The primary aim of this investigation was to identify the reported number of dentures lost in hospitals in Kent, Surrey and Sussex, and the financial reimbursements paid out by the Trusts concerned. The secondary aim was to determine whether or not there were clear pathways for hospital staff to follow in the event of denture loss.
Method
All 12 NHS hospital trusts in Kent, Surrey and Sussex took part in the data collection, as part of the acute branch of the Health Education England initiative 'Mouth Care Matters (MCM)'. This is a programme designed to improve the oral health of people in hospitals and care homes.7 Within the MCM initiative, each trust was required to recruit a mouth care lead for 12 months who was responsible for leading the implementation of the programme within their trust. Trusts were made aware that data would be collected, anonymised and shared in their agreement with Health Education England. Permission to conduct the study was granted by the post graduate dental dean. The research and development team at Surrey and Sussex Health Care Trust was consulted and they advised ethical approval was not necessary.
The MCM leads were asked to collect data on the number of dentures that had been reported lost by the trust from 2009–16, via Datix, a hospital incident reporting system.
The MCM leads were also asked to collect data on financial reimbursements paid to patients by their trust for replacements of lost dentures. This was achieved by liaising with the hospital financial department.
Finally, the leads were asked to investigate whether or not there was an established pathway in place that was to be followed in the event of a denture being lost, to enable it to be reported and remade if appropriate. Initial enquiries were made, asking a range of hospital staff what procedure they would follow should an inpatient denture loss occur or if there was a concern from a patient/relative that a denture had gone missing during a hospital admission.
Results
Number of dentures lost
Out of 12 trusts taking part in the evaluation, eight returned completed data, three returned incomplete data, and one did not return data (Table 1).
To enable comparison between 11 trusts, data were analysed between 2011–16, data from 2009–10 was excluded so that three more trusts could be included in the analysis. The total number of dentures reported lost over this 5-year period was 695.
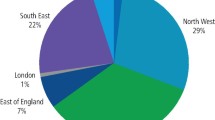
The number of dentures lost by the different trusts over the five period varied widely from the mean value of 63 (range from 20 to 218), with the number of dentures lost not being related to the number of hospital sites, number of beds or number of wards within the trust.
Financial reimbursement for denture losses
Out of 12 trusts taking part in the evaluation, six returned completed data, one returned incomplete data, and five did not return data on financial reimbursement for lost dentures (Table 2).
To enable complete recording from seven trusts, data were included from 2010–16. The total reimbursements over this 6-year period was £357,672. The mean total per trust was £51,096 (with a range from £9,842 to £164,533). Four trusts reported information that included individual reimbursements for dentures, with reimbursements regularly seen above £1,000 per denture. Of these the three highest amounts reimbursed were £2,200, £1,820 and £1,750.
Evaluation of pathways present in hospital for dentures lost
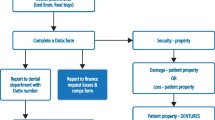
Of the 12 trusts taking part in the evaluation, 12 returned information regarding current pathways in their hospital. Five out of these 12 trusts reported having a known, established care pathway in place for when a denture was reported missing in hospital.
Of these five trusts a common theme emerged where the area around the patient's bed was checked and the denture confirmed as missing. If the denture was not located an incident report was completed, and the patient and relatives given information on how to claim for reimbursement of the denture. In four of these trusts the patient was expected to have their new dentures made by a GDP on discharge and one trust had an onsite dental department who would remake the denture if appropriate.
Discussion
The average of 63 dentures lost each year shows the problem of losing dentures to be a significant issue. The trust that made dentures onsite reported that although six dentures were reported lost in one year via Datix, the dental department had records of remaking 21 dentures that year due to loss within their hospital. It is therefore likely that denture loss is an unreported problem in hospitals due to a lack of awareness among hospital staff.
Losing a denture in hospital can have a profound effect on a person. They may struggle to eat without their denture, impacting on their nutritional status which consequently may keep them in hospital for longer. Many people feel the need for prosthodontic privacy8 and hide the fact that they wear dentures from their family and friends. One MCM lead reported that a patient had refused all visitors following her dentures being misplaced in hospital, she expressed that she felt miserable and could not bear to see her grandchildren without teeth as she felt her appearance would scare them.
Another MCM lead reported on a case where a patient fell asleep and woke up to find her dentures missing from the place she had left them. She had wrapped them in tissue to keep them safe, but they had been accidently mistaken for rubbish and disposed of by staff. The patient was undergoing palliative care and by the time new dentures could be remade the ward nurse advised it was likely she would have died. The patient cared about her appearance, she was still brushing her hair and applying lipstick every day but was very upset that her teeth had been lost and that she did not look like her normal self in her last days with her family and friends.
The construction of a new denture can take several weeks or months, more if the patient remains in hospital and there is no access to dental care. Once discharged if the patient is immobile or has severe medical problems they are likely to require hospital transport to appointments or domiciliary visits with increased associated costs. Many patients are discharged from acute hospital into community care where there may be dental access issues.9 If a new denture is remade the patient may struggle to adapt, following the use of their existing set for years.5 Sadly, it appears those who receive a replacement or compensation are more likely to do so if they have someone to speak on their behalf. One MCM trust lead reported that, in their trust, a review of 15 individual cases found that 13 claims had been made by the patient's family, one claim was submitted by a dentist and only one patient claimed themselves.
The results of how the dentures were lost via Datix, indicated the most common reasons to be when:
-
Wrapped in tissue and left on meal trays
-
Hidden in linen
-
Mistaken for rubbish and thrown away
-
Lost in transit between wards or theatre
-
Disposed of following an episode of vomiting when the denture was expelled at the same time.
Methods to reduce denture loss
This study has identified several ways in which to help reduce denture loss by hospital inpatients: They include:
1. Staff training
Hospital staff, including those in theatre, on wards and porters transporting patients, should have training to raise awareness of denture loss. Hostess and cleaning staff should also be trained to be vigilant for dentures when changing linen or removing meal trays to reduce the risk of them being accidently hidden and disposed of.
2. Dentures pots
Once it has been identified a patient wears dentures, labelled denture pots with lids should be supplied if the patient does not have one, this will help to keep the dentures in a known, identified place when they are not in the mouth.10 Patients should be asked to put their dentures in the denture pot and be made aware of the risk of loss if they do not keep them in a safe place.
3. Denture labelling
Denture labelling should be standard practice at the manufacture.11 One advantage of marking dentures is that if they are found, they can be returned to the wearer,5 otherwise there is little chance they will be returned. One MCM lead reported finding eight unidentified dentures – two of which were cobalt chrome dentures, in their Trust's linen room. Lost or mislaid dentures are also a common problem in care homes.12
4. Raising awareness among patient and family
Nursing staff should advise patients not to wrap dentures in tissues or linen while in hospital, and explain that there is a risk that if they do they may be mistaken for waste.
If patients are not regularly wearing their dentures, their family should be advised to take the dentures home to keep them safe.
Financial implications of denture loss
Although small within the scope of NHS expenditures, denture loss at an average of £51,096 over 6 years per trust is notable. Trusts should work to reduce these losses and create a more robust way to report and reimburse the dentures. There is a potential for the costs to be much higher if everyone who reported their dentures claimed the highest amount of £2,200. Changes could include an agreed maximum amount to be paid out for a lost denture, or a thorough investigation into why the denture was lost, to ensure it is in fact the trust's responsibility to financially reimburse. One MCM lead found that their trust took measures to ensure they kept costs to a minimum in such a situation. The loss was investigated, if the patient had special needs, was medically compromised, or the trust was obviously at fault, the denture was reimbursed at NHS band 3 prices. In cases where the patient may have been at fault, that is, they did not make use of their denture pot or the patient or relative 'could not recall events', the trust reimbursed 50% of the NHS band 3 price. This ensured each denture loss reimbursement was capped at a potential £233.70.
An ideal care pathway to ensure the management of a patient after they have suffered denture loss would aim to help that all patients have a fair chance to move efficiently towards a positive outcome. A possible care pathway for denture loss would require first confirming the patient had their denture in hospital to start with, by checking the notes to see if dentures were recorded on admission. The area surrounding the patient's bed should be checked as well as laundry and lost property. If not found the nurse in charge and ward manager should be informed and a Datix return completed. Staff should explain to patients and their relatives if appropriate how to claim for reimbursement. It should be determined how the patient will obtain a replacement – whether while in hospital, if possible, or from their own dentist. Finally, staff should review what impact this loss may have on the patient's care, such as a change in the consistency of their meals.
Conclusion
This investigation has identified that denture loss is an under-reported yet significant problem for patients while they are in hospital. By raising awareness through training and educating both patients and hospital staff through dentally-led initiatives like 'Mouth Care Matters' may help to reduce this problem.
References
Papadaki E, Anastassiadou V. Elderly complete denture wearers: a social approach to tooth loss. Gerodontology 2012; 29: 721–727.
Hellyer P. The older dental patient – who cares? Br Dent J 2011; 211: 109–11.
Steele J G, Treasure E, Pitts N B, Morris J, Bradnock G. Adult dental health survey: Total tooth loss in the United Kingdom in 1998 and implications for the future. Br Dent J 2000; 180: 598–603.
Bergendal B. The relative importance of tooth loss and denture wearing in Swedish adults. Community Dent Health 1989; 6: 103–111.
Michaeli L, Davis D M, Foxton R. Denture loss: an 8-month study in a community dental setting. Gerodontology 2007; 24: 117–120.
Awath-Behari, Harper. Retrospective study of dental treatment for elderly hospital inpatients in Wolverhampton. Community Dent Health 1991; 7: 437–42.
Mouth Care Matters. Online information available at http://www.mouthcarematters.hee.nhs.uk/ (accessed April 2017).
Fiske J, Davis D M, Frances C, Gelbier S. The emotional effect of tooth loss in edentulous people. Br Dent J 1998; 184: 90–93.
Fox C. Evidence summary: why is access to dental care for frail elderly people worse than for other groups? Br Dent J 2010; 208: 119–122.
M J. Faigenblum. The denture box. An aid to denture hygiene. Br Dent J 2014; 218: 9–12.
A. Kalyan R K. F. Clark D R. Radford. Denture identification marking should be standard practice. Br Dent J 2014; 216: 615–617.
Welsh S. Caring for smiles: improving the oral health of residents. Dent Nurs 2014; 10: 224–228.
Acknowledgements
The authors would like to thank the 'Mouth Care Matters' leads who collected the data for this investigation
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Health Education England is funding the training initiative called Mouth Care Matters across Hospitals in Kent, Surrey and Sussex.
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Mann, J., Doshi, M. An investigation into denture loss in hospitals in Kent, Surrey and Sussex. Br Dent J 223, 435–438 (2017). https://doi.org/10.1038/sj.bdj.2017.728
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.728
This article is cited by
-
The prevalence of denture loss within community residential settings
British Dental Journal (2024)
-
Prevention of oral diseases for the older person (Part 2)
British Dental Journal (2024)
-
Denture loss: incidence and impact within an acute hospital setting
British Dental Journal (2022)
-
The impact of a quality improvement initiative to reduce denture loss in an acute hospital
British Dental Journal (2022)
-
Dental care pathways for adult inpatients in an acute hospital: a five-year service evaluation
British Dental Journal (2020)