Key Points
-
Provides new evidence of the impact of medication.
-
This evidence could have practical application in risk assessment.
-
Offers an increased insight into the biological action of the medication involved.
Abstract
Bony disease is typically evident with radiographic examination. Loss of bone mass consistent with osteoporosis is evident on plain dental radiographs, and it is reasonable to expect that anti-resorptive treatment of osteoporosis would lead to changes in radiodensity of structures visible on dental radiographs. Review of a number of radiographs of patients receiving anti-resorptive (bisphosphonate) treatment appears to confirm increased radiodensity of the structures, which may have implications in risk assessment of complications following dental procedures.
Similar content being viewed by others
Introduction
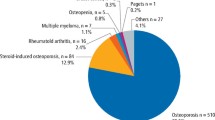
Bisphosphonate and other anti-resorptives have been increasingly widely used within medicine for the last 20 years or so. Their indications have been widely published, and include osteoporosis, Paget's disease, hyperparathyroidism, metastatic malignancy, hypercalcaemia of malignancy, and multiple myeloma.1 Probably the largest group being treated at any time are those patients requiring management of moderate to advanced osteoporosis. In 2012, 7.2 million FP10 prescriptions were issued for Alendronate alone in England2.
Anti-resorptives may have significant impacts upon the oral environment, not least the induction of a chemo-necrosis of the jaws – bisphosphonate related osteo-necrosis of the jaw (BRONJ), or medicine related osteo-necrosis of the jaw (MRONJ), depending upon the agents involved. However, these agents have other impacts in the oral environment, and some become evident radiographically over time. Appreciation of these changes may help the practitioner plan treatment, and understand complexities and risks more clearly before commencing interventions.
Background
Osteoporosis and bisphosphonates
Osteoporosis is a condition where reduced bone mass and structural degradation of the bone itself leads to overall fragility of the skeleton. This may present with low force fracture of long bones (eg proximal femur), and vertebral collapse. According to the British Orthopaedic Association, osteoporosis accounts for at least 300,000 patients attending UK hospitals with fractures annually.3 The prevalence of osteoporosis is linked with post-menopausal changes in women, and age in both sexes, and increases sharply with time.
Conventional approaches to diagnosis of osteoporosis have been opportunistic, however guidance from National Institute for Health and Care Excellence (NICE)4 now suggests targeted risk assessment of all women over 65 years of age, and all men over 75 years (assumed levels of bony change being based upon age), with assessment of younger patients only if other risk factors exist (such as previous fragility fracture, a family history of fracture, or steroid use). Incidental chance diagnoses of osteopenia may occur, leading to increased surveillance. Risk assessment is focused on the prevention of fractures, and for those within the risk groups the WHO Fracture Risk Assessment Tool (FRAX)5 may be used to assess the risk of fracture.
Formal screening of bone density is undertaken using a dual energy X-ray absorptiometry (DXA) system. The DXA system may be used on any bone, and although it is typically used for assessment of bone density at the neck of femur, and lumbar/sacral spine, as these are high risk sites for symptom initiation, it could also be used on the mandible. The OSTEODENT project demonstrated the viability of osteoporosis diagnosis using dental radiographs in 2007,6,7 and others have confirmed the feasibility of the use of dental radiographs in assessing osteoporosis.8
A DXA assessment produces a scoring of reduction in bone mass (the 'T' score – a comparison against normal bone mineral density at age 30 – with T score of -2.5 standard deviations or more being necessary for a diagnosis of osteoporosis), and may be used in combination with FRAX assessment of to produce a longer (ten year), more accurate, risk analysis for fracture, that forms the basic indication for the prescribing of bisphosphonates to prevent fragility fractures. Alendronate is presently the first line agent for treatment.9
A number of anti-resorptives presently exist, with the largest group being the bisphosphonates, and the second main group the RANK-L inhibitors. While these operate by significantly differing mechanisms, the overall aim and end-result is the same – to inhibit loss of bone volume, and enhance bone deposition. The progress of treatment with these agents may be tracked by use of radiological screening approaches, and indeed is reviewed with repeat DXA assessments. Information provided by these assessments can indicate a change in protocols of treatment, and a number of patients who are poor responders to oral bisphosphonates are treated with (low dosage) intravenous regimens, or alternative anti-resorptives.
However while computer assisted assessments of radiographs are available,6,10,11 radiographic changes are evident to the naked eye, including both intra-oral and extra-oral dental radiographs, in cases where patients present with osteoporosis, or are treated and show bisphosphonate treatment osteosclerosis. These changes can be identified in the routine examination of dental radiographs, and may assist the practitioner in planning some treatments, and facilitate a more valid patient consent.
Evident radiographic changes
Osteoporosis
In cases of clear osteoporosis, routine examination of radiographs will reveal a number of morphological changes to the gross structure on the bone of the mandible and maxilla, although this is clearest in the mandible. These changes form aspects of the OSTEODENT project identifiers, and may be clearly seen. However there are variations, and a good understanding of the normal is essential.
By definition, in osteoporosis there is a loss of bone mass, and this is evident in both cortical and trabecular bone. While this is visible on intra-oral films (which are used by the ImaTx system11), it is probably easiest seen on dental panoramic films. Figure 1 is the panoramic film of a patient recently diagnosed with untreated osteoporosis. There is a generalised decrease in the number and bulk of trabeculae in the cancellous bone, with reduction in the general radiodensity of the mandible (note – there is a degree of rotation, and the Hyoid bone is superimposed).
Panoramic radiograph of recently diagnosed osteoporotic patient prior to bisphosphonate treatment demonstrating radiographic changes consistent with reduced bone mass, including thinning of inferior border and scalloping of upper surface of cortex, reduction in number of trabeculae and loss of definition of inferior dental canal
As loss of bone mass occurs in cortical as well as cancellous bone, it would be expected that structures outlined by cortical bone would become less well defined, as it is their relative radiodensity that allows naked eye interpretation and identification of the relevant radioanatomy. This can be seen in Figure 1 with the definitive structures being vague, a loss of clarity of the inferior dental canal bilaterally, with thinning of the inferior border of the mandible, and scalloping of the upper margin of the inferior border. Horner et al.12 noted these changes of the inferior border in patients with osteoporosis, and categorised the cortical margin into three forms: Cortical Margin Indicators (CMI) 1-3. The CMI was considered to be a reliable diagnostic indicator of osteoporosis. In Figure 1, there is also marked cortical thinning at the mandibular angles, and reduced clarity of the lamina dura around many teeth. In some cases there is also a reduction in the cortical thickness at the head of the condyle, although this probably bears no relationship to condylar head remodelling seen in cases of tempromandibular joint pathology.
Bisphosphonate therapy
It would be expected that following treatment with a bisphosphonate or other anti-resorptive, the opposite effects should be evident. Treatment progress monitoring with DXA would be expected to show progressive accumulation of bone mass, in cortical as well as cancellous bone. This can be demonstrated with dental radiographs, using a digital subtraction technique.10 In studies by Phal et al.13 and Hutchinson et al.14 looking at imaging of patients with BRONJ, a range of radiographic findings become evident in patients with diagnosed BRONJ, and while these studies used both plain film and computerised tomography (CT) examinations, retrospective review of a series of plain film radiographs for this pilot (27 patients; 25F, 2M, age range 55–90, average age 73.3 years), attending for outpatient consultation, treated with bisphosphonates but without BRONJ show a range of similar radiographic changes. These changes are most evident to the naked eye in cortical bone, appear to occur consistently, and before the inception of BRONJ. These changes are detailed in Table 1.
Examination of radiographs may reveal many, although not necessarily all, of these features, and are demonstrated in Figures 2, 3, 4, 5. Several aspects are striking, and are consistent with expectations from treatment with anti-resorptives. Possibly the most obvious is the increased density and depth of the inferior border of the mandible, with loss of the porosity expected in cases of osteoporosis. This would be expected, given the action of anti-resorptives, but is marked in many cases, with a pronounced increased depth of the cortical bone. While this change has not been observed on serial radiographs, changes in the inferior border are a proven radiographic sign of osteoporosis, and as such it is reasonable to infer that increased depth of the inferior border is indeed a sign of the impact of anti-resorptive treatment.
Patient (a) has no history of bisphosphonate treatment, patient (b) treated with alendronate for more than five years. Note the increased density of trabeculae with treatment, reduction in marrow spaces, and pronounced thickening of lamina dura as a result of bone deposition, when compared to normal bony architecture
Other sites that clearly show morphological changes are the lamina dura, and the interdental bone. Here the structures increase in both density and width, in some cases the lamina dura may appear three times thicker than normal. Again, such changes would be anticipated from the action of anti-resorptives.
Discussion
The use of bisphosphonates is now widespread, and their effects long lasting. Their impact on the oral structures is significant, and while the clinical complication of BRONJ is the most obvious expression of this, bisphosphonates may affect endothelial, epithelial, fibroblast, and myogenous cell differentiation, proliferation and migration.15,16,17 In bone, their action favours deposition of bone, thus increasing net bone mass, in addition to other actions such as promoting tumour cell apoptosis, and impaired adhesion of tumour cells.18
Interpretation of radiographs is typically considered as a process of differentiating the normal from the pathological. However the interpretation process is much more complex, and starts with an appreciation of the way that the eye 'sees' the image, and how the information is processed for interpretation by the brain. When reading a radiograph, the eye is seeing changes in relative radiodensity representing the structures, and is effectively reading the edges between these variations. Consequently the patterns produced at these areas form the recognisable image. With increased deposition of bone, two changes occur: an increase in the bulk of the structure itself as a result of an increase in bone mass, and an increase in visibility of structures on radiographs as the greater mass absorbs more X-ray photons, leading to an increase in observed radiodensity.
Clinically these changes may be relevant; for example, as bone density of the lamina dura increases, and the width of the lamina dura increases, then the potential difficulty of extraction also increases, as the socket becomes less flexible. Increased bony density may also suggest reduced perfusion of the bone by blood, and thus a degree of bony ischaemia, which may predispose to poor healing or BRONJ. The rigidity of the sockets and density of the lamina dura might well explain the clinical observation of frequent sequestration of small fragments of bone following extractions for patients taking bisphosphonates. Low grade inflammatory changes, for example related to a chronic periapical lesion, may show pronounced associated sclerosis, and likewise chronic periodontal inflammation may also prompt increased density of the lamina dura, and surrounding bone, evident radiographically, possibly as a result of inflammatory changes leading to localised increases in bisphosphonate concentration following release of entombed bisphosphonate by inflammatory mediated bone resorption associated with periodontal disease. Low grade inflammatory changes are often accompanied by increased bone deposition and this would be accentuated by bisphosphonates. It is possible that this may provide an indicator of a greater risk of problems with healing, and in the presence of excellent oral hygiene – and thus by inference no gingival inflammation – the risk of BRONJ is reduced.19 The key question is – will it be possible to predict from radiographs a relative risk of induction of BRONJ?
Torres et al.20 examined panoramic radiographs of patients with and without BRONJ. They identified mandibular inferior border changes in both groups, with a statistically greater depth of inferior border evident in those with BRONJ, and suggested that the depth of the inferior mandibular border might provide an indicator of bisphosphonate treatment, and eventually perhaps a predictor of those patients at greater risk of BRONJ. Takaishi et al.21 used bone mass density assessment from dental radiographs looking specifically at the areas surrounding extraction sites and suggested that the sharp increase in bone density measured was a potential risk indicator –although they were not really able to definitively establish if this was a pre-existing finding before extractions, or a response of tissues to inflammatory changes present with BRONJ, as these changes are typically observed retrospectively once BRONJ is identified.
Type 1 collagen carboxy-terminal telopeptide (CTX) assay has been suggested as a method to predict risks for BRONJ.22 CTX is a degradation product of collagen that may be used to measure bone resorption, effectively an indicator of osteoclast activity, and thus potentially the impact of bisphosphonates on remodelling and healing following extractions. A comparison of radiographic changes against CTX assay suggested that radiographic evidence of periodontal changes, particularly widening of the periodontal ligament, may be more reliable than CTX assay in predicting BRONJ,23 but this is still an inexact assessment. Certainly studies tend to show that poor oral health and periodontal disease is associated with BRONJ.20,24
However, it should be noted that it is observation of the biological behaviour in the tissues that is important in understanding the development and progress of the condition, and this may inform discussions with patients during consent to procedures such as extraction. Prediction of risks of osteonecrosis induced by an anti-resorptive is likely to remain an imprecise process –possibly due to the number of variables, but the reviewing of radiographs to assess the extent of radiographic evidence (and thus effectiveness) of antiresorptive therapy, as well as other aspects of care, may prove useful in understanding the biological behaviour of the tissues.
Conclusion
Anti-resorptives lead to increased deposition of bone, and this should be evident radiographically – indeed one assessment of the effectiveness of treatment for osteoporosis is repeated DXA scans. These changes are also evident when viewing dental radiographs, particularly at the inferior border of the mandible, and lamina dura, but may be evident in any bony structure imaged. An appreciation of these changes will help inform understanding of the underlying progress of the biology of the tissues, and may inform discussions with patients.
References
Ruggiero S L, Dodson T B, Fantasia J et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw - 2014 update. J Oral Maxillofac Surg 2015; 72: 1938 956.
Health and Social Care Information Centre. Prescriptions Dispensed in the Community: England 2002–12. 30 July 2013. Available at: https://catalogue.ic.nhs.uk/publications/prescribing/primary/pres-disp-com-eng-2002-12/pres-disp-com-eng-2002-12-rep.pdf (accessed March 2016).
British Orthopaedic Association. The care of patients with fragility fracture. London: British Orthopaedic Association, 2007.
Osteoporosis: assessing the risk of fragility fracture. NICE guidelines [CG146]. August 2012. Available at: https://www.nice.org.uk/guidance/cg146/chapter/1-Guidance#ftn.footnote_8 (accessed 3 September 2015).
FRAX –The WHO Fracture risk assessment tool. Available at: http://www.shef.ac.uk/FRAX/ (accessed 3 September 2015).
Devlin H, Karayianni K, Mitsea A et al. Diagnosing osteoporosis by using dental panoramic radiographs: The OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 821–828.
Karayianni K, Horner K, Mitsea A et al. Accuracy in osteoporosis diagnosis of a combination of mandibular cortical width measurement on dental panoramic radiographs and a clinical risk index (OSIRIS): the OSTEODENT project. Bone 2007; 40: 223–229.
Calciolari E, Donos N, Park J C, Petrie A, Mardas N . Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res 2015; 94 (3 Suppl): 17S–27S.
Alendronate, etidronate, risedronate, raloxifene, strontium ranelate and teriparatide for the secondary prevention of osteoporotic fragility fractures in postmenopausal women (amended). NICE, October 2008. Available at: https://www.nice.org.uk/guidance/ta161/chapter/1-guidance (accessed 27 July 2015).
Zaman M U, Nakamoto T, Tanimoto K . A retrospective study of digital subtraction technique to detect sclerotic changes in alveolar bone on intraoral radiographs of bisphosphonate-treated patients. Dentomaxillofac Radiol 2013; 42: 20130242. 10.1259/dmfr.20130242. Epub 2013 Oct 29.
Liew S, Steines S, Jeffcoat M et al. Dental X-rays Identify women with low hip and spine BMD. Imaging Therapeutics Inc., 2005.
Horner K, Karayianni K, Mitsea A et al. The mandibular cortex on radiographs as a tool for osteoporosis risk assessment: the OSTEODENT project. J Clin Densitom 2007; 10: 138–146.
Phal P, Myall R W T, Assael L A, Weissman J L . Imaging findings of bisphosphonate associated osteonecrosis of the jaws. AJNR Am J Neuroradiol 2007; 28: 1139–1145.
Hutchinson M, O'Ryan F, Chavez V et al. Radiographic Findings in Bisphosphonate-Treated Patients With Stage 0 Disease in the Absence of Bone Exposure. J Oral Maxillofac Surg 2010; 68: 2232–2240.
Donetti E, Gualerzi A, Sardella A, Lodi G, Carrassi A, Sforza C . Alendronate impairs epithelial adhesion, differentiation and proliferation in human oral mucosa. Oral Dis 2014; 20: 466–472.
Ravosa M J, Ning J, Liu Y, Stack M S . Bisphosphonate effects on the behaviour of oral epithelial cells and oral fibroblasts. Arch Oral Biol 2011; 56: 491–498.
Shiomi K, Nagata Y, Kiyono T, Harada A, Hashimoto N . Differential impact of the bisphosphonate alendronate on undifferentiated and terminally differentiated human myogenic cells. J Pharm Pharmacol 2014; 66: 418–427.
Santini D, Virzi V, Fratto M E et al. Can we consider zoledronic acid a new antitumor agent? Recent evidence in clinical setting. Curr Cancer Drug Targets 2010; 10: 46–54.
Polymeri A A, Kodovazenitis G J, Polymeris A D, Komboli M . Bisphosphonates: clinical applications and adverse events in dentistry. Oral Health Prev Dent 2015; 13: 289–299.
Torres S R, Chen C S K, Leroux B G et al. Mandibular inferior cortical bone thickness on panoramic radiographs in patients using bisphosphonates. Oral Surg Oral Med Oral Pathol Oral Radiol 2015; 119: 584–592.
Takaishi Y, Ikeo T, Nakajima M, Miki T, Fujita T . A pilot case-control study on the alveolar bone density measurement in risk assessment for bisphosphonate-related osteonecrosis of the jaw. Osteoporos Int 2010; 21: 815–825.
Marx R, Cillo J, Ulloa J . Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg 2007; 65: 2397–2410.
Fleisher K E, Welch G, Kottal S, Craig R G, Saxena D, Glickman R S . Predicting risk for bisphosphonate-related osteonecrosis of the jaws: CTX versus radiographic markers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 509–516.
Kos M . Association of dental and periodontal status with bisphosphonate-related osteonecrosis of the jaws. A retrospective case controlled study. Arch Med Sci 2014; 10: 117–123.
Acknowledgements
My thanks to Professor Keith Horner for his comments on this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Thayer, M. Radiographic evidence of treatment with bisphosphonates. Br Dent J 222, 507–510 (2017). https://doi.org/10.1038/sj.bdj.2017.307
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.307