Key Points
-
Educates the reader about recent political debates concerning the placement of implants in periodontally compromised patients.
-
Highlights the aetiology, risk factors and prevention of peri-implantitis.
-
Highlights the importance of periodontal stabilisation prior to implant placement to prevent peri-implantitis.
-
Highlights the need for regular periodontal maintenance therapy following the placement of implants in periodontally compromised patients.
Abstract
Dental implants are seen as a good option for replacing missing teeth. The success and survival rates for implants are very high. Concerns are developing about the problem of peri-implantitis. The reports of its prevalence vary but it is noted that the presence of periodontal disease is a risk factor. The issue of peri-implantitis was raised in the House of Lords in 2014. Complaints relating to implants is on the rise with the General Dental Council. Placement of implants in patients with periodontal disease is not a treatment that should be done without a full periodontal assessment and stabilisation of periodontal disease first. This review considers the risk of placing implants in patients with aggressive and chronic periodontitis.
Similar content being viewed by others
Introduction
Dental implants are ever increasing in popularity and are now considered one of the standard treatment options for patients who require the replacement of missing teeth. The most recent UK adult dental health survey reported that half a million adults in the United Kingdom have at least one dental implant.1 Unfortunately, and somewhat unsurprisingly, the rise in popularity of dental implants has corresponded with a rise in General Dental Council (GDC) complaints concerning implants.2 As a result of patient complaints, a publication provided by a UK indemnity provider reported that the two types of claims which now predominate relate to either dental implants or periodontal disease.3 Periodontal disease accounted for 44.7% of claims by value and dental implants accounted for 28.8% of claims by value, with implant complications as a result of periodontal disease accounting for 5.5% of claims by value.3 Complaints are predominantly related to lack of informed consent, implant failure and damage to vital structures. Regarding informed consent for implants, recent Royal College of Surgeons (RCS) guidelines state that patients need to be aware that implant-based restorations require long-term maintenance and can suffer from significant morbidities such as peri-implantitis which can effect prognosis and longevity.4 The importance of informing patients of the growing risks associated with dental implants, such as peri-implant disease, is fundamental before considering implant treatment; so much so that it was debated in the House of Lords. On 23 July 2014 Baroness Gardner of Parkes, a Conservative backbencher and retired dentist, stated that:
'Peri-implantitis is an important and growing health problem and there needs to be an awareness and a degree of understanding of the present position and the growing risks associated with this increasingly popular form of dental treatment [...] It must also be made clear that an implant is not a treatment you just have and forget. Regular follow-up visits are required to ensure that a periodontal condition does not develop [...] The RCS points out that long-term assessment and maintenance need to be assured [...] It (RCS) believes that the GDC should introduce minimum standards of education and training for complex dental treatment, such as implants [...] The GDC should include peri-implant assessment and maintenance in the undergraduate curriculum.'5
Following this parliament debate, the Faculty of General Dental Practice UK [FGDP(UK)]issued a report stating that it is essential for patients to receive appropriate periodontal checks following dental implant surgery and that all general dental practitioners (GDPs) have a duty of care to carry out an assessment of the health of the peri-implant tissue and recognise peri-implantitis.6
Periodontal disease is a major cause of tooth loss, however, it is also a major risk factor for peri-implantitis.7 In the UK approximately 45% of the population has periodontitis, with 8% of periodontally affected patients displaying severe attachment loss (>6 mm pocketing).1 This leaves clinicians in a difficult position when considering implants as a tooth replacement option for periodontally compromised patients. This article discusses the considerations of dental implants for patients with periodontal disease.
Tooth loss
Although tooth loss has reduced in the UK over the last three decades it remains a common problem for patients and dentists alike.1 The 2009 UK adult dental health survey revealed that 60% of adults had missing teeth. Periodontitis is the second most common reason for tooth extraction (following caries), with around 35% of tooth extractions occurring as a result of periodontitis.8,9
Periodontal disease
Up to 40-80% of the population may be susceptible to moderate periodontal disease, with the prevalence of severe chronic periodontitis (CP) being around 10% and aggressive periodontitis (AgP) up to 4%.10 The global figure for severe periodontitis is 11.2% (Kassebaum et al.), making severe periodontitis the sixth most prevalent global disease.11
CP is the most common form and is characterised by its slow rate of progression with short periods of rapid progression. Currently only four species have been identified as true periodontal pathogens; Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, Tanerella forsythia and Treponema denticola.12 Furthermore, several additional bacterial species (known as a climax community) provide nutritional interdependencies for periodontal pathogens and are therefore often related to the progression of periodontal disease (Table 1).12
AgP is a rare form of periodontitis which is characterised by rapid attachment loss and bone destruction, familial aggregation and presentation in persons under 30 years of age.10 It is typically associated with the pathogens A. actinomycetemcomitans and P. gingivalis.12
Implants success and survival
Over the last 25 years the placement of dental implants has dramatically increased in popularity, with an increased number of clinical situations whereby implants are being used.15 In the UK approximately 1% of dentate adults have at least one dental implant.1
Success and survival rates for dental implants are frequently reported as very high, with meta-analyses describing success rates of 96.7% to 97.5% for single-unit implant retained restorations and 92.5% to 93.6% for implant retained fixed partial dentures over six to seven years.16 However, recent literature suggests that one in twenty implants is lost over a period of ten years.17 Many operative factors affect the success of implants, however, it is not the purpose of this article to fully describe the difference between these operative techniques and further reading is available elsewhere.18
Complications which can affect implant success fall broadly into two categories; biological and technical complications. Technical complications, which are the most common, include loosening/fracture of the abutment screw, failure of the implant retained prosthesis and fracture of the implant fixture itself.19 Biological complications relate to inflammation and potential destruction of the peri-implant tissues.19 Peri-implant inflammation can occur as a result of improper site selection (for example, no keratinised mucosa),18 peri-mucositis as a result of plaque retention, residual cement, bacterial micro-leakage and smoking,20 and host-related disease such as peri-implantitis.
Peri-implantitis is a complication with slow progression and therefore an implant may be considered to have a long survival rate even though it is undergoing a disease process which ultimately affects function, aesthetics and long-term prognosis. Implant loss as a result of peri-implantitis has been reported to range from 0 to 13.6% at the patient level and from 0 to 8.3% at the implant level.21
Peri-implantitis
Peri-implantitis is an infectious disease which causes an inflammatory lesion that resides in peri-implant mucosa and affects the supporting bone.7 A recent systematic review with meta-analysis reported the prevalence of peri-implantitis to be 21.7%, with the authors stating that this figure may be an underestimation.21
It is widely accepted that around 1.5 mm of non-pathological crestal bone loss can be expected during the first year of implant function, with a subsequent annual bone loss of less than 0.2 mm regarded as normal.22,23 Any bone loss greater than this is regarded as pathological and peri-implantitis should be suspected. Peri-implant bone loss is characterised by a crater-like defect surrounding the circumference of the implant as well as increased probing depths. Bleeding on probing and/or suppuration may also be present. The criteria suggested for diagnosing peri-implantitis differs between authors. One definition suggests healthy peri-implant tissues allow 3 mm probe penetration and therefore a reading of 4 mm or more may indicate peri-implantitis.22,24 Alternatively, one systematic review proposed 2.5 mm or more bone loss, probing depth >6 mm and the presence of bleeding on probing or suppuration as diagnostic criteria for peri-implantitis.25 A more recent consensus report suggested changes in the level of crestal bone, presence of bleeding on probing and/or suppuration; with or without concomitant deepening of peri-implant pockets should be used to define a case of peri-implantitis.23 These inconsistencies have complicated the interpretation of prevalence, survival and success data for the diagnosis and treatment of peri-implantitis.
For implants affected by peri-implantitis, osseointegration remains apical to the peri-implant bone loss. As a result, the disease can progress without any notable signs of mobility. Furthermore, peri-implantitis is often asymptomatic and therefore patients can be unaware of the disease process. Consequently, without appropriate maintenance and monitoring appointments, patients can experience significant bone loss before presenting to a dentist.
As with periodontitis, peri-implantitis occurs as a result of bacterial colonisation of the peri-implant tissues which in turn causes an unfavourable host immune response and tissue destruction. Human cross-sectional studies have shown that peri-implantitis and periodontitis are associated with similar bacterial species (mainly gram negative anaerobes)14 (Table 1). Peri-implantitis and periodontitis have similar histopathology, with the peri-implant connective tissue becoming infiltrated with similar inflammatory cells and inflammatory biomarkers as seen in periodontitis.26,27
Progression rates of peri-implantitis and periodontitis differ, with peri-implantitis causing more rapid tissue destruction. It is thought that the absence of inserting collagen fibres into the implant (as opposed to a natural tooth in periodontitis) may be the reason for increased susceptibility to bone loss.28 Furthermore, tissues around natural teeth possess a 'self-limiting' process whereby supracrestal gingival fibres separate the inflammatory lesion from alveolar bone, whereas in peri-implant tissues the inflammatory lesion extends to the bone.29
Risk factors for periodontitis and peri-implantitis
Somewhat unsurprisingly peri-implantitis and periodontal disease share similar risk factors (Table 2). Patients who have a history of periodontal disease have been shown to be at higher risk of developing peri-implantitis.7 Patients with a history of CP are four times more likely to develop peri-implant disease than patients with healthy periodontal tissues.28 Patients with AgP have been shown to have a 14 times greater risk of peri-implantitis than periodontally healthy patients.31
A large body of evidence shows that smoking is a major risk factor for periodontal disease and subsequent tooth loss, with smokers having an odds ratio of 2.1–2.4 for periodontal disease and of 7.0 for severe periodontal disease.32 Similarly, there is an increased risk of peri-implantitis in smokers, with an odds ratio for peri-implantitis in smokers of 2.1–2.6.33,34
Numerous studies have shown a higher prevalence of periodontal disease in type I and type II diabetics.35 Diabetes has been cited as a risk factor for peri-implantitis, and although there is a plausible biological mechanism, evidence is limited due to a small number of studies investigating this relationship.
Implants in patients with a history of periodontitis
Six systematic reviews have investigated the outcomes of dental implants placed in partially dentate patients with a history of periodontitis.38,39,40,41,42 Schou et al.38 investigated the outcome of implant therapy in patients with periodontitis at five and ten years. Periodontitis patients had a significantly higher rate of peri-implantitis at ten years and significantly increased peri-implant bone loss after five years compared to periodontally healthy patients. Ong et al.39 reported that implant survival was lower for treated periodontitis patients than periodontally healthy patients. These results related particularly to patients with CP, however, the authors stated the results may also apply to patients with a history of AgP. Safi et al.40 reported that periodontitis subjects underwent more marginal bone loss in comparison with periodontally healthy subjects. The meta-analysis showed the odds ratio for implant survival was significantly in favour of periodontally healthy patients. Chrcanovic et al.41 reported that implant failure rates for periodontally healthy, CP and AgP patients were 3.84%, 5.37% and 4.71% respectively and suggested that an increased susceptibility for periodontitis led to an increased susceptibility for implant loss, loss of supporting bone, and postoperative infection. Sgolastra et al.42 revealed that a significantly higher risk for implant loss was present in patients affected by periodontal disease. Furthermore, periodontitis patients had significantly increased risk of peri-implantitis. Most recently, Sousa et al.43 bone loss and incidence of peri-implantitis was increased in patients with history of periodontitis and there was a higher tendency for implant loss in patients previously with severe forms of periodontitis. It is evident from this strong body of research that partially dentate patients with a history of periodontal disease are at a higher risk of the development of peri-implantitis and implant loss.
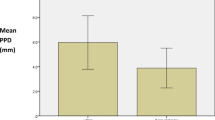
One theory explaining the increased risk of peri-implantitis in partially dentate periodontitis patients is the transmission of periodontal pathogens from the residual dentition to the peri-implant tissues.44 In patients treated for periodontal disease, periodontal pathogens found around natural teeth can be detected around the implant surface at one month, and at three years periodontal bacteria around implants are found as frequently as around natural teeth.45 Therefore, natural teeth serve as a reservoir of bacteria for colonisation of peri-implant tissues. Residual periodontal pockets have been shown to be a risk factor for peri-implantitis.44,45 In patients with a history of periodontitis, patients with residual periodontal pockets (>6 mm) around their natural teeth have shown to have significantly more implants with pocket depths of >5 mm, bleeding on probing and radiographic bone loss than periodontal patients with no residual pocketing.46 Furthermore, treated periodontal patients with evidence of peri-implantitis have been shown to have a higher number of residual periodontal pockets (>5 mm) around their natural teeth, whereas treated periodontal patients without peri-implantitis have fewer residual periodontal pockets.45 These studies suggest that periodontally compromised patients without residual periodontal pockets (>6 mm) have improved implant outcomes compared to periodontally compromised patients with residual periodontal pockets. However, evidence from several systematic reviews indicate that periodontal susceptibility (for example, host response) is as likely as residual pocket depth to be the determinant of peri-implant disease. Therefore, even if periodontal disease is well-controlled, implants placed in patients with a history of CP or AgP should be closely monitored.39,42,43
Implants in patients with chronic periodontitis
The majority of evidence regarding implant outcomes in periodontal patients relates to CP. The incidence of peri-implantitis in partially dentate CP patients has been reported to range from 3.1% to 66.7% over a five to ten years period.43 A ten-year prospective cohort study has reported the success and survival rates of implants in patients with CP as 52.4% and 90.5% respectively, as compared to periodontally healthy patients with success and survival rates of 79.1% and 96.5% respectively.47 A long-term cohort study has reported that the severity of CP affects implant failure over time, with failures among severe CP patients reported as higher than moderate CP patients (5.2% and 3.3% respectively).48 Similarly, a ten year prospective cohort study reported implant survival rate as 96.6% in periodontally healthy patients, 92.8% in moderate CP patients and 90% in severe CP patients.49 Interestingly, this study showed that periodontally compromised patients who adhered to supportive periodontal therapy had less implant failure than those who did not follow a maintenance program.49 Successful elimination residual periodontal pockets before implant placement is likely to improve implant success rates.46 When CP patients are enrolled in a thorough maintenance programme, the survival rate of implants has been reported to be as high as 94.7% after ten years.50
Implants in patients with aggressive periodontitis
Relatively fewer studies have been conducted concerning partially dentate AgP patients. The incidence of peri-implantitis in AgP patients has been reported as 26% over a period of 3–16 years, as compared to 10% in periodontally healthy individuals.50 Implant survival in generalised AgP patients has been reported as 88% to 96% at eight to ten years respectively and success as 33%-83% at eight to ten years respectively.51,52 In comparison, implant survival in periodontally healthy patients has been reported as 100% at ten years and success as 50–100% at eight to ten years respectively.51,52 Furthermore, generalised AgP patients have been reported to have a five times greater risk of implant failure and a 14 times greater risk of peri-implantitis.51 Expectedly, smokers with generalised AgP have been shown to have a significantly reduced implant survival rate (63%) than patients with generalised AgP who stopped smoking (78%).53 The importance of periodontal diagnosis before implant treatment was highlighted by Mengel et al.,54 who established that implant success rates in patients with generalised AgP patients are around 10% less than patients with CP.
Discussion
Implant survival, the presence of the implant in a patient's mouth, has been used as a primary outcome measure for the assessment of the prognosis and longevity of implant treatment as it provides data on the predictability of osseointegration within different patients.55 Studies present high implant survival rates,16 however, survival does not take into account the presence or absence of disease such as peri-implantitis. Implant success rates however, are based on clinical parameters related to the implant and peri-implant tissues, such as bone levels and probing depths. Unfortunately, there is a lack of consensus regarding the definition of success, therefore the validity and comparability of implant success data is ambiguous. Furthermore, success and survival data generally does not include periodontally compromised patients, and therefore is not clinically relevant to periodontal patients. To confuse matters further there are currently no standardised criteria for diagnosing and defining peri-implantitis, therefore disparities in prevalence data are present and clinical diagnosis of peri-implantitis may vary between clinicians and institutions. As a practitioner it is important to be aware of the limitations of implant success and survival data in order to appropriately consent all patients who wish to receive implant therapy.
Periodontal disease is a true risk factor for the development of peri-implantitis, however this does not mean implants are contraindicated in periodontal patients. Patients with a history of CP and AgP are at a higher risk of developing peri-implantitis, particularly AgP patients. Periodontally compromised teeth act as a reservoir of periodontal pathogens which colonise the peri-implant tissues (Figs 1 and 2). Interestingly, elimination of the subgingival environment by extraction of all natural teeth probably initiates the disappearance of the two periodontal bacteria, A. actinomycetemcomitans and P. gingivalis, therefore reducing the risk of peri-implantitis.56 In light of this, Royal College of Surgeons guidelines concerning selection of appropriate patients for dental implants in the National Health Service (NHS) suggest that patients who have been rendered completely edentulous from AgP should be considered for implant retained overdentures.57 However, a recent study has shown that although complete edentulation results in a significant reduction of bacteria related to periodontitis and peri-implantitis, A. actinomycetemcomitans was not eliminated, indicating that key periodontal pathogens can survive without pockets.58 Therefore, this patient cohort requires long term monitoring and maintenance due to their susceptibility to peri-implantitis.
Implants placed in a poorly maintained severe localised aggressive periodontitis patient with residual periodontal pocketing present 16, 46, 26 and 36 leading to inflamed hyperplastic gingivae, probing pocket depths of 6 mm+ and circumferential bone loss around implants in the 12, 11, 21 and 22 position
In order for implants to be placed successfully in patients with a history of periodontitis, correct pre-operative periodontal diagnosis and stabilisation is required. Making a correct periodontal diagnosis before implant placement is important to provide any necessary periodontal therapy and discuss prognosis and potential risks. As demonstrated by Cho-Yan Lee et al.,46 periodontally compromised patients without residual periodontal pockets have improved implant related clinical outcomes, therefore it is recommended that periodontitis should be stabilised before implant placement (Fig. 3). As periodontitis and peri-implantitis share a number of risk factors, pre-operative periodontal therapy should help control risk factors before implant treatment. However, it must be reiterated that similarly to periodontal disease, multiple factors are associated with the development of peri-implantitis (for example, host response, specific bacterial colonisation, host factors) and therefore long term monitoring and maintenance, as well as appropriate consent, should be provided.
Following implant placement, periodontal supportive therapy is required to maintain periodontal health and prevent peri-implantitis. Patients with residual periodontal pocketing have been shown to be at higher risk of developing peri-implantitis, therefore it is important regular monitoring and maintenance appointments are scheduled to prevent periodontal disease recurrence. All patients with a history of periodontal disease should be informed of the necessity of regular periodontal supportive therapy following implant placement as part of the consent process.
It is essential that adequate oral hygiene measures can be undertaken by the patient to ensure good plaque control. Good plaque control depends not only on patient education, compliance and dexterity, but prosthesis design also. Prostheses should allow adequate access for brushing, flossing and inter-proximal cleaning to help prevent peri-implantitis or periodontitis (Fig. 4). Interestingly, one study investigating peri-implantitis in association with plaque control reported that a high proportion of implants with a diagnosis of peri-implantitis (48%) were associated with no accessibility for appropriate oral hygiene measures, while accessibility for plaque control was rarely associated with peri-implantitis.59 Although this study was relatively small (23 patients), it highlights the important relationship between prosthesis design, plaque control and peri-implantitis. Unfortunately, research suggests that many implant patients fail to maintain adequate oral hygiene, with one UK study reporting that almost half of patients had unsatisfactory plaque control.60 Upon designing an implant retained prosthesis manual dexterity should be taken into account, with easily cleansable designs provided for patients with poor manual dexterity. It is fundamental that patients are educated on how to maintain adequate plaque control, and that this is frequently reviewed and reinforced to ensure long-term maintenance (Fig. 5).
Compared to the management of periodontitis, there is a paucity of data available for the management of peri-implantitis. Peri-implantitis treatment strategies are largely based on the evidence available for the treatment of periodontitis. However, the surface of implants differs significantly from the surface of natural teeth due to the screw shaped thread and various surface modifications, therefore making biofilm removal more difficult. In peri-implantitis lesions non-surgical debridement alone is ineffective, however, adjunctive local or systemic antibiotics alongside non-surgical treatment has shown to reduce bleeding on probing and pocket depths.60 Surgical access and debridement has scarcely been investigated, however, a case-series reported 58% of peri-implantitis lesions resolved following surgical debridement over 5 years61 (Fig. 5). Furthermore, a 12-month prospective study demonstrated 92% of implants had crestal bone stabilisation surgical debridement alongside systemic anti-microbial therapy.62 However, it must be iterated that there is currently not enough evidence to demonstrate the benefit of using antibiotics alongside surgical management. There is also a lack of evidence regarding the use of membranes or graft materials to encourage tissue regeneration, and although the few studies conducted report largely improved outcomes, reported failures and unpredictability of success were emphasised.61 A recent systematic review of seven studies reported favourable short-term outcomes for both surgical and non-surgical therapy, however the authors concluded that the available evidence does not allow any specific recommendations for the therapy of peri-implantitis.63 It is therefore fundamental that emphasis is put on the prevention of peri-implantitis.
Conclusion
The points raised by Baroness Gardner and the subsequent reports released by the GDC and FGDP(UK) in response to the House of Lords debate have significant relevance in the prevention of an increase in the prevalence of peri-implantitis. Case selection for patients receiving implants is extremely important and dental implants should not be seen as a panacea for tooth replacement. Implants can be placed in patients with a history of periodontitis, however, initial periodontal stabilisation is essential and regular maintenance therapy is paramount to minimise the risk of peri-implantitis. From a litigious point of view, documentation of pre-assessment periodontal status, periodontal treatment, monitoring and maintenance, early diagnosis of peri-implantitis and peri-implantitis treatment will be paramount if the number of complaints to the GDC and the incidence of reported legal activity by dental defence unions are to reduce. To ensure implant patients are being appropriately consented, selected and maintained, the FGDP(UK) have made a set of recommendations regarding dental implants and periodontal checks which are outlined in Box 1. To promote the prevention and detection of peri-implantitis, this guidance should be understood and followed in all implant cases.
References
White D A, Tsakos G, Pitts N B et al. Adult Dental Health Survey 2009: common oral health conditions and their impact on the population. Br Dent J 2012; 213: 567–572.
General Dental Council. Dental Complaints Service Annual Review 2013. Available online at http://www.gdc-uk.org/Newsandpublications/Publications/Publications/DCS%20Annual%20Review%202013%20FINAL.pdf (accessed Novermber 2016).
Dental Protection UK. Claims. Teamwise 2015; 16: 10.
Alani A, Bishop K, Renton T, Djemal S . Update on guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS-the position after 15 years. Br Dent J 2014; 217: 189–190.
Baroness Gardner of Parkes asked for Health: Dental Implants Question for Short Debate (HL Deb 23 July 2014 col GC494, GC495, GC496).
Faculty of General Dental Practice (UK) (FGDP(UK)). Briefing: House of Lords debate on dental implants and periodontal checks. Grand Committee, 23 July 2014.
Lindhe J, Meyle J ; Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 2008; 35: 282–285.
McCaul L K, Jenkins W M, Kay E J . The reasons for the extraction of various tooth types in Scotland: a 15-year follow up. J Dent 2001; 29: 401–407.
Fure S, Zickert I . Incidence of tooth loss and dental caries in 60-, 70-and 80-year-old Swedish individuals. Community Dent Oral Epidemiol 1997; 25: 137–142.
Demmer R T, Papapanou P N . Epidemiologic patterns of chronic and aggressive periodontitis. Periodontol 2000 2010; 53: 28–44.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J, Marcenes W . Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res 2014; 93: 1045–1053.
Socransky S S, Haffajee A D . Periodontal microbial ecology. Periodontol 2000 2005; 38: 135–187.
Genco R J . Current view of risk factors for periodontal diseases. J Periodontol 1996; 67: 1041–1049.
Heitz-Mayfield L J, Lang N P . Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 2000 2010; 53: 167–181.
Albrektsson T, Sennerby L, Wennerberg A . State of the art of oral implants. Periodontol 2000 2008; 47: 15–26.
Lindh T, Gunne J, Tillberg A, Molin M . A meta-analysis of implants in partial edentulism. Clin Oral Implants Res 1998; 9: 80–90.
Mombelli A, Müller N, Cionca N . The epidemiology of peri-implantitis. Clin Oral Implants Res 2012; 23: 67–76.
Porter J A, von Fraunhofer J A . Success or failure of dental implants? A literature review with treatment considerations. Gen Dent 2005; 53: 423–432.
Albrektsson T, Donos N . Working Group 1. Implant survival and complications. The Third EAO consensus conference 2012. Clin Oral Implants Res 2012; 23: 63–65.
Renvert S, Polyzois I . Risk indicators for peri-implant mucositis: a systematic literature review. J Clin Periodontol 2015; 42: 172–186.
Derks J, Tomasi C . Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol 2015; 42: 158–171.
Adell R, Lekholm U, Rockler B, Brånemark PI . A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981; 10: 387–416.
Albrektsson T, Zarb G, Worthington P, Eriksson A R . The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986; 1: 11–25.
Apse P, Zarb G A, Schmitt A, Lewis D W . The longitudinal effectiveness of osseointegrated dental implants. The Toronto Study: peri-implant mucosal response. Int J Periodontics Restorative Dent 1991; 11: 94–111.
Berglundh T, Persson L, Klinge B . A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol 2002; 29: 197–212.
Sanz M, Chapple I L ; Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol 2012; 39: 202–206.
Javed F, Al-Hezaimi K, Salameh Z, Almas K, Romanos G E . Proinflammatory cytokines in the crevicular fluid of patients with peri-implantitis. Cytokine 2011; 53: 8–12.
Schou S, Holmstrup P, Reibel J, Juhl M, Hjørting-Hansen E, Kornman K S . Ligature-induced marginal inflammation around osseointegrated implants and ankylosed teeth: stereologic and histologic observations in cynomolgus monkeys (Macaca fascicularis). J Periodontol 1993; 64: 529–537.
Berglundh T, Zitzmann N U, Donati M . Are peri-implantitis lesions different from periodontitis lesions? J Clin Periodontol 2011; 38: 188–202.
Casado P L, Pereira M C, Duarte M E, Granjeiro J M . History of chronic periodontitis is a high risk indicator for peri-implant disease. Braz Dent J 2013; 24: 136–141.
Swierkot K, Lottholz P, Flores-de-Jacoby L, Mengel R . Mucositis, peri-implantitis, implant success, and survival of implants in patients with treated generalized aggressive periodontitis: 3-to 16-year results of a prospective long-term cohort study. J Periodontol 2012; 83: 1213–1225.
Bergström J, Preber H . Tobacco use as a risk factor. J Periodontol 1994; 65: 545–550.
Strietzel F P, Reichart P A, Kale A, Kulkarni M, Wegner B, Küchler I . Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. Clin Periodontol 2007; 34: 523–544.
Hinode D, Tanabe S, Yokoyama M, Fujisawa K, Yamauchi E, Miyamoto Y . Influence of smoking on osseointegrated implant failure: a meta-analysis. Clin Oral Implants Res 2006; 17: 473–478.
Fernandes J K, Wiegand R E, Salinas C F et al. Periodontal disease status in gullah african americans with type 2 diabetes living in South Carolina. J Periodontol 2009; 80: 1062–1068.
Karimbux N Y, Saraiya V M, Elangovan S et al. Interleukin-1 gene polymorphisms and chronic periodontitis in adult whites: a systematic review and meta-analysis. J Periodontol 2012; 83: 1407–1419.
Genco R J, Borgnakke W S . Risk factors for periodontal disease. Periodontol 2000 2013; 62: 59–94.
Schou S, Holmstrup P, Worthington H V, Esposito M . Outcome of implant therapy in patients with previous tooth loss due to periodontitis. Clin Oral Implants Res 2006; 17: 104–123.
Ong C T, Ivanovski S, Needleman I G et al. Systematic review of implant outcomes in treated periodontitis subjects. J Clin Periodontol 2008; 35: 438–462.
Safii S H, Palmer R M, Wilson R F . Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: a systematic review and meta-analysis. Clin Implant Dent Relat Res 2010; 12: 165–174.
Chrcanovic B R, Albrektsson T, Wennerberg A . Periodontally compromised vs. periodontally healthy patients and dental implants: a systematic review and meta-analysis. J Dent 2014; 42: 1509–1273.
Sgolastra F, Petrucci A, Severino M, Gatto R, Monaco A . Periodontitis, implant loss and peri-implantitis. A meta-analysis. Clin Oral Implants Res 2015; 26: 8–16.
Sousa V, Mardas N, Farias B et al. A systematic review of implant outcomes in treated periodontitis patients. Clin Oral Implants Res 2016; 27: 787–844.
Leonhardt A, Adolfsson B, Lekholm U, Wikström M, Dahlén G . A longitudinal microbiological study on osseointegrated titanium implants in partially edentulous patients. Clin Oral Implants Res 1993; 4: 113–120.
Pjetursson B E, Helbling C, Weber H P et al. Peri-implantitis susceptibility as it relates to periodontal therapy and supportive care. Clin Oral Implants Res 2012; 23: 888–894.
Cho-Yan Lee J, Mattheos N, Nixon K C, Ivanovski S . Residual periodontal pockets are a risk indicator for peri-implantitis in patients treated for periodontitis. Clin Oral Implants Res 2012; 23: 325–333.
Karoussis I K, Salvi G E, Heitz-Mayfield L J, Brägger U, Hämmerle C H, Lang N P . Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res 2003; 14: 329–339.
Levin L, Ofec R, Grossmann Y, Anner R . Periodontal disease as a risk for dental implant failure over time: a long-term historical cohort study. J Clin Periodontol 2011; 38: 732–737.
Roccuzzo M, De Angelis N, Bonino L, Aglietta M . Ten-year results of a three-arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clin Oral Implants Res 2010; 21: 490–496.
Leonhardt A, Dahlén G, Renvert S . Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol 2003; 74: 1415–1422.
Swierkot K, Lottholz P, Flores-de-Jacoby L, Mengel R . Mucositis, peri-implantitis, implant success, and survival of implants in patients with treated generalized aggressive periodontitis: 3-to 16-year results of a prospective long-term cohort study. J Periodontol 2012; 83: 1213–1225.
Mengel R, Behle M, Flores-de-Jacoby L . Osseointegrated implants in subjects treated for generalized aggressive periodontitis: 10-year results of a prospective, long-term cohort study. J Periodontol 2007; 78: 2229–2237.
De Boever A L, Quirynen M, Coucke W, Theuniers G, De Boever J A . Clinical and radiographic study of implant treatment outcome in periodontally susceptible and non-susceptible patients: a prospective long-term study. Clin Oral Implants Res 2009; 20: 1341–1350.
Mengel R, Schroder T, Flores-de-Jacoby L . Osseointegrated implants in patients treated for generalized chronic periodontitis and generalized aggressive periodontitis: 3-and 5-year results of a prospective long-term study. J Periodontol 2001; 72: 977–989.
Tonetti M, Palmer R ; Working Group 2 of the VIII European Workshop on Periodontology. Clinical research in implant dentistry: study design, reporting and outcome measurements: consensus report of Working Group 2 of the VIII European Workshop on Periodontology. J Clin Periodontol 2012; 39: 73–80.
Danser M M, van Winkelhoff A J, van der Velden U . Periodontal bacteria colonizing oral mucous membranes in edentulous patients wearing dental implants. J Periodontol 1997; 68: 209–216.
Alani A, Bishop K, Renton T, Djemal S . Update on guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS-the position after 15 years. Br Dent J 2014; 217: 189–190.
Quirynen M, Van Assche N . Microbial changes after full-mouth tooth extraction, followed by 2-stage implant placement. J Clin Periodontol 2011; 38: 581–589.
Serino G, Ström C . Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res 2009; 20: 169–174.
Allen P F, McMillan A S, Smith D G . Complications and maintenance requirements of implant-supported prostheses provided in a UK dental hospital. Br Dent J 1997; 26: 298–302.
Renvert S, Polyzois I, Claffey N . Surgical therapy for the control of peri-implantitis. Clin Oral Implants Res 2012; 23: 84–94.
Heitz-Mayfield L J, Salvi G E, Mombelli A, Faddy M, Lang N P ; Implant Complication Research Group. Anti-infective surgical therapy of peri-implantitis. A 12-month prospective clinical study. Clin Oral Implants Res 2012; 23: 205–210.
Heitz-Mayfield L J, Mombelli A . The therapy of peri-implantitis: a systematic review. Int J Oral Maxillofac Implants 2014; 29: 325–345.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
King, E., Patel, R., Patel, A. et al. Should implants be considered for patients with periodontal disease?. Br Dent J 221, 705–711 (2016). https://doi.org/10.1038/sj.bdj.2016.905
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.905