Key Points
-
Provides an update on existing systems and procedures in relation to patient safety in dentistry in the UK.
-
Highlights the existence of conflicting advice which further complicates an overly burdensome process.
-
Suggests solutions to address the problems surrounding patient safety development in dentistry.
Abstract
Since the 'Francis Report', UK regulation focusing on patient safety has significantly changed. Healthcare workers are increasingly involved in NHS England patient safety initiatives aimed at improving reporting and learning from patient safety incidents (PSIs). Unfortunately, dentistry remains 'isolated' from these main events and continues to have a poor record for reporting and learning from PSIs and other events, thus limiting improvement of patient safety in dentistry. The reasons for this situation are complex.This paper provides a review of the complexities of the existing systems and procedures in relation to patient safety in dentistry. It highlights the conflicting advice which is available and which further complicates an overly burdensome process. Recommendations are made to address these problems with systems and procedures supporting patient safety development in dentistry.
Similar content being viewed by others
Introduction
Patients expect to be treated safely when seeking healthcare. 'Safe' means that patients are protected from abuse and avoidable harm. A patient safety incident (PSI) is defined as any unintended event caused by healthcare that either resulted in, or could have led to patient harm. PSIs have been shown to cause harm in 3% to 17% of hospital inpatients.1,2
When patient harm occurs in relation to healthcare it can be devastating, not just for the patient and their extended family and social network, but also for the treating clinician and their team. The CQC estimates that there are approximately 11,000 incidents of severe harm and up to 100,000 incidents of serious harm occurring each year within the NHS. Indeed, preventable adverse events could be costing 'approximately £1 billion' per year.3 We now recognise that by embracing a systems approach and a supported open culture, prevention of future adverse events is possible, as already demonstrated within the aviation industry.
Significant changes in healthcare regulation in the UK have taken place over the last 10 years. While some have arisen due to the changes in political leadership, many regulatory changes have been in response to alarming adverse events within NHS patient care. The most recent response to the events in the Mid Staffordshire NHS Trust, the 'Francis Report' (2012),4 recommended significant changes in amending our culture (whistleblowing without consequences) in recognising potential weaknesses in our healthcare systems, and has resulted in the implementation of improved regulation and new systems to ensure patient safety is prioritised.
In the Government's initial response to the Francis Inquiry, published in March 2013, we accepted the need to introduce a statutory 'duty of candour' for health and care providers. This contractual duty of candour was imposed on all NHS and non-NHS providers of services to NHS patients in the UK to 'provide to the service user and any other relevant person all necessary support and all relevant information' in the event that a 'reportable patient safety incident' occurs. A 'reportable patient safety incident' is one which could have or did result in moderate or severe harm or death. The Francis Inquiry also noted that observance of the duty should be policed by the Care Quality Commission (CQC).5,6,7
The Report4 made a number of recommendations about the duty of candour that can be summarised as follows:
-
Healthcare providers should be under a statutory duty of candour:
-
– To inform the patient, or other duly authorised person
-
– To inform their employer as soon as practicable, when they believe or suspect that treatment or care it provided has caused death or serious injury to that patient, and thereafter, provide such information and explanation as the patient reasonably may request
-
It should be a criminal offence for any registered medical practitioner, or nurse or allied health professional or director of an authorised or registered healthcare organisation to knowingly obstruct another in the performance of these statutory duties, provide information to a patient or nearest relative with the intent to mislead them about such an incident or dishonestly make an untruthful statement to a commissioner or regulator, knowing or believing that they are likely to rely on the statement in the performance of their duties.
It is recognised that patient safety incident reporting is particularly poor in dentistry compared with other healthcare settings.8,9,10,11,12 Both NHS and independent providers are obliged to report serious events, and there are stipulated guidelines regarding these events (including 'Never Events') clarifying the responsibility for all healthcare providers in their duty to report. Absence of a centralised and open reporting culture in dentistry means that we will not benefit from a learning culture and repeated errors compromising patient safety will continue to persist. This situation must be addressed.
This paper is an attempt to unravel the complex and multiple regulations, systems, processes and online recommendations for reporting patient safety incidents relating to healthcare and more specifically to dentistry. Recommendations are made to challenge some of the complexities within the current systems and to provide potential solutions.
What is a patient safety incident?
Patient safety incidents (PSIs) include; Adverse events/incidents, clinical incidents, critical incidents, medical errors, clinical errors, medical mistakes and sentinel events. These events may result in high, moderate, low or no harm (near misses). It is often said that 'near misses' are the 'nuggets' in developing improvement in patient safety, as we learn about preventable risks without harming the patient. There are a variety of regulations applied by numerous regulatory bodies that make reporting certain patient safety (notifiable) incidents obligatory for healthcare providers, whether in independent or NHS practice (Box 1).
Permanent harm is defined as arising directly from the incident (medical or surgical) and not related to the natural course of the patient's underlying condition. It is defined as permanent lessening of bodily functions, sensory, motor, physiological or intellectual, including removal of the wrong limb, organ, tooth and brain damage.
What is a Never Event?
A 'Never Event' is defined as a serious incident, although not all Never Events necessarily result in severe harm or death.13 A Never Event must:
-
Be wholly preventable, where guidance or safety recommendations are available at a national level and that provide strong systemic protective barriers
-
Have the potential to cause serious patient harm or death
-
Have occurred in the past, for example through reports to (NRLS)
-
Be easily recognised and clearly defined.
The 2015–2016 Never Event list published April 201513 includes 13 categories.
Here are some examples of Never Events of relevance to dentistry:
-
Wrong site surgery (WSS): (includes permanent dentition only) refers to a surgical intervention performed on the wrong patient or wrong site. The incident is detected at any time after the start of the procedure
-
Wrong side block: (includes permanent dentition only) refers to the use of local anaesthetic block on the wrong side and also, initiation of surgery (ie an incomplete extraction and re-implantation of an inadvertently extracted wrong tooth is still a Never Event)
-
Wrong implant refers to surgical placement of the wrong implant or prosthesis where the implant/prosthesis placed in the patient is other than that specified in the surgical plan either prior to or during the procedure and the incident is detected at any time after the implant/prosthesis is placed in the patient
-
Retained foreign object: 'Foreign object' includes any items that should be subject to a formal counting/checking process at the commencement of the procedure and a counting/checking process before the procedure is completed (such as swabs, needles, instruments and guide wires). Other examples include; displaced teeth, fractured bur heads, bone screws, orthodontic appliances, dentures, implant and endodontic related equipment which may be inhaled, swallowed or displaced into the inferior dental canal or maxillary antrum.
In some instances, Never Events may be discovered some time after the incident occurred. While delayed discovery is not a factor in determining whether an incident is a Never Event, it may have a bearing on the 16 improvements deemed necessary following investigation (for example, where subsequent procedural changes mean that additional action may be unnecessary). Where a Never Event is discovered by one organisation but appears to be the responsibility of another, the 'discovering' organisation should inform the originating organisation, and is not required to report the incident as its own responsibility.
Systems and processes
The tripartite regulation of dentistry by the General Dental Council (GDC), Care Quality Commission (CQC) and NHS lacks clarity and is further complicated by the multiple regulations pertaining to patient safety in dental practice. As a result of these regulations the obligatory reporting is multiple and complex.
To whom should PSIs be reported?
The type of incident, relating to patient care, will dictate how, when and to whom you report the incident. There are many regulatory bodies (Box 1) to which dental providers may have to report incidents and some incidents have a stipulated timescale for reporting.
Who should report the PSI?
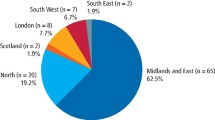
All PSIs should be reported anonymously by a pre-designated registered provider (usually practice principal or service manager), whilst protecting the patient's privacy in line with Data Protection regulations 1998 (Fig. 1 provides an overview on reporting a PSI in dentistry in relation to wrong site extraction).
Reporting PSIs is simple for general medical practitioners as there is an electronic proforma available for NHS practices.1 This simplifies PSI reporting to relevant bodies, most commonly the National Reporting and Learning System (NRLS). The CQC must also be informed of the PSIs in primary care NHS or independent practise. Within a trust or community dental service, the PSI would be reported through local risk management systems which are uploaded to the NRLS whilst directly informing local care commissioners. Serious events, including Never Events, must be reported within two days of their occurrence
Does reporting of PSIs only apply to NHS practice?
Both NHS and independent providers must report PSIs to the appropriate regulator. Recommendations for reporting of serious incidents occurring in independent sector healthcare or other provider outside the NHS include:
-
Independent sector healthcare providers must report any serious incident involving a patient receiving NHS funded care to the commissioning organisation with responsibility for the contract
-
Independent sector healthcare providers should report to the NRLS via the eForm15 of the NRLS, although this is voluntary and the CQC must be notified directly of abuse, serious injury and all deaths
-
Independent sector healthcare providers are also responsible for reporting the incident directly to their appropriate regulator.
NHS Commissioning area teams can, if appropriate, provide access to STEIS for non-NHS providers for reporting purposes as long as those providers are on the NHS N3 network (which most dentists are not), although NHS emails can be used instead.
What should happen after reporting PSI?
Managing the response to Never Events is a critical component of corporate and clinical governance. Providers must establish effective governance mechanisms to ensure the following:
-
The patient/family/carer must be informed as soon as possible when a Never Event occurs. Details of the conversation must be documented in the patient records; disclosure must not be delayed whilst the Never Event status is being determined. All staff should be familiar with related requirements of 'being open'15 and the 'duty of candour'.4 It is imperative that there is early, meaningful and sensitive engagement with the affected patients and/or their families/carers from the point that the Never Event is identified, throughout the investigation and action planning, to closure of the incident. Information should be shared in line with 'Being Open' guidance and the duty of candour15.
-
– Investigations are undertaken by appropriately trained and resourced staff and/or teams that are sufficiently removed from the incident to be able to provide an objective view
-
– An open and supportive culture is essential to facilitate and enable open reporting and learning from PSIs.
PSIs should be investigated via root cause analysis
Specifically dedicated trained staff should establish effective governance mechanisms to ensure the following:
-
Timely reporting and liaison with their commissioning bodies
-
Compliance with reporting and liaison requirements with agencies such as Monitor, the Trust Development Authority, the Care Quality Commission (CQC), Public Health England, the Health and Safety Executive, and coroners
-
Investigations follow a systems-based methodology to ensure identification of all the possible contributory factors and root causes, with focused actions and learning outcomes
-
Staff involved in the Never Event are supported and treated fairly, with reference to the NPSA Incident Decision Tree.16 The primary focus of the investigation should be on identifying underlying factors that contributed to the Never Event occurring, including understanding why the relevant barriers were not properly in place to prevent the Never Event
-
Commissioners are encouraged to publish information relating to all serious incidents, including Never Events, within annual reports and other public facing documents such as governing body reports, including data on the numbers and types of incidents, ensuring patient confidentiality is respected
-
Incidence of Never Events must be identified in the commissioner's annual report and the provider's quality accounts (ensuring patient confidentiality). This should include, where possible:
-
– Data on the type and number of Never Events, including historical context and related incidents
-
– A summary of each Never Event
-
– The learning derived from the incidents, with a particular focus on the system changes that have been made to reduce the probability of recurrence
-
– How learning has been shared at all levels within the organisation, and also, externally
-
Never Events are clearly defined as serious incidents and therefore, must be reported to the CQC
-
Failure to report a Never Event which subsequently comes to light through a third party route, (for example, a coroner's inquest, claim, media report, or patient complaint) is a serious failing on the part of staff involved and the organisation, and is likely to constitute a breach of CQC requirements17 (Regulation 16 and 18 of the CQC [Registration] Regulations 2009) and Service Condition 33 of the 2014/15 NHS Standard Contract, which sets out provider responsibilities for reporting incidents
-
For any failure to report a Never Event where there is evidence that there were opportunities for the provider to identify and report the incident, commissioners should consider using the full range of powers afforded via the NHS Standard Contract, including the following remedial actions:
-
– A detailed review and analysis of the circumstances leading to the failure to recognise and/or report the incident; relevant training (where indicated); and consideration of disciplinary action against individuals where there is evidence of deliberate non-disclosure
-
– Requiring the provider's chief executive (or equivalent) to deliver full written and verbal explanations of the failure to report a known Never Event, the circumstances of the incident and the actions taken in response, in public to the CCG board and to the relevant patient (subject to their agreement)
-
– Continued monitoring of agreed actions and use of powers to intervene (as per the NHS Standard Contract), where satisfactory progress is not made and patients remain at risk.
PSI reporting to the Care Quality Commission
In accordance with CQC's operating model, inspectors will ask if practices are safe, effective, caring, responsive and well-led, and will report their findings under the five key questions.
-
Are they safe? By safe, they mean that people are protected from abuse and avoidable harm.
-
Are they effective?
-
Are they caring?
-
Are they responsive to people's needs?
-
Are they well led?
The CQC use Key Lines of Enquiry (KLOEs) (Box 2) and request examples which demonstrate that no regulations have been breached. Specific examples of good practice are highlighted, including;
-
Having a clear understanding of and reporting as per RIDDOR (Reporting of Injuries, Diseases and Dangerous Occurrences Regulations 2013) and COSHH (Control of Substances Hazardous to Health)
-
Staff understand their responsibilities to raise concerns, to record safety incidents, concerns and near misses, and report them internally and externally where appropriate
-
The provider complies with relevant patient safety alerts, recalls and rapid response reports issued from the Medicines and Healthcare products Regulatory Authority (MHRA) and through the Central Alerting System (CAS).
The CQC will also investigate 'How are lessons learned and improvements made when things go wrong?'
-
Patients are told when they are affected by something that goes wrong, given an apology and informed of any actions taken as a result
-
The provider identifies and analyses clinical errors, incidents, errors and near misses involving all relevant staff and patients where applicable
-
Lessons are learned and communicated to make sure action is taken to improve safety.
What incidents should be reported to the CQC?
The incidents requiring obligatory reporting are as follows:
-
Never Events, serious incidents to people who use the activity delivered by the service and sentinel events (Box 3)
-
Changes in; statement of purpose for an activity, new provider to carry out activity, cessation of provider contract, name changes, nomination changes
-
Deaths of persons using the service
-
Allegations of abuse
-
Events that may stop the service from running safely and properly.
'Other incidents': The law says that you must notify the CQC without delay about a variety of 'other incidents' that take place while a regulated activity is being delivered or as a consequence of an activity being delivered.
Injuries: NHS providers notify relevant injuries to the NPSA using their local risk management system (LRMS) or the relevant eForm on the NPSA website.16
Deprivation of liberty applications and outcomes: There is a standard CQC form for notifying applications to deprive a person of their liberty under the Mental Capacity Act 2005, including the outcome of the applications. NHS providers can use this form to tell the CQC about applications by a hospital to a 'supervisory body', or to the Court of Protection for any other setting.
Abuse and allegations of abuse: It is important that providers tell relevant local safeguarding authorities about abuse and allegations of abuse in relation to their services appropriately, as described in the guidance about compliance.
Incidents reported to or investigated by the police: This notification requirement does not apply to NHS bodies.
Admission of a child or young person to an adult psychiatric ward or unit: Registered persons who provide psychiatric units for adults must notify CQC if they admit a child or young person aged under 18 years to such a location if that placement has lasted for a continuous period of more than 48 hours. All 'other incidents' notifications must be submitted without delay.
Medication adverse events: There is no requirement to notify CQC about medicine errors. However, a CQC notification would be required if the cause or effect of a medicine error met the criteria for one of the following to be notified:
-
A death (must also be reported to NRLS)
-
An injury (must also be reported to NRLS)
-
Abuse or an allegation of abuse
-
An incident reported to or investigated by the police.
Where relevant, it should be made clear that a medicine error was a known or possible cause or effect of these incidents or events being notified.
How to report these incidents to the CQC
All PSIs should be reported anonymously by a registered provider (usually practice principal or manager), whilst protecting the patient's privacy in line with the 1998 Data Protection Regulations, to the CQC or the NRLS and local primary care commissioners should be informed (see Box 4). Registered persons must use the forms supplied by CQC to submit notifications.
Discussion
Clinical practice is fraught with challenges and dentistry, in particular, is faced with increasing numbers of patient complaints and safety issues. Legislation for dental practice is predicated upon both patient and staff safety, however, the evolution of legislation into practice-based regulation and implementation has been slow with regards to patient safety. A recent systematic review of patient safety in primary care dentistry, reported that improving patient safety is a relatively new concept with a distinct lack of evidence base. In addition, reporting of adverse events in dentistry is significantly low.8,9,10,11,12 A previous analysis of NRLS data relating to dentistry also highlighted poor practice in reporting adverse events in dentistry.9
Why is incident reporting so poor in dentistry?
There are several areas that contribute towards poor learning from PSIs in dentistry9,11,12including;
-
Lack of a supportive and open culture
-
Complex and obtuse systems and processes
-
Lack of training and awareness of these systems and processes
-
Lack of examples whereby reporting systems have benefited patients and practitioners in dentistry
-
Poor communication and shared learning
-
Poor understanding of what can be learnt from the reporting of near misses.
Improving patient safety is based upon learning from mistakes. Without an open, supportive and non-punitive culture, mistakes will not be reported and nor will healthcare workers learn from them. Currently, the dental 'system' is not supportive of open reporting and many dentists in both primary and secondary care are fearful and reticent about reporting difficulties and failures. There are examples of junior doctor intimidation in hospitals where they have caused WSS and as a result, have left their jobs. This needs to change.
The current reporting systems are complex and obscure. This paper highlights how complex and confusing the various systems are when applied to primary care and specifically, to dentistry. For example, it is clearly stated that Never Event PSIs are serious events and must be reported to the CQC from NHS or independent providers. However, the NRLS Revised Policy and framework for Never Events (2014)18 clearly state that Never Events occurring in NHS care provision must be reported, with no reference to independent healthcare provision. It is no wonder that confusion arises with such conflicting information.
How can we improve reporting of PSIs in dentistry?
There is evidence that PSI reporting in a hospital environment may not be as effective as more labour intensive case note reviews.19
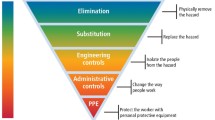
In 2004, the National Patient safety agency published Seven Steps to improving patient safety:20
-
Build a safety culture
-
Lead and support your practice team
-
Integrate your risk management activity
-
Promote reporting
-
Involve and communicate with patients and the public
-
Learn and share safety lessons
-
Implement solutions to prevent harm.
The paper also identified barriers to reporting PSIs, including unclear benefits to regular reporting, fear of blame, sense of failure, concern regarding litigation, lack of resources, 'not my job', lack of definitions and obscure processes.
The NPSA (2004)20 recommendations made to improve reporting of PSIs in primary care included:
-
Improving awareness and understanding
-
Adopting a common language for reporting
-
Linking local reporting system with national MRLS reporting system
-
Improving connectivity.
The British Government stated a commitment to making quality and safety the organising principle of NHS (2008).3 Despite this high profile initiative, improvement in the UK has been slow. The simple objective of avoiding preventable harm would seem straight forward but it remains difficult to implement. The key challenges to improving patient safety were identified as visibility, ambiguity, complexity and autonomy. Standards published by the GDC fall short of requirements (General Dental Council [GDC] in 2013) and make little reference to patient safety:
-
Principle 1 – put the patients' interest first
-
Standard 1.5.4 – you must record all patient safety incidents and report them promptly to the appropriate national body
-
Principle 8 – raise concerns if patients are at risk
-
Standard 8.1 – always put patients' safety first.
Barriers to reporting PSIs in dentistry
The main issues with regard to under reporting in dental primary care appear to be complex21 and most likely include a lack of understanding of:
-
Definitions of PSIs
-
Systems by which to report and learn
-
The benefits of reporting PSIs
-
A supportive open culture.24
Why should we bother reporting PSIs?
If the aviation operators continued to ignore safety incidents at work, many more deaths would have occurred. More importantly, there are missed opportunities for learning from each incident, which could potentially improve the quality of care/service provided and the environment in which the work is carried out.
Without an open and supportive culture, under reporting will continue. Unfortunately, there are still ongoing examples of intimidation and even junior staff that have been discharged following wrong site surgery (WSS) in dentistry, contravening the NPSA's 'Being Open' Framework.22
It is recognised that patient safety incident reporting is particularly poor in dentistry compared with other healthcare settings.8,9,10,11,12,14,21 Unless there is a centralised open reporting culture in dentistry, there will be no benefit from a learning culture and repeated errors compromising patient safety will persist. Urgent action is required to rectify this situation.
The duty of candour15,23,24 summaries the key action points:
-
The importance of learning from mistakes by reporting incidents and near misses
-
Ensuring management/regulators and commissioners provide organisational support to do this, as well as their responsibility to act on this information
-
The undertaking of relevant investigations and analyses
-
The importance of keeping patients informed and about ensuring affected patients know that things are being done to prevent harm to others.
Recommendations
-
Development of a supportive and non-punitive culture
-
Mandatory team training in patient safety, including PSI reporting for the whole dental team with team leader (champions) development in all provider settings
-
Development of a single, central, nationally funded PSI reporting process, supported by all the regulators, which has the responsibility of onward reporting of incidents to the regulatory bodies and dissemination of learning outcomes
-
Encourage a culture change in dentistry, similar to primary care medicine, in order to improve reporting of, and learning from patient safety incidents. Dentistry should be more immersed in general healthcare directives and initiatives related to improving patient safety
-
Clarify lines of communication for dissemination of patient safety information throughout dentistry (for example the recently published Nat SSIPPs or 'Sign up to Safety' campaign)
-
Obtain national agreement for a more relevant data set for PSIs in dentistry (to improve learning outcomes)
-
Promote the use of the eform14 (as currently used by GPs) for reporting patient safety incidents in primary care dentistry.
-
Improve the engagement with dental regulators GDC, CQC and NHS primary care dentistry, to align responsibility of promoting patient safety, and to address under reporting and mandatory training
-
Promote alignment of dental commissioning with patient safety initiatives
-
Advise amendment of the CQC Dental Provider Handbook to include sections on reporting (who/when/how) and a glossary of terms to define Never Events and other notifiable events.
This paper is an attempt to unravel the complex and multiple regulations, systems, processes and online recommendations for improving and reporting patient safety incidents relating to dentistry. A radical change is required to provide an open culture which encourages learning from and reporting incidents in dentistry. Standardisation, simplification and alignment between the regulators will significantly improve the processes and systems. The issues which have been raised are challenging, the concerns are well founded and the recommendations should be addressed as soon as possible, if the quality and safety of dental practice is to be improved.
References
Vincent C, Neale G, Woloshynowych M . Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001; 322: 517–519.
Brennan T, Leape L, Laird N et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard medical practice study I. N Engl J Med 1991; 324: 370–376.
House of Commons Health Committee Patient Safety Sixth Report of Session 2008–2009 Volume I Report Available online at http://www.publications.parliament.uk/pa/cm200809/cmselect/cmhealth/151/151i.pdf (accessed September 2016).
The Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry, February 2013. Available online at http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/report (accessed September 2016).
Care Quality Commission. A new start: consultation on changes to the way CQC regulates, inspects and monitors care, June 2013. Available online at https://www.cqc.org.uk/sites/default/files/documents/cqc_consultation_2013_tagged_0.pdf (accessed September 2016). https://www.cqc.org.uk/sites/default/files/documents/cqc_consultation_2013_tagged_0.pdf.
Registration under the Health and Social Care Act 2008 Statutory notifications Guidance for registered providers and managers of: · independent healthcare · adult social care · primary dental care · private ambulances April 2015 (PDF) https://www.cqc.org.uk/sites/default/files/20150331_100501_v6_00_guidance_on_statutory_notifications_ASC_%20IH_PDC_PA_Reg_Persons.pdf (accessed October 2016)
National Advisory Group on the Safety of Patients in England. A promise to learn – a commitment to act: improving the safety of patients in England, August 2013. Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/226703/Berwick_Report.pdf (September 2016).
E. Bailey M. Tickle & S. Campbell Patient safety in primary care dentistry: where are we now? Br Dent J 2014; 217: 339344.
Thusu S, Panesar S, Bedi R . Patient safety in dentistry state of play as revealed by a national database of errors. Br Dent J 2012; 213: E3; 10.1038/sj.bdj.2012.669.
Hiivala, Mussalo-Rauhamaa H, Murtmaa H . Patient safety incidents reported by Finnish dentists; results from an internet-based survey. Acta Odontol Scand 2013; 71: 1370–1377.
Pemberton M N . Developing patient safety in dentistry. Br Dent J 2014; 217: 335–337; 10.1038/sj.bdj.2014.856.
Bailey E, Tickle M, Campbell S, O'Malley L . Systematic review of patient safety interventions in dentistry. BMC Oral Health 2015; 15: 152.
NHS England. The 2015–2016 Never Events List 2015/16. March 2015. Available online at https://www.england.nhs.uk/wp-content/uploads/2015/03/never-evnts-list-15-16.pdf (accessed September 2016).
NHS England GP Patient Safety Incident Report e-form. Available online at https://report.nrls.nhs.uk/GP_eForm. (accessed September 2016).
Building a Culture of Candour Author: The Royal College of Surgeons of England Year: 2014 Area: Professional Clinical Standards (PDF) https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/building-culture-candour/ (accessed October 2016).
National Framework for Reporting and Learning from Serious Incidents Requiring Investigation (PDF) http://www.nrls.npsa.nhs.uk/EasySiteWeb/getresource.axd?AssetID=68464&type=full. (accessed October 2016).
Care Quality Commission. Regulation 5: Fit and proper persons: directors and Regulation 20: Duty of candour - Guidance for NHS bodies. November 2014. Available online at http://www.cqc.org.uk/sites/default/files/20141120_doc_fppf_final_nhs_provider_guidance_v1-0.pdf (accessed September 2016).
NHS England. Revised Never Events policy and framework 2015. Available online at https://www.england.nhs.uk/patientsafety/wp-content/uploads/sites/32/2015/04/never-evnts-pol-framwrk-apr2.pdf (accessed September 2016).
Baba-Akbari Sari, A, Sheldon T A, Cracknell A, Turnbull A . Sensitivity of routine system for reporting patient safety incidents in an NHS hospital: retrospective patient case note review. BMJ. 2007 Jan 13; 334: 79.
Seven steps to patient safety for primary care step - Full reference guide - Seven Steps (PDF) http://www.nrls.npsa.nhs.uk/resources/collections/seven-steps-to-patient-safety/?entryid45=59804 (accessed October 2016).
Bailey E . Contemporary views of dental practitioners' on patient safety. Br Dent J 2015; 219: 535–540.
NHS. Being Open Framework. Available online at www.nrls.npsa.nhs.uk/beingopen (accessed September 2016).
Medical Defence Union. Statutory duty of candour in secondary care. Available online at http://www.themdu.com/guidance-and-advice/guides/statutory-duty-of-candour/statutory-duty-of-candour (September 2016).
Guidance on Discharging the Duty of Candour and Disclosure in Judicial Review Proceedings (PDF). https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/285368/Tsol_discharging_1_.pdf (accessed October 2016).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Renton, T., Master, S. The complexity of patient safety reporting systems in UK dentistry. Br Dent J 221, 517–524 (2016). https://doi.org/10.1038/sj.bdj.2016.782
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.782
This article is cited by
-
Patient safety in dentistry - the bigger picture
British Dental Journal (2022)
-
Developing agreement on never events in primary care dentistry: an international eDelphi study
British Dental Journal (2018)
-
Patient safety: reducing the risk of wrong tooth extraction
British Dental Journal (2017)