Key Points
-
Explores patients' journey through the two-week wait referral process and makes suggestions for improving patients' experiences.
-
Identifies the top nine most commonly urgently referred benign conditions in this cohort.
-
Encourages discussions about more innovative ways of triaging referrals and oral cancer detection education.
Abstract
Objectives i) To prospectively explore patients' experience through the two-week wait (2WW) referral process; ii) To compare the relative true malignancy diagnostic rate between general medical practitioners (GMPs) and general dental practitioners (GDPs) over a six-month period; iii) To compare management of 2WW referral cases between GMPs and GDPs before the referral and during the 2 weeks in regards to symptomatic support, investigations in primary care, and information communicated to patients and secondary care clinicians; iv) To investigate the benign conditions that comprise 2WW referrals by finding out the final diagnoses of all cases included in the study.
Method The patient inclusion criteria were all 2WW referral patients who attended consultation clinics during the six-month study period in Royal Cornwall Hospital NHS Trust. We prospectively distributed patient questionnaires and clinician's referral assessment forms. We obtained the final diagnoses of all participants electronically, and also identified all malignancies diagnosed via routine referral route during the study period from the cancer services team.
Results Two hundred and twenty patients referred via 2WW pathway participated in the study. Of these, 148 referrals were from GMPs and 72 from GDPs. The overall malignancy diagnostic yield was 6.2%; markedly higher from GMPs (9.5%) than GDPs (1.4%), and higher number than those from routine pathway. The GMPs and GDPs showed similar levels of clinical management and information exchange judging from the participants' responses. We also identified the top nine most commonly urgently referred benign conditions.
Conclusion We reiterate the need for improved communication between clinicians and patients and between clinicians. We also suggest more focus on education in commonly encountered conditions as well as malignant lesions. The number of 2WW referrals we received from GMPs was nearly twice as many as those from GDPs, highlighting the importance of delivering oral medicine education to medical students, trainees and GMPs.
Similar content being viewed by others

Introduction
The two-week wait (2WW) head and neck cancer referral system was implemented nationwide in 2000,1 preceded by the white paper, The new NHS: modern, dependable2 published in 1997 – a proposal from the government that everyone with suspected cancer be seen by a specialist within two weeks of the date of general practitioner referral. In 2005, the National Institute for Clinical Excellence (NICE) published national referral guidelines outlining ten symptoms and signs of cancer that should prompt primary care clinicians to make an urgent referral.3
However, several studies have suggested that more cancer cases are identified through the routine referral pathway rather than the 2WW route.4,5,6,7 A 12-month period 2WW audit by Lyons et al.4 showed 15% malignancy yield. A prospective study by Shah et al.5 found 6% malignancy yield. McKie et al.6 conducted a retrospective audit of 1,079 2WW referrals received over a period of two years, and reported 10.9% malignancy yield from 2WW referrals. Williams et al.7 found an increasing number of 2WW referrals to their ear, nose, and throat department in ten years, but conversely, decreasing malignancy yield rate by approximately 50%.
Despite a great deal of literature demonstrating disappointing malignancy pick-up rates from the 2WW system, little has been written about some aspects of the system such as patients' experience of the 2WW system and, if there are so few malignancies identified through the 2WW pathway, which benign conditions comprise the 2WW referrals. Our study included investigations into these areas.
In addition, we compared general medical practitioners (GMPs) and general dental practitioners (GDPs) in regards to the relative true malignancy diagnostic rate and management of 2WW referral cases before the 2WW referral and during the two weeks. Oral and maxillofacial surgery units have a unique situation in that a significant number of referrals come from GDPs as well as GMPs. GDPs receive more undergraduate training in oral medicine/pathology, and are theoretically in a better position to detect oral cancers than GMPs.
A number of studies have previously compared GMPs and GDPs in regards to their ability to detect oral cancer and make appropriate referrals. Schnetler8 found that GMPs were better at referring early and suggesting malignancy as a diagnosis, but when a delay occurred it was longer than when it occurred with a GDP referral. Carter and Ogden9 reported that GMPs were less likely to examine patients' oral mucosa routinely, and felt less confident about diagnosing oral cancer from clinical appearance than GDPs. Greenwood and Lowry10 conducted a regional study to compare the knowledge of oral cancer between GDPs and GMPs, using a questionnaire. They found that the knowledge level of both groups was generally good with discrepancies in a few areas such as risk factor knowledge and clinical examination techniques.
Aims and objectives
The objectives of this study are as follows:
-
To prospectively explore patients' experience through the 2WW referral process
-
To compare the relative true malignancy diagnostic rate between GMPs and GDPs over a six-month period
-
To compare management of 2WW referral cases between GMPs and GDPs before the referral and during the two weeks in regards to symptomatic support, investigations in primary care, and information communicated to patients and secondary care clinicians
-
To investigate the benign conditions that comprise 2WW referrals by finding out the final diagnoses of all cases included in the study.
Ultimately, we aim to find out whether the current head and neck cancer referral triage system satisfactorily ensures an effective referral pathway for suspected cancer patients and efficient use of NHS resources.
Patients and methods
The patient inclusion criteria were all 2WW referral patients who attended consultation clinics over the study period of six months (from 2 January 2015 to 3 July 2015) in all sites of the Royal Cornwall Hospital NHS Trust (RCHT) where the oral and maxillofacial surgery team holds consultation clinics (Royal Cornwall Hospital and St Michael's Hospital). We used a patient questionnaire and a clinician's referral assessment form to investigate 2WW referrals prospectively. A patient questionnaire (appendix 1) was completed by 2WW patients before the consultation, except for the last two questions which could only be completed after the consultation. A clinician who assessed the patient completed the clinician's referral assessment form (appendix 2) after the consultation. The patient details were recorded on the questionnaires and assessment forms to allow tracking of the results of any diagnostic tests electronically. Additionally, we identified all malignancies diagnosed via routine referrals in the study period from the data provided by the cancer services team. All collected data were kept safely in accordance with the Data Protection Act of 1998.
Results
In the period of six months, the department received 243 referrals through the 2WW pathway; two of these patients did not show, two cancelled appointments, and 19 did not participate in the study. Therefore, 220 patients (148 from GMP referral and 72 from GDP referral) participated in the study (116 males and 104 females; mean age of 59.8 years). Eleven clinicians of varying grades in the oral and maxillofacial surgery department of the RCHT participated in the study.
Diagnoses
Malignant diagnoses
In total, 14 cases of malignancy were found among the participants referred through the 2WW route (13 from GMPs and 1 from a GDP). There was one case (GMP 2WW referral) of malignancy out of the nineteen 2WW patients who did not participate. During the study period, the department had three cases of malignancies from routine pathway; two from GMPs and one from a GDP. This means the overall malignancy diagnostic yield was 6.2% (15) from 2WW referrals over a six month period
Table 1 shows classification of malignant cases from 2WW referrals and routine pathways in terms of site, differentiation, and staging. The tongue was the most frequent site of malignancy – 8 out of 18 cases (44.4%). In terms of treatment, nine patients required excision only, four had neck dissection, two required major surgical procedures (one maxillectomy, one hemiglossectomy and floor of mouth resection with free flap reconstruction), three were inoperable; two of whom received palliative radiotherapy and one declined treatment. Five patients received radiotherapy. At the time of writing, there is one mortality from one of the patients with an inoperable tumour.
Common conditions
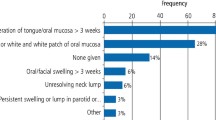
Table 2 shows the top nine most frequently referred common benign conditions in the 2WW cohort, and comparison of the number of referrals between GMPs and GDPs for each condition. The most commonly found condition was benign ulceration (37) diagnosed clinically (27) or histologically (10). The causes of benign ulceration included trauma (18), idiopathic (11), folate deficiency (3), serum ferritin deficiency (1), plasmacytosis (1), and nicorandil (1). The second most frequently urgently referred condition was non-neoplastic dental condition (21), ten of which came from GDPs. These conditions comprised periapical pathology (12), cyst of dental origin (3), dental abscess (2), oroantral fistula (2), and granulation tissue in a healing socket (2). Other commonly urgently referred conditions included normal anatomy (17), fibroepithelial polyp (16), keratosis (15), lichen planus (14), mucocele (10), haemangioma (10), and papilloma (9).
Patients' experience
The principle findings from patients' perspective are summarised in Table 3.
The number of visits to referrer before referral
All patients were seen by their referrer at least once before referral. 15.9% (35) of the referrers (17.6% of GMPs and 12.5% of GDPs) saw the participating patients twice before making the referral. 8.2% (18) of the cohort visited their referrer more than twice before referral. Out of the total 14 participants with malignancy, two patients (acinic cell carcinoma left naris and verrucous carcinoma anterior maxilla) saw their referrer three times before the referral was made, and the rest were referred after one visit to their referrer.
Information discussed regarding referral
The majority of patients were informed by their referrers the reason for referral (90.5%) and which speciality they were being referred to (69.5%). However, only 61 patients (27.7%) were told provisional or differential diagnoses and 65 patients (29.5%) were informed what they should expect to happen in the first appointment. Less than half of the cohort (44%) knew that they should expect to be seen within two weeks – GMPs communicated better than GDPs in this aspect (48.6% and 34.7%, respectively). The participating patients' responses showed similar levels of information exchange from GMPs and GDPs for all other categories questioned.
Support offered from primary care practitioners
Ninety-one patients (41.4%) in this cohort reported that their condition was accompanied by pain. Thirty-two (35.2%) out of all patients with pain received symptomatic support in terms of topical gel/cream/mouthwash (29), analgesics (8), or other systemic medications (14). GMPs and GDPs were similar in this aspect.
The department received 37 2WW referrals for a non-healing ulcer. Among them, 25 patients had pain – seven received analgesic support. Out of the total 14 participants with lichen planus (LP), ten had pain and four received analgesic support. Among the 14 participants with malignancy, nine had pain, four of whom did not receive analgesic support.
Investigations before referral
Twenty-five patients (11.6%) underwent investigations before referral; blood test (6), imaging (12), both blood test and imaging (1), swab (2), unspecified (4). A greater proportion of patients from GDP referrals (15.3%, 11) than those from GMP referrals (9.5%, 14) underwent investigations before referral. None of the 37 patients with ulcers had blood tests before referral.
Anxiety – before and after consultation
Before their first consultation at the RCHT, 170 patients (77.2%) in this cohort were anxious, to varying degrees, about the fact that they were being referred to a specialist unit. Two out of the 33 patients in the 'very anxious' group had malignancies. Six malignancies were diagnosed out of the 61 patients in the 'moderately anxious' group, five malignancies out of the 76 patients in the 'slightly anxious' group and one malignancy out of the 50 patients in the 'not anxious at all' group.
After their first consultation at the RCHT, 39 patients (17.7%) felt anxious, and nine of them were diagnosed with malignancy. 208 out of 220 patients (94.5%) found their first consultation at the RCHT helpful and informative.
Secondary care clinicians' 2WW referral assessment
The NICE guidelines
The vast majority of the referrals (93.6%) indicated how their case conformed to the NICE guidelines. Table 4 shows reasons for referral categorised into the NICE guidelines criteria. The most frequent reason for 2WW referral was unexplained suspicious lesion/symptoms persisting for more than four weeks. Fourteen referrers (nine referrals from GMPs and five from GDPs) did not specify how their referral met the NICE guidelines.
Information in the referral proforma and/or letter
Table 5 shows the information provided by the referrers in the referral proforma and/or letter. Medical history was the most frequently recorded information in the referral proforma/letter (65.5%), followed by drug history (59.1%), symptoms (56.4%), duration of the condition (55.5%), and social history (47.7%). The least-frequently recorded information was investigations and treatment already carried out (12.3%). A referral letter was attached in addition to the proforma in 64.1% of the cases. The frequency of each category of information given by GMPs and GDPs were mostly similar except in 'duration of the condition' and 'investigations/treatment already carried out' which GMPs communicated more often than GDPs.
Justifiable 2WW referral?
One hundred and twenty-five referrals (56%), including all 14 malignant cases, were deemed to be justifiable 2WW referrals by clinicians at the RCHT after the first consultation; 87 GMP referrals (58.8%) and 38 GDP referrals (52.8%). Analysis of free text responses to the last question revealed that the most frequent reason for considering a 2WW referral to be unjustifiable was 'classical/routine benign condition' (90).
Outcome of the first consultation
Table 6 shows plans after the first consultation. Further appointments (review, further investigation, added to operating list, or onward referral) were given to 166 out of 220 patients (75.5%). There were 149 patients referred for the top nine frequently urgently referred benign conditions outlined in Table 2. Out of these, 103 patients (69.1%) were given further appointment for management of a benign condition. Nearly one quarter (24.5%) of the cohort required no follow-up. Diagnosis (provisional or definitive) was reached in 195 cases (88.6%) in the first consultation.
Discussion
Diagnoses
Although the total malignancy diagnostic yield was low in keeping with results of other studies,4,5,6,7 we have found a much higher malignant diagnostic yield from 2WW referrals than routine ones which contrasts with the findings of many previously published studies.4,5,6,7 This should be interpreted with caution as the limitations of this study are that the results are only representative of the county of Cornwall over a six-month period only.
Due to the small number of malignancies diagnosed from the routine referrals during this study period, it was meaningless to compare the malignancies identified from the routine pathway with those from the 2WW referrals in terms of site, stage, treatment, and outcome.
The top nine frequently urgently-referred benign conditions in Table 2 comprised 67.7% (149) of the 2WW referrals. These results may indicate that the focus on oral cancer detection education should be more evenly distributed towards recognition of classical routine benign conditions.
A notable finding in this area was the number of non-neoplastic routine dental conditions referred through the 2WW pathway. This poses a question whether some primary care clinicians are over-using the 2WW system – as stated in Department of Health 2002,11 the hospital staff cannot change a 2WW referral to a non-urgent one. Brocklehurst et al.12 demonstrated that the default behaviour for primary care dentists is to refer the patient when in doubt. Their results were that high-risk social history factors were determinant in making the decision to refer, even when the GDPs expected the lesion to be benign.12
Patients' experience
To the authors' knowledge, this is the first study to prospectively investigate 2WW referrals from patients' perspectives. In terms of information discussed before referral, the majority of the cohort was not informed of their provisional/differential diagnoses by their referrers, and unaware that their expected waiting time for consultation was two weeks. Over 99% of 2WW referrals are seen within two weeks.13 Having an idea of the waiting period may reduce patient anxiety. Also, should patients not receive any correspondence from the specialist unit within the expected time, they can take appropriate steps to investigate.
Our study results showing that only 32 out of 91 patients (35.2%) with pain received symptomatic support from their referrers should be interpreted cautiously. It could be that some patients were not in enough pain to require analgesics, declined analgesics, or had a different source of analgesics. Nevertheless, under-usage of topical medication was noted from the results. Simple measures such as a prescription of steroid mouthwash could not only relieve symptoms of benign ulcers and LP, but also treat the condition and potentially negate the need for referral to secondary care. This is important considering the proportion (23.2%) of the benign ulcers and LP in this cohort.
Only a small proportion (11.4%) of the cohort had investigation before referral. Although primary care clinicians are generally not expected to carry out a biopsy of a lesion, it was disappointing that none of the 37 patients with benign ulcers had blood tests in their primary medical practice to exclude causes of benign ulcers such as vitamin B12, folate, or ferritin deficiency.
Secondary care clinicians' 2WW referral assessment
Despite the vast majority of the referrals (93.6%) meeting the NICE guidelines, the malignancy yield from 2WW referrals was only 6.2%. Our results about the outcomes of first consultation appointments should be carefully interpreted. Although 75.5% of our cohort required a follow-up appointment, for many of these patients, further appointments were made for management of routine benign conditions, rather than for management of suspected malignancy.
Interestingly, the participating clinicians commented that some cases met the NICE guidelines despite their classical history and appearance of a benign lesion, due to the duration of the lesion or the fact that the lesion was an 'unexplained' entity to the referrer. For example, it would be 'appropriate' to use the 2WW route to refer a symptomless fibroepithelial polyp on the tip of a tongue that has been present for five years with classical appearance and history, if the lesion is an 'unexplained' entity to the referrer.
This highlights the high sensitivity and low specificity of the current NICE guidelines, which may increase the use of the 2WW pathway by primary care clinicians as they may feel obliged to make such referrals in order to conform to the NICE guidelines and defend themselves medico-legally. This inevitably challenges the capacity of secondary care centres to meet the 2WW target. Indeed, Brocklehurst et al.14 reported that the most important determinant in predicting professional delay was hospital structural factors.
Having stated the above, it is difficult to imagine how guidelines can become more specific and exhaustive at the same time. A proposed solution to lower sensitivity and increase specificity is to improve communication between primary and secondary care clinicians by utilising technology. Given the trend of hospital records becoming increasingly electronic, a secure electronic referral system allowing transfer of digital photographs may be feasible in the not so far future. A study by Morton et al.15 found that photo-triage in a dermatology unit allowed definitive treatment to be delivered in the initial appointment in 91% of the patients, compared to 63% of the patients being referred via the letter-only referral.
Of course, the use of photography in the oral and maxillofacial surgery speciality would have its limitations. Specifically, oropharyngeal cancers and some neck lumps would not be detectable by photography in primary care. However, as Table 2 shows, we found the top nine frequently urgently referred benign conditions to be all oral lesions, and form a significant portion (67.7%) of the total cohort. Photography may have its place for classical oral lesions such as mucocele, fibroepithelial polyp, papilloma, and haemangioma, when accompanied by a history of the condition.
GMPs vs GDPs
GDPs have more training in oral medicine than GMPs. Yet, interestingly, GMPs had a much higher malignancy yield compared to GDPs, and managed cases very similarly in most aspects of the 2WW referral process investigated in this study. It may be that many of the unnecessary referrals are coming from clinicians who have not had much exposure to head and neck cancer detection in their training or postgraduate education. Or it may be that a more innovative approach to the education on oral cancer detection is required. Rafiq et al.16 found an increase in the urgent referrals during and after Mouth Cancer Awareness Week at Aintree oral and maxillofacial surgery unit, but could not definitively attribute this to the campaign. It would be interesting to compare the effects of different modalities of education in the long-term.
It should be pointed out that we had a much higher number of 2WW referrals and malignance pick-up rate from GMPs (148 referrals, 9.5%) than from GDPs (72 referrals, 1.4%). Some interesting questions that this study does not answer are: how many of the patients referred by GMPs had a registered GDP or a regular dental review; and how many of the GMP-referred 2WW cases could have been dealt with or routinely referred by GDPs? Rodgers et al.17 found that 59% of the participants with concerns about their oral health consulted their GMP rather than their GDP (29%). The authors suggested reasons for this phenomenon, including: patients associating dentists only with teeth; not being registered with a GDP; financial reasons; and fear of the dentist.17 Importantly, lower dental attendance of high-risk patients has been reported previously,18 and there is a general lack of awareness of mouth cancer among those treated for oral and oropharyngeal cancer.19 These findings support the need for increased exposure to oral medicine in medical training. Shanks et al.20 reported that 73% of their medical student cohort had not been taught how to examine the oral cavity, and 89% felt that the tuition given had not been adequate.
Conclusion
The overall malignancy diagnostic yield was low, but markedly higher from GMPs than GDPs, and also higher than that from the routine pathway. Generally, GMPs and GDPs managed patients similarly in the aspects investigated in this study, before 2WW referral and during the two weeks. We reiterate the need for improved communication between clinicians and patients, and between clinicians. We also suggest more focus on education in commonly encountered conditions as well as malignant lesions. The number of 2WW referrals we received from GMPs was nearly twice as many as those from GDPs, highlighting the importance of delivering oral medicine education to medical students/trainees and GMPs.
References
Department of Health. The NHS cancer plan. London, 2000.
Department of Health. The new NHS: modern, dependable. London, 1997.
National Institute for Health and Clinical Excellence (NICE). Referral guidelines for suspected cancer. London, 2005.
Lyons M, Philpott J, Hore I, Watters G . Audit of referrals for head and neck cancer – the effect of the 2week, fast track referral system. Clin Otolaryngol Allied Sci 2004; 29: 143–145.
Shah H V, Williams R W, Irvine G H . Fast-track referrals for oral lesions: a prospective study. Br J Oral Maxillofac Surg 2005; 44: 207–208.
McKie C, Ahmad U A, Fellows S et al. The 2-week rule for suspected head and neck cancer in the United Kingdom: Referral patterns, diagnostic efficacy of the guidelines and compliance. Oral Oncol 2008; 44: 851–856.
Williams C, Byrne R, Holden D, Sherman I, Srinivasan V R . Two-week referrals for suspected head and neck cancer: two cycles of audit, 10 years apart, in a district general hospital. J Laryngo Otol 2014; 128: 720–724.
Schnetler J F C . Oral cancer diagnosis and delays in referral. Br J Oral Maxillofac Surg 1992; 30: 210–213.
Carter L M, Ogden G R . Oral cancer awareness of general medical and general dental practitioners. Br Dent J 2007; 203: 248–249.
Greenwood M, Lowry R J . Primary care clinicians' knowledge of oral cancer: a study of dentists and doctors in the North East of England. Br Dent J 2001; 191: 510–512.
Department of Health (2002) Achieving the 2week Standard: Questions and Answers. Available online at http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4054826.pdf (accessed in May 2016).
Brocklehurst P R, Baker S R, Speight P M . Factors which determine the referral of potentially malignant disorders by primary care dentists. J Dent 2010; 38: 569–578.
Richards M . Cancer ten years on: improvements across the whole care pathway. London: Department of Health, 2007.
Brocklehurst P R, Rafiq R, Lowe D, Rogers S . Analysis of the impact of deprivation on urgent suspected head and neck cancer referrals in the Mersey region between January 2004 to December 2006. Br J Oral Maxillofac Surg 2012; 50: 215–220.
Morton C, Downie F, Auld S et al. Community photo-triage for skin cancer referrals: an aid to service Delivery. J Clin Exp Derm 2011; 36: 248–254.
Rafiq R, Brocklehurst P R, Rogers S N . Effect of Mouth Cancer Awareness Week on urgent suspected head and neck cancer referrals. Br J Oral Maxillofac Surg 2013; 51: e183–e185.
Rodgers J, Macpherson L M, Smith G L, Crighton A J, Carton A T, Conway D I . Characteristics of patients attending rapid access clinics during the West of Scotland Cancer Awareness Programme oral cancer campaign. Br Dent J 2007; 202: 680–681.
Haughney M G J, Devennie J C, Macpherson L M D, Mason D K . Integration of primary care dental and medical services: a three year study. Br Dent J 1998; 184: 343–347.
Rogers S N, Vedpathak S V, Lowe D . Reasons for delayed presentation in oral and oropharyngeal cancer: the patients perspective. Br J Oral Maxillofac Surg 2011; 49: 349–353.
Shanks L A, Walker T W M, McCann P J, Kerin M J . Oral cavity examination: beyond the core curriculum? Br J Oral Maxillofac Surg 2011; 49: 640–642.
Acknowledgements
We are grateful to the Cancer Services team and Oral and Maxillofacial Surgery team at the Royal Cornwall Hospital for their support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hong, B., Shaikh, Z., Adcock, S. et al. Two-week wait false alarms? A prospective investigation of 2WW head and neck cancer referrals. Br Dent J 220, 521–526 (2016). https://doi.org/10.1038/sj.bdj.2016.376
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.376