Key Points
-
IAN exposure during third molar surgery cannot be considered a 'warning sign' of nerve damage.
-
The crown luxation should preferably be performed in a direction ipsilateral to the IAN running.
-
Difficult surgeries, multi-rooted teeth and changes in IAN running in relation to tooth roots are real predictors of IAN damage.
Abstract
Aim The risk factors associated with inferior alveolar nerve damage during third molar surgery were investigated.
Material and methods Surgeries performed during a period of 50 months by a single expert surgeon were reviewed. Only those surgeries that met the selected inclusion criteria were considered for this study. The following tests were applied for the statistical analysis: the Kolmogorov-Smirnov test, the principal components analysis, the Mann-Whitney U test, the two-tailed exact Fisher test and the Bonferroni sequential correction.
Results The surgical difficulty index, multi-rooted third molars and changes in the inferior alveolar nerve running in relation to the tooth roots are predictors of nerve damage.
Conclusions Computed tomography is mandatory when the nerve is superimposed on the tooth root on the ortopantomography.
Scientific rationale for study Lower third molar extraction is one of the most common procedures in oral and maxillofacial surgery, and it is burdened by the risk of inferior alveolar nerve damage. Understanding which factors are able to predict this complication is therefore essential in correctly programming surgery.
Principal findings Surgical difficulty index, multi-rooted third molars and changes in inferior alveolar nerve running in relation to the tooth roots are predictors of nerve damage.
Practical implications If, on the orthopantomography, the nerve is superimposed on the tooth root, a computed tomography is mandatory to define all of these variables.
Similar content being viewed by others
Introduction
Lower third molar extraction is one of the most common procedures in oral and maxillofacial surgery,1,2 and it is burdened by a 0.26–8.4% risk of inferior alveolar nerve (IAN) damage.3,4,5,6,7,8 Fortunately, the damage is mostly temporary and it spontaneously resolves within six months, while in less than 1% of cases sensory alterations persist.7,9,10,11
The most important predisposing factor of IAN damage seems to be close proximity between the nerve and the third molar roots.6,11 Many studies have found a positive correlation between some orthopantomographic signs and nerve damage, but the data were not univocal.4,5,6,10,12,13,14,15,16,17,18,19,20,21
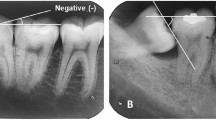
Three out of the seven radiographic aspects that were proposed by Rood and Shehab10 in 1990 are suggestive that a close relationship between the nerve and tooth roots seems to be strongly predictive of surgical nerve damage: mandibular canal deviation, root darkening and morphological root alterations.6
Other factors or conditions affecting the risk of nerve damage seem to be patient age, horizontal tooth position, deep impaction, local haemorrhage, intra surgical nerve exposure and lingual split technique.5,6,7,10,14,17,22
There is not a unanimous consensus concerning the role that the surgeon's experience may play in the risk of IAN damage.6,14,22,23
Coronectomy has been proposed to completely avoid the risk of nerve damage. However, this technique does not seem to represent a broad consensus because it is burdened with limited complications and because of the prognostic dilemma related to an incomplete intervention.11,24,25,26
The preoperative diagnostic usefulness of computed tomography is still debated due to its high biological and economic costs compared to the low incidence rate of IAN damage.3,5,10,11,14,17,18,19,21,27,28,29,30,31,32
Perfect knowledge of the factors that affect the risk of nerve damage is important for adequately programming surgery and for obtaining informed consent from the patient.
Therefore, the aim of the present study is to evaluate whether any of the following factors are associated with a high risk of IAN damage during lower third molar surgery:
-
Patient-related factors, including gender and age
-
Radiographic signs, including orthopantomography (OPG), which determines the risk markers, Pell and Gregory class, impaction depth (Modified Winter's Classification), root morphology and tooth position, and computed tomography (CT), which determines mandibular canal position in relation to each tooth root and the cortical bone presence/absence separating the nerve from the tooth
-
Clinical/surgical factors, including the maximum mouth opening, impaction type, IAN intra-operative exposure, intra-operative haemorrhage, real post-surgical root anatomy and the impression of the mandibular canal on the tooth root
-
Other factors including the surgical time and difficulty index.
Materials and methods
Third molar surgical extractions performed in an outpatient setting under local anaesthesia from 1 March 2008 to 30 June 2012 at the Complex Operative Unit of Oral Surgery, Department of Odontostomatological and Maxillofacial Sciences, 'Sapienza' University of Rome, by a single expert surgeon (RP) were retrospectively reviewed. The inclusion criteria were the following:
-
Complete clinical and radiographic documentation
-
Availability of both OPG and CT exams of each case to be revaluated
-
The presence of an OPG superimposition between the third molar roots and the upper half of the mandibular canal, in association or not with one or more radiographic signs are among those proposed by Rood and Shehab10
-
Surgical technique with a buccal approach and the following requirements: luxation of the upper portion of the tooth in the direction ipsilateral to the IAN running to limit nerve compression; use of a magnification device (Zeiss 4 × 300) during inspection of the residual bone cavity while searching for IAN identification, due to surgical exposure
-
Patients' consent to statistical treatment of their clinical and radiographic data collected upon surgery
-
Radiographic evaluation that was independently performed by two different surgeons (RP, MS); in the case of different interpretation, the evaluation of a third investigator was scheduled.
For each surgery, a difficulty index was calculated assigning a score of 1–3 to each of the following six variables: tooth inclination (mesio-angular/vertical = 1, horizontal = 2, disto-angular = 3), impaction depth (Modified Winter's Classification: A/B = 1, C1 = 2, C2 = 3); Pell and Gregory's class (I = 1, II = 2, III = 3), root morphology (fused or separated but non-divergent = 1, separated divergent = 2, with apical anomalies = 3), IAN/root relationship (not present = 1, present on the horizontal plane = 2, imbrications = 3); and maximum mouth opening (>4 cm = 1; 3–4 cm = 2; <3 cm = 3). Therefore, for each extracted third molar, a total score between 6–18 was obtained.33
For statistical analysis, the 'damage/no damage' dependent binary variable was used. This variable showed an unusual distribution with only 6/74 cases of damage differing by either a binomial distribution (k–s: d = 0.919; p <0.01) or by a Poisson distribution (k–s: d = 0.922, p <0.01), and therefore a non-parametric analysis was used. The principal component analysis34 (PCA) was first performed on the following quantitative explanatory variables: age of the patients, number of OPG risk signs, number of third molar roots on the OPG and CT images, maximum mouth opening, surgical difficulty index and surgical time.
The PCA is a multivariate analysis that allows to replace the original explanatory variables with a lower number of compound variables called 'factors', linearly independent between them (correlation = 0), and thus it allows to reduce the number of statistical tests to be carried out, decreasing the risk of incurring spurious significance. Specifically, the factors represent a linear combination of the original variables, that is, they represent that part of the data variability that is common to each of the original variables. In other words, each factor 'captures' the common part of each original variable and 'discards' its specificity. The factors are all constructed by combining the same original variables but differ in relation to the regression coefficient associated with each original variable which is in turn proportional to the correlation between the same factor and that variable. They have a mean value of zero and a standard deviation of one. Normally, the PCA provides a factor for each of the original variables, but since the first two factors, taken together, generally explain at least 70% of the total data variability, they can be used alone. However, because in the present case the first two PCA factors explained only 51% of the total data variability, the first four factors were therefore used for the analysis because they together explained approximately 80% of the total data variability. The Mann-Whitney test was then used to verify the association between each of these factors and the 'IAN damage' dependent variable.
Finally, the two-tailed exact Fisher test was used to evaluate the effect of the following qualitative explanatory variables on the probability of IAN damage: gender, presence/absence of OPG risk signs, change of nerve position with respect to third molar (yes/no), presence of cortical bone between the nerve and the tooth (continuous/interrupted), surgical IAN exposure (yes/no), nerve impression on the tooth root (yes/no), ostectomy (yes/no), odontotectomy (yes/no), CT IAN position with respect to the third molar (L = lower, B = buccal, L = lingual, IR = inter-radicular), third molar position (V = vertical, D = disto-angular, M = mesio-angular, H = horizontal), root anatomy (fused/slightly divergent, highly divergent, imbricated), Pell and Gregory Class (I, II, III), impaction depth (A–B/C1/C2), and impaction type (partial, osteo-mucosal, osseous).
When a series of different tests is carried out on the same data, a significant result is likely to be found due to the effect of chance. To prevent this, the 'Bonferroni sequential correction' was applied to 'adjust' the significance level (α = 0.05) of all the significant variables and to avoid false positives.
Results
During the reporting period, 74 lower third molar extractions satisfied all inclusion criteria of the study. In all cases the radiographic evaluations performed by the two surgeons coincided.
Surgery was performed on 63 patients, of which 23 were males (36.5%) and 40 were females (63.5%). All patients were symptomatic because of third molar impaction. Eleven patients underwent two surgeries in different time periods. To meet the objectives of the study, each lower third molar was considered a statistical unity. The age of the patients at the time of surgery was between 16 and 57 years, with an average age of 24.8 ± 6.37. Temporary nerve impairments (9–22 days) occurred in six cases (8.1%); they were clinically diagnosed with the tactile test using a 27-gauge needle tip and personally followed once a week until resolved, that is, when the patient reported to perceive the pin-prick in the affected side in the same way as healthy side. In none of the cases intra-operative haemorrhage occurred and the real tooth anatomy always coincided with that visualised on CT images.
Sample characteristics for the selected variables are listed in Tables 1 and 2.
Factor one of the PCA (Table 3) showed a strong negative correlation with the root number that was observed on the OPG (−0.844) or on CT (−0.855) images, while it had a weak positive correlation with either the difficulty index (0.511) or the patient age (0.493). Therefore, teeth with highly negative factor one scores were multi-rooted, easy to extract and were extracted from young patients. Moreover, the number of roots detected with OPG was strongly related to that detected with CT. Specifically, they co-varied in the same direction.
Factor two of the PCA (Table 3) showed a negative correlation with the difficulty index (−0.577), the surgical time (−0.517) and the number of roots, (−0.490 OPG; −0.449 CT), while it had a positive correlation with the mouth opening (0.460). Therefore, teeth with high factor two scores were associated with difficult and long-lasting surgeries, patients with limited mouth opening capability and with multi-rooted teeth. Factor two was also significantly associated with IAN damage (p = 0.0016) in that 'no nerve damage' was associated with higher factor two values (medium rank: 2709), whereas 'nerve damage' was associated with lower factor two values (medium rank: 66.00, Fig. 1). Therefore, IAN damage was significantly more likely to occur during more difficult extractions of multi-rooted teeth, whereas these types of teeth did not significantly affect the probability of nerve damage if associated with more simple surgeries (factor one of the PCA).
Lower values of factor 2 indicate more difficult surgeries and multi-rooted teeth, whereas higher values indicate easier surgeries in single-rooted teeth. Smaller squares in the centre represent the median values on 'factor 2'. Boxes represent values comprising the second and third quartiles; vertical axes indicate the minimum and maximum values of 'factor 2'
It is important to note that while the factor one represented teeth with multiple roots associated with not difficult extractions or teeth, with one root associated with difficult extractions, the factor two represented teeth with multiple roots associated with difficult extractions or teeth with one root associated with not difficult extractions.
Factor three of the PCA (Table 3) was strongly positively related with maximum mouth opening (0.693) and surgical time (0.633). This represented the cases in which the surgery time was long-lasting, although the patients presented with a large mouth opening that facilitated surgery.
Factor four of the PCA (Table 3) was strongly negatively related only to the number of risk signs detected on the OPG (−0.884).
As for qualitative variables, only 'IAN/third molar position change', 'depth' and 'impaction type' were significantly associated with nerve damage. Specifically, the probability of damage seems to increase when IAN position changes with respect to the third molar roots (p = 0.0029) and when the tooth is superficially impacted (p = 0.0057) and is completely in the bone (p = 0.0228).
Lastly, the 'Bonferroni sequential correction' for the 18 performed tests showed that only 'factor two' and 'IAN/third molar position change' could be considered statistically significant variables (Table 4).
Discussion
In the present study, the percentage of sensitivity impairments (8.1%) was at the upper end of the range reported in the international literature (0.26–8.4%),3,4,5,6,7,8 although all of the procedures were performed by the same expert surgeon. However, the study sample was comprised only of third molars with a high risk of IAN damage, due to the radiographic superimposition between the third molar roots and the mandibular canal, and, in all cases, the symptoms completely disappeared within 22 days; therefore, all of the lesions can be classified as 'neuropraxia'.
Although four out of six patients with IAN alterations were females, no significant statistical correlation was found between gender and nerve damage. Variable results were previously reported as gender concerns.6,14,15,22
Smaller mandible dimensions may explain the greater incidence of IAN damage in females due to a more strict relationship between third molar roots and IAN.15
The age of patients at the time of surgery was also not found to be statistically related with IAN damage as well.3,14,15,22,23,35,36,37,38
Given that mandibular extraction was previously found to be more simple and the healing process was better in young patients than in older ones, many authors suggest performing this type of surgery during adolescence when third molar roots are not completely mineralised, which thereby reduces the risk of nerve damage due to apical compression.9,14,22,38
None of the radiographic signs proposed by Rood and Shehab10 were significantly related with the risk of IAN damage, even when more than one sign was simultaneously present. In fact, the OPG was previously found to be unsuitable for predicting nerve damage due to its low sensibility and high specificity in defining the relationship between the third molar and the IAN.3,5,10,14,17,19
Intra-operative IAN exposure was not found to be related to nerve injury, in contrast to what many other authors have previously reported (Table 5).3,5,13,14,16,22,28,36,38,39,40,41 In the present study only a 6.5% incidence of IAN damage was found in the cases of nerve exposure, compared to a 9.3% incidence when the nerve was not exposed.
It seems logical that the risk of nerve damage is higher if the nerve is not exposed during surgery. If ostectomy is limited and/or the root axis is inclined, resulting in the nerve not being exposed, a slightly more intense force is necessary for root luxation, which results in an increased risk of nerve compression. Therefore, inferior alveolar nerve exposure cannot be considered a 'warning sign' of nerve damage but only a clinical confirmation of the close spatial relationship between the tooth and the nerve trunk. However, IAN visibility can be hindered by the following conditions: a narrow ostectomy for extraction, inclination of the alveolar walls, blood clotting on the bottom of the alveolar cavity, and identification difficulties when viewed at life-size.
The first two conditions are unavoidable. The third condition can be avoided by looking for the IAN immediately after the root extraction is completed and a saline irrigation is performed. The fourth condition is limited by using a magnification tool during surgery as in the present study sample.
Contrary to previous reports,6,27,39,40 no significant correlation was found between nerve damage and the absence of the cortical bone to separate the nerve from the tooth, ie an interruption of the IAN canal wall, or between nerve damage and nerve impression on the tooth root. Nevertheless, in the present study, a specific extraction technique was always used to avoid nerve compression. Specifically, the tooth crown was always pushed ipsilaterally towards the root side, which was in contact with the nerve. However, to the best of the authors' knowledge, no technical suggestions were ever previously reported.
According to Maegawa et al.27 and Ghaeminia et al.,41 the lingual position of the nerve to the third molar seems to be more liable to nerve damage (67%), although no statistical correlation was found. This result seems to contradict the expectations of the surgeon in that the luxative movements on tooth crowns directed ipsilaterally to the nerve position are more difficult to perform when the nerve is buccal because an effective fulcrum for the elevator action ismissing on the lingual side.
Although non univocal results were found by different authors with reference to the possible correlation between nerve damage and some third molar topographic variables such as position, Pell and Gregory class, and the type and depth of tooth impaction, both the full and deep impaction and the horizontal position were previously associated with a greater risk of nerve damage.3,7,14,21,22,23,36,37
The present study did not show a significant correlation between third molar anatomic-topographic variables and nerve damage. However, all such variables were used to define the difficulty index of third molar surgery, which contrarily, resulted in statistical significance related to the risk of nerve damage. To the best of the authors' knowledge, no other authors have found a statistically significant relationship between nerve damage and the difficulty index of surgery. Specifically, contrary to the study carried out by Jeries et al.,7 no correlation was found between IAN damage and the horizontal position of the impacted third molar because, as argued by the authors, greater bone removal is required for this condition, thus reducing the luxative force needed for extraction.
The presence of more than one root was the only anatomic variable related to IAN damage, but this variable was not included among those considered in calculating the total difficulty index. Moreover, no correlation was found between surgical time and nerve damage. Therefore, it is suggested from this study that highly difficult surgeries with a high risk of nerve damage are not necessarily associated with long surgical times.
As for the qualitative variables, the greater risk related to superficial impaction can be explained by underestimation of the difficulty of tooth extraction prompting the surgeon to perform a luxative movement mainly directed in an upper and distal direction, regardless of the root-nerve relationship. As for the greater risk related to complete bone impaction, this condition usually involves a high undercut and, consequently, a high resistance to tooth luxation especially when the cavity obtained around the tooth is not wide enough to reduce the amount of the removed bone. In this last case, the force required for tooth luxation may be too strong, resulting in high compression on the adjacent nerve.
As for the IAN/third molar relationship, dissimilar to the results reported by de Melo Albert et al.,12 the IAN did not always maintain the same spatial relationship with the tooth roots in this study (five cases = 6.7%). This has proven to be a significant risk factor for nerve damage. Actually, it is possible that tooth luxation caused nerve compression in case the surgeon decided not to perform root separation due to the limited superimposition between the nerve and the root (one out of five cases with IAN damage in multi-rooted teeth and IAN/third molar position change). Moreover, it is possible that nerve compression occurred when tooth luxation was directed upwards in the presence of slight lingual or buccal curvatures of the roots or when a close contact with one of the roots was present but not radiographically evident, as the nerve impression on the extracted root showed.
Despite the low rate of nerve damage in lower third molar surgery and the biological costs, which additional radiological exams incur, CT must be considered as an important tool in programming this type of surgery when a superimposition between the IAN and the third molar roots is clearly evident on OPG. Moreover, because the identification of any change in the nerve running in relation to the tooth root can be assumed to be a predictor of nerve damage, CT allows the surgeon to obtain true informed consent from the patient.
Results of the present study are not generalisable because surgeries were performed only by one surgeon and because the present analysis was strongly affected by the low frequency of IAN damage. A prospective study involving more than one surgeon, with different surgical experience, and a wider third molar sample should therefore be analysed to confirm the present results. In conclusion, within the limits of the study, it can be asserted that the surgical difficulty index, multi-rooted third molars and changes in IAN running in relation to the tooth roots are predictors of nerve damage. If, on the OPG, the nerve is superimposed on the tooth root, a CT should be mandatory to define all of these variables and to obtain true informed consent from the patient and to correctly programme the surgery to reduce the risk of nerve damage.
References
Umar G, Bryant C, Obisesan O, Rood J P . Correlation of the radiological predictive factors of inferior alveolar nerve injury with cone beam computed tomography findings. Oral Surg 2010; 3: 72–82.
Tay A B, Zuniga J R . Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg 2007; 36: 922–927.
Szalma J, Lempel L, Jeges S, Szabó G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 294–302.
Susarla S M, Dodson T B . Risk factor for third molars extraction difficulty. J Oral Maxillofac Surg 2004; 62: 1363–1371.
Sedaghatfar M, August M A, Dodson T B . Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg 2005; 63: 3–7.
Kjølle G K, Bjørnland T . Low risk of neurosensory dysfunction after mandibular third molar surgery in patients less than 30 years of age. A prospective study following removal of 1220 mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 411–417.
Jerjes W, Upile T, Shah P, Nhembe F, Gudka D, Kafas P et al. Risk factors associated with injury to the inferior alveolar andlingual nerves following third molar surgery - revisited. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 335–345.
Queral-Godoy E, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 259–264.
Blondeau F, Daniel N G . Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Ass 2007; 73: 325–325e.
Rood J P, Shebab B A . The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 1990; 28: 20–25.
Smith WP . The relative risk of neurosensory deficit following removal of mandibular third molar teeth: the influence of radiography and surgical technique. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115: 18–24.
de Melo Albert D G, Gomes AC, do EgitoVasconcelos B C, de Oliveira e Silva E D, Holanda G Z . Comparison of orthopantomographs and conventional tomography images for assessing the relationship between impacted lower third molars and the mandibular canal. J Oral Maxillofac Surg 2006; 64: 1030–1037.
Tantanapornkul W, Okouchi K, Fujiwara Y et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 253–259.
Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Inferior alveolar damage after lower third molar surgical extraction: A prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 377–383.
Nakagawa Y, Ishii H, Nomura Y et al. Third molar position: reliability of panoramic radiography. J Oral Maxillofac Surg 2007; 65: 1303–1308.
Nakamori K, Fujiwara K, Miyazaki A et al. Clinical assessment of the relationship between the third molar and the inferior alveolar canal using panoramic images and computed tomography. J Oral Maxillofac Surg 2008; 66: 2308–2313.
Gomes A, Vasconcelos E B, Silva O E, Caldas F, Neto I . Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg 2008; 66: 256–259.
Jhamb A, Dolas R S, Pandilwar P K, Mohanty S . Comparative efficacy of spiral computed tomography and ortopantomography in preoperative detection of relation of inferior alveolar neurovascular bundle to the impacted mandibular third molar. J Oral Maxillofac Surg 2009; 67: 58–66.
Momen A . Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg 2010; 68: 74–82.
Leung Y Y, Cheung L K . Correlation of radiographic signs, inferior dental nerve exposure, and deficit in third molar surgery. J Oral Maxillofac Surg 2011; 69: 1873–1879.
Kim J-W, Cha I-H, Kim S-J, Kim MR . Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg 2012; 70: 2508–2514.
Hasegawa T, Ri S, Umeda M, Komori T . Multivariate relationships among risk factors and hypoesthesia of the lower lip after extraction of the mandibular third molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 111: e1–e7.
Jerjes W, Swinson B, Moles D R et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: e1–e7.
Renton T, Hankins M, Sproate C, McGurk M . A randomised controlled clinical trial to compare the incidence of injury to the ID nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg 2005; 43: 7–12.
Dolanmaz D, Yildirim G, Isik K, Kucuk K, Ozturk A . Preferable technique for protecting the inferior alveolar nerve: coronectomy. J Oral Maxillofac Surg 2009; 67: 1234–1238.
Pippi R . A case of inferior alveolar nerve entrapment in the roots of a partially erupted mandibular third molar. J Oral Maxillofac Surg 2010; 68: 1170–1173.
Maegawa H, Sano K, Kitagawa Y et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 639–646.
Monaco G, Montevecchi M, Bonetti G A, Gatto M R, Checchi L . Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 2004; 135: 312–318.
Bundy M J, Cavola C F, Dodson T B . Panoramic radiographic findings as predictors of mandibular nerve exposure following third molar extraction: Digital versus conventional radiographic techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: e36–e40.
Susarla M, Dodson B . Preoperative computed tomography imaging in the management of impacted mandibular third molars. J Oral Maxillofac Surg 2007; 65: 83–88.
Ueda M, Nakamori K, Shiratori K et al. Clinical significance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral Maxillofac Surg 2012; 70: 514–520.
Sanmartí-Garcia G, Valmaseda-Castellón E, Gay-Escoda C . Does computed tomography prevent inferior alveolar nerve injuries caused by lower third molar removal? J Oral Maxillofac Surg 2012; 70: 5–11.
Pippi R . Evaluation capability of surgical difficulty in the extraction of impacted mandibular third molars: a retrospective study from a post-graduate institution. Ann Stomatol (Roma) 2014 Mar 31; 5: 7–14.
Giuliani A, Ghirardi O, Caprioli A, Di Serio S, Ramacci M T, Angelucci L . Multivariate analysis of behavioral aging highlights some unexpected features of complex systems organization. Behav Neural Biol 1994; 61: 110–122.
Bruce R A, Frederickson G C, Small G S . Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc 1980; 101: 240–245.
Tay A B, Go W S . Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg 2004; 62: 592–600.
Chuang S K, Perrott D H, Susarla S M, Dodson T B . Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg 2007; 65: 1685–1692.
Chiapasco M, Crescentini M, Romanoni G J . Germectomy or delayed removal of mandibular impacted third molars: the relationship between age and incidence of complications. J Oral Maxillofac Surg 1995; 53: 418–422 ; discussion 422–423.
Susarla M, Sidhu K, Avery L, Dodson B . Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg 2010; 68: 1296–1303.
Nakayama K, Nonoyama M, Takaki Y et al. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg 2009; 67: 2587–2591.
Ghaeminia H, Meijer G J, Soehardi A, Borstlap W A, Mulder J, Berge S . Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg 2009; 38: 964–971.
Acknowledgements
The present study was approved by the local Ethical Committee with the protocol number 987/12. All authors have viewed and agreed to the submission.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Pippi, R., Santoro, M. A multivariate statistical analysis on variables affecting inferior alveolar nerve damage during third molar surgery. Br Dent J 219, E3 (2015). https://doi.org/10.1038/sj.bdj.2015.661
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.661
This article is cited by
-
Risk stratification against inferior alveolar nerve injury after lower third molar extraction by scoring on cone-beam computed tomography image
Odontology (2020)
-
A multivariate statistical analysis on variables affecting inferior alveolar nerve damage during third molar surgery
British Dental Journal (2015)