Key Points
-
Highlights the need for research to be undertaken in primary dental care.
-
Provides examples of clinical research which is being undertaken in the primary care dental services.
-
Introduces some of the regulatory issues and enablers to implementing clinical research in primary care.
Abstract
Many commissioning bodies for research expect that researchers will actively involve the public and patients in their projects. The National Institute for Health Research (NIHR), for example, involves members of the public in reviewing funding applications and making recommendations about research funding. The NIHR's portfolio is currently operating in 97% of NHS Trusts and this now includes research sited in primary dental care. This paper presents some case studies of these and other projects which are designed specifically for patient benefit in dental services in the community. This means there is no necessity to translate the outcomes of such research from a university or hospital base to the general population as the projects are undertaken in dental practices that provide primary dental care to (predominantly) NHS patients. The relevance of the outcomes to dental care is, therefore, likely to be of direct interest and importance to commissioners of healthcare funding in the UK who have a duty to use evidence bases for commissioning decisions.
Similar content being viewed by others
Introduction
There is a growing recognition that dental practices in the primary care NHS sector provide an excellent environment to carry out clinical dental research and an opportunity for all members of the dental team to develop and expand their roles into the research field. In addition, it is mandated in the NHS Constitution that 'all patients should be offered the opportunity to be involved in research' and this should extend to dental patients as well.1 This is, of course, an eminently logical development so as to identify the benefit of new developments, treatments and management philosophies that may ultimately be adopted by the team and delivered in primary care. Only when both the care providers and their patients are involved in projects will crucial aspects of research be evaluated successfully. For example, in addition to evaluating treatment outcomes, the practicality, feasibility, acceptability, expense and cost-effectiveness of a new treatment regimen are crucial to its overall deliverability in NHS dentistry.
The mission of the National Institute for Health Research (NIHR) is to provide a health research system in which the NHS supports leading-edge research focused on the needs of patients and the public.2 In achieving this mission, the Institute's aims are to increase the opportunities for patients and the public to participate in, and benefit from, research and to promote and protect the interests of patients and the public in health research.3 These are commendable statements with a strong emphasis on the involvement of both the public and patients in research. With 23,000 dentists providing just under than 40 million courses of NHS treatment to 30 million patients in 2012–13, it is clear to see that there is an immense opportunity for dental research to expand into primary care.4
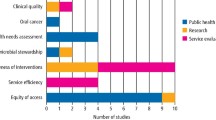
The aims of the paper are firstly to provide a brief overview of some of the dental research being undertaken in primary care and then to outline some of the important regulatory issues and other requirements that may need to be in place in order to undertake clinical dental research in the UK, as well as the support and enablers available.
Case studies of primary dental care research
DEEP (Developing effective and efficient care pathways in chronic pain)5
Chronic orofacial pain (COFP) is a relatively common problem in the UK where pain affects the face or mouth and lasts longer than three months. Healthcare professionals can be uncertain how to diagnose and manage the condition and sufferers experience negative impacts in their everyday lives because of it. Patients may undergo multiple referrals between different health professionals in an attempt to secure successful management.
This project aims to identify, from both patient and financial perspectives, where and how changes can be made to the way patients with COFP are managed in the NHS and then to suggest potential new and improved care pathway(s) for COFP. The new pathway(s) will be based on improving the quality of life of sufferers, decreasing their pain and providing efficiency for the patient and the NHS.
Data collection for this longitudinal study uses both quantitative and qualitative methods, and the cohort of patients is surveyed at regular, predefined intervals with a set of four questionnaires in order to capture the effects of their individual care pathway on their pain, quality of life and illness perspective. A subsample of the population will be invited to participate in sequential qualitative semi-structured interviews at baseline, 12 and 24 months.
FiCTION (Filling children's teeth: Indicated or not?)6
Dental decay, being one of the most common diseases of childhood, has a large health and economic impact. Although conventional clinical opinion is that carious primary teeth should be restored the majority of cavities in young children remain unrestored and there is, as yet, no conclusive evidence for the most effective approach to managing decay in primary teeth. FiCTION is funded by the NIHR Health Technology Assessment (HTA) programme and aims to provide that evidence by means of a randomised controlled trial (RCT). The results of this multi-centre, pragmatic RCT will provide evidence for the most clinically-effective and cost-effective approach to managing caries in children's teeth in primary care by comparing conventional restorations with biological management of caries and with prevention without restorations.
The chief investigators are Professor Jan Clarkson and Dr Nicola Innes (Dundee), Professor Gail Douglas (Leeds) and Professor Anne Maguire (Newcastle) with collaborators at universities in Cardiff, Glasgow, London and Sheffield. Clinical lead centres in Cardiff, London, Newcastle, Scotland and Yorkshire have recruited and trained 68 dental practices who are 'live' and recruiting patients between 3 and 7 years with at least one primary molar where caries extends into the dentine. The trial aims to recruit 1,113 children in total. Children taking part in the trial are randomised and treated according to one of three treatment arms: conventional plus best practice prevention; biological plus best practice prevention; and best practice prevention alone. This multi-disciplinary research team has been established to work alongside a UK-wide team of specialist paediatric and primary care dentists and dental teams.
Recruited practices screen patient lists to identify potentially eligible patients who are then invited to take part in the trial. Recruited participants and their parents complete questionnaires at every visit to the dental practice recording quality of life and self-efficacy data. Follow up lasts up to three years.
IMPACT
IMPACT is a care-based study investigating a relatively unexplored area within healthcare by looking at whether actually taking part in a randomised controlled trial (FiCTION) in primary care impacts on a parent's dental anxiety, oral health related-quality of life and attitude towards dental care and that of their children. IMPACT has recruited parents whose children are participating in the FiCTION Trial (as well as some parents whose children are not participating in FiCTION) from each participating dental practice in Scotland and North-East England. Parents are followed up for 18 months. The study is being funded by Newcastle University and NHS Education for Scotland (through the Scottish Dental Practice Based Research Network).
INTERVAL (Investigation of NICE technologies for enabling risk-variable-adjusted-length dental recalls trial)7
INTERVAL is a parallel group RCT taking place in dental practices throughout the UK. It has been commissioned by the NIHR HTA programme and the lead centre is the Dental Health Services Research Unit (DHSRU) at the University of Dundee.
Traditionally dentists recommend 6-monthly check-ups for patients although there is little evidence available to either support or refute this practice, or to provide advice to patients or dentists as to the best dental recall interval for the maintenance of oral health for adults. The purpose of INTERVAL is to investigate and compare the effect of three different arrangements for the timing of dental check-up recall intervals on adults' oral health:
-
6-month recall interval
-
Risk-based recall interval based on the patient's risk of dental disease
-
24-month recall interval.
Two thousand seven hundred and thirty-two participants have been recruited from 53 dental practices across the UK, from London and Cardiff in the south, up to Wick in the North of Scotland, and Belfast. The target is 52 patient participants per practice. The trial has recruited dental practices in varying locations including urban and rural practices and both fluoridated and non-fluoridated areas.
Participants receive an annual questionnaire to obtain quality of life and self-efficacy data. The primary outcome is measurement of disease (periodontal and caries) assessed at four years by blinded outcome assessors.
IQuaD (Improving the quality of dentistry)8
IQuaD has been commissioned by the NIHR HTA programme, and is being undertaken in Scotland and the North East of England. The lead centre is the Dental Health Services Research Unit at the University of Dundee. The study will provide much needed and robust evidence on the relative effectiveness of different types of oral hygiene advice and scale and polish.
IQuaD is a 5-year, multi-centre, randomised, controlled, open trial comparing oral hygiene advice and periodontal instrumentation for the prevention of periodontal disease in adults attending primary dental care.
Sixty-three NHS dental practices have recruited 1,877 adult patients who have been randomised to receive either routine or personalised oral hygiene advice to patients. The routine advice aligns to current practice for the care providers, whereas personalised advice is based on an individualised assessment for the patient. Additionally, in order to test the effectiveness and cost-effectiveness of a scale and polish, each patient has been randomised to one of three groups: no scale and polish; 6-monthly; or 12-monthly scale and polish. The patients are followed through the trial for 3 years and the primary outcomes for the study are gingival inflammation and measures of plaque control, as well as economic measures including 'willingness-to-pay' for treatment, costs to the NHS and costs to the patients. Questionnaires are being used to assess a profile of patient-centred outcomes including dental quality of life, oral health behaviours and knowledge of dental treatments, and to gain information of the clinicians' beliefs relating to the effectiveness of oral hygiene advice and the maintenance of periodontal health.
The design of this pragmatic trial necessitated a coordinated approach between the practices and the local, clinical research teams (outcome assessors). The protocol for the study was introduced to the dental practices at training sessions at which the recruitment procedures, the trial paperwork, randomisation procedures and the interventions were also discussed in detail. The practice staff then identified potential patients who were invited to a screening appointment to further assess eligibility, provide consent, complete questionnaires and undergo baseline clinical measurements by the outcome assessors before having an examination by the practice dentist, and a scale and polish from the practice hygienist.
Some of the feedback that we have received from dentists and dental care professionals who have participated in these primary care research projects is shown in Table 1.
Regulatory considerations for clinical research in primary care
This can be a confusing environment for researchers with a wealth of different terminologies. This section sets out as a guide to aid you.
Terminology
A 'research site' is not defined according to the geographical location of research activities, but to an overarching organisation that is responsible for that research activity; it is the single organisation responsible for conducting the research at a particular locality. So when research is conducted at several NHS dental practices that are within one local area team region then this single organisation will normally be considered as the single research site.
In the UK the chief investigator for a project assumes the overall responsibility for the design, conduct and reporting of the trial which includes ensuring patient safety, proactively leading the research team and coordinating the interaction between the researchers and the appropriate regulatory bodies.9 In primary care research there are often multiple research sites around the UK and the chief investigator will then appoint a principal investigator at each research site to assume responsibilities at the local level. The principal investigator will also be the point of contact for each dental practice at that research site.
Ethical and research and development (R&D) reviews
The governance arrangements for research ethics committees9 stipulate that review by an NHS Research Ethics Committee is required for research projects involving:
-
Research participants identified from, or because of their past or present use of, services for which the UK Health Departments are responsible (including services provided under contract with the private or voluntary sectors), including participants recruited through these services as healthy controls
-
Research participants identified because of their status as relatives or carers of past or present users of these services; collection of tissue (that is, any material consisting of or including cells) or information from any users of these services, including those who have died within the last 100 years
-
Use of previously collected tissue or information from which the research team could identify individual past or present users of these services, either directly from that tissue or information, or from its combination with other tissue or information in or likely to come into their possession.
The primary purpose of this review is to ensure that the safety, dignity and rights of the research participants (dental patients) are protected and a favourable decision by just one committee is required. This is a particular advantage where there are multiple dental practices in multiple research sites across the UK.
Similarly, for research conducted in the NHS (or Health and Social Care (HSC) in Northern Ireland), NHS (or HSC) management permission (R&D approval) for each NHS/HSC research site must be obtained.10 This has, in the past been a time-consuming process although with network support, the time taken for study set-up has now reduced by 43% during the period 2013–14.11 There are now coordinated systems in place for NHS R&D review across the UK and the Health Research Agency is currently developing an assessment for implementing a single review of the ethical, R&D and legal aspects of research projects across the four nations.
Medicines and Healthcare Products Regulatory Agency (MHRA)
If the clinical trial involves the use of an investigational medicinal product (CTIMP) then the project will be covered by the EU Clinical Trials Directive and the Medicines for Human Use (Clinical Trials) Regulations 2004, a clinical trial authorisation is required and an application must be made to the responsible regulatory body, the MHRA.
Similarly, an application to MHRA is required where the study is a clinical investigation of a medical device undertaken by the manufacturer for CE marking purposes. Or when a CE-marked product has been modified or is to be used outside its intended purpose.
In dentistry, an example of a CTIMP would be an investigation of a new local delivery antimicrobial system for the treatment of periodontal disease and although the field of medical devices includes dental materials, dental equipment and dental implants, if it can be shown that the device to be researched is broadly comparable to one or more already on the market (for example, in terms of technology, performance, design, operation, biological safety, conditions of use and clinical purpose12), then clinical testing may not be necessary. For this reason, medical (dental) device studies are uncommon in dentistry.
Good clinical practice
A key requirement for those involved in clinical research is good clinical practice (GCP) training. The EU Clinical Trials Directive (2001/20/EC) states that:
'Good clinical practice is a set of internationally recognised ethical and scientific quality requirements which must be observed for designing, conducting, recording and reporting clinical trials that involve the participation of human subjects.'13 The Department of Health's Research governance framework for health and social care, however, extends this beyond clinical trials to all research involving patients.14 According to the Medical Research Council's Guidelines for good clinical practice in clinical trials: 'Each individual involved in conducting a trial should be qualified by education, training and experience to perform his or her respective task(s).'15
In practical terms this means that those involved in research within the NHS are required to undertake specific GCP training at regular intervals. GCP training is available from a number of providers as single-day workshops and online courses. Training covers many aspects of conducting clinical research including: relevant laws, frameworks and guidelines, responsibilities of those involved in research and safety reporting requirements. Some courses are tailored to different settings, for example, primary care or paediatric settings, and online refresher courses are available. Training is available free of charge for those working with an NIHR clinical research network (CRN) or on NIHR CRN portfolio studies. Within commercial medical research GCP training is expected to be completed every 2 years, while for non-commercial studies the frequency of training is dictated by individual NHS organisations.
Research passports
Research passports are a system for issuing researchers from higher education institutions (HEIs) with honorary research contracts or letters of access to allow them to conduct research within the NHS. The research passport provides evidence of appropriate training and qualifications (including GCP), criminal record disclosure and evidence of occupational health clearance. The research passport is signed off by human resources within a single NHS organisation and this is provided to all NHS organisations in which the researcher is working as evidence of pre-engagement checks. Individual NHS organisations will then issue either an honorary contract or letter of access to the researcher (depending on the type of research being conducted). Research passports can be study-specific or valid for multiple studies and last a maximum of 3 years. Although NHS employees may not require a research passport, they may still require a letter of access to carry out research within a different NHS organisation which can be obtained via an 'NHS-to-NHS confirmation of pre-engagements checks proforma'.
Support available to undertake research
To deliver the mission of the NIHR to increase the research activity, there is a plethora of support available. The NIHR has evolved 15 local clinical research networks (LCRNs) across England each with 30 specialities and a specific oral and dental health theme. This is lead nationally by Professor Jimmy Steele and has leadership in each of the 15 areas.16
To deliver the national objectives NIHR funding is required to pay for the service time in which dental practices use to enable research to be undertaken. In addition to research funding for the activities like data collection and analysis there is also service support cost funding available from the LCRN to dental practices. There is also support from the LCRN, or whatever partner organisations undertake the activities on their behalf to support the process through the regulatory requirements described previously.
Conclusion
Opportunities for the dental team and dental practices to take part in primary care research are likely to increase over the next few years as sponsors and funding bodies continue to recognise the importance of offering NHS patients in particular the chance to take part in research. It is apparent that such projects provide exciting and unique challenges for all those involved and particularly so for the patients who volunteer to take part.
Those readers who might be interested in participating in primary care dental research should visit the appropriate website for their clinical research network for England, Wales Scotland or Northern Ireland.17,18,19,20
References
Department of Health. The NHS Constitution. July 2015. Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/170656/NHS_Constitution.pdf (accessed August 2015).
The National Institute for Health Research. Mission of the NIHR. Available online at http://www.nihr.ac.uk/about/mission-of-the-nihr.htm (accessed August 2015).
The National Institute for Health Research. Patient and public involvement. Available online at http://www.nihr.ac.uk/funding/pgfar-patient-and-public-involvement.htm (accessed August 2015).
Health and Social Care Information Centre. NHS dental statistics for England: 2012/13. Available online at http://www.hscic.gov.uk/catalogue/PUB11625/nhs-dent-stat-eng-12-13-rep-v2.pdf (accessed August 2015).
DEEP Study website. DEEP study: Developing effective and efficient care pathways for patients with chronic pain. Available online at http://research.ncl.ac.uk/deepstudy (accessed August 2015).
FiCTION Study website. Available online at http://research.ncl.ac.uk/fictiontrial/ (accessed August 2015).
Interval Study website. NIHR HTA INTERVAL dental recalls trial. Available online at http://dentistry.dundee.ac.uk/nihr-hta-interval-dental-recalls-trial (accessed August 2015).
IQuaD Study website. Available online at https://w3.abdn.ac.uk/hsru/IQuaD/ (accessed August 2015).
Department of Health. Governance arrangements for ethics committees: a harmonised edition (April 2012). Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213753/dh_133993.pdf (accessed August 2015).
NHS Health Research Authority. NHS/HSC R&D review or permission. Available online at http://www.hra.nhs.uk/resources/applying-for-reviews/nhs-hsc-rd-review/ (accessed August 2015).
Clinical Research Network Key Statistics for 2013–2014. Available online at http://www.crn.nihr.ac.uk/about-crn/our-performance/key-statistics-2/ (accessed August 2015).
Medicines and Healthcare Products Regulatory Agency. Clinical trials and investigations. Available online at http://www.mhra.gov.uk/Howweregulate/Devices/Clinicaltrials/index.htm#1 (accessed August 2015).
European Parliament (2001). Directive 2001/20/EC of the European Parliament and Council of 4 April 2001. Official Journal of the European Communities L121: 34–44.
Department of Health. Research Governance Framework for Health And Social Care. 2nd edition. 2005. Available online at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/139565/dh_4122427.pdf (accessed August 2015).
Medical Research Council. Guidelines for Good Clinical Practice in Clinical Trials. London: MRC, 1998. Available online at http://www.mrc.ac.uk/documents/pdf/good-clinical-practice-in-clinical-trials/ (accessed August 2015).
Clinical Research Network. About Oral and dental health research. Available online at http://www.crn.nihr.ac.uk/oral/about-oral-and-dental-health-research/ (accessed August 2015).
Clinical Research Network (England). Homepage. Online at http://www.crn.nihr.ac.uk/ (accessed August 2015).
Scotland's Clinical Research Networks. Homepage. Online at http://www.nhsresearchscotland.org.uk/317_Scottiish+Clinical+Research+Networks.html (accessed August 2015).
Regional Research Networks (Wales). Homepage. Online at http://www.wales.nhs.uk/sites3/page.cfm?orgid=580&pid=28571 (accessed August 2015).
Clinical Research Network (Northern Ireland). Homepage. Online at http://www.nicrn.hscni.net/category/nihr/clinical-research-network/ (accessed August 2015).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Heasman, P., Macpherson, L., Haining, S. et al. Clinical research in primary dental care. Br Dent J 219, 159–163 (2015). https://doi.org/10.1038/sj.bdj.2015.645
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.645