Key Points
-
Investigates the approach of restorative dentists towards the assessment and treatment planning of oral cancer patients in the UK.
-
Emphasises the variability in the approach to dental and oral rehabilitation of patients undergoing radiotherapy treatment for oral cancer patients.
-
Highlights the increased use of dental implants for post-surgery rehabilitation.
Abstract
Aims To investigate the approach of restorative dentists towards the assessment and treatment planning of oral cancer patients in the UK.
Material and methods The survey was conducted at the annual meeting of the Association of Consultants in Restorative Dentistry (ACSRD) and Specialist Registrar in Restorative Dentistry group (SRRDG) in September 2011. Delegates were requested to fill in a two-section questionnaire; the first section included 16 questions, evaluating cancer service provision in their units, and the second included five questions based on a clinical scenario evaluating dental management of a patient undergoing pre-radiotherapy treatment.
Results Ninety-four questionnaires were distributed; 65 (69.1%) were returned. Thirty (46.1%) respondents were consultants, 27 (41.5%) were specialist registrars and the remaining 8 (12.3%) were either specialist practitioners or trust grade dentists working in the speciality of restorative dentistry. Forty-eight (73%) of the respondents worked in NHS posts and the remaining 17 (27%) worked in academic posts. A total of 50 (77%) respondents carried out clinical work which regularly included the dental assessment or treatment of head and neck (H&N) oncology patients, before or post radiotherapy. Among the respondents who were involved in the dental assessment of oncology patients, 32% of them did not have a protocol for review appointments in their units. Ninety-one percent of respondents said that they used dental implants for rehabilitation post cancer surgery and 80% also used implants either always or sometimes in irradiated bone. Answers to scenario questions highlighted that all the respondents would extract very poorly prognostic tooth (that is, root stumps) before radiotherapy, irrespective of it being at the side of the planned radiotherapy field. Fifty-eight percent of respondents preferred to extract a non-functional, heavily restored, non-carious, distal maxillary molar tooth which was not in the area of radiotherapy beam and the majority (84%) chose to carry out root canal treatment (RCT) of a functional premolar tooth if considered non vital.
Conclusion This study highlights the variability in the approach of clinicians in dental and oral rehabilitation of patients undergoing radiotherapy treatment for oral cancer patients.
Similar content being viewed by others
Introduction
Oral cancer is the 15th most common cancer in the UK, accounting for around 2% of all new cases.1 It is the 12th most common cancer among men in the UK, accounting for over 2% of all new cases of cancer in males.1 It is the 16th most common cancer among women, responsible for more than 1% of all new cases of cancer in females.1 In 2009, there were 6,236 new cases of oral cancer in the UK; 4,097 (66%) in men and 2,139 (34%) in women, giving a male: female ratio of 19:10. The crude incidence rate shows that there are more than 13 new oral cancer cases for every 100,000 males in the UK and around 7 for every 100,000 females.1
Calman-Hine was the first comprehensive cancer report to be produced in the UK, and set out seven principles (Table 1).2 Stemming from the Calman–Hine Report, the Department of Health commissioned a series of evidence-based improving outcomes guidance (IOGs) reports. The National Institute of Health and Clinical Excellence improving outcome guidelines manual (NICE-IOG) for head and neck cancer was published in 2004. The aim was to facilitate the standardisation of head and neck cancer services which had previously been delivered in a widely heterogeneous way.3 Clinical guidelines for the oral management of oncology patients requiring radiotherapy, chemotherapy and/or bone marrow transplantation require a designated permanent member of dental staff, who is responsible for organising oral care both at the pre-treatment assessment and acute phase of cancer therapy.4 A national survey of oral and maxillofacial surgeons' attitudes towards the treatment and dental rehabilitation of oral cancer patients highlighted a growth in multidisciplinary team working but also showed variation in the utilisation of care team members across trusts and specialties. In particular, there was a significant discrepancy in utilisation of restorative team members and how and at what level they input into the care of head and neck oncology patients.5 The SIGN, NICE, Royal College of Surgeons and Calman-Hine guidelines outline the need for a restorative dentistry consultant as part of the multidisciplinary team care (MDT) but the above survey showed that the perceived ideal of a fully integrated consultant in restorative dentistry present on the multidisciplinary team was recorded in only 30% of their responses.5 Further to this multidisciplinary management guidelines for head and neck (H&N) cancer patients (produced jointly by the British Association of Head and Neck Oncologists, British Association of Plastic Reconstructive and Aesthetic surgeons, British Association of Oral and Maxillofacial surgeons, British Association of Otorhinolaryngology - Head and Neck Surgery and British Association of Endocrine and Thyroid Surgeons) outlined the importance of a consultant in restorative dentistry/oral rehabilitation within the head and neck cancer team because many patients face complex oral rehabilitation and dental health issues during and after their oncology treatment.6
Treatment for head and neck cancer may involve surgery, chemotherapy and radiotherapy which can cause adverse short- and long-term oral side effects. Osteoradionecrosis (ORN) of the mandible is a well-recognised late complication following high-dose radiotherapy (RT) for head and neck cancer. Its aetiology has been described in landmark studies by Dr Robert Marx, who introduced the principle of the '3 H's,' namely: hypocellularity, hypovascularity, and hypoxia.7 The reported incidence of mandibular ORN after high-dose RT is variable, ranging from approximately 5% to 15%.8,9 Pathological studies have demonstrated that RT-induced changes in the mandibular vasculature can result in a significant decrease in the blood flow to the mandible, perhaps partially explaining the mandible's increased susceptibility to ORN.10 Although the maxilla is often exposed to high doses of RT, it is probably less vulnerable to ORN than the mandible, possibly due to collateral circulation.11
As part of the pre-treatment evaluation, dentate patients with head and neck cancer are ideally evaluated by a restorative specialist before beginning RT. The condition of the teeth in the treatment field is assessed to determine the likelihood of requiring post treatment extractions because of the possible progression of dental disease over the patient's anticipated remaining lifetime. Depending on individual circumstances, teeth displaying advanced decay or periodontal disease, or those with signs of dental disease are usually extracted before RT, and treatment is postponed two to three weeks to allow for adequate healing. By removing these teeth while the healing capacity of the bone is normal, it is thought that the risk of delayed healing and ORN will be reduced.12,13,14
In light of the above guidelines and the fact that there have been no prior UK studies to assess the approach of restorative dentists in management of H&N oral cancer patients, this study was carried out to primarily investigate the approach of restorative dentists in the treatment and dental rehabilitation of oral cancer patients in the UK.
Methods
A questionnaire survey was conducted at the annual meeting of Association of Consultants in Restorative Dentistry (ACSRD) and Specialist Registrar in Restorative Dentistry group (SRRDG) in 2011 (Appendices 1 and 2). The delegates were requested to fill in the questionnaire and hand it back after completion. The questionnaire involved two sections; the first section included 16 background close-ended questions evaluating cancer service provision in the units nationally. The second section of the questionnaire included five questions based on a clinical scenario evaluating the dental management of a patient undergoing pre-radiotherapy treatment. The clinical scenario reflected a patient previously seen at the Birmingham Dental Hospital for radiotherapy assessment.
As the annual meeting involved mainly restorative dentists, either in training or consultants, it was considered that an overview of their approach in management of H&N oral cancer patients would be obtained.
Results
A total 94 questionnaires were distributed, of which 65 were returned (response rate 69.1%). Of this, 30 (46.1%) of the respondents were consultants or senior lecturers, 27 (41.5%) were specialist registrars and the remaining 8 (12.3%) were either specialists or trust grade dentists working in restorative dentistry speciality. Among the specialist trainees, 11 were in their fifth year of training, ten were in their fourth year of training, five in their third year of training and one in second year of training. Forty-eight (73%) of the total respondents worked in NHS posts and the remaining 17 (27%) respondents worked in academic posts. Figure 1 shows the distribution of responses to the question 'what's your main area of clinical interest?' within the restorative discipline. A total of 50 (77%) respondents carried out clinical work which regularly included the dental assessment or treatment of H&N oncology patients before or post radiotherapy, chemotherapy or surgical treatment. Out of the 15 respondents who did not carry out clinical work involving the H&N oncology patients, ten were consultants, three were trust grade doctors and two were specialist trainees in their third year of training. Among the ten consultants not involved in oncology work, four had periodontology, three had endodontics and the remaining four had prosthodontics as their main speciality within the restorative discipline.
Among the 50 respondents whose clinical work involved assessment and management of H&N oncology clinics, the majority 45 (90%) of them participated in either one to two sessions per week of oncology clinics. The remaining five (10%) were involved in more than two sessions. These were respondents who worked in district general hospitals and were all consultants. With regard to how many patients they would see on average per session, 48 (96%) see 3-6 patients per session and two respondents see more than six patients per session. The patients seen at the oncology pre-assessment clinics were referred mainly (95%) from a member of the MDT; Figure 2 shows the source of referral of patients to the restorative dentist for a pre-radiotherapy assessment. The respondents were varied in terms of where they worked, but the majority (65%) worked in a teaching dental hospital (Fig. 3 shows their distribution list). When asked if their pre-therapy oncology patients were seen in a multidisciplinary team clinic, all those who answered the question (45, 90% of total respondents) said yes but five of respondents (10%) left the question blank. When asked if there was a protocol for oncology patients to be reviewed following surgical or radiotherapy treatment, 16 (32%) respondents did not have a protocol for review appointments in their units. Among the ones who had a protocol; ten (20%) saw the patient within one month, 20 (40%) within 1-3 months after treatment and four respondents said it varied.
The results showed that either the restorative dentist or surgeon placed dental implants in their units (Fig. 4). Among the respondents, 91% use dental implants in rehabilitation of post cancer surgery and 80% said they used implants either always or sometimes in irradiated bone. Eighty-one percent of respondents have used CT guided technology in planning for dental implants (Fig. 5). When asked about the regular use of hyperbaric oxygen therapy (HBO) for patients who have undergone radiotherapy requiring dental implants, none of the respondents said they used it routinely, 25% have used it in the past or might consider using it in future if the implants were planned for the mandible in areas covered by radiotherapy field.
Clinical scenario (Appendix 2)
Response to questions on clinical scenario:
-
1
Would you recommend pre-radiotherapy extractions for this patient?
-
2
All the 65 returned questionnaires from respondents said yes they would recommend extractions. Figure 6 shows the percentage distribution in terms of the choice of tooth/teeth/root for which extraction would be recommended by the respondents.
-
3
If the 14 tooth showed a negative response to a sensibility test, would you change your decision to extract the tooth if not done in question 1 response?
-
4
Among the 72% who chose not to extract the tooth previously, 71% were in favour of RCT and 29% chose to extract the tooth.
-
5
The 27 is non-functional tooth and also responds negatively to a thermal test, would you change your decision to extract the tooth if not done in question 1 response?
-
6
Among the 43% who chose not to extract previously, 70% of the respondents changed their decision to extract the tooth.
-
7
Following radiotherapy, considering that you did not extract the 45 before treatment. This tooth is now painful and has signs and symptoms of apical periodontitis. What would be your choice?
-
8
Among the 37% who chose not to extract the tooth previously, 84% still favoured root canal treatment over extraction, 10% preferred extraction following HBO and 6% opted for extraction under local anaesthetic without HBO.
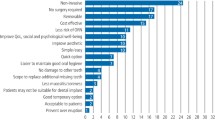
In response to what factors are thought important in making the decision of either extraction or non-extraction of tooth or teeth in irradiated bone: the majority (94%) considered risk of ORN (site and dose), followed by extension of caries in a tooth (81%), and then restorability of the tooth (76%). Patient's age (22%) and aesthetics (30%) were considered the least important factors in their decision-making (Fig. 7).
Discussion
Oral and dental assessment by the restorative dental specialist before cancer treatment is essential in order to effectively plan oral rehabilitation and dental management in patients whose oral cavity, teeth, salivary glands and jaws will be affected.3,4,5,6,15 It is important to include a consultant in restorative dentistry within the head and neck cancer team as many patients face complex oral rehabilitation and dental health issues during and after their oncology treatment.6 A previous survey of oral and maxillofacial surgeons highlighted that only 30% of the services (oncology MDT) nationally had an integrated restorative specialist involvement.5
Management of irradiated patients with cancer in the head and neck region represents a challenge for multidisciplinary teams. Radiotherapy promotes cellular changes and decrease in vascularity that results in a lower healing rate.7,14,16,17 Consequently, surgical procedures in irradiated tissues present with high rates of complication.18,19,20 Osteoradionecrosis (ORN) is the most severe sequelae caused by radiotherapy.16 It is associated with previous extractions especially those carried out post-irradiation.16 It has long been thought that pre-radiotherapy extraction of teeth in poor condition within the high-dose volume area would reduce the risk of ORN.21 This hypothesis has been extended to patients with teeth in fair to good condition who have a good chance of a cure and long life expectancy, particularly when the likelihood of maintaining the health of their teeth is thought to be questionable.16,21 Interestingly, a study to determine if pre-radiotherapy (pre-RT) dental extractions reduce the risk of ORN concluded that they appear not to.21 The authors of this study, however, recommended extraction of teeth in the proposed high-dose treatment field when they are in poor condition due to existing dental disease. However, teeth that are in fair to good condition, as determined by a restorative dentist, need not be prophylactically extracted before RT for the sole purpose of preventing future ORN, even if they are located in a proposed high-dose area.
Considering there are no clear guidelines, the decision to either extract or not extract a tooth at the pre-radiotherapy assessment of a tooth/teeth with not so obvious prognosis seems to be dependent on numerous factors which may include patient factor and their choice, site and dose of planned radiotherapy, potential future restorative plan, and the clinicians own preference and expertise within the discipline of restorative dentistry. It is often subjective based on their judgement. Hopefully, it follows through dialogue with the patient allowing informed choice in which risks and benefits of treatment options, and subsequent strategies of replacement if necessary, are discussed.
This survey set out to ascertain the approach of restorative dentists in the treatment and dental rehabilitation of oral cancer patients in the UK. The intention was to target the cohorts at the annual national conference which the majority of the restorative trainees and consultants attend. An initial response rate of 69% was considered high and therefore no follow up was done. The response was varied in terms of level of expertise with an almost equal percentage of consultants (46.1%) and specialist trainees (41.5%). It was also varied in terms of where the respondents worked (65% in teaching dental hospital or 34% in district general hospital). Seventy-three percent of respondents were based in the NHS and the remaining 27% were academic staff members. Twenty-three percent of respondents carried out no clinical work which regularly included the dental assessment or treatment of head and neck (H&N) oncology patients and among them 86% were either academic consultants or trust grade dentists.
The patients seen at the oncology pre-assessment clinics were referred mainly from a member of the MDT (95%). Pre-therapy oncology patients were seen at the MDT (90%) and 68% of respondents said that they had a protocol for review for these patients following surgical or radiotherapy treatment. These factors suggest that there is higher involvement and representation of restorative dentistry as a speciality in MDT care compared to the 30% response in the national maxillofacial surgeons survey carried out two years previously. The question as to whether or not they were part of the MDT was not asked in the questionnaire, as it was not the intention of this survey to evaluate this.
The use of dental implants in the reconstructive phase of treatment was undertaken at their units by over 91% of the respondents, out of which 60% said both the surgeons and restorative dentists were placing implants. Dental implants allow effective oral and facial rehabilitation following cancer treatment including radiotherapy. They are used to support oral or facial prostheses. The increase in implant usage at the restorative phase of H&N oral cancer patients is perhaps due to the increased involvement of restorative dentists in the MDT and the increased availability of training in implant placement for restorative dentistry trainees. Other factors include guidelines identifying oncology patients as priority groups for implant rehabilitation.22,23
A high percentage of respondents (80%) also used implants in irradiated bone. This is possibly due to the fact that dental implant placement into irradiated jaws is a successful treatment modality.6,24 However, the success rates reported in various studies are lower than in non-irradiated bone.25,26,27 High success rate of osseointegration of dental implants has been reported in cases when implants are placed pre-radiotherapy (97%) and post radiotherapy (97.9%). However, implants placed in irradiated bone in general should be always approached with caution as there is evidence to support a slightly reduced success rate comparing to a non-irradiated bone.28,29
In this survey, none of the respondents said they used HBO therapy routinely; however, 25% had used it in the past or would consider in future if the implants were planned for the mandible and the radiotherapy field was in line with the planned implant placement. The use of HBO before implant treatment is a controversial area with no clear-cut evidence supporting for or against. A study (randomised controlled trial) looking at a treatment to prevent jaw bone damage in head and neck cancer (HOPON) is ongoing, supported by Cancer Research UK. In the literature there is evidence supporting the use of HBO before dental implant placement, as implant placement in irradiated bone is associated with a higher failure rate and adjuvant HBO therapy can reduce the failures.30,31,32 Similarly there is evidence not supporting the use of HBO for dental implant placement.33,34,35,36 The conclusion of the systematic review, with consideration to the limited amount of research available, is that (HBO) therapy in irradiated patients requiring dental implants may not offer any appreciable clinical benefits.36
A high proportion (81%) of respondents had used CT guided technology in their planning for implant treatment. CT guided technologies in implant dentistry have expanded with the concepts of a team approach to the planning and placement of dental implants. Recent advances in this technology have revolutionised treatment and created an interdisciplinary environment in which communication can lead to better patient care and outcomes.37
Clinical scenario response
Based on the scenario, in response to the question on which tooth or teeth would they recommend extracting, all the respondents recommended extraction of at least one tooth. This was not surprising considering there was a remaining root stump (37) with a hopeless prognosis. The response with regard to which teeth they would recommend extracting was varied. Excluding the obvious 37 root stump from the equation, the majority (63%) opted to extract the 45 that showed extensive radiographic signs of caries. There could be numerous reasons for this: an unrestorable tooth due to extensive caries; tooth in line of planned radiotherapy field; and a mandibular tooth increasing the chance of ORN if this tooth does fail and would require extraction in future following radiotherapy.21,38,39,40 Out of the 37% who chose not to extract the tooth, when asked if they would reconsider their option if the tooth following radiotherapy were to be non-vital and showed signs and symptoms of apical periodontitis; 84% favoured root canal treatment over extraction. This may be because post-irradiation dental extraction has generally been considered a potentially hazardous procedure.14,41 Murray and co-workers found that seven out of eight patients who had post-irradiation extractions were subsequently affected with ORN.13 Similarly Morrish et al. also found 11 out of 18 patients suffered with ORN following extraction in irradiated jaw.42 Beumer et al. reported a 22% incidence of bone exposure for three months or longer in 72 post-radiation extraction episodes.41 They reported that the mandible sustained a significantly higher risk of ORN than the maxilla (29% versus 11%); the risk was further increased when the radiation dose exceeded 65 Gy and the treatment volume covered not less than 75% of the body of the mandible.41 The authors concluded that in view of the undesirably high rate of ORN, root canal therapy was preferable to dental extraction in the management of dental infection after radiotherapy.41 Epstein et al. compared the incidence of ORN in relation to extractions before and after radiotherapy. They were able to demonstrate a higher risk in post-irradiation extraction than pre-irradiation extraction, which was in accordance with the results reported by Beumer et al.14 Contrary to this Koga et al. showed only three cases of ORN in 1,647 extractions in 316 patients and concluded that there is low prevalence of ORN suggesting the possibility of performing extractions after radiotherapy by experienced dentists.16 A systematic review looking at the incidence and the factors influencing the development of ORN after tooth extraction in irradiated patients showed the total incidence of ORN of only 7%. In this review 19 papers were selected and the authors concluded that while the incidence of ORN after post-radiotherapy tooth extractions is low, the extraction of mandibular teeth within the radiation field in patients who received a radiation dose higher than 60 Gy represents the highest risk of developing ORN.43
In this study, for those who chose to extract the 45 tooth, 10% preferred extraction following HBO and 6% opted for extraction under LA without HBO. This alludes to the fact that there is no clear evidence to support the use of HBO before extraction of tooth in irradiated bone and whether this therapy would reduce risk of ORN. There are studies in favour of HBO use before dental extractions supporting potential benefit of HBO therapy.44,45 Contrary to this, there are numerous studies including two systematic reviews not in favour of HBO therapy before dental extractions.46,47,48,49 A systematic review suggested that based on weak evidence; prophylactic use HBO therapy is effective in reducing the risk of developing ORN after post-radiation extractions.43 Similarly a Cochrane review concluded that for people with late radiation tissue injury affecting tissues of the head and neck, HBO therapy is associated with improved outcome and appears to reduce the chance of ORN following tooth extraction in an irradiated field.50 The application of HBO therapy to selected patients and tissues may be justified.50
The radiographic picture (OPG) of the clinical case showed that the 14 tooth is heavily restored but with no clinical or radiographic signs of pathology. Considering this, 28% still chose to extract this tooth pre-RT. The reason could be that this tooth is heavily restored which has a potential progressive sequelae of pulpal involvement that could ultimately render the tooth non-vital (apical periodontitis) subsequently requiring RCT or extraction. Among the 28% who chose to extract the tooth, all of them chose to also extract the 16 (heavily restored and carious) and 27 (heavily restored and non-functional) teeth, and 90% of these considered a shortened dental arch as an important factor compared to 63% overall in their decision-making of either extraction or non-extraction of tooth pre-RT treatment. Interestingly, among the 72% who chose not to extract the tooth, the majority (71%) still favoured RCT over extraction when asked what if the tooth was non-vital. These results highlight that there are two basic types of clinician. One who tends to prefer extraction, which may be based on a cautious approach in view of the potential risk of ORN, and the difficulties in its management, irrespective of the jaws involved and would consider extraction of tooth with questionable prognosis. The other type is more conservative and would consider RCT of a tooth with questionable prognosis. This may also be due to the fact that they may have more experience and expertise in carrying out the RCT procedure or additionally may feel that retention of teeth long term may improve function and avoid future removable denture wear.
The 27 tooth is a non-functional tooth, non-carious, heavily restored and not in line of radiotherapy field. More than half (57%) opted to extract the tooth pre-RT and among the 43% who chose not to, 70% of them changed their decision to extract the tooth when told the tooth was not vital. The reason could be that with no opposing tooth in the lower left quadrant; there is a potential for the 27 tooth to over erupt and cause potential occusal interference. A study on occlusal changes following posterior tooth loss in adults shows positional changes, which may alter arch forms and occlusal planes.51 This may result in the development of occlusal interferences.51 In one study extraction of all non-functional molars without opposing teeth was considered as the formation of food traps following over-eruption of these teeth results in root surface caries in contact areas that are difficult to manage.48 This study also recommended extraction of all second molars unless the patient is keen to maintain meticulously good oral hygiene and has demonstrated the ability to do so.48
This survey was solely intended to assess the response of restorative delegates at the Annual Restorative Conference. The majority of delegates comprised of consultants and specialist registrars in restorative dentistry representing both the NHS and academic environments. There is a large number of teaching hospital representatives 3:1 compared to district general hospitals, which has a potential for bias as although restorative dentistry is largely a teaching hospital speciality, most head and neck cancer treatment is delivered in district general hospitals. It was not the intention of the study to analyse the difference among the two groups as most trainees working at the teaching hospital nationally receive significant experience in head and neck oncology through their association with head and neck oncology units locally.
A recent Cochrane review on dental extractions before radiotherapy to the jaws for reducing post-radiotherapy dental complications highlighted that at present there are no randomised controlled trials to assess the effect of extracting teeth before radiotherapy compared to leaving teeth in the mouth during radiotherapy to the jaws.52 All studies resulting from the search were either cohort studies or quality-of-life questionnaires. The review failed to support or refute the extraction or non-extraction of healthy or diseased teeth before radiotherapy for the reduction of subsequent dental complications.
Conclusion
This study highlights the variability in the approach of clinicians in the dental and oral rehabilitation of patients undergoing radiotherapy treatment for oral cancer as there are no clear-cut guidelines available to assist restorative dentists in making decision for pre-radiotherapy extraction or non-extraction of teeth. The decision to extract a tooth before radiotherapy treatment depended mainly on the risk of ORN (site and dose of radiation) and in the absence of defined guidelines this is often based on clinical judgement, expertise of the clinician and patients' choice. Well-designed controlled trials are needed to establish good scientific evidence for or against any treatment modality.
There are various national clinical guidelines and reports that highlight the importance of a restorative dentist and its speciality support in multidisciplinary management of these H&N patients. Complex restorative rehabilitation of these patients is often needed to improve quality of life.
This study also highlights the increased use of dental implants for post-surgery rehabilitation and shows the different trends in which these implants are placed with increased use of CT guided technology.
References
Cancer Research UK. Oral cancer incidence statistics. Data from the Office for National Statistics; ISD Scotland; Welsh Cancer Intelligence and Surveillance Unit and Northern Ireland Cancer Registry. Cancer Research UK, 2011.
Haward R A . The Calman-Hine report: a personal retrospective on the UK's first comprehensive policy on cancer services. Lancet Oncol 2006; 7: 336–346.
National Institute for Health and Care Excellence. Improving outcomes in head and neck cancers - the manual. London: NICE, 2004.
Faculty of Dental Surgery of the Royal College of Surgeons of England. National clinical guidelines 2012. Restorative dentistry section: guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS. London: Royal College of Surgeons of England, 2012.
Alani A, Owens J, Dewan K, Summerwill A . A national survey of oral and maxillofacial surgeons' attitudes towards the treatment and dental rehabilitation of oral cancer patients. Br Dent J 2009; 207: E21.
Butterworth C, MaCaul L, Barclay C . Restorative dentistry/oral rehabilitation. In Paleri V (eds) Head and neck surgery head and neck cancer: multidisciplinary management guidelines. 4th ed. London: ENT UK, 2011.
Marx R E, Johnson R P, Kline S N . Prevention of osteoradionecrosis: a randomized prospective clinical trial of hyperbaric oxygen versus penicillin. J Am Dent Assoc 1985; 111: 49–54.
Balogh J M, Sutherland S E . Osteoradionecrosis of the mandible: a review. J Otolaryngol 1989; 18: 245–250.
Mendenhall W M . Mandibular osteoradionecrosis. J Clin Oncol 2004; 22: 4, 867–864.
Bras J, de Jonge H K, van Merkesteyn J P . Osteoradionecrosis of the mandible: pathogenesis. Am J Otolaryngol 1990; 11: 244–250.
Perrier M, Moeller P . Osteoradionecrosis. A review of the literature. Schweiz Monatsschr Zahnmed 1994; 104: 271–277.
Bedwinek J M, Shukovsky L J, Fletcher G H, Daley T E . Osteonecrosis in patients treated with definitve radiotherapy for squamous cell carcinomas of the oral cavity and naso and oropharynx. Radiology 1976; 119: 665–667.
Murray C G, Herson J, Daly T E, Zimmerman S . Radiation necrosis of the mandible: a 10 year study, Part 2: Dental factors, onset, duration and management of necrosis. Int J Radiat Oncol Biol Phys 1980; 6: 549–553.
Epstein J B, Rea G, Wond F L, Spinelli J, Stevenson-Moore P . Osteoradionecrosis: study of the relationship of dental extractions in patients receiving radiotherapy. Head Neck Surg 1987; 10: 48–54.
Scottish Intercollegiate Guidelines Network. Diagnosis and management of head and neck cancer: a national clinical guideline. Edinburgh: SIGN, 2006.
Koga D H, Salvajoli J V, Alves F A . Dental extractions and radiotherapy in head and neck oncology: review of the literature. Oral Dis 2008; 14: 40–44.
Johnson R P, Marx R E, Buckley S B . Hyperbaric oxygen in oral and maxillofacial surgery. In: Worthington P, Evans J R (eds) Controversies in oral and maxillofacial surgery. pp 107–126. Philadelphia: Saunders, 1994.
Glanzmann C, Gratz K W . Radionecrosis of the mandibula: a retrospective analysis of the incidence and risk factors. Radiother Oncol 1995; 36: 94–100.
Struder G, Gratz K W, Glanzmann C . Osteoradionecrosis of the mandibula in patients treated with different fractionations. Strahlenther Onkol 2004; 180: 233–240.
Store G, Boysen M . Mandibular osteoradionecrosis: clinical behaviour and diagnostic aspects. Clin Otolaryngol 2000; 25: 378–384.
Chang D T, Sandow P R, Morris C G, Hollander R, Scarborough L, Amdur R J, Mendenhall W M . Do pre-irradiation dental extractions reduce the risk of osteoradionecrosis of the mandible? Head Neck 2007; 29: 528–536.
Faculty of Dental Surgery of the Royal College of Surgeons of England. National clinical guidelines 2012. Restorative dentistry section: guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS. London: Royal College of Surgeons of England, 2012.
Assael L A . Dental implant education and practice in oral and maxillofacial surgery: 25 years of progress. J Oral Maxillofac Surg 2008; 66: 611–612.
Fenlon M R, Lyons A, Farrell S, Bavisha K, Banerjee A, Palmer R M . Factors affecting survival and usefulness of implants placed in vascularized free composite grafts used in post-head and neck cancer reconstruction. Clin Implant Dent Relat Res 2012; 14: 266–272.
Visch L L, van Waas M A, Schmitz P I, Levendag P C . A clinical evaluation of implants in irradiated oral cancer patients. J Dent Res 2002; 81: 856–859.
Granström G . Osseointegration in irradiated cancer patients: an analysis with respect to implant failures. J Oral Maxillofac Surg 2005; 63: 579–585.
Ihde S, Kopp S, Gundlach K, Konstantinović V S . Effects of radiation therapy on craniofacial and dental implants: a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 56–65.
Schepers R H, Slagter A P, Kaanders J H, van den Hoogen F J, Merkx M A . Effect of postoperative radiotherapy on the functional result of implants placed during ablative surgery for oral cancer. Int J Oral Maxillofac Surg 2006; 35: 803–808.
Wagner W, Esser E, Ostkamp K . Osseointegration of dental implants in patients with and without radiotherapy. Acta Oncol 1998; 37: 693–696.
Larsen P E, Stronczek M J, Beck F M, Rohrer M . Osteointegration of implants in radiated bone with and without adjunctive hyperbaric oxygen. J Oral Maxillofac Surg 1993; 51: 280–287.
Ueda M, Kaneda T, Takahashi H . Effect of hyperbaric oxygen therapy on osseointegration of titanium implants in irradiated bone: a preliminary report. Int J Oral Maxillofac Implants 1993; 8: 41–44.
Granström G, Tjellström A, Brånemark P I . Osseointegrated implants in irradiated bone: a case-controlled study using adjunctive hyperbaric oxygen therapy. J Oral Maxillofac Surg 1999; 57: 493–499.
Franzén L, Rosenquist J B, Rosenquist K I, Gustafsson I . Oral implant rehabilitation of patients with oral malignancies treated with radiotherapy and surgery without adjunctive hyperbaric oxygen. Int J Oral Maxillofac Implants 1995; 10: 183–187.
Keller E E, Tolman D E, Zuck S L, Eckert S E . Mandibular endosseous implants and autogenous bone grafting in irradiated tissue: a 10-year retrospective study. Int J Oral Maxillofac Implants 1997; 12: 800–813.
Andersson G, Andreasson L, Bjelkengren G . Oral implant rehabilitation in irradiated patients without adjunctive hyperbaric oxygen. Int J Oral Maxillofac Implants 1998; 13: 647–654.
Esposito M, Grusovin M G, Patel S, Worthington H V, Coulthard P . Interventions for replacing missing teeth: hyperbaric oxygen therapy for irradiated patients who require dental implants. Cochrane Database Syst Rev 2008; 23: CD003603.
Orentlicher G, Abboud M . Guided surgery for implant therapy. Oral Maxillofac Surg Clin North Am 2011; 23: 239–256.
McCaul L K, Jenkins W M, Kay E J . The reasons for extraction of permanent teeth in Scotland: a 15-year follow-up study. Br Dent J 2001; 23: 658–662.
Hull P S, Worthington H V, Clerehugh V, Tsirba R, Davies R M, Clarkson J E . The reasons for tooth extractions in adults and their validation. J Dent 1997; 25: 233–237.
Worthington H, Clarkson J, Davies R . Extraction of teeth over 5 years in regularly attending adults. Community Dent Oral Epidemiol 1999; 27: 187–194.
Beumer J III, Silverman S Jr, Benak S B Jr. Hard and soft tissue necroses following radiation therapy for oral cancer. J Prosthet Dent 1972; 27: 640–644.
Morrish R B, Chan E, Silverman S Jr, Meyer J, Fu K K, Greenspan D . Osteonecrosis in patients irradiated for head and neck carcinoma. Cancer 1981; 47: 1980–1983.
Nabil S, Samman N . Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: a systematic review. Int J Oral Maxillofac Surg 2011; 40: 229–243.
Lambert P M, Intriere N, Eichstaedt R . Management of dental extractions in irradiated jaws: A protocol with hyperbaric oxygen therapy. J Oral Maxillofac Surg 1997; 55: 268–274.
Chavez J A, Adkinson C D . Adjunctive hyperbaric oxygen in irradiated patients requiring dental extractions: outcomes and complications. J Oral Maxillofac Surg 2001; 59: 518–522.
Shaw R J, Sutton A F, Cawood J I et al. Oral rehabilitation after treatment for head and neck malignancy. Head Neck 2005; 27: 459–470.
Clayman L . Management of dental extractions in irradiated jaws: a protocol without hyperbaric oxygen therapy. J Oral Maxillofac Surg 1997; 55: 275–281.
Tong A C, Leung A C, Cheng J C, Sham J . Incidence of complicated healing and osteoradionecrosis following tooth extraction in patients receiving radiotherapy for treatment of nasopharyngeal carcinoma. Aust Dent J 1999; 44: 187–194.
Fritz G W, Gunsolley J C, Abubaker O, Laskin D M . Efficacy of pre-and postirradiation hyperbaric oxygen therapy in the prevention of postextraction osteoradionecrosis: a systematic review. J Oral Maxillofac Surg 2010; 68: 2653–2660.
Bennett M H, Feldmeier J, Hampson N, Smee R, Milross C . Hyperbaric oxygen therapy for late radiation tissue injury. Cochrane Database Syst Rev 2012; 5: CD005005.
Craddock H L . Occlusal changes following posterior tooth loss in adults. Part 3. A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. J Prosthodont 2008; 17: 25–30.
Eliyas S, Al-Khayatt A, Porter R W, Briggs P . Dental extractions before radiotherapy to the jaws for reducing post-radiotherapy dental complications. Cochrane Database Syst Rev 2013; 28: CD008857.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Dewan, K., Kelly, R. & Bardsley, P. A national survey of consultants, specialists and specialist registrars in restorative dentistry for the assessment and treatment planning of oral cancer patients. Br Dent J 216, E27 (2014). https://doi.org/10.1038/sj.bdj.2014.544
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.544
This article is cited by
-
The role of the clinical nurse specialist in head and neck cancer care
British Dental Journal (2022)
-
Wider consultation
British Dental Journal (2021)
-
A cross sectional study of dental implant service provision in British and Irish dental hospitals
British Dental Journal (2019)
-
The reconstructive oral cancer patient: what the general dental practitioner needs to know
British Dental Journal (2019)