Key Points
-
Describes the prevalence and aetiology of severe hypodontia.
-
Highlights the typical dental and craniofacial features seen in association with this condition.
-
Stresses the importance of multidisciplinary teamwork in the management of these patients.
-
Discusses conventional removable and fixed prosthodontic treatment options and the challenges that may be encountered.
Abstract
Severe hypodontia is the absence of six or more permanent teeth and is relatively uncommon (estimated prevalence of 0.1-0.2%). This condition may have considerable functional, aesthetic and psychological implications for the patient, as well as presenting a significant challenge for the restorative dentist. There are a number of additional dental and craniofacial features that are seen frequently in patients with severe hypodontia that may complicate the provision of restorative treatment. These patients typically present at a young age and are likely to require lifelong support from the dental team. Initially this may be limited to oral health education and delivery of effective preventative regimes in childhood. Where required, missing teeth may be replaced using conventional removable and fixed prosthodontics as well as implant retained restorations. This article, part one of a two-part series, deals with the assessment of patients and factors to consider when treatment planning for the provision of conventional restorative solutions in severe hypodontia.
Similar content being viewed by others
Introduction
Hypodontia is defined as the developmental absence of one or more teeth, which can affect both the primary and the permanent dentition. The prevalence of this is in the permanent dentition is estimated at 3.5-6% in a British population.1 Over 80% of patients with hypodontia present with the absence or one or two missing teeth.2,3 The absence of six or more teeth, defined as severe hypodontia or oligodontia, is much less common, with an estimated prevalence of between 0.1-0.2% in the general population.4,5
The aetiology of hypodontia is multifactorial, however, genetics are considered to have a key role. Tooth development is a complex process involving multiple genes, which are also implicated in the development of the craniofacial structures and structures of ectodermal origin.6 Mutations of these genes can therefore have wider effects and as a result hypodontia may occur as a feature of a number of syndromes including the ectodermal dysplasias (ED)5,6 and cleft lip and palate. Alternatively and more commonly, hypodontia may be an isolated finding, associated with lesser craniofacial or dental anomalies (Table 1). These associated features can complicate dental rehabilitation, especially in cases of severe hypodontia where they may be more pronounced and edentulous spans are longer.
It is likely that the majority of patients with severe hypodontia will require a range of treatment modalities over their lifetimes to address functional and aesthetic concerns. When the condition is identified, whether in childhood or adulthood, it is advisable to refer for a specialist advice and possible treatment.
Many severe hypodontia cases share similar clinical traits, however, it is important to treatment plan for each patient as an individual, considering the potential psychosocial impact of the condition as well as the more obvious functional and aesthetic issues.7,8 Patients do benefit from a multi-disciplinary team (MDT) approach, which usually includes paediatric dentistry, restorative dentistry, orthodontics and maxillofacial surgery as needed. They are likely to require the involvement of numerous clinicians, supporting the patient and their family from infancy to adulthood.
This article aims to outline the important factors in assessment (Table 2), treatment planning and also discuss treatment options with a particular focus on conventional restorations.
Considerations in severe hypodontia
Patient factors
Oral health and motivation
The patient's concerns and expectations of treatment are the most important driver for treatment. Complex treatment is likely to require attendance at numerous appointments over a lengthy period, as well as an ongoing commitment to the maintenance of oral health and repeat treatments in the future. It is important that the patient understands this long-term picture and is prepared to take responsibility for their oral health. Complex restorations will not be suitable for all, with a pragmatic approach to treatment planning being important to the long-term success of any intervention.
In general, severe hypodontia itself is not associated with a heightened caries risk unless it is seen as part of a syndrome, such as ED, of which xerostomia is a feature. Caries risk should be assessed considering the usual parameters with thorough history taking and clinical examination.9 The most useful indicator of future caries risk is previous caries experience.10 Other significant factors include socioeconomic group, oral health motivation both of the patient and parent, dietary control and optimal use of fluoride.11
Where there has been a high caries rate the use of a four-day diet diary may help to identify areas of potential concern.12 Advice with regard to fluoride and oral hygiene measures should be tailored for the individual and reviewed at follow up appointments.
Age
In the early years, the dental team in general dental practice or as part of a specialist paediatric dental unit, have a crucial role to play in the education of not only the patient, but also the parents. At this time, appropriate support and advice will lay the foundations for good oral health so that the primary dentition is maintained for as long as possible as this has been shown to have functional benefits.13
When patients are in the primary and mixed dentition, treatment should be kept minimal and depending on the patient's concerns it may be possible to avoid restorative intervention at this stage. Older children tend to become more conscious of their appearance and peer pressure; hence the demand for treatment increases14 and compliance for extensive dental treatment may also improve.
The placement of dental implants in children to retain prostheses is technically possible, however, as osseointegrated implants behave as ankylosed teeth, they may become infra-occluded if they are placed before cessation of craniofacial growth,15 rendering them non-functional or resulting in poor aesthetics. This may not be so important where patients are virtually edentulous, a situation common in ectodermal dysplasia,16 as where teeth are absent alveolar height does not change significantly with growth. The anterior mandible changes minimally from the age of eight years17 and hence two implants placed in the canine or lateral incisor regions may allow successful early rehabilitation. Although this is not a widely accepted treatment modality it is an area of emerging evidence.18
It should, however, be noted that late growth and gingival maturation may continue into adulthood, and this may affect implant restorations in the aesthetic zone where there are adjacent natural teeth.19
Dental factors
As for any patient for whom advanced restorative work is proposed, a good level of oral health is a prerequisite. A decision must be made as to which of the missing teeth need to be replaced for reasons of aesthetics, function, occlusal stability and oral comfort. In many cases it is not appropriate to restore all missing teeth and a shortened dental arch can be considered.20
Position and quality of teeth present
Where primary teeth are retained and have a reasonable prognosis, aesthetics may be improved significantly by the use of composite bonding.21 Various techniques for composite build-ups have been described, although with primary teeth care should be taken to control occlusal forces as functional overload may increase tooth mobility. In this way primary teeth can be utilised as part of either a conformative or reorganised approach and may provide useful function, often into middle age, with reasonable aesthetics (Fig 1).
a-d 19-year-old patient with severe hypodontia (13 missing permanent teeth and multiple retained primary teeth) following orthodontics; e-h Extraction of the LLD and replacement with a conventional bridge from the retained ankylosed primary LLE. Restoration with composite build ups to the upper central incisors and all remaining primary teeth
In severe hypodontia the few permanent teeth present are often found to be in aberrant positions, with small tooth size and unusual morphology. Orthodontics can be very useful in redistributing space within the arches to create realistic pontic spaces. It may also help realign ectopic or malpositioned teeth, close diastemas, level the occlusal plane and establish a favourable inter-radicular space for possible future implant placement. Creation of a more favourable interocclusal space and incisor overjet and overbite changes can also greatly facilitate restorative treatment. However, placing orthodontic brackets on microdont teeth can be very difficult and with multiple missing teeth securing sufficient orthodontic anchorage is challenging. This problem can sometimes be overcome with the placement of temporary anchorage devices,23 although these are not yet commonly used. Microdont teeth can be built up to a more desirable size and shape with composite before orthodontic treatment begins in order to facilitate placement of brackets and give the orthodontist a clearer idea of the exact space requirements to facilitate restorative treatment. Similarly, conical/pointed teeth can be recontoured carefully with rotary instruments before orthodontics.
In some circumstances teeth may have erupted into such an aberrant position that it is more expedient to consider their extraction rather than orthodontic realignment, although this needs careful assessment. Likewise, unerupted, ectopic teeth may be best left in situ, as their surgical removal may threaten the longevity of adjacent teeth or cause such destruction of the alveolar ridges that future restorative treatment is complicated further.
Anatomical factors
Skeletal pattern and soft tissue profile
It is common to see reduced lower face height14 in patients with severe hypodontia and some authors have reported a tendency towards a Class III skeletal pattern, which increases with the severity of the hypodontia.24 A reduction in lip protrusion, particularly of the upper lip has also been reported.25
It is important to assess these factors when planning restorative treatment as there may be a need to increase the lower face height and reorganise the occlusal scheme for both functional and aesthetic reasons. Careful bucco-lingual positioning of the prosthetic teeth relative to the alveolar ridges may help to disguise mild skeletal discrepancies, by providing more support for the facial soft tissues and hence improving the appearance. This is often more effective when a removable prosthesis is used as there is more flexibility to position the prosthetic teeth and use acrylic flanges to achieve the desired effects.
Bony anatomy and position of vital structures
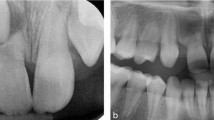
In severe hypodontia patients, the absence of permanent teeth results in restricted alveolar growth.26 As a result there may be insufficient bone for provision of dental implants. Even where primary teeth are retained and immediate implant placement is possible, there is often concavity of the alveolar process beyond the root apices, giving an 'hour glass' ridge morphology in cross section (Fig. 2).
The amount of bone and the position of key anatomical features should be assessed with appropriate imaging. In some cases, plain films may be adequate, however, where there is clinical doubt about local anatomy, three-dimensional imaging using a cone beam CT scanner is indicated.27 When taken with a radiographic stent based on planned tooth position in situ, these images can provide detailed information about bone availability at potential osteotomy sites28 and relate the site to anatomical features of note. In the maxilla these include the maxillary sinuses, the floor of the nose and the incisive canal; in the mandible, key features to avoid are the submandibular fossa and neurovascular bundles associated with the mental foramen and the inferior dental canal.27
Options for replacing missing teeth
The typical hypodontia patient presents when young and therefore providing some type of fixed solution to replace missing teeth in the long term should be a priority. Depending upon a variety of factors, this may be achieved through adhesive, conventional or implant supported fixed prostheses or a combination of some or all of these modalities. There are some cases however, where conventional removable prosthodontics provide the only realistic option for restoration.
All patients will require a thorough clinical assessment to plan their treatment effectively. In addition, the preparation of articulated study models, a diagnostic wax up or Kesling set up, can help both clinician and patient visualise the potential results. An aesthetic preview or construction of a wax trial prosthesis can go even further to transfer this information to the patient's mouth.29
Conventional and adhesive fixed bridgework
Where there are edentulous spans of short length it may be possible to place tooth-supported bridgework, however, the abutment teeth must be of sufficient quality. Microdont teeth and immature, coronally located gingival margins may not provide sufficient enamel surface area for bonding of resin bonded bridge retainers. The use of electrosurgery to increase the clinical crown height and composite bonding to increase the tooth size and improve the morphology can greatly facilitate successful adhesive bridgework.30 Primary molar teeth that are ankylosed or have reasonable root length can also act as abutments as they have good coronal surface area provided the occlusal surface is utilised for bonding.21
Conventional bridgework is generally contraindicated in young adult patients with relatively immature pulps and where abutment teeth are sound. However, in a few selected cases it may be a reasonable option especially where tooth preparation is relatively minimal and the edentulous span short. This may be the case where teeth are conical, diminutive or worn and there is a plan to increase the occlusal vertical dimension, meaning that inter-occlusal space is provided without making significant occlusal or incisal reduction. In these cases tooth preparation is often limited to the creation of a cervical finish line (Fig. 3).
a) 21-year-old patient with severe hypodontia at presentation wearing old lower partial denture; b) Note the narrow alveolar ridge width in the central incisor region, unsuitable for implants; c) 42 and 32 prepared as conventional bridge abutments; d) Conventional fixed-fixed metal ceramic bridge replacing three incisors
In older patients with a smaller pulpal volume, more sclerotic dentine and previous restorative interventions, conventional bridgework may be the most appropriate option for small to medium length edentulous spans. This treatment option has well documented predictability over reasonable time periods when carried out with appropriate clinical techniques.31
Conventional removable prostheses
Where implants are not possible, options for restoring long spans and multiple missing teeth are generally limited to removable partial dentures (RPDs). These can provide a predictable solution and are often better able to replace soft and hard tissue deficiencies without recourse to invasive surgery. However, as in adults, these do have the potential to increase caries incidence and periodontal problems, increasing the importance of preventative measure and appropriate case selection.
When designing the retentive components of RPDs, the morphology of potential abutment teeth in severe hypodontia may be inadequate in terms of their small size, lack of crown height and undercut areas. Consideration should be given to modifying these teeth by adding composite to create undercuts, and even using milled crowns in older patients with previously restored teeth to provide an improved prognosis for the removable prosthesis.
Where there is a need to increase the OVD to facilitate restoration of missing units or to improve facial aesthetics, removable prostheses can be designed to fit over the teeth that are present. Onlay, overlay or overdentures benefit from being tooth supported and in cases where the denture bearing area typically lacks features that aid retention and support, this is an advantage (Fig. 4). It is key, however, that patients have a high level of plaque control and excellent denture hygiene as this design of denture contacts the majority of tooth surfaces increasing the risk of caries and gingival inflammation.32
Conclusion
The effective management of severe hypodontia is likely to require the input of multiple clinicians, in both general dental practice and the specialist services, over a lengthy time period. It is important to ensure that in childhood, preventative regimes are initiated and where possible the primary dentition is maintained.
Where teeth are missing, conventional fixed and removable prosthodontics can offer excellent options for the restoration of aesthetics and function and are the most appropriate treatment modality for some patients. Implant retained restorations may also be considered and the provision of these will be discussed in the second part of this series.
References
Brook A H . Dental anomalies of number, form and size: their prevalence in British schoolchildren. J Int Assoc Dent Child 1974; 5: 37–53.
Bergstrom K . An orthopantomographic study of hypodontia, supernumeraries and other anomalies in school children between the ages of 8–9 years. An epidemiological study. Swed Dent J 1977; 1: 145–157.
Muller T P, Hill I N, Peterson A C, Blayney J R . A survey of congenitally missing permanent teeth. J Am Dent Assoc 1970; 81: 101–107.
Worsaae N, Jensen B N, Holm B, Holsko J . Treatment of severe hypodontia-oligodontia-an interdisciplinary concept. Int J Oral Maxillofac Surg 2007; 36: 473–480.
Hobkirk J A, Brook A H . The management of patients with severe hypodontia. J Oral Rehabil 1980; 7: 289–298.
Larmour C J, Mossey P A, Thind B S, Forgie A H, Stirrups D R . Hypodontia-a retrospective review of prevalence and aetiology. Part I. Quintessence Int 2005; 36: 263–270.
Wong A T, McMillan A S, McGrath C . Oral health-related quality of life and severe hypodontia. J Oral Rehabil 2006; 33: 869–873.
Meaney S, Anweigi L, Ziada H, Allen F . The impact of hypodontia: a qualitative study on the experiences of patients. Eur J Orthod 2012;34: 547–552.
Shaw L . Prevention of dental caries in children. Consultants in Paediatric Dentistry Group of United Kingdom and Ireland, Paediatric Dentistry Clinical Audit Committee. Int J Paediatr Dent 1997; 7: 268–272.
Zero D, Fontana M, Lennon A M . Clinical applications and outcomes of using indicators of risk in caries management. J Dent Educ 2001; 65: 1126–1132.
Walsh T, Worthington H V, Glenny A M, Appelbe P, Marinho V C, Shi X . Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2010; CD007868.
Section on Pediatric Dentistry and Oral Health. Preventive oral health intervention for paediatricians. Paediatrics 2008; 122: 1387–1394.
Laing E, Cunningham S J, Jones S, Moles D, Gill D . Psychosocial impact of hypodontia in children. Am J Orthod Dentofacial Orthop 2010; 137: 35–41.
Hobkirk J A, Goodman J R, Jones S P . Presenting complaints and findings in a group of patients attending a hypodontia clinic. Br Dent J 1994; 177: 337–339.
Bernard J P, Schatz J P, Christou P, Belser U, Kiliaridis S . Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults. A retrospective study. J Clin Periodontol 2004; 31: 1024–1028.
Yap A K, Klineberg I . Dental implants in patients with ectodermal dysplasia and tooth agenesis: a critical review of the literature. Int J Prosthodont 2009; 22: 268–276.
Cronin R J Jr., Oesterle L J, Ranly D M . Mandibular implants and the growing patient. Int J Oral Maxillofac Implants 1994; 9: 55–62.
Mankani N, Chowdhary D R, Patil DB, E DN and Madalli D P . Dental implants in children and adolescents: a literature review. J Oral Implantol 2012; epub ahead of print.
Fudalej P, Kokich V G, Leroux B . Determining the cessation of vertical growth of the craniofacial structures to facilitate placement of single-tooth implants. Am J Orthod Dentofacial Orthop 2007; 131: S59–67.
Kanno T, Carlsson G E . A review of the shortened dental arch concept focusing on the work by the Kayser/Nijmegen group. J Oral Rehabil 2006; 33: 850–862.
Robinson S, Chan M F . New teeth from old: treatment options for retained primary teeth. Br Dent J 2009; 207: 315–320.
Robinson S, Nixon P J, Gahan M J, Chan M F . Techniques for restoring worn anterior teeth with direct composite resin. Dent Update 2008; 35: 551–552, 555–558.
Nohl F, Cole B, Hobson R, Jepson N, Meechan J, Wright M . The management of hypodontia: present and future. Dent Update 2008; 35: 79–80, 82–84, 86–88 passim.
Chung L K, Hobson R S, Nunn J H, Gordon P H, Carter N E . An analysis of the skeletal relationships in a group of young people with hypodontia. J Orthod 2000; 27: 315–318.
Ogaard B, Krogstad O . Craniofacial structure and soft tissue profile in patients with severe hypodontia. Am J Orthod Dentofacial Orthop 1995; 108: 472–477.
Bondarets N, McDonald F . Analysis of the vertical facial form in patients with severe hypodontia. Am J Phys Anthropol 2000; 111: 177–184.
European Commission radiology protection No 172: cone beam CT for dental and maxillofacial radiology. Evidence based guidelines. European Commission, 2012.
Harris D, Buser D, Dula K et al. E A O. guidelines fo the use of diagnostic imaging in implant dentistry. A consensus workshop organized by the European Association for Osseointegration in Trinity College Dublin. Clin Oral Implants Res 2002; 13: 566–570.
Seymour D W, Patel M, Chan M F . Aesthetic preview: a novel approach. Dent Update 2012; 39: 422–424, 426.
Durey K A, Nixon P J, Robinson S, Chan M F . Resin bonded bridges: techniques for success. Br Dent J 2011; 211: 113–118.
Tan K, Pjetursson B E, Lang N P, Chan E S . A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res 2004; 15: 654–666.
Budtz-Jorgensen E . Effects of denture-wearing habits on periodontal health of abutment teeth in patients with overdentures. J Clin Periodontol 1994; 21: 265–269.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Durey, K., Cook, P. & Chan, M. The management of severe hypodontia. Part 1: considerations and conventional restorative options. Br Dent J 216, 25–29 (2014). https://doi.org/10.1038/sj.bdj.2013.1236
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.1236
This article is cited by
-
Management of missing maxillary lateral incisors in general practice: space opening versus space closure
British Dental Journal (2019)
-
The restorative management of microdontia
British Dental Journal (2016)
-
Management of a child with severe hypodontia in the mixed dentition stage of development
European Archives of Paediatric Dentistry (2014)