Key Points
-
Compares patient attendance patterns at primary care medical and dental practices.
-
There is a subgroup of patients who attend general dental practices more frequently than they do primary medical services.
-
Dental teams are in strong position to identify patients at high risk of general medical health problems.
-
Supports the development of a preventive general healthcare philosophy by the dental team in general dental practice.
Abstract
Background The dental team could have an important role to play in general health risk assessment within primary and community healthcare.
Aims To describe medical and dental attendance patterns, demographics and health profiles of patients routinely attending general dental practices in Warwickshire. To identify whether a subgroup attend dental practices regularly but attend medical practices infrequently and discuss whether preventive healthcare interventions delivered in general dental practice would be appropriate.
Methods A self-completion questionnaire was administered to patients attending 16 dental practices in Warwickshire.
Results Eight hundred and eleven completed questionnaires were returned (74% response). Seven hundred and eighty-nine (98%) respondents visited their dentist every one to two years or more frequently and of these a subgroup of 121 (15.3%) visited their general medical practice surgery or health centre less often than every two years. In the subgroup 9.5% reported high blood pressure, 17.6% currently smoked, 22% drank above recommended guidelines, 32.1% were overweight and 7.3% obese.
Discussion The data suggest there may be a role for dental practitioners in identifying patients at risk of having undiagnosed or future general health problems and providing appropriate general health advice, screening or signposting the patient to relevant general healthcare facilities either within or external to the dental practice.
Similar content being viewed by others
Background
The government is keen to encourage an environment where National Health Service (NHS) dentistry can become a more active part of local health services and an integral part of overall health improvement.1 The report of the NHS Future Forum states that 'every healthcare professional should use every contact with an individual to maintain or improve their mental and physical health and well-being where possible, whatever their specialty or the purpose of the contact'.2 This suggests that the dental team could have an important role to play in the wider sphere of primary healthcare in not only being involved in preventive healthcare programmes, such as smoking cessation,3,4 but also in the identification of general health risk factors such as excessive alcohol consumption,5 high blood pressure6 and obesity.7 Reducing obesity is a priority for the Government since nearly one in four adults is obese8 and obesity can have a severe impact on people's health, increasing the risk of type 2 diabetes,9 some cancers,10 heart11 and liver disease.12 Diabetes is particularly relevant in a primary dental care setting since patients with poor glycaemic control have a significantly increased prevalence of severe periodontitis.13 Furthermore, there is increasing evidence that periodontal disease contributes to problems of glycaemic control14 and inflammatory responses produced by inflamed periodontal tissues can increase the severity of diabetes, worsen cardiovascular outcomes and increase mortality.15
Recent research has shown that the screening in general dental practice for hypertension, an important risk factor for stroke and coronary heart disease, may be of benefit to the population at large.6 If the identification of risk factors and screening is to be considered in general dental practice it is useful to establish if there is a subgroup of the patient population routinely visiting a dental practice but infrequently attending a primary care general medical practice: this would add additional relevance to the potential benefits of undertaking a general health risk assessment and the dental team becoming more involved in general preventive healthcare programmes.
Since caries and periodontal disease are both widespread in the community and generally asymptomatic, dentists encourage their patients to be monitored on a regular basis, whereas many patients report attending their general medical practitioner only when symptomatic or for the ongoing management of an identified medical condition. However, there is very little evidence to support the contention that these two populations are different. Haughney et al.16 included dentistry in established screening programmes in a combined medical and dental health centre but provided no data on the attendance patterns of the patients, other than that 24% of patients were common to both practices. In a retrospective study of general medical practice by Carney et al.17 it was concluded that diseases, rather than patients, appear to dictate high consultation rates in general medical practice, and that high attendance is largely due to the presence of multiple pathology. The 2009 Adult Dental Health Survey18 showed that approximately twice as many dentate adults in the UK reported attending regular dental check-ups (61%) than reported only attending when they had trouble with their teeth (27%). The survey reported that dentate women were more likely than men to attend for regular check-ups (68% for women compared with 54% for men). No studies have been identified which compare the attendance patterns of patients attending both primary care medical and dental practices. The Department of Health undertakes a quarterly patient survey addressing a number of NHS issues, particularly focusing on the accessibility of general dental and general medical services and the frequency of attendance19 but not the relationship in attendance at both primary dental and medical care centres.
Methods
The aim of this study was to describe the medical and dental attendance patterns, demographics and health profiles of patients routinely attending general dental practices in Warwickshire, to identify whether there is a subgroup who regularly attend dental practices but attend medical practices (general practitioner surgery or health centre) infrequently and to discuss whether preventive healthcare interventions delivered in general dental practice would be appropriate. The study was approved by the Coventry and Warwickshire NHS Research Ethics Committee.
The study involved the administration of an anonymous 25 item paper-based self-completion questionnaire to patients attending general dental practices in Warwickshire. All 74 NHS dentistry providers on the NHS Warwickshire list providing general dental services under contract (67 practices with approximately 232 dentists) were invited to participate by letter and non-responders were sent a reminder letter three weeks after the initial invitation. It was planned to deliver 100 questionnaires to a maximum of20 providers selected at random from those that agreed to participate. The sample size and number of questionnaires was limited by the available funding. The first 100 consecutive patients attending the selected practices aged 18 years or over who consented were invited to complete the questionnaire either at the surgery or at home after their visit. The patients participating were not differentiated according to whether care was being received under private or NHS contract. Completed questionnaires were either collected from the practice or sent in a freepost envelope to a member of the research team. The questionnaire was developed with the input of the Warwick Diabetes Research and Education User Group and piloted in one practice to establish any practical difficulties in administering the questionnaire. The questionnaire addressed attendance at general dental and medical practices, age, gender and ethnicity, height and weight and general health history, including diabetes, cardiac and circulatory disease, smoking and drinking habits.
Results
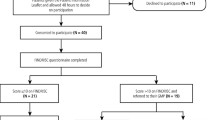
A total of 20 NHS providers initially agreed to participate in the study. Since this was the intended sample size, no random selection was necessary. The participating providers covered a large geographical area of Warwickshire and represented a range of urban, rural, deprived and non-deprived settings.
The questionnaire was piloted at one practice and since no modifications to the questionnaire were made, the 50 completed responses from this practice were included in the data analysis. Questionnaires were distributed during January and February 2011 and 811 completed questionnaires were returned giving a 74% response rate of which 39% were male and 61% female. This represented data from 16 practices since four participating practices were excluded because they failed to follow the research protocol.
Whole sample data
From the questionnaire data analysis (Table 1) almost half the respondents were aged 45-64 (mean age 51.7, SD 14.78). Ninety-five percent gave their ethnicity as White British. Ninety-eight percent stated that they visited their dentist every one to two years or more frequently and 84% visited their doctor every one to two years or more frequently. Fifty-three percent were on medication from their doctor. Eighty-eight percent rated their general health as good, very good or excellent and 12% rated it as fair or poor. 55.6% stated they undertook 30 minutes of moderate exercise on at least five days each week. 6.4% had diabetes (4.4% type 2) and 19.4% had a relative with diabetes. Twenty-nine percent had high blood pressure; 7% had heart problems and 7% had circulation problems. 11.3% reported currently smoking and 29% had smoked in the past. 16.4% admitted to drinking more than the daily recommended guidelines.20
The mean body mass index (BMI) calculated from the patient's age, height and weight was 26 (SD 4.99) from which it was calculated that 2% were underweight (BMI ≤18.5), 45% were a healthy weight (BMI = 18.5-24.9), 35% overweight (BMI = 25-30) and 18% obese (BMI ≥30) (Table 2). Where data were complete, the QD score21 was calculated to estimate the 10% or greater risk of developing type 2 diabetes within ten years and 14.6% were found to be at risk (excluding 8.1% who already had diabetes).
Subgroup data
One of the aims of the study was to identify whether there was a subgroup of the population who frequently visited the dentist but rarely visited their doctor. In this sample, 789 (98%) stated that they visited their dentist every one to two years or more frequently and of these 121 (15.3%) stated that they visited their doctor or nurse at their general practice surgery or health centre less often than every two years. The data from this selected subgroup were analysed separately.
In this subgroup 55% were male and 45% were female. The age range was similar to the whole sample although there were fewer respondents aged 65-84 (11.6%) (mean age 49.7, SD 12.69). Ninety-nine percent gave their ethnicity as White British. 9.1% were on medication from their doctor. Ninety-five percent rated their general health as good, very good or excellent and 5% rated it as fair or poor. 55.5% stated they undertook 30 minutes of moderate exercise on at least five days each week. 0.8% had diabetes and 22.9% had a relative with diabetes. 9.5% had high blood pressure; 2.5% had heart problems and 5% had circulation problems. 17.6% reported currently smoking and 25.2% had smoked in the past. Twenty-two percent admitted to drinking more than the daily recommended guidelines. The mean BMI was 24.5 (SD 3.29) from which it was calculated that 3.7% were underweight, 56.9% healthy weight, 32.1% overweight and 7.3% obese. Where data were complete, the QD score21 was calculated to estimate the 10% or greater risk of developing type 2 diabetes within 10 years and 10.8% were found to be at risk.
Discussion
Attendance characteristics of the whole sample
The results from this study (Table 1) indicated that 61% of females regularly attended the dentist which was similar to the national attendance pattern of 68%.18 However, there was a significant subgroup of the sample population (15.4%) who attended their dentist frequently but accessed primary medical care services infrequently. It was found that there was a smaller percentage of females (45%) in this subgroup when compared to the whole sample (61%) which is not surprising since consultation rates in general practice tend to be higher for females except in the very young and very elderly.22 These results suggest that there may be a significant subgroup of the population who infrequently visit their doctor and could be potentially at risk from general health problems, for example diabetes and heart disease, and could be identified within the dental practice setting.
Health characteristics of whole sample
In the whole sample (Table 1), which was predominantly White British, the number of respondents who reported that they currently smoked (11%) was lower than a reported national level of 22%18 but this was not directly comparable as the present study excluded children under 18 years. Excessive drinking was reported by 16.4% of the whole sample. Of concern was that 35% were overweight which was similar to national statistics23 and nearly 18% were obese: in 2007, 24% of adults (aged 16 or over) in England were classified as obese (BMI 30 kg/m2 or over) an overall increase from 15% in 1993.23 Over half of the sample reported undertaking regular exercise (Health and Safety Executive high activity level defined as 30 minutes of moderate physical activity on at least five days each week).
Health characteristics of the subgroup of regular attenders at their dental practice and infrequent attenders at their medical practice
In this subgroup, there were 16% more males and 84% of the population was in the 25-64-year-old age group. The risk factors for disease were notable in that 17.6% were smokers and 22% were drinking above recommended guidelines. Although obesity was lower than in the whole sample, there were a similar number of patients overweight (32%). Obesity can have a severe impact on people's health, increasing the risk of type 2 diabetes, some cancers, and heart and liver disease and when these data were used to calculate the risk of suffering from type 2 diabetes within 10 years,21 10.8% were found to be at risk. These results suggest that within this subgroup there are patients at significant risk with respect to their general health. This may be because they may not be participating in health promoting behaviour as frequently as those who visit their doctor more often. Patients who do not visit primary medical services may be unaware of services that can offer support in smoking cessation, dietary advice, etc and the dental team may have an important role to play in signposting patients to these services.
Signposting and screening
The Government has the aim of improving the health of the whole population and there is a clear role for local agencies acting together, offering help with the decisions that individuals make.24 Questions about diabetes, tobacco use and alcohol consumption are now commonly included in dental patient medical history questionnaires;25 there is a stipulation for completion of a medical history questionnaire for 90% of all patients in the new dental contract pilots Dental Quality Outcome Framework (DQOF) and so it should be an essential part of dental practice.26 The questionnaire used in this study included additional questions on height and weight which enabled the calculation of BMI and diabetes risk and it was found that 88% of participants were prepared to disclose this information which is encouraging. Although errors in self-reported height and weight may occur, it may not be practical to measure these parameters in a primary dental care setting.
Asking health-related questions, however, does not necessarily mean that the dental team are acting on the information given by patients. The 2009 Adult Dental Health Survey (ADHS)18 found that only 9% of adults sampled had been given smoking cessation advice by their dental practice in the preceding two years (22% of the sample population reported being smokers): the ADHS report states that this figure 'may well reflect a reluctance among members of the dental team to give this sort of advice'.
The use of dental practices to provide general health prevention and screening is becoming increasingly common. Some primary care trusts have commissioned services from dental practices that include brief interventions for smoking cessation and alcohol consumption, and screening for chlamydia. It is suggested that dental professionals should establish the smoking status of their patients on a regular basis,4 as has been the case with the majority of Scottish dentists since 1995,3 and evidence exists to suggest that undertaking alcohol brief interventions (ABIs),27 brief interventions for smokers28 and screening for hypertension6 can be effective and could be considered reasonable preventive practice.29
The level of trust placed in professionals, particularly health professionals, may help to prompt people towards behaviour change if advice and support is provided in a sympathetic and realistic manner.30 UK dentists who undertake conscious sedation must measure blood pressure as part of their pre-operative patient assessment31 and the dental team is therefore well placed to do this.32 A recently published study from the USA describes a more invasive intervention: identifying patients at possible risk of developing diabetes by questionnaire, periodontal examination and a blood test.33
The dental practice is often perceived by patients as being outside or independent of primary medical care services. However, for all patients identified as being at risk, particularly those who infrequently attend their doctor, dentists and the dental team are ideally placed to provide preventive advice and health promotion messages,34 undertake screening, or direct patients to appropriate services outside the dental practice. It has been suggested that the more we can use dental appointments to communicate a 'staying healthy' message, not only will the impact be more widespread and consistent but also more sustainable in the long term.35 Dietary advice, for example delivered by dental teams, has traditionally had a narrow focus not always consistent with general health advice and could be more effective if it is integrated into general health advice.36,37 This supports guidance by the National Institute for Health and Clinical Excellence (NICE).38
Barriers
A number of barriers to the delivery of general health interventions in general dental practice have been reported which include insufficient funding, poor use of dentists' time, need for training, lack of knowledge, lack of a health focus and more of a disease focus by dentists32 and these must all be addressed. The views of patients regarding dental teams' involvement in health screening and risk assessment should also be explored. However, there appears to be a real willingness by dentists to expand the dental team's remit through using dental care professionals (DCPs) in a public health role.32 It is to be hoped that the new dental contract currently under development will provide an opportunity to address some of these barriers.
IT development
One of the current problems of capturing patient medical health data is the inability to transfer the data electronically from the medical health questionnaire into a computerised patient management system. This currently wastes time and can lead to transcription errors. With the wide availability of electronic touch-pads, once the legality problems of the acceptance of electronic signatures have been resolved,39 it should be possible for patients to input their medical health details directly into their electronic record. Calculating the BMI and from this the obesity level and the diabetes risk using such algorithms as the QD score21 could all be undertaken electronically with no loss of clinical or administrative time. This would provide an opportunity for software developers to provide the dentist with an alert system that could give a visual display of those patients who are potentially at an increased health risk based on their medical history. The dentist could then provide appropriate advice, signposting or screening more selectively.
Conclusion
This study suggests that there is a subgroup of the population who attend the dentist more frequently than primary medical services. The results of this study suggest that there is a role for the dental team firstly in identifying those patients who could be at risk of current or future general health problems by means of a comprehensive medical health questionnaire and secondly after having identified the at risk patient, by providing appropriate general health advice, screening or signposting the patient to relevant general health care facilities either within or external to the dental practice.
References
Department of Health. Improving oral health and dental outcomes: developing the dental public health workforce in England. London: Department of Health, 2010. Available online at http://www.dh.gov.uk/publications.
NHS Future Forum. Summary report on proposed changes to the NHS. London: NHS Future Forum, 2011. Available online at http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127540.pdf (accessed 12 January 2012).
Chestnutt I G, Binnie V I . Smoking cessation counselling – a role for the dental profession? Br Dent J 1995; 179: 411–415.
Chestnutt I G . Tobacco use: The role of the dental team in smoking cessation. Dent Update 2010; 37: 55–62.
Room R, Babor T, Rehm J . Alcohol and public health. Lancet 2005; 365: 519–530.
Sproat C, Beheshti S, Harwood A N, Crossbie D . Should we screen for hypertension in general dental practice. Br Dent J 2009; 207: 275–277.
World Health Organization. Obesity and overweight. Fact sheet no. 311. Geneva: World Organization, 2011. Available online at http://www.who.int/mediacentre/factsheets/fs311/en/index.html (accessed 27 August 2011).
NHS Information Centre. Health survey for England 2009: health and lifestyles. Leeds: NHS Information Centre, 2010. Available online at http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england (accessed 1 March 2012).
Golay A, Ybarra J . Link between obesity and type 2 diabetes. Best Pract Res Clin Endocrinol Metab 2005; 19: 649–663.
Calle E E, Thun M J . Obesity and cancer. Oncogene 2004; 23: 6365–6378.
Baena-Díez J M, Byram A O, Grau M et al. Obesity is an independent risk factor for heart failure: Zona Franca Cohort study. Clin Cardiol 2010; 33: 760–764.
Marchesini G, Moscatiello S, Di Domizio S, Forlani G . Obesity-associated liver disease. J Clin Endocrinol Metab 2008; 93: S74–S80.
Tsai C, Hayes C, Taylor G W . Glycaemic control of Type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral Epidemiol 2002; 30: 182–192.
Taylor G W. Periodontal treatment and its effects on glycaemic control: a review of the evidence. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87: 311–316.
Skamgas M, Breen T L, LeRoith D . Update on diabetes mellitus. In Getchell T V (ed) Smell and taste in health and disease. pp 829–843. New York: Raven Press, 2008.
Haughney M G, Devennie J C, Macpherson L M, Mason D K . Integration of primary care dental and medical services: a three-year study. Br Dent J 1998; 184: 343–347.
Carney T A, Guy S, Jeffrey G . Frequent attenders in general practice: a retrospective 20-year follow-up study. Br J Gen Pract 2001; 51: 567–569.
The Health and Social Care Information Centre. Adult dental health survey. Leeds: The Health and Social Care Information Centre, 2011. Available online at http://www.ic.nhs.uk/statistics-and-data-collections/primary-care/dentistry/adult-dental-health-survey-2009--summary-report-and-thematic-series (accessed 1 March 2012).
Department of Health. Annual GP patient survey. London: Department of Health, 2008. Available online at http://www.gp-patient.co.uk/info (accessed 2 March 2012).
Office for National Statistics. General lifestyle survey 2009. UK: Office for National Statistics, 2011. Available online at http://data.gov.uk/dataset/general_lifestyle_survey (accessed 27 August 2011).
Hippisley-Cox J. QDScore®-2011 risk calculator. Available online at http://qdscore.org (accessed 2 March 2012).
NHS Information Centre. Trends in consultation rates in general practice 1995 to 2008: analysis of the QResearch® database. Leeds: NHS Information Centre, 2009. Available online at http://www.ic.nhs.uk/webfiles/publications/gp/Trends_in_Consultation_Rates_in_General_Practice_1995_2008.pdf (accessed 2 March 2012).
NHS Information Centre. Statistics on obesity, physical activity and diet: England 2009. Leeds: NHS Information Centre 2009. http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles/obesity/statistics-on-obesity-physical-activity-and-diet-england-february-2009 (accessed 2 March 2012).
Department of Health. Saving lives: our healthier nation. London: Department of Health, 1999.
British Dental Association. Patient medical history questionnaire. London: British Dental Association.
Faculty of General Dental Practice (UK). Clinical examination and record keeping — good practice guidelines. UK: Faculty of General Dental Practice (UK), 2009.
McAuley A, Goodall C A, Ogden G R, Shepherd S, Cruikshank K . Delivering alcohol screening and alcohol brief interventions within general dental practice: rationale and overview of the evidence past. Br Dent J 2011; 210: E15.
National Institute for Health and Clinical Excellence. Brief interventions and referral for smoking cessation in primary care and other settings. London: National Institute for Health and Clinical Excellence, 2006. Available online at http://www.nice.org.uk/nicemedia/pdf/PH001_smoking_cessation.pdf (accessed 2 March 2012).
Greenwood M, Lowry R J . Blood pressure measuring equipment in the dental surgery: use or ornament? Br Dent J 2002; 193: 273–275.
Eagle L, Morey Y, Case P, Verne J, Bowtell N . Response to the government's healthy lives, healthy people: our strategy for public health in England white paper. Bristol: South West Public Health Observatory, 2011.
Longman L, Heap P . Sedation. In Ireland R (ed) Advanced dental nursing. 2nd ed. p 171. Oxford: Wiley-Blackwell, 2010.
Dyer T A, Robinson P G . General health promotion in general dental practice – the involvement of the dental team part 2: a qualitative and quantitative investigation of the views of practice principals in South Yorkshire. Br Dent J 2006; 201: 45–51.
Lalla E, Kunzel C, Burkett S, Cheng B, Lamster I B . Identification of unrecognized diabetes and pre-diabetes in a dental setting. J Dent Res 2011; 90: 855–860.
British Dental Association. The British Dental Association oral health inequalities policy. London: The British Dental Association, 2009.
NHS Yorkshire and the Humber. Delivering healthy ambitions: better for less. NHS Yorkshire and the Humber. Available online at http://www.healthyambitions.co.uk/Uploads/BetterForLess/08%20BETTER%20FOR%20LESS%20every%20contact%20counts.pdf (accessed 2 March 2012).
Dyer T A, Robinson P G . General health promotion in general dental practice – the involvement of the dental team part 1: a review of the evidence of the effectiveness of brief public health interventions. Br Dent J 2006; 200: 679–685.
Department of Health. Delivering better oral health. An evidence-based toolkit for prevention. 2nd ed. London: Department of Health/The British Association for the Study of Community Dentistry, 2009. Available online at http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_102331 (accessed 2 March 2012).
National Institute for Health and Clinical Excellence. Preventing type 2 diabetes – population and community interventions: quick reference guide. PH35. London: National Institute for Health and Clinical Excellence, 2011. http://www.nice.org.uk/nicemedia/live/13472/54347/54347.pdf (accessed 2 March 2012).
Birkin D. No record, no defence. BDA News (London) 2011; Aug: 10–11.
Acknowledgements
The authors would like to acknowledge the financial support of the University of Liverpool Dental Alumni Research Fund in supporting this study and the Warwick Diabetes Research and Education User Group for their valuable contributions to the questionnaire development.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ireland, R., Bowyer, V., Ireland, A. et al. The medical and dental attendance pattern of patients attending general dental practices in Warwickshire and their general health risk assessment. Br Dent J 212, E12 (2012). https://doi.org/10.1038/sj.bdj.2012.313
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.313
This article is cited by
-
Opportunistic health screening for cardiovascular and diabetes risk factors in primary care dental practices: experiences from a service evaluation and a call to action
British Dental Journal (2023)
-
A scoping review of the implications of adult obesity in the delivery and acceptance of dental care
British Dental Journal (2016)
-
Type 2 diabetes risk screening in dental practice settings: a pilot study
British Dental Journal (2014)
-
Sawbones no longer?
British Dental Journal (2012)
-
Summary of: The medical and dental attendance pattern of patients attending general dental practices in Warwickshire and their general health risk assessment
British Dental Journal (2012)