Key Points
-
Provides an overview of factors traditionally known to cause alveolar osteitis or dry socket, including age, gender, traumatic extraction, smoking and post-extraction of third molars.
-
Suggests a new factor, irrigation of the socket with H20/saline solution, as an overlooked possible cause of dry socket.
-
Discusses the distinction between post-operative (post-extraction) pain syndrome and true dry socket syndrome.
Abstract
Purpose The aim of this prospective comparative split-mouth study was to evaluate the role of socket irrigation with a normal saline solution routinely used at the end of extraction on the development of alveolar osteitis (AO) after removal of impacted mandibular third molars (MTMs).
Materials and methods Thirty-five patients who satisfied the inclusion criteria were involved in the study and underwent extraction of four third-molars. To be included in the study, the mandibular third molars had to be impacted (partial or full bone) and require an osteotomy for extraction with use of a motorised drill. All surgeries were done under local anaesthesia or IV sedation. This was a prospective split-mouth study. The patient's left (assistant) side was a control side; it had a standard extraction technique of an impacted mandibular third molar that required a buccal full-thickness flap, buccal trough (osteotomy) and extraction of the tooth (with or without splitting the tooth into segments), followed by a traditional end-of-surgery debridement protocol consisting of a gentle curettage, bone filing of the socket walls, socket irrigation with approximately 5 ml of sterile normal saline solution and socket suctioning. The patient's right (operator) side was an experimental side; it also had a standard extraction technique of an impacted mandibular third molar at the beginning with a flap and osteotomy, but it was followed by a modified end-of-surgery protocol. It consisted of gentle curettage but the socket was not irrigated and not suctioned. It was simply left to bleed. The gauze was placed on top of the socket for haemostasis on both sides and the patient was asked to bite. On both sides, the buccal flap was positioned back without the suture. All patients were seen for a follow-up appointment four to seven days after the surgery to assess healing and check for symptoms and signs of alveolar osteitis, if present, on both irrigated and non-irrigated sides. This study followed the ethical guidelines of human subjects based on the Helsinki Declaration.
Results Thirty-five patients or 70 sockets were evaluated. Eleven out of 35 patients in the study were subjected to a dry socket syndrome (31.4%). The higher number of AO was likely related to specifics of MTM selection in this study – only impacted (partial and full bone) MTMs were chosen. Among eleven patients with AO, two patients had a bilateral condition. By excluding two patients with bilateral dry sockets from the study, there were nine patients (18 extraction sites) with unilateral AO in the study. Seven out of nine patients (14 extraction sites) developed unilateral dry socket on the control (irrigated) side (77.8%) and only two (four extraction sites) on the experimental (non-irrigated) side (22.2%). Therefore, in this study there were 3.5 times more patients (extraction sites) with dry socket syndrome on the irrigated (control) side than patients (extraction sites) in the non-irrigated (experimental) side.
Conclusion A noticeable difference of dry socket syndromes (77.8% on the irrigated versus 22.2% on non-irrigated side) was demonstrated between the traditional extraction protocol versus modified approach without the end-of-surgery irrigation. The study demonstrated that the post-extraction socket bleeding is very important for the proper uncomplicated socket healing. If it's not washed away with irrigation solution at the end of extraction, the normal blood clot has a higher likelihood to form, and therefore, can potentially lead to an uncomplicated socket healing without development of alveolar osteitis. Socket bleeding at the extraction site creates a favourable environment for the formation of a blood clot – a protective dressing – necessary for a favourable osseous healing of the socket.
Similar content being viewed by others
Introduction
One of the most common complications following tooth extraction is alveolar osteitis (AO) or dry socket (DS).1,2 Crawford first coined the term 'dry socket' in 1896.3 The incidence of dry socket is estimated between 1% and 4% after routine extractions and between 5% and 30% after removal of impacted mandibular third molars.4 Overall, dry sockets occur about ten times more often after extraction of mandibular molars compared with maxillary molars.5
Dry socket is usually a self-limiting process that starts two to three days after extraction of a tooth and progresses to its peak between the third and fifth day. The condition usually lasts for five to ten days and slowly subsides by the end of the second week in the majority of cases.4,6 The most common symptoms of dry socket are moderate-to-severe throbbing and/or radiating pain (back to the ear, down to the neck, or up to the temple) and occasional local swelling. Frequently, pain is strong enough to wake patients up at night. On examination, a dry socket is lacking a normal and healthy blood clot (appearing empty). A small degree of erythema, swelling, and occasionally foul smell might also be present. Food debris that fills the socket in these cases are common.
Aetiology of alveolar osteitis or fibrinolytic alveolitis is attributed to the partial or total disintegration of the blood clot within the alveolar socket4 due to an increased fibrinolytic activity (fibrinolysis) that destroys the blood clot early.7 In comparison, in a healthy post-extraction socket, a properly formed fibrin clot undergoes organisation, vascularisation and gradual replacement with bone through an osteoproliferation process.8
Based on the literature, risk factors that contribute to the development of AO include the following local and systemic factors: gender (females on oral contraceptives have three times more risk of dry socket than those who are not);9 age (25-30 years old and above carries a higher risk of dry socket);10,11 traumatic extraction/inexperienced surgeon;1,7,12,13 smoking (on the day of surgery and within 24 hours postoperatively, due to an apparent suction that impedes a clot formation);12,14 presence of pre-existing pericoronitis or pathology;15,16 high pre- and postoperative bacterial counts (with emphasis on the overall oral hygiene at the time of extraction);17 inadequate irrigation while using a motorised drill for an osteotomy for extraction of an impacted mandibular third molar);8 immunocompromised status of a patient (systemic antibiotics, like metronidazole, is often advisable in these cases due to mostly anaerobic bacterial presence)4,18 and others.
Treatment strategies are varying. In addition to some benefit of systemic antibiotics,19,20 a variety of local intra-socket preventative and therapeutic measures were tried and advocated in the literature. Among them are: primary versus secondary closure of surgical wound/socket that showed that secondary closure resulted in less postoperative discomfort;21 pre-operative and postoperative 0.12% chlorhexidine mouth rinses that showed the reduction in the incidence of dry socket;22 placement of intra-socket chemotherapeutic agents after extraction, like topical thermosetting gel containing 2.5% prilocaine and 2.5% lidocaine;23 insertion of tetracycline or clindamycin-impregnated Gelfoam24,25 that demonstrated decrease in dry socket cases and others agents.
The goal of this split-mouth study was to evaluate how a sterile NS irrigation (lavage) used at the end of extraction affected extraction sites and socket healing in terms of development of alveolar osteitis.
Materials and methods
Qualification for the study included healthy patients of 15 to 35 years of age and any gender or race with two impacted (partial or full bone) mandibular third molars. Only those mandibular third molars (MTMs) that required an intraoperative osteotomy (at least a buccal trough) with a motorised drill for extraction were included into the study. Exclusion criteria for the study comprised of: patients who required extraction of erupted or only soft tissue impacted mandibular third molars without bone osteotomy; an acute infection of the mandibular third molar with a discharge; an extremely complicated surgery in cases of deep impactions that required removal of large amount of alveolar bone; cases that required intra-socket root tip surgery (root fractures and root tips that had to be removed separately using additional instruments, like root tip picks); profuse postoperative bleeding that required additional surgical procedures or placement of local haemostatic agents; admittedly non-compliant patients that did not follow standard postoperative instructions (like, avoid using the straw, eating crunchy foods, drinking alcohol, spitting, etc.) and immunocompromised (diabetes, HIV) or medically-compromised (chronic heart condition, chronic liver, kidney disease etc.) patients. Thirty-five patients in this volunteer split-mouth clinical research study met the inclusion criteria and were scheduled for extraction of four third molars in the author's oral and maxillofacial surgery practice. All procedures were done under local anesthesia or IV sedation.
The author of this article, a board-certified oral surgeon, was the main and single right-handed operator for this study with a consistent positioning on the right side of the patient (the side was not changed during the surgery). Both mandibular third molars in all 35 patients in the study had a standard extraction protocol done for an impacted MTM that included: reflection of the buccal flap, buccal osteotomy and sectioning of the crown and/or tooth structure, if needed. When a surgical drill was used during extraction of a mandibular third molar (buccal osteotomy, crown/root sectioning), an adequate sterile normal saline (NS) irrigation was used at the time of drilling. After completion of extraction, the MTM socket debridement protocol varied on the right and left sides of the patient. The patient's left (assistant) side (left MTM) was a control side: it had a traditional end-of-surgery debridement protocol with a gentle curettage and bone filing of the socket after extraction followed by sterile NS irrigation of the socket with a monoject syringe (about 5 cc was used). Then, the irrigation solution in the socket was suctioned and the flap was positioned back without suture. The patient's right (operator) side (right MTM) was an experimental (research) side that had a modified protocol: after post-extraction gentle curettage, the socket was not irrigated with any solution and not suctioned. The buccal flap was positioned back without the suture. In cases of continuous oozing from the socket on any side, folded gauze was placed and a patient was asked to apply pressure by biting for a longer time.
Postoperatively, patients in the study controlled their discomfort with Ibuprofen 600 mg with or without hydrocodone 5 mg. Post-operative antibiotic treatment (amoxicillin 500 mg TID) was routinely prescribed to all study patients. All patients used 0.12% chlorhexidine rinse for three days prior to surgery and one week following. Patients initiated the rinsing the evening of the procedure. All 35 patients were seen in our clinic within four to seven days after their surgery to assess postoperative healing and symptoms of dry socket, if they were present. Three main criteria of dry socket syndrome in the study were used to make the diagnosis of alveolar osteitis:
-
1
Moderate-to-severe throbbing and/or radiating pain that started two to five days after the extraction of MTM
-
2
Pain that woke a patient up at night
-
3
Visual confirmation of a compromised socket healing without a blood clot with/without foul odour.
The following study criteria were assessed and entered into the data analysis: patient's age; gender; use of birth-control pills (BCP) by women in the study; chronic use of smoking tobacco (TOB); level of oral hygiene at the time of the surgery (classified as good, average or poor on the consultation appointment); the MTM angulation (mesioangular, vertical, distoangular and horizontal) and the depth of impaction (only partial or full bone impactions were included in the study) (Table 1).
At the time of the postoperative appointment (at four to seven days), the presence of AO on the control and experimental sides was checked. In cases of dry socket syndrome, a standard treatment protocol included use of local irrigation, pain management and occasional dry socket dressing (iodoform packing strip with eugenol-based paste).
Results
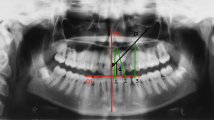
Thirty-five patients (or 70 sockets) were evaluated. Eleven out of 35 patients in the study were subjected to dry socket syndrome (31.4%). The higher number of AO in this study (than commonly reported) was likely related to specifics of MTM selection – only impacted (partial and full bone) 'difficult' MTMs were chosen and these patients were specifically followed and 'looked for'. This also agrees with a report by Nuair and Younis demonstrating a broad spectrum of AO from 3.2% for non-surgical to 20.1% for surgical extractions.26 Among 11 patients with AO, 2 patients had a bilateral condition. It was decided to exclude these two patients with bilateral dry sockets from the study. Therefore, there were nine patients (18 extraction sites) with unilateral AO in the study (example of DS case in the study, Fig. 1). Seven out of nine patients (14 extraction sites) developed unilateral dry socket on the control (irrigated) side (77.8%) and only two (four extraction sites) on the experimental (non-irrigated) side (22.2%) (Table 1). Therefore in this study, there were 3.5 times more patients (extraction sites) with dry socket syndrome on the irrigated (control) side than patients (extraction sites) in the non-irrigated (experimental) side.
Among nine patients with DS, eight were females and one male. The role of gender as a factor has already mentioned (females on oral contraceptives have three times more risk of dry socket than those who are not).9 Among eight females in the study with DS, only two were on birth-control pills that might have contributed to their DS condition. The role of difficulty of extraction (level of impaction) in this study was based on about an equal division between partially and full bony impacted MTM extractions that developed dry sockets: four were full bony and five partial bone impactions. It is known that traumatic extraction plays a role in development of AO.1,7
A statistical analysis was done to test the hypothesis that the proportion of dry sockets is smaller on the side of the surgery without irrigation (experimental side). The sign test considered only those patients where there was a difference between the two sides (those patients with dry socket condition on both sides and those with dry sockets on neither sides were excluded). Nine patients met this criterion with seven dry socket cases occurring on the side of irrigation. The probability of this occurrence by chance is p = 0.09. Other statistical studies were reserved for future follow-up reports.
All patients in the study used postoperative pain control with ibuprofen with or without hydrocodone and perioperative course of 0.12% chlorhexidine rinse for three days prior to surgery and one week following (two to three times a day, starting the evening of the procedure).
Discussion
Prevention of alveolar osteitis remains a key approach in management of this painful post-extraction condition.6 To decrease risk of AO, the goal of an operator is to perform an atraumatic tooth removal (with controlled reflection of the flap and decreased exposure to the motorized drill) that will conclude with formation of a blot clot in the fresh post-extraction socket. During this study, it was noticed that younger patients had a higher capacity for socket wall bleeding and blood repopulation even after the copious irrigation with NS solution, while older patients or patients with a denser bone had less ability to reconstitute the blood clot. It seems that 'older' sockets are especially sensitive to end-of-surgery effects of irrigation (washing away the blood) and should likely not be irrigated at the completion of the tooth removal. It is possible that the NS irrigation in these cases could not only physically empty the socket from the blood filling it but also may interrupt the coagulation cascade leading to a delayed socket healing. Obviously, sound surgical principles in MTM surgery should be followed and irrigation with NS is important in cases of gross surgical debris seen at the end of the complicated extraction under the periosteal flap (to prevent subperiosteal abscess) or loose bone spicules noticed inside the socket that cannot be removed with a mosquito haemostat.
In the literature, there is a lack of distinction between AO (dry socket syndrome) and 'simple' postoperative pain. That is to say that not every painful postoperative socket (alveolus) after extraction of a mandibular third molar should be immediately diagnosed with dry socket syndrome (a disturbance of post-extraction site wound healing).27 Some painful conditions after removal of MTM could point to the fact that a patient had a traumatic extraction of a complicated impacted mandibular third molar that may not become a dry socket. Thus, attention to post-extraction symptoms and signs helps distinguish between alveolar osteitis (AO) and postoperative non-dry socket pain. Pain associated with dry socket syndrome starts on the third to fifth day after the procedure as a moderate-to-severe sharp radiating/throbbing and awakening pain. A postoperative (post-traumatic) pain associated with extensive hard tissue osteotomies and considerable soft tissue dissections, starts on the day of surgery after the anaesthetic wears off as a moderate-to-severe dull pain that parallels the postoperative swelling, picks up at 24-48 hours, and slowly subsides (both swelling and pain) over the following two to three days. If a development of AO depends on the constitution of a normal blood clot at the end of the surgery, development of postoperative (non-dry socket) pain relates to an amount of local surgical trauma. A patient's overall condition on the day of surgery and individual pain threshold are important for both syndromes. A distinction of these two pain syndromes can be difficult due to the fact that many (but not all) complicated and traumatic extractions develop a dry socket condition.
A sterile NS irrigation solution is utilised routinely in mandibular third molar surgery in two circumstances: during the osteotomy (that is, buccal trough, crown/root sectioning) to decrease heat generated by the surgical drill in contact with the bone, and at the end of extraction to presumably eliminate bone debris in the socket after osteotomy. Although it is understandable to use a cool NS irrigation during the bone drilling, it may not be prudent in many cases to use irrigation when an extraction is complete. Lavage with irrigation solution (sterile NS, in most cases) delivered by a hand monoject syringe tends to wash away the fresh blood and decrease socket bleeding. The bleeding may or may not repopulate again in the socket, often leaving the socket empty or full of water (NS) instead of blood (Fig. 2).
There are very few clinical studies in the literature concerning postoperative lavage of the MTM extraction sites. Relevant to this research were only two literature reports by Butler and Sweet28,29 that analysed the effect of NS lavage on the incidence of AO in MTM extraction sites. They compared large amounts of irrigation (175 ml NS solution) with small amounts (less than 25 ml). The authors concluded that more AO cases (23 vs 12) occurred with minimal-volume lavage, advocating a large amount of postoperative NS irrigation to reduce the incidence of localised osteitis.
This preliminary study demonstrated less need for immediate postoperative lavage of the MTM extraction sites. Some limitations of this study included the small sample size and right-handed surgeon operating on the right side only (operating on the contralateral side from the surgeon may add to the difficulty of the surgery and the amount of postoperative complications).
It is obvious that the aetiology of alveolar osteitis is complex and many variables are partially responsible for this condition. In this article, the author attempted to highlight one more possibly overlooked factor contributing to AO – an immediate postoperative irrigation of the fresh extraction socket commonly utilised as a part of the surgical technique in these cases. Further clinical studies on this subject utilising a larger sample size and randomised double-blind approach with multitude of statistical tests are recommended to confirm this preliminary report.
References
Colby R C . The general practitioner's perspective of the etiology, prevention, and treatment of dry socket. Gen Dent 1997; 45: 461–467.
Haug R H, Perrott D H, Gonzalez M L, Talwar R M . The American Association of Oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg 2005; 63: 1106–1114.
Crawford J Y . Dry socket. Cosmos 1896; 38: 929.
Blum I R : Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg 2002; 31: 309–317.
Alling C C III, Helfrick J F, Alling R D . Impacted teeth. Philadelphia: W B Saunders, 1993.
Noroozi A R, Philbert R F . Modern concepts in understanding and management of the 'dry socket' syndrome: comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 30–35.
Birn H . Etiology and pathogenesis in fibrinolytic alveolitis (dry socket). Int J Oral Surg 1973; 2: 215–263.
Houston J P, McCollum J, Pietz D, Schneck D . Alveolar osteitis: a review of its etiology, prevention, and treatment modalities. Gen Dent 2002; 50: 457–463.
Lilly G E, Osbon D B, Rael E M, Samuels H S, Jones J C . Alveolar osteitis associated with mandibular third molar extractions. J Am Dent Assoc 1974; 88: 802–806.
MacGregor A J . Aetiology of dry socket: a clinical investigation. Br J Oral Surg 1968; 6: 49–58.
Clauser B, Barone R, Briccoli L, Baleani A . Complications in surgical removal of mandibular third molars. Minerva Stomatol 2009; 58: 359–366.
Bortoluzzi M C, Manfro R, De Déa B E, Dutra D C . Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J Contemp Dent Pract 2010; 11: E033–E040.
Contar C M, de Oliveira P, Kanegusuku K, Berticelli R D, Azevedo-Alanis L R, Machado M A . Complications in third molar removal: a retrospective study of 588 patients. Med Oral Patol Oral Cir Bucal 2010; 15: e74–e78.
Sweet J B, Butler D P . The relationship of smoking to localized osteitis. J Oral Surg 1979; 37: 732–735.
Kay L W . Investigations into the nature of pericoronitis. Br J Oral Surg 1966; 3: 188–205.
Chuang S K, Perrott D H, Susarta S M, Dodson T B . Risk factors for inflammatory complications following third molar surgery in adults. J Oral Maxillofac Surg 2008; 66: 2213–2218.
Brown L R, Merrill S S, Allen R E . Microbiologic study of intraoral wounds. J Oral Surg 1970; 28: 89–95.
Fazakerley M, Field E A . Dry socket: a painful post-extraction complication (a review). Dent Update 1991; 18: 31–34.
Halpern L R, Dodson T B . Does prophylactic administration of systemic antibiotics prevent postoperative inflammatory complications after third molar surgery? J Oral Maxillofac Surg 2007; 65: 177–185.
Ren Y F, Malmstrom H S . Effectiveness of antibiotic prophylaxis in third molar surgery: a meta-analysis of randomized controlled clinical trials. J Oral Maxillofac Surg 2007; 65: 1909–1921.
Danda A K, Krishna Tatiparthi M, Narayanan V, Siddareddi A . Influence of primary and secondary closure of surgical wound after impacted mandibular third molar removal on postoperative pain and swelling - a comparative and split mouth study. J Oral Maxillofac Surg 2010; 68: 309–312.
Shepherd J . Pre-operative chlorhexidine mouth rinses reduce the incidence of dry socket. Evid Based Dent 2007; 8: 43.
Burgoyne C C, Giglio J A, Reese S E, Sima A P, Laskin D M . The efficacy of a topical anesthetic gel in the relief of pain associated with localized alveolar osteitis. J Oral Maxillofac Surg 2010; 68: 144–148.
Swanson A E . A double-blind study on the effectiveness of tetracycline in reducing the incidence of fibrinolytic alveolitis. J Oral Maxillofac Surg 1989; 47: 165–167.
Trieger N, Schlagel G D . Preventing dry socket: a simple procedure that works. J Am Dent Assoc 1991; 122: 67–68.
Nusair Y M, Younis M H . Prevalence, clinical picture, and risk factors of a dry socket in a Jordanian dental teaching centre. J Contemp Dent Pract 2007; 8: 53–63.
Adeyemo W L, Ladeinde A L, Ogunlewe M O . Clinical evaluation of post-extraction site wound healing. J Contemp Dent Pract 2006; 7: 40–49.
Butler D P, Sweet J B . Effect of lavage on the incidence of localized osteitis in mandibular third molar extraction sites. Oral Surg Oral Med Oral Pathol 1977; 44: 14–20.
Sweet J B, Butler D P, Drager J L . Effects of lavage techniques with third molar surgery. Oral Surg Oral Med Oral Pathol 1976; 41: 152–168.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Tolstunov, L. Influence of immediate post-extraction socket irrigation on development of alveolar osteitis after mandibular third molar removal: a prospective split-mouth study, preliminary report. Br Dent J 213, 597–601 (2012). https://doi.org/10.1038/sj.bdj.2012.1134
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.1134
This article is cited by
-
Alveolar ridge preservation: why, when and how
British Dental Journal (2019)
-
Postoperative socket irrigation with drinking tap water reduces the risk of inflammatory complications following surgical removal of third molars: a multicenter randomized trial
Clinical Oral Investigations (2017)
-
Observe the healing process
British Dental Journal (2013)
-
Wrong message
British Dental Journal (2013)