Key Points
-
Investigates immediate effects of acupuncture in patients with oromyofacial pain in a randomised, double-blind and placebo-controlled trial.
-
Shows immediate and effective pain relief (VAS) using microsystem acupuncture in patients with oromyofacial pain, headaches and neck pain.
-
Suggests a close relationship between occlusion, muscles and the cervical spine.
Abstract
Background Patients presenting with oromyofacial disorders and pain in the head and neck area are often resistant to conventional therapy. Acupuncture has been shown to be effective in pain reduction.
Methods Twenty-three patients with craniomandibular disorders, headache and, in particular, local pain in the orofacial, cervical and temporomandibular joint areas were randomised into acupuncture or placebo laser therapy groups. Pain was assessed by a visual analogue scale (VAS) and by palpation of 14 muscles and groups of muscles immediately before and after treatment, the assessor being blinded to the patients' allocation. Applicable acupuncture points were searched and pricked using the 'very-point' technique.
Findings Pain reduction measured by VAS was significantly more pronounced after acupuncture than after placebo treatment (p = 0.031). Sum of pain scores across 14 muscles was considerably more reduced after acupuncture as compared to sham laser treatment.
Interpretation Acupuncture may bring about immediate pain relief in patients with oromyofacial disorders, increasing the chance to initiate other therapeutic measures.
Similar content being viewed by others
Introduction
Patients with craniomandibular disorders (CMD) frequently suffer not only from pain and dysfunction in the temporomandibular joint (TMJ) and the masticatory muscles, but also from headaches, cervical spine disorders, impaired opening of the mouth, joint clicking,1,2,3,4,5,6,7,8,9 sinusitis, chronic neck pain, and reduced cervical spine mobility.10,11 This variety of pain symptoms apply not only to dentistry but also to many other disciplines of medicine.
Acupuncture has been acknowledged to be effective in pain relief for more than 2000 years (traditional Chinese medicine, TCM).12 Not only pain conditions but also muscular dysfunction and tension and psychosomatic disorders, as well as dysregulation of the lymphatic and immune systems, respond well to acupuncture treatment, as has been confirmed by numerous scientific studies.13,14,15,16 Trials performed using MRI revealed immediate signals in specific areas of the brain.17,18
Modern pain research has disclosed the various effects of acupuncture quite incidentally, providing, at the same time, neurophysiological explanations. Purposeful needle stimulation applied to specific skin or mucosa points activates the organism's self-regulation and modulation abilities. Pain modulation is affected in many different ways. One of the more outstanding results of pain research is the activation of endorphins and neurotransmitters when acupuncture stimuli are being applied.19,20
In traditional acupuncture, points of analogous reflex relations are found in linear sequences (chains), ie meridians. In recently discovered microsystem acupuncture, systematic point patterns are found on circumscribed parts of the body, eg the auricle, the oral cavity and other areas. These microsystems of acupuncture can be defined as somatotopies, representing the multitude of organs and their respective functions. Microsystem points are only detectable in a state of irritation. Activation of microsystem points expresses itself in increased sensitivity and pressure, signalling functional disorders in the corresponding organ.
Stimulating microsystem points has proved to be a very effective method of acupuncture treatment. For optimum results, the microsystem points are preferably detected and pricked by means of the 'very-point' technique.21
In cases of pain in the stomatognathic system and dysfunction of the TMJ, remote points situated on the hands, on the auricles, at the sternum and particularly in the enoral retromolar area of the lower jaw, have been indicated to be effective in previous open trials. Freedom from pain and muscular tension can often be achieved immediately by 'very-point' therapy.21
There exist various reports on the effects of acupuncture but only a small number of them provide results from placebo-controlled trials. Therefore, an investigation was undertaken to study the immediate effects of acupuncture in patients with myofacial pain and craniomandibular disorders (CMD) in a randomised, double-blind and placebo-controlled fashion.
Methods
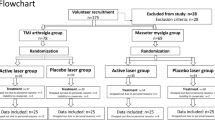
A total of 23 female patients aged 18 to 64 years, with dysfunction and pain in the stomatognatic system – particularly in the TMJ – and all receiving no therapy, were included in the trial during February 2002 and July 2003. Consecutive patients presenting at the outpatient unit of the Department of Prosthetic Dentistry with dysfunction and pain in the stomatognatic system not attributable to a known underlying disease or disorder were eligible if they were female and between 18 and 65 years. All contacted patients consented to take part. Patients were randomised using a computer generated random permutation list into two groups: one group was treated by acupuncture (n = 11) and the other group received sham laser treatment (n = 12).13,22,23 Randomisation was done after consent was obtained and before arrangements for the date of therapy were made by a nurse. The study protocol had been approved by the ethics committee of the Medical University of Vienna. Therapy was performed in the Department of Prosthetic Dentistry of the Medical University of Vienna. Allocation of patients into the arms of the study was performed after informed consent was obtained and therapy was scheduled two to seven days after enrolment.
The patients were unaware of whether they were receiving verum or placebo treatment; this was only disclosed after the final assessment. Placebo treated patients were then informed that another kind of treatment might be more effective, and needle acupuncture was offered. All patients in the placebo group agreed and were consequently treated by acupuncture.
The physician who palpated the different muscles and registered patients' pain scores was blinded to their verum or placebo status. Patients were assessed immediately before and after treatment.
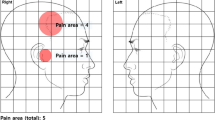
Patients' subjective pain experience was evaluated on a visual analogue scale (VAS). Muscle palpation included the following muscles and areas: atlanto-occipital junction, m. temporalis anterior, m. temporalis medialis, m. temporalis posterior, muscles of the cranio-mandibular junction, pterygoid muscles, masseter muscles, m. digastricus, and m. sternocleidomastoideus, bilaterally. Pain sensation at muscle palpation was rated on a four point scale rising according to intensity from 0 to 3.
Classical acupuncture points according to TCM as well as microsystem points were palpated, especially points corresponding to the disorders in question. Table 1 shows acupuncture points that were positive on palpation and those that were used in therapy. In microsystem acupuncture, points that show a high degree of irritation have proven to be more suitable for therapy. These points have, therefore, been given preference. Adler points were used for diagnostic purposes as well as for assessment of therapy.
Oral acupuncture was performed by means of superficial injection canulas, as it is impractical to use acupuncture needles in the mouth. For precise point detection and subsequent point insertion, the 'very-point' technique was used. This technique enables acupuncture points to be spotted and pricked with maximum accuracy. Point detection and immediate needle insertion of skin points is carried out with very fine and sharp injection needles in the oral cavity. Firstly, the area surrounding the suspected enoral point is palpated manually. Secondly, the region in which the maximum sensitivity was noted by the patient is tapped gently and tangentially with the therapy needle itself, preferably at an angle about 45°. The point of greatest sensitivity and tenderness, the 'very point', forms, as a rule, the centre of the area of irritation, and the patient reacts accordingly by mimic expression and/or verbal affirmation.
Treatment was performed double blind as neither the patient nor the evaluating person were informed about the non-functioning laser pen. The placebo laser was a soft laser pen which, however, had been inactivated – only a normal red light was emitted. To make this placebo procedure appear real to the patient, visual and acoustic signals accompanied the red light emission. Criteria of point selection were the same as in the verum group. Every point was 'sham irradiated' for about two minutes. The laser pen did not touch the skin but was held at a distance of about 0.5-1 cm.
Statistical methods
Sample size was determined based on data from a preliminary open trial. Under the assumption of a difference of one standard deviation with respect to the primary endpoint between groups, an alpha level of 5% and a power goal of 80%, ten patients per group are necessary. The primary endpoint was the subjective assessment of pain by the patient using a visual analogue scale. Secondary endpoints were pain on palpation of the different muscles and muscle groups. The latter were combined by computing the sum of pain ratings over all muscles and muscle groups. Medians and quartile ranges were computed as estimates for central tendency and dispersion. Before/after treatment differences in VAS ratings and sum score of pain on palpation were compared between groups by Mann-Whitney tests. For the primary endpoint, alpha error was set to 0.05. Exploratory tests were performed for the secondary endpoints and uncorrected p-values are reported.
Results
Figure 1 shows results for muscles and muscle groups that were initially painful on palpation in at least 20% of either verum or placebo patients. Pain reduction, as assessed by palpation, was more pronounced in the acupuncture group than in the placebo laser group. Of fourteen muscles or groups of muscles examined, nine initially scored painful on palpation in 20% or more of the patients. Palpation pain was most commonly observed in the pterygoid and masseter muscles (up to 96% of patients). Greater reduction in pain was achieved by acupuncture (average 40%), than with placebo treatment (average 8%).
A large proportion of patients had suffered initially from pain of the shoulder-neck area (91% in the acupuncture group and 58% of patients in the placebo group). In the acupuncture group, 64% of patients reported a reduction on the pain scale, while 20% proved completely pain-free on palpation. In contrast, none of the patients in the placebo group were pain-free after sham treatment.
Fifty percent of the acupuncture group patients who had initially felt pain on palpation of m. digastricus showed recovery upon treatment. In more than 50% of the placebo-treated patients, however, palpative pain of the same muscle persisted after therapy. In the temporal muscles acupuncture achieved a reduction in almost 100% of the patients while no reduction in pain was observed following placebo treatment. Placebo treatment had also no effect for the m. sternocleidomastoideus, whereas of the 64% of verum patients with pain in this area, acupuncture brought about a reduction in pain in 9% of them. Palpative pain in the hyoid muscles was only rarely encountered and it was resolved by acupuncture in most of the cases. A summary of the results with pain ratings assessed by palpation is given in Table 2.
The results of overall pain ratings on a visual analogue scale (VAS) are summarised in Table 3. VAS scores decreased both after acupuncture and after sham treatment, however, following acupuncture, pain score reduction proved significantly more pronounced (p = 0.031).
Discussion
In a previous trial comparing one single session of acupuncture treatment with no treatment, a significant improvement in cervical mobility of patients with chronic neck pain was reported, this being in line with the results of other authors.24,25,26 The present study was designed to test immediate effects of acupuncture on oromyofacial pain refractive to prior conventional therapeutic interventions. Our results indicate that acupuncture therapy using remote points – either traditional points or corresponding microsystem points found in a state of irritation – has an immediate effect on both motion-related pain and pain at rest in patients with CMD, TMJ and cervical spine mobility disorders.
Although results in the control group indicate a certain potential for a placebo effect, it must be considered that these patients were also palpated and that palpation and relaxation alone may relieve pain. Pain in placebo patients was reduced in one muscle (m. masseter), but in three muscles (m. digastricus, m. sternocleido, m. atl-occ-junct.) there was an increase in pain.
The absence of local therapy applications is of particular significance where issues of subjective sensitivity to treatment may be involved and, consequently, a higher percentage of placebo effects may occur. Moreover, the study demonstrates the importance of specific point selection, performed by finger palpation, needle detection and subsequent needle insertion, at punctual sites of maximum sensitivity within a suspected point area. This 'very-point' method can be applied to both skin and mucous membrane points.
In the mouth, a system of very effective points is to be found in the mucous membranes. These points act as reflex points in modern pain therapy, as well as in acupuncture. Mucosa points, in a state of irritation, have a high degree of sensitivity to pressure during palpation. In this case, reflex therapy of specific points proves highly effective. The topography of the points determines the direction of possible therapeutic effects. From the retromolar area in particular, immediate relaxation, releasing tensions in the upper and lower jaw, can be achieved. The reflex action from the retromolar areas, affects, above all, the cervical muscles, including the deep muscles of the receptor field of the neck. Even if the immediate effects of an enoral treatment do not guarantee a permanent outcome, instant relief from muscular tension and pain is an important and strong motivating factor for the patient. Once such initial relief and improvement is achieved, the patient is more open-minded about further treatment.
Specific traditional points on the sternum (Renmai), as well as the cervical Adlerlanger points were used both in diagnosis and in follow-up checks to assess patients' progress. Local pain points – trigger points – were not treated locally in this study. Treatment was carried out via remote points and via superior systems in order to break pain memories and to avoid local pain areas during initial therapy.
One feature of microsystem acupuncture is that specific points act as points of input to the organism's regulatory systems. Microsystem points are categorised as remote points, far away from the pain-affected site – a fact well appreciated by patients suffering from intensive local pain. A very small number of patients do not respond to the treatment suggested in the study. This indicates that these patients are non-responders to treatment via their regulatory system. The vast majority of patients, however, experience immediate pain relief without the affected area having to be touched. Thus, they are motivated for follow-up therapy.
One single acupuncture session may provide immediate pain relief, alleviation of muscle tension and simultaneous improvement of mobility and the interplay between both TMJ and cervical spine. This demonstrates the close interrelationship of the TMJ and the cervical areas, craniomandibular dysfunction and neck and shoulder complaints. Such disorders have become very common and are of relevance to various medical disciplines, amongst which dentistry plays a key role as teeth occlusion, muscles, TMJ and cervical spine indeed form a functional unit.7,15,27
References
Gelb H. Clinical management of head and TMJ pain and dysfunction. Philadelphia: Saunders, 1977.
Wanman A. Longitudinal course of symptoms of craniomandibular disorders in men and women. A 10-year follow-up study of an epidemiologic sample. Acta Odontol Scand 1996; 54: 337–342.
Freesmeyer W B. Funktionelle Befunde im orofacialen System und deren Wechselwirkung. München: Hanser, 1987.
Slavicek R. Clinical and instrumental functional analysis for diagnosis and treatment planning. Part 7. Computer-aided axiography. J Clin Orthod 1988; 22: 776–787.
Solberg W K. Temporomandibular disorders: physical tests in diagnosis. Br Dent J 1986; 160: 273–277.
Krogh-Poulsen W G, Olsson A. Occlusal disharmonies and dysfunction of the stomatognathic system. Dent Clin North Am 1966; 10: 627–635.
Rauhala K, Oikarinen K S, Raustia A M. Role of temporomandibular disorders (TMD) in facial pain: occlusion, muscle and TMJ pain. Cranio 1999; 17: 254–261.
Gsellmann B, Schmid-Schwap M, Piehslinger E, Slavicek R. Anamnestic findings in patients with temporomandibular joint disease. J Gnathol 1995; 14: 41–46.
Hieber G. Kiefergelenksbeschwerden. Dtsch Z Akupunktur 1999; 4: 216–222.
Costen J B. A syndrome of ear and sinus symptoms dependant upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol 1934; 43: 1–15.
Travell J. TMJ pain referred from muscles of the head and neck. J Prosthet Dent 1960; 10: 745–763.
World Health Organisation. WHO indication list for acupuncture. WHO, 1970.
Irnich D, Behrens N, Molzen H et al. Randomised trial of acupuncture compared with conventional massage and 'sham' laser acupuncture for treatment of chronic neck pain. BMJ 2001; 322: 1574–1578.
Irnich D, Behrens N, Gleditsch J M et al. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: results of a randomized, double-blind, sham-controlled crossover trial. Pain 2002; 99: 83–89.
Rosted P. Practical recommendations for the use of acupuncture in the treatment of temporomandibular disorders based on the outcome of published controlled studies. Oral Dis 2001; 7: 109–115.
Bossy J. Immune systems, defense mechanisms and acupuncture: fundamental and practical aspects. Am J Acupunct 1990; 18: 219–232.
Hui K K S, Liu J, Makris N et al. Acupunture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp 2000; 9: 13–25.
Pert A, Dionne R, Ng L, Bragin E, Moody T W, Pert C B. Alterations in rat central nervous system endorphins following transauricular electroacupuncture. Brain Res 1981; 224: 83–93.
Beers R F. Mechanisms of pain and analgesic compounds. New York: Raven Press, 1979.
Sandkühler J. The organisation and function of endogenous antinociceptive systems. Prog Neurobiol 1996; 50: 49–81.
Gleditsch J M. The 'very point' technique: a needle based point detection method. Acupunct Med 1995; 13: 20–21.
Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998; 352: 364–365.
Vincent C, Lewith G. Placebo controls for acupuncture studies. J R Soc Med 1995; 88: 199–202.
Löhnert V, Roniger I, Keusch R, Tilscher H. Akupunktur bei Zervikalsyndromen. Manuelle Medizin 1996; 34: 269–274.
Gleditsch J M. Oral acupuncture. Acupunct Med 1995; 13: 15–19.
Melzack R, Stillwell D M, Fox E J. Trigger points and acupuncture points for pain: correlations and implications. Pain 1977; 3: 3–23.
Lu D P, Lu G P, Kleinman L. Acupuncture and clinical hypnosis for facial and head and neck pain: a single crossover comparison. Am J Clin Hypn 2001; 44: 141–148.
Acknowledgements
This study has been approved by the Ethics Committee of the Medical School of the University of Vienna and the General Hospital of the City of Vienna (No.: 427/2001).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Simma, I., Gleditsch, J., Simma, L. et al. Immediate effects of microsystem acupuncture in patients with oromyofacial pain and craniomandibular disorders (CMD): a double-blind, placebo-controlled trial. Br Dent J 207, E26 (2009). https://doi.org/10.1038/sj.bdj.2009.959
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.959
This article is cited by
-
Efficacy of acupuncture and laser acupuncture in temporomandibular disorders: a systematic review and meta-analysis of randomized controlled trials
BMC Oral Health (2024)
-
Acupuncture and Traditional Chinese Medicine in the Management of Orofacial Pain and Temporomandibular Disorders: a Narrative Review
Current Oral Health Reports (2024)
-
Die Very-Point®-Technik nach Gleditsch
Deutsche Zeitschrift für Akupunktur (2023)
-
Mundakupunktur
Deutsche Zeitschrift für Akupunktur (2023)
-
Assessing and treating primary headaches and cranio-facial pain in patients undergoing rehabilitation for neurological diseases
The Journal of Headache and Pain (2017)