Key Points
-
Panoramic radiographs do not seem to be a good screening tool for detection of carotid stenosis and are not cost effective for this purpose.
-
There is poor clinical correlation between calcifications in panoramic radiographs and carotid ultrasound unless the patient has an advanced coronary problem.
Abstract
Objectives Carotid artery calcification is responsible for an estimated 5% of ischaemic strokes. Carotid doppler sonography (DS) is a frequently used non-invasive method for assessing carotid artery stenosis and calcification. This study assessed the utility of panoramic radiography to detect any carotid artery calcification in patients with and without coronary artery disease, as well as the level of agreement between panoramic radiographs and DS findings.
Methods Ninety subjects who underwent coronary angiography for any reason in Namazi Hospital, Shiraz University of Medical Science during an 11 month period received a DS assessment and panoramic radiograph. The radiopacities adjacent to the cervical vertebrae at or below the intervertebral space between C3-C4 were diagnosed as carotid artery calcifications. Carotid calcifications were scored as present or absent and pattern of calcification was noted by a maxillofacial radiologist who was blind to the angiogram and sonogram results. The final sample population was 84 subjects, providing data on 168 carotid arteries.
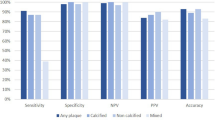
Results The panoramic radiograph had a sensitivity of 66.6% and a positive predictive value of 45% for detecting carotid artery calcifications in patients whose angiograms confimed the coronary artery disease. It had 50% sensitivity in patients with normal angiogram. The level of agreement between panoramic radiographs and DS results was weak.
Conclusion Because of low sensitivity and positive predictive value, the panoramic radiograph can not be considered an accurate or reliable method for detecting carotid artery calcification.
Similar content being viewed by others
Introduction
Cerebrovascular accident (CVA) is the third most common cause of death in industrialised countries, following cardiovascular disease and cancer.1 In Iran it is a significant public health issue, not only due to its high incidence, but also because of the high costs involved in the physical and psychological rehabilitation of these patients.2,3,4
Eighty-five percent of CVAs are ischaemic, two-thirds of which are believed to be caused by thrombus and embolus formation in the region of the carotid artery bifurcation.1 Atherosclerotic plaques are the main cause of progressive luminal narrowing of an artery, which results in impairment of flow once more than 50-70% of the lumen diameter is obstructed. This impairment in flow results in inadequate blood supply to the target organ in the event of increased metabolic activity and oxygen demand. Stable angina pectoris, intermittent claudication, and mesenteric angina are examples of the clinical consequences of this mismatch. Rupture of a plaque or denudation of the endothelium overlying a fibrous plaque may result in exposure of the highly thrombogenic sub-endothelium and lipid core. This exposure may result into thrombus formation, which may partially or completely occlude the flow in the involved artery.5
Early detection of those patients at risk of cerebral ischaemic attack is the main tool for reducing the prevalence of the disease. A strong association between the extent of carotid atherosclerosis and coronary atherosclerosis has been demonstrated, and one follow-up study has reported the relation between coronary artery disease and carotid plaque progression. Patients with coexistent narrowing of the carotid and coronary arteries represent a particularly high-risk group and to date there has been no consensus with regard to their management. While in a general adult population the prevalence of carotid stenosis approaches 4%, in patients with coronary artery disease it can reach 30-70%.6 Previous studies reported a strong correlation between the extent of coronary atherosclerosis and extracranial carotid atherosclerosis using non-invasive ultrasonography.7 Duplex ultrasonography (DS) is the most frequently used gold standard for assessing carotid artery stenosis and as a non-invasive technique to determine calcifications and stenosis caused by atherosclerotic.8
In recent years, a number of publications9,10,11,12 have described carotid artery calcifications (CACs) in the region of the carotid bifurcation on panoramic radiographs. Despite the great prevalence of carotid stenosis in patients with coronary artery disease (CAD), there has been no investigation into assessing carotid artery atheromas via panoramic imaging in CAD patients. Hence, we evaluated patients with and without diagnosed CAD for carotid atherosclerosis using panoramic radiography and Doppler sonography.
Methods and materials
From April 2007 to March 2008, 90 patients who underwent coronary angiography in Fars Heart Foundation (FHF) for any reason and agreed to be enrolled in the research were entered into this study. A cardiologist classified the patients into two groups, those with and without CAD, according to angiogram results. All patients underwent Doppler sonography and panoramic radiography as a routine protocol in FHF.
Imaging studies
Carotid Doppler (B mode ultrasounds) were carried out by an experienced general radiologist as a routine set protocol in patient management. Angle adjustment for calculation of blood-flow velocity was based on the flow direction as depicted by colour Doppler (Logiq 9, General Electric, USA) using 7.5 MHz linear array transducers. The radiologist interpreted all reports and assessed any calcification as present or absent in bilateral carotid artery sonograms and was blind to the angiogram results.
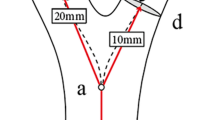
The patients then underwent panoramic radiography in the Radiology Department of Shiraz Dental School using the standard technique and positioning (ProlineXC, Planmeca, Finland). The size of the panoramic film was 15-30 cm. Radiographs that were distorted because of the subjects' movements during the exposure or that did not include C3 and C4, especially in patients with large faces, were eliminated. Films were processed by an Optimax 2010 processor (Protec, Germany) and interpreted by an oral and maxillofacial radiologist. The study radiographs were viewed consecutively in a room with dimmed light. No time limit was imposed. 'Hot-spot' illumination was available. Any irregular, heterogeneous, verticollinear or circular radiopaque mass adjacent to the cervical vertebrae at or below the intervertebral space between C3 and C4 was diagnosed as a carotid artery calcification (Fig. 1).13
Carotid calcifications were scored as present or absent and the pattern of calcification was noted by the maxillofacial radiologist, who was blind to the angiogram and sonogram results.
Results
Of the 90 subjects initially evaluated, six had radiographs of poor image quality and were excluded. The final sample population was 84 subjects, providing data for 168 carotid arteries. The subjects ranged in age from 35 to 76 years with a mean age of 55.56 ± 10.91 years, and 44 (52.3%) were male.
Twenty-two subjects were normal in their angiograms, while 62 patients had signs of CAD. Fifty-four (32.1%) arteries in 35 participants were judged to be calcified based on the radiographs. The number of arteries judged from the ultrasound to have any calcification was 39 (23.2%). Comparing the two groups, the percentage of calcified plaques was not higher in CAD patients (21.8 compared with 27.3).
In CAD-free patients, six out of 12 arteries that were reported calcified by DS were also detected in panoramic radiographs, and 23 of 32 arteries which were judged not calcified based on DS were confirmed by panoramic radiography. In patients with CAD, 18 out of 27 arteries reported calcified and 75 of 97 confirmed to be non-calcified by DS were confirmed by panoramic radiography.
Utility of panoramic radiography to detect carotid artery calcification
The panoramic radiograph had a sensitivity of 50% in detecting carotid artery calcification in patients with normal angiogram (Table 1). This figure reflects the unreliability of panoramic radiography for detecting carotid artery calcification; the number of false positive results was 9.
Considering patients whose angiograms confirmed the CAD (124 arteries), panoramic radiographs could detect any carotid artery calcification in 66.6% of these patients. There were 22 false positives (Table 2).
Measurements of agreement between panoramic radiographs and DS results considering all patients in the two groups were assessed by Kappa statistics (k = 0.27, p = 0.000). The agreement rate with respect to p <0.05 was ranked as follows: k <0.4 = weak; k 0.4-0.75 = average to good; k >0.75 = very good to excellent. The agreement rate for our results was therefore weak.
Discussion
The present study focused on the level of agreement between DS diagnostics and panoramic radiographic signs of carotid calcification in individuals who had a confirmed diagnosis of coronary disease or not. To the best of our knowledge, this is the first study designed to assess the panoramic radiograph as a viable tool to detect atherosclerosis by using DS results as the gold standard in patients with coronary artery disease. In this clinical study, the positive predictive values of radiographic findings for calcified carotid artery atheromas were low. It was also found that radiographic findings had a high negative predictive value for having negative DS interpretations in both groups.
Although the significance of the detectability of calcified carotid atheromas by panoramic radiography is uncertain, several studies examining the prevalence and characteristics of these lesions have been performed. These studies have seldom described the accuracy of panoramic radiography for such lesions because few have been controlled with an adequate gold standard. Ravon et al. were the first who confirmed calcifications radiographically by the means of DS gold standard. Their results suggested that unilateral observed calcifications in panoramic radiography with a size of 10 mm or above were consistent with positive DS readings, suggesting that these patients should be referred to a physician for evaluation of cardiovascular disease.14 It was also found that similarly to our study, radiographic findings had a high negative predictive value for having negative DS interpretations on both sides of the neck. This means that most patients who do not have panoramically detectable carotid calcification also do not have carotid stenosis. Unlike the study by Ravon et al., we did not measure the dimensions of carotid calcification to avoid erroneous measurements owing to uneven panoramic magnification. Ravon et al. also reported measurements of agreement between panoramic and DS results assessed by Kappa statistics (k = 0.61, p = 0.001) which were considerably higher than our agreement levels.
In a study conducted by Friedlander et al., of the sample population of 65 patients who had visible opacities consistent with carotid artery calcification on their panoramic radiographs, all were confirmed to have atherosclerotic lesions by DS scans. They assessed radiographically the observed calcifications based on the degree of carotid stenosis according to DS evaluation, and suggested that clinicians should refer all patients with atheroma like lesions on their radiographs to a physician to decrease the likelihood of fatal and nonfatal strokes.15 These results are in contrast to ours with regard to the usefulness of panoramic radiography in detecting carotid calcification, which may be due to our patient selection and the fact that we performed DS for all cases, not just those with positive findings in panoramic radiography. However, any improvement is welcome.
Madden et al. determined the utility of panoramic radiographs for detecting extracranial calcified carotid atheroma and carotid luminal stenosis. Their results reflect the unreliability of the panoramic radiograph in detecting moderate to severe carotid artery calcification and a high number of false positives. They concluded that because of low sensitivity and positive predictive values, the panoramic radiograph can not be considered an accurate or reliable detector of calcification or stenosis.16 Although there are some differences between our results and this study, probably because of our selection criteria, we are in agreement with the authors of this research on the unreliability of panoramic radiography to detect the carotid artery calcifications.
Deahl compared the Madden study with an earlier ultrasound-controlled study by Ravon et al. and suggested a larger population-based study to settle the apparent conflict between these two studies. He also commented on an overestimation in positive and negative predictive values in they Madden study due to the use of a sample of subjects who were likely to be at higher-than-usual risk of carotid artery disease.17
Our study showed a lower occurrence of carotid calcification in CAD patients. Although the degree of stenosis was higher in CAD patients, detected calcification by DS had an inverse relationship with stenosis. This may suggest that CACs can not be a predictive of CAD in old age. Currently, the global trend of coronary disease is to affect increasingly younger populations. Calcification, on the other hand, is mostly related to the aging process. So the weak association of coronary disease and carotid calcification in our results may be explained on that basis.
In addition, the smaller sample size of our study may have limited its ability to show differences between CACs and the associated coronary disease. Perhaps a larger, population-based study could be done in the future to calculate a more realistic result.
A significant limitation of using panoramic radiographs to detect calcified carotid atheromas is the number of false positive findings. Many nearby or overlying anatomical structures and some unrelated pathological conditions can make it difficult to diagnose calcified carotid atheroma via these radiographs. Triticeous cartilage is frequently confused with a calcified atheroma plaque.1 In addition, the wide range of radiographic appearances of CACs that have been found in some studies, including irregular, heterogeneous verticollinear or circular radiopaque masses at the level of the C3-C4 intervertebral junction, make the differentiation more complicated. CACs are mostly circular and often superimposed over the prevertebral soft tissue when small, and mostly linear or thin rectangular when enlarged and appear more laterally on the panoramic view than calcified triticeous cartilage. They may also be unilateral or bilateral with a location that is not restricted by the imaginary line between the hyoid bone and the thyroid cartilage.11,18,19 Even if a narrow spectrum of calcification patterns can not be defined, it seems worthwhile to train and make dental practitioners aware of calcifications in this area.
When deciding whether to refer a patient to a physician, our results were in agreement with studies that reported a weak ability of panoramic radiography to detect CACs. Some research demonstrated a certain correlation between carotid calcifications and clinical events. Moreover, the presence of calcification was more commonly associated with severe stenosis than any other morphologic features of atheroma.20 If the correlation between carotid calcification and development of cerebrovascular clinical events was effectively demonstrated, it would be possible, through panoramic radiographs, not only to contribute to the early detection of patients at risk of CVA, but also to that of those at risk of heart failure. However, recent vascular studies have shown that symptomatic plaques are more echolucent and less calcified than asymptomatic plaques and are associated with a greater degree of histopathologic plaque necrosis.21,22 They appear to overestimate the accuracy of panoramic radiography to predict carotid bifurcation disease, and this may predispose patients with asymptomatic carotid disease to untoward costly diagnostic imaging and intervention.
Although duplex ultrasonography is the most accurate screening method short of angiography, and is non-invasive, its cost-benefit ratio is unfavourable, even when limited to the population over the age of 65. Nevertheless, in high-risk groups, there are authors who consider that its use might be profitable.23 Since panoramic radiography is commonly used in dental clinics to evaluate the maxillofacial region, and modern ultrasonic screening is non-invasive, accurate and inexpensive, the clinical importance and severe side-effects of stroke may yet justify the identification of at-risk subgroups of patients using these more cost-effective evaluations of carotid artery stenosis.
Yoon et al. used CT scanning as a gold standard to show the moderate diagnostic accuracy of panoramic radiography in detection of carotid artery calcification with low sensitivity.24 The potential choices for measuring CAC depends upon considerations such as differences in radiation exposure, cost, and availability. While carotid CT scanning is considered the best tool for detecting calcifications, because the pathological significance of calcification can not be assessed by CT alone and ultrasound has excellent value for detecting both calcium and stenosis in the carotid arteries, it is considered as the best clinical tool for evaluation of the carotid arteries in study populations.
Recently, the new computed tomography technique electron beam tomography (EBT) has been used to establish the extent of coronary atherosclerosis. It offers short acquisition time and high spatial resolution which permit the visualization of coronary arteries without motion artefacts and therefore the detection and quantification of coronary calcification.25 In future, EBT may permit the non-invasive detection of carotid atherosclerosis with high reliability.
Conclusion
To our knowledge, this study is the first to determine whether panoramic radiographs are useful for detecting calcified carotid atheromas and stenoses, using carotid artery ultrasound as the gold standard diagnosis in patients with signs of coronary artery disease. We conclude that because of low sensitivity and positive predictive value, the panoramic radiograph cannot be considered an accurate or reliable detector for calcification or stenosis.
References
Chicano R R, Sánchez R E, Castaño F L, Merino C C, López F M. Panoramic radiograph as a method for detecting calcified atheroma plaques. Review of literature. Med Oral Patol Oral Cir Bucal 2006; 11: E261–E266.
Kelishadi R, Sadri G, Tavasoli A A et al. Cumulative prevalence of risk factors for atherosclerotic cardiovascular diseases in Iranian adolescents: IHHP-HHPC. J Pediatr (Rio J) 2005; 81: 447–453.
Yazdi A T, Rezaei A, Azari J B et al. Prevalence of atherosclerotic plaque in autopsy cases with non-cardiac death. Iranian J Pathol 2009; 4: 101–104.
Kelishadi R, Hashemipour M, Sarraf-Zadegan N, Amiri M. Trend of atherosclerotic risk factors in children of Isfahan. Asian Cardiovasc Thorac Ann 2001; 9: 36–40.
Boudi F B. Causes and treatment of atherosclerosis. Published online in eMedicine Specialties, 2006. http://emedicine.medscape.com/specialties
Komorovsky R, Desideri A. Carotid ultrasound assessment of patients with coronary artery disease: a useful index for risk stratification. Vasc Health Risk Manag 2005; 1: 131–136.
Fuster V, Alexander R W, Orouke R A (eds). Hurst's The heart. Volume 2. 11th ed. pp 2335–2336. New York: McGraw-Hill, 2004.
Wyman R A, Fraizer M C, Keevil J G et al. Ultrasound-detected carotid plaque as a screening tool for advanced subclinical atherosclerosis. Am Heart J 2005; 150: 1081–1085.
Friedlander A H, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol 1981; 52: 102–104.
Friedlander A H, Manesh F, Wasterlain C G. Prevalence of detectable carotid artery calcifications on panoramic radiographs of recent stroke victims. Oral Surg Oral Med Oral Pathol 1994; 77: 669–673.
Carter L C, Haller A D, Nadarajah V, Calamel A D, Aguirre A. Use of panoramic radiography among an ambulatory dental population to detect patients at risk of stroke. J Am Dent Assoc 1997; 128: 977–984.
Lewis D A, Brooks S L. Carotid artery calcification in a general dental population: a retrospective study of panoramic radiographs. Gen Dent 1999; 47: 98–103.
Pornprasertsuk-Damrongsri S, Thanakun S. Carotid artery calcification detected on panoramic radiographs in a group of Thai population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101: 110–115.
Ravon N A, Hollender L G, McDonald V, Persson G R. Signs of carotid calcification from dental panoramic radiographs are in agreement with Doppler sonography results. J Clin Periodontol 2003; 30: 1084–1090.
Friedlander A H, Neal R, Garrett, Chin E E, Baker J D. Ultrasonographic confirmation of carotid artery atheromas diagnosed via panoramic radiography. J Am Dent Assoc 2005; 136: 635–640.
Madden R P, Hodges J S, Salmen C W et al. Utility of panoramic radiographs in detecting cervical calcified carotid atheroma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 543–548.
Deahl S T 2nd. Panoramic radiography does not reliably detect carotid artery calcification nor stenosis. J Evid Based Dent Pract 2007; 7: 172–173.
Ahmad M, Madden R, Perez L. Triticeous cartilage: prevalence on panoramic radiographs and diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 225–230.
Carter L C. Discrimination between calcified triticeous cartilage and calcified carotid atheroma on panoramic radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 108–110.
Culebras A, Otero C, Toledo J R, Rubin B S. Computed tomographic study of cervical carotid calcification. Stroke 1989; 20: 1472–1476.
Grogan J K, Desai T, Schwarze G et al. B-mode ultrasonographic characterization of carotid atherosclerotic plaques in symptomatic and asymptomatic patients. J Vasc Surg 2005; 42: 435–441.
Shaalan W E, Cheng H, Gewertz B et al. Degree of carotid plaque calcification in relation to symptomatic outcome and plaque inflammation. J Vasc Surg 2004; 40: 262–269.
Callow A D, Trachtenberg J D. Diagnosis and surgical management of asymptomatic carotid stenosis. In Ernst C B, Stanley J C (eds) Current therapy in vascular surgery. 3rd ed. pp 29–34. St. Louis: Mosby-Year Book, 1999.
Yoon S J, Yoon W, Kim O S, Lee J S, Kang B C. Diagnostic accuracy of panoramic radiography in the detection of calcified carotid artery. Dentomaxillofac Radiol 2008; 37: 104–108.
Seese B, Brandt-Pohlmann M, Moshage W, Achenbach S, Schwarz T, Bachmann K. Evaluation of the association between coronary calcification detected by electron beam computed tomography and atherosclerosis of extracranial carotid arteries in vivo. Int J Angiol 1998; 7: 301–306.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Khosropanah, S., Shahidi, S., Bronoosh, P. et al. Evaluation of carotid calcification detected using panoramic radiography and carotid Doppler sonography in patients with and without coronary artery disease. Br Dent J 207, E8 (2009). https://doi.org/10.1038/sj.bdj.2009.762
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.762
This article is cited by
-
Diagnostic accuracy of panoramic radiography in the detection of calcified carotid artery atheroma: a meta-analysis
Clinical Oral Investigations (2019)
-
Modern dental imaging: a review of the current technology and clinical applications in dental practice
European Radiology (2010)
-
Odd practice
British Dental Journal (2009)
-
Summary of: Evaluation of carotid calcification detected using panoramic radiography and carotid Doppler sonography in patients with and without coronary artery disease
British Dental Journal (2009)