Key Points
-
Highlights the extent of damage a simple complication can cause.
-
Details the specific precautions that can prevent such a complication.
-
Highlights the difficulty faced in resolving the residual damage in such a patient.
Abstract
Facial atrophy of the buccal fat pad following inadvertent subcutaneous extrusion of sodium hypochlorite is very rare. It is a complication which leaves the patient with a defect which is very difficult to treat. We present the case of a 46-year-old lady who presented with almost complete unilateral atrophy of the buccal fat pad. She has undergone multiple surgeries over the past two years. We highlight the precautions that must be taken to prevent such a complication and the difficulties in rehabilitating such a patient.
Similar content being viewed by others
Case report
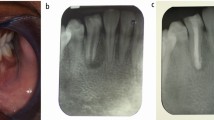
A 46-year-old lady was undergoing root canal treatment on the maxillary right first molar (16) with her general dental practitioner. During the procedure an endodontic syringe was used to irrigate the root canal system with 5.5% sodium hypochlorite. After three cycles of irrigation the patient felt severe pain and swelling in the right cheek. Treatment was immediately stopped. Examination revealed a swelling on the right cheek. She was referred to Glasgow Dental Hospital for further management where she was initially prescribed antibiotics. Shortly afterwards the 16 was removed. The swelling resolved slowly over a four month period. Once the swelling had resolved she noted a progressive shrinkage of the tissues of her right face over the following two years. She was referred to the Department of Oral and Maxillofacial Surgery for further management.
On examination the facial nerve was intact and she had no paraesthesia or anaesthesia of the cheek and lip. There was atrophy of the subcutaneous tissues of the right face causing a marked facial asymmetry (Figs 1,2). All treatment options were outlined to the patient including free flap augmentation of the subcutaneous tissue and fat grafting. She elected to undergo fat transposition.
Under general anaesthesia fat transfer was performed from the anterior abdominal wall to the right cheek defect which succeeded in increasing volume in the right cheek. The procedure was repeated twice over the next 18 months because of graft atrophy. While it has not been possible to completely eliminate the defect, the patient is happy with the result and does not want further surgery (Figs 3,4).
Discussion
Sodium hypochlorite has been used as an endodontic irrigant since the 1920s. It is now routinely used worldwide owing to its ability to cause liquefaction of organic material by reacting with fatty acids and amino acids.1 The potential complications to its use in endodontics were reviewed by Spencer, Ike and Brennan.2 The risk of tissue necrosis of the surrounding mucosa, subcutaneous tissues and skin3 following periradicular extrusion of sodium hypochlorite has been mentioned. There have, however, not been any published cases highlighting this complication. The clinical presentation of this patient is further interesting because of the extreme nature of the residual damage that occurred.
While the risk of tissue necrosis has been mentioned in the review of complications, there have not been any published cases highlighting this problem. The clinical presentation of this patient is further interesting because of the extreme nature of the residual damage that occurred.
The common causes for periradicular extrusion are excessive irrigation pressure, use of an improper syringe for irrigation and improper positioning of the endodontic needle in the canal.4
Nerve damage to the branches of the facial and trigeminal nerve have been described.4,5,6 Patients being treated under local anaesthesia they may not experience pain immediately. The patient described above developed a swelling associated with severe pain in the cheek. She had however sustained no sensory or motor damage to the nerves in the area.
If the canal is to be irrigated using a needle and syringe, the needle must be side venting. The use of hypodermic (end exiting) needles in root canal irrigation risks accidental inoculation into the soft tissues. Only Luer-Lok style syringes and needles should be used, as taper seat needles may dislodge in use, with uncontrolled loss of the hypochlorite solution under pressure.7 The needle should not engage the sides of the canal, but be loosely positioned within the canal. The needle should not reach the apical extent of the prepared canal. The irrigant is delivered slowly with minimal pressure to reduce the likelihood of forcing it through the apex. This is most easily achieved by using the index finger rather than thumb to depress the plunger.8
Subcutaneous augmentation using free vascularised tissue would allow substantial restoration of facial volume. However, even with this technique it is difficult to predictably restore the symmetry of the face. In this case the defect was small and this technique was not necessary. Free fat grafting by the Coleman method can restore volumes to a lesser extent but again achieving symmetry is difficult and the grafted fat partially resorbs with time. Another approach is to remove subcutaneous fat from the 'normal' side of the face. This would carry a risk of facial nerve damage and achieving symmetry is once again unpredictable
References
Estrela C, Estrela R A C, Barbin E L et al. Mechanism of action of sodium hypochlorite. Braz Dent J 2002; 13: 113–117.
Spencer H R, Ike V, Brennan P A . Review: the use of sodium hypochlorite in endodontics – potential complications and their management. Br Dent J 2007; 202: 555–559.
Sabala G L, Powell S E . Sodium hypochlorite injection into periapical tissues. J Endod 1989; 15: 490–492.
Witton R, Henthorn K, Ethunandan M et al. Neurological complications following extrusion of sodium hypochlorite solution during root canal treatment. Int Endod J 2005; 38: 843–848.
Becking A G . Complications in the use of sodium hypochlorite during endodontic treatment. Oral Surg Oral Med Oral Pathol 1991; 71: 346–348.
Serper A, Ozbek M, Calt S . Accidental sodium hypochlorite-induced skin injury during endodontic treatment. J Endod 2004; 30: 180–181.
Clarkson R M, Moule A J . Sodium hypochlorite and its use as an endodontic irrigant. Aust Dent J 1998; 43: 250–256.
Manogue M, Patel S, Walker R . The principles of endodontics. pp 138–139. Oxford University Press, 2005.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Markose, G., Cotter, C. & Hislop, W. Facial atrophy following accidental subcutaneous extrusion of sodium hypochlorite. Br Dent J 206, 263–264 (2009). https://doi.org/10.1038/sj.bdj.2009.166
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.166