Abstract
To draw attention to a rare neurological deterioration after spinal cord injury (SCI) and to discuss evidence supporting an increase in cerebrospinal fluid pressure (CSFP), we present an extremely rare case of subacute post-traumatic ascending myelopathy (SPAM) in which the patient sustained a T12 fracture initially resulting in paraplegia and after undergoing posterior fixation and anterior decompression. The patient was a 32-year-old healthy man who sustained a T12 burst fracture with complete paraplegia after a fall injury. The patient underwent a posterior reduction and short-segment fixation 8 h after the injury and an anterior thoracoscopic-assisted decompression on post-traumatic day 8. On post-traumatic day 21, he had a progressive neurological deterioration with dyspnoea and decreased muscle strength of both upper extremities that could not be relieved by conservative intervention. After undergoing a cervical posterior laminectomy and durotomy, the patient exhibited the clinical manifestation of brain herniation. There was no recovery of autonomous respiration, and the patient entered a coma. The patient died on post-traumatic day 25 because of cardiac and respiratory arrest. SPAM is a rare, potentially fatal neurological deterioration after SCI; however, a prompt diagnosis can be made by magnetic resonance imaging. Our observations suggest that an increase in CSFP may be the main cause of SPAM. The paraplegic level should be recorded daily so that neurological deterioration can be recognised as soon as possible.
Similar content being viewed by others
Introduction
Subacute post-traumatic ascending myelopathy (SPAM) is a rare complication after spinal cord injury (SCI) that is defined as neurological deterioration involving four or more vertebral segments above the initial injured site and usually occurring within the first few weeks after the injury.1,2 A typical SPAM magnetic resonance imaging (MRI) includes a hyperintense signal on T2-weighted sequences, a heterogeneous intramedullary signal on T1-weighted sequences and an expanded spinal cord typically without a syringe.1 Frankel was the first to report this type of neurological deterioration.3
The exact cause and pathophysiological mechanisms of SPAM remain elusive, although several causes have been postulated. These include arterial thrombosis, venous thrombosis, congestive ischaemia, inflammatory or autoimmune reaction, and infection in the form of meningitis or myelitis.
Neurological deterioration ascending from the thoracolumbar spine to the cervical spine is distinctly rare. Here we present an extremely rare case of SPAM that developed in a patient who initially sustained a T12 fracture resulting in paraplegia and after undergoing posterior fixation and anterior decompression. The patient subsequently experienced a striking neurological deterioration that ultimately resulted in death. We will discuss the possible mechanism of this condition and a reasonable therapeutic regimen.
Case report
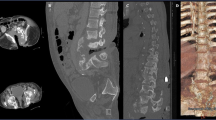
A 32-year-old healthy man fell from a 10-foot height at work. Upon physical examination, he exhibited complete paraplegia below the T12 level (ASIA Impairment Scale Grade A). Radiological examinations, including plain radiograph, computed tomography scan and MRI, revealed a T12 burst fracture with a large retropulsed fragment causing significant compression of the spinal cord (Figures 1a–e). There were no clinical or radiological abnormalities in the cervical spine or upper extremities. A high dose of methylprednisolone was administered with gastric protection medication. The patient underwent a posterior reduction and short-segment fixation procedure without decompression from T11 to L1 8 h after injury (Figures 2a and b). Postoperatively, the patient was haemodynamically and neurologically stable. A postoperative computed tomography scan showed that a large retropulsed fragment remained in the canal (Figure 1f), and anterior thoracoscopic-assisted decompression and internal fixation surgery was performed on post-traumatic day 8 (Figures 2c and d).
Preoperative plain radiography, computed tomography (CT) scan and MRI showed a T12 burst fracture with severe canal compromise (a–e). (a) X-ray of thoracolumbar lateral view. (b) MRI sagittal view of thoracolumbar T2-weighted sequence. (c) MRI sagittal view of thoracolumbar T1-weighted sequence. (d) MRI axial view at injured site. (e) Axial CT scan at injured site. Postoperative CT scan revealed there was still a canal compromise (f).
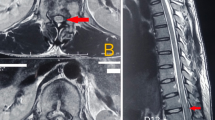
His postoperative period was uneventful without episodes of low blood pressure or other complications. On post-traumatic day 21, he complained of headache, neck pain, and tingling and numbness in both hands. Upon neurological examination, his muscle strength was normal, and there were no abnormal reflexes in either of his upper extremities. The paraplegic level had risen to the C8 level, but an MRI could not be performed because it was the weekend. We suspected neurological deterioration; therefore, methylprednisolone, mannitol and low-molecular-weight heparin were empirically administered to improve the neurological symptoms, which eventually disappeared. However, on post-traumatic day 23, his neurological deterioration became aggravated, and his sensory level ascended to C4. He had dyspnoea, and his muscle strength decreased to grades 1–2/5 for the flexors and extensors of the wrist and fingers and to 3/5 for the brachioradialis, biceps, triceps and deltoid muscles. A cervical MRI revealed spinal cord swelling from the thoracic level to C2 and a diffused, mildly hyperintense signal on T2-weighted sequences (Figure 3). There was no evidence of haemorrhage or syringomyelia. When the patient first showed the symptom of dyspnoea, he received supplementary oxygen through a mask, which did not alleviate the dyspnoea. He developed a progressive hypoxemia; thus, mechanical ventilation was used to improve respiratory failure and prevent cardiopulmonary arrest. His respiratory parameters were not measured after his neurological status began to deteriorate. Conservative therapy could not improve the patient’s life-threatening deterioration. A cervical posterior laminectomy and durotomy were performed to improve the intrathecal compression of the spinal cord. After incising the dura mater, an obviously enlarged spinal cord herniated from the thecal cavity.
Cervical spine MRI performed on post-traumatic day 23. (a) T2-weighted sequence showed increased signal and swelling between C2 and upper thoracic cord. (b) T1-weighted sequence showed heterogeneous intramedullary signal. (c) Axial T2-weighted image obtained at the C5 level showing an obviously swelling cord.
After the operation, the patient failed to show recovery of autonomous respiration and entered a coma with a Glasgow Coma score of five. He required intubation and mechanical ventilation. Both of his pupils were dilated and failed to constrict in response to light. This patient died on post-traumatic day 25 because of cardiac and respiratory arrest. His relatives refused an autopsy. This patient had no medical record indicating the paraplegic level after the anterior approach procedure was performed.
Discussion
Although SPAM is a rare condition of neurological deterioration, it is well recognised according to its typical clinical manifestations and characteristics on MRI. A number of conservative interventions, including close observation, maintaining normal blood pressure, anticoagulation, antiapoptotic treatment, physical therapy, steroids and osmolar treatments have been carried out.1,3–7 Slight neurological improvement can occur over time in the majority of cases; however, none of these patients return to their baseline level of functioning. Unfortunately, in our case, conservative therapy could not improve SPAM, and the patient had a progressive neurological deterioration for which ventilatory support was required.
Yablon et al.8 found that thorough decompression of the injured cord with rigid internal fixation could markedly reduce the incidence of neurological deterioration by comparing the result of conservative therapy. Although traditional epidural decompression seems adequate during surgery, postoperative MRI often reveals that the swollen cord has filled the subarachnoid space.9,10 Obvious cerebrospinal fluid pressure (CSFP) elevation has been shown after SCI in preclinical and clinical studies,11–13 and CSFP elevation may lead to neurological dysfunction.14
Meagher et al.15 and Planner et al. 2 reported that disruption of CSF dynamics was the major cause of SPAM. In an SCI animal model, Jones et al.16 found that an enlarged cord immediately occluded the subarachnoid space in severe SCI, and CSF pressure was only partially decreased by epidural decompressive surgery.11 Okada et al.17 found that systemically increased intraspinal pressure is involved in the pathogenesis of ascending myelopathy.
In our case, there was a large retropulsed fragment that remained in the spinal canal after the first posterior correction by short-level fixation. This led to a continuous compression of the spinal cord that might have caused an increase in CSFP and contributed to the process of SPAM. When a cervical posterior durotomy was performed, the enlarged cord herniated from the intrathecal cavity, indicating an obvious increase in CSFP. After durotomy, the patient showed clinical manifestations of brain herniation, including dilated pupils and the loss of consciousness and autonomous respiration, which also could have indicated the SCFP was elevated.
The theory of CSF flow alterations as a cause of SPAM correlates well with the time period in which the clinical symptoms were observed and the imaging findings.7 Although ascending myelopathy is often thought to be partly reversible, the persisting increase in intraspinal pressure may result in intramedullary ischaemia and irreversible neurological deficits.
Interventions to reduce an increased SCFP before SPAM develops are very important. In a case of SPAM reported by Meagher et al.,15 a cordectomy was performed at the initial injured site, and 4 weeks after the cordectomy, the neurological examination revealed a complete resolution of SPAM. Duraplasty and cord untethering also have been shown to be effective in improving the deteriorated neurological dysfunction of SPAM.18
MRI should be performed to observe whether there is a complete obstruction of CSF flow around the injured site because it may have a key role in confirming the aetiology of SPAM. Planner et al.2 thought that MRI changes could occur without a detectable neurological deterioration. Unfortunately, our patient could not receive an MRI because of the anterior and posterior instruments. Aito S et al.4 had stressed the importance of adopting MRI-compatible instrumentation for the surgical stabilisation of the spine.
A paraplegic level should be recorded daily so that neurological deterioration can be recognised as soon as possible. In our patient, there was no medical record of the paraplegic level after the anterior decompressive surgery. If we could have detected the neurological deterioration in the early stage of SPAM, the patient might have had a better prognosis.
This patient’s death was likely related to respiratory failure secondary to SPAM, but there was no measurement of respiratory parameters when his neurological status began to deteriorate. Respiratory status according to objective spirometry should be monitored closely and evaluated; thus, it would be useful to give appropriate ventilatory support, especially before his death.
Conclusion
SPAM is a rare, potentially fatal neurological deterioration after SCI. Its onset is most common within a couple of weeks after the initial injury. Our observation suggests that an increase in CSFP may be the main cause of SPAM. Close observation of the paraplegic level should be performed daily so that neurological deterioration can be detected as soon as possible. A prompt diagnosis can be made by MRI. Adoption of MRI-compatible instrumentation for the surgical stabilisation of the spine may help in confirming the aetiology of SPAM. Surgical intervention to reduce the increased SCFP or even normalise the CSFP might be a promising procedure for managing SPAM.
References
Belanger E, Picard C, Lacerte D, Lavallee P, Levi AD . Subacute posttraumatic ascending myelopathy after spinal cord injury. Report of three cases. J Neurosurg 2000; 93: 294–299.
Planner AC, Pretorius PM, Graham A, Meagher TM . Subacute progressive ascending myelopathy following spinal cord injury: MRI appearances and clinical presentation. Spinal Cord 2008; 46: 140–144.
Frankel HL . Ascending cord lesion in the early stages following spinal injury. Paraplegia 1969; 7: 111–118.
Aito S, El Masry WS, Gerner HJ, Lorenzo ND, Pellicanò G, D'Andrea M et al. Ascending myelopathy in the early stage of spinal cord injury. Spinal Cord 1999; 37: 617–623.
Al-Ghatany M, Al-Shraim M, Levi AD, Midha R . Pathological features including apoptosis in subacute posttraumatic ascending myelopathy. Case report and review of the literature. J Neurosurg Spine 2005; 2: 619–623.
Schmidt BJ . Subacute delayed ascending myelopathy after low spine injury: case report and evidence of a vascular mechanism. Spinal Cord 2006; 44: 322–325.
Kovanda TJ, Horn EM . Subacute posttraumatic ascending myelopathy in a 15-year-old boy. J Neurosurg Spine 2014; 21: 454–457.
Yablon IG, Ordia J, Mortara R, Reed J, Spatz E . Acute ascending myelopathy of the spine. Spine 1989; 14: 1084–1089.
Matsuyama Y, Kawakami N, Mimatsu K . Spinal cord expansion after decompression in cervical myelopathy. Investigation by computed tomography myelography and ultrasonography. Spine 1995; 20: 1657–1663.
Harada A, Mimatsu K . Postoperative changes in the spinal cord in cervical myelopathy demonstrated by magnetic resonance imaging. Spine 1992; 17: 1275–1280.
Jones CF, Newell RS, Lee JH, Cripton PA, Kwon BK . The pressure distribution of cerebrospinal fluid responds to residual compression and decompression in ananimal model of acute spinal cord injury. Spine 2012; 37: E1422–E1431.
Horn EM, Theodore N, Assina R, Spetzler RF, Sonntag VK, Preul MC . The effects of intrathecal hypotension on tissue perfusion and pathophysiological outcome after acute spinalcord injury. Neurosurg Focus 2008; 25: E12.
Kwon BK, Curt A, Belanger LM, Bernardo A, Chan D, Markez JA et al. Intrathecal pressure monitoring and cerebrospinal fluid drainage in acute spinal cord injury: a prospective randomized trial. J Neurosurg Spine 2009; 10: 181–193.
Fedorow CA, Moon MC, Mutch WA, Grocott HP . Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: rationale and practical considerationsfor management. Anesth Analg 2010; 111: 46–58.
Meagher TM, Belci M, López de Heredia L, Ansorge O, Jamous A, Saif M et al. Resolution of SPAM following cordectomy: implications for understanding pathophysiology. Spinal Cord 2012; 50: 638–640.
Jones CF, Cripton PA, Kwon BK . Gross morphological changes of the spinal cord immediately after surgical decompression in a large animal model of traumatic spinal cord injury. Spine 2012; 37: E890–E899.
Okada S, Saito T, Kawano O, Hayashida M, Matsumoto Y, Harimaya K et al. Sequential changes of ascending myelopathy after spinal cord injury on magnetic resonance imaging: a case report of neurologic deterioration from paraplegia to tetraplegia. Spine J 2014; 14: e9–e14.
Lee TT, Arias JM, Andrus HL, Quencer RM, Falcone SF, Green BA . Progressive posttraumatic myelomalacic myelopathy: treatment with untethering and expansive duraplasty. J Neurosurg 1997; 86: 624–628.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, J., Wang, H., Liu, H. et al. Subacute post-traumatic ascending myelopathy after T12 burst fracture in a 32-year-old male: case report and surgical result of cervical durotomy. Spinal Cord Ser Cases 2, 16004 (2016). https://doi.org/10.1038/scsandc.2016.4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.4
This article is cited by
-
Subacute posttraumatic ascending myelopathy: a literature review
Spinal Cord Series and Cases (2017)