Abstract
Autonomic dysreflexia (AD) following spinal cord injury can lead to a physiologic state where there is unopposed sympathetic tone and subsequent hypertension, bradycardia, hyperhidrosis and anxiety. It is known to be triggered by nociceptive stimuli below the level of injury—most commonly constipation and bladder retention. We present a case of a C6–7 tetraplegic who developed AD 20 years after his injury with the unusual trigger of positional spinal instability due to osteomyelitis and discitis. The patient’s clinical course began when he was diagnosed with L2–3 and L3–4 osteomyelitis, discitis and myositis of the bilateral paraspinous muscles. The infection did not respond well to an attempted course of medical management and degenerated into an unstable spinal segment. This instability in the vertebral column led to positional AD with symptom onset in extension (lying supine) and relieved with flexion (patient sitting up and bending forward). Once the trigger for his AD was determined, he was successfully treated with spinal fusion to stabilize the mobile segment and further antibiotic treatment. He had complete resolution of his AD after surgery and eradication of his infection.
Similar content being viewed by others
Introduction
Autonomic dysreflexia (AD) is a well-known phenomenon associated with spinal cord injury. Common symptoms include: sudden increase in systolic blood pressure (SBP), reflex bradycardia (occasionally tachycardia), blurred vision, anxiety, headaches, flushing, hyperhidrosis and piloerection.1 AD is seen in injuries at or above T6, and can occur in complete and incomplete injuries (although has been reported in patients with injuries as low as T8: Moeller and Scheinberg2 in 1973 JAMA article).3 Nociceptive stimuli below the level of injury results in over activity of sympathetics leading to vessel constriction.1 Common stimuli include distended bladder, constipation, lacerations, tight clothing and sexual intercourse.3 In the case reported here, the nociceptive stimuli was an unstable spinal segment producing symptoms in a positionally dependent manner (supine or in extension). When hypertension is detected by baroreceptors in the aortic arch and carotid body, it stimulates parasympathetics leading to cranial nerve IX- and X-mediated bradycardia. Additional sympathetic inhibitory outflow is sent from the vasomotor centers in the brainstem leading to vasodilation above the level of the injury: flushing and headache. The sympathetic ganglia below the injury do not receive this output and thus sympathetic input prevails. In serious cases, this can lead to pulmonary edema, spinal subarachnoid hemorrhage and seizures.4
Case presentation
We present here a case study of a 47-year-old ASIA A C6–7 tetraplegic male with positional AD secondary to osteomyelitis-induced spinal instability. The patient had a history of tetraplegia secondary to C6–7 cervical spine injury sustained during a motor vehicle collision with subsequent fusion in 1992. In March 2011, he began experiencing episodes of marked hypertension with SBP over 200 accompanied by hyperhidrosis and anxiety when lying down or extending his back. In the months preceding his presentation, he slept sitting upright in a slightly flexed position. Despite these modifications, symptoms became progressively worse and he was ultimately admitted to our hospital in December 2011. On hospital admission, patient was having night sweats and low grade fevers, white blood cell count was elevated at 13 with C-reactive protein (CRP) of 10.2 and erythrocyte sedimentation rate (ESR) of 93. His symptoms, when triggered, were so marked that he was transferred to the intensive care unit for elective endotracheal intubation and optimal medical management. It was only with general anesthesia that we were able to control his AD sufficiently to obtain a prone magnetic resonance imaging (MRI). MRI revealed myositis of the bilateral paraspinous muscles (Figure 1) that was followed by computerized tomography-guided biopsy with unrevealing microbiology. Management options were discussed with the patient, and it was agreed to attempt bracing with a thoracolumbosacral orthodesis brace and broad-spectrum antibiotics, with recommendations from the infectious disease service. The patient’s initial posthospital course was complicated by vancomycin-induced acute kidney injury, and antibiotics were switched to meropenem and daptomycin. With conservative and nonsurgical management, his AD continued.
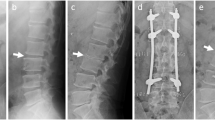
Repeat MRI obtained 2 months after initiation of antibiotics revealed increased involvement of pre and post-vertebral soft tissue, and worsening pyomyositis, establishing the case as refractory to medical management (Figure 2). AD in association with Charcot spine is rare, but well-documented in the literature.4 Although this must certainly be on the differential for our patient, we believe that this is far less likely than progressive discitis and osteomyelitis as the patient’s symptoms began at the same time that he developed fevers, a leukocytosis, an elevated ESR and CRP, and had a contrast enhanced MRI showing a new paraspinal myositis and abnormal signal enhancement of the L2–3 and L3–4 disc spaces consistent with discitis. After discussion with the patient, surgery was planned. A L1–L2 laminectomy, discectomy, decompression, partial vertebrectomy and T11–L4 fusion with placement of an anterior column cage was performed without complication (Figure 3). Intraoperative cultures were unrevealing as the patient had already been on broad-spectrum antibiotics for several months. Postoperatively, the patient was kept on intravenous (IV) antibiotics, and his CRP and ESR were followed closely. He was ultimately discharged to a spinal cord injury rehabilitation unit on antibiotics. His ESR and CRP trended downward and his AD resolved.
Discussion
As stated above, AD following spinal injury is well known to be triggered by nociceptive stimuli, most commonly constipation and bladder retention, and has been extensively documented in the literature.4 We present the unusual case of a C6–7 tetraplegic who developed AD 20 years after his initial injury in the setting of positional vertebral column instabiliity due to L2–3 and L3–4 discitis, and myositis of the bilateral paraspinous muscles. The patient had complete resolution of his AD after spinal fusion and IV antibiotics. AD is known to be mediated by unopposed sympathetic tone below the level of injury leading to vasoconstriction. This sympathetic discharge is caused by nociceptive stimuli and has been documented to be caused by gynecological, urological or gastrointestinal pain, or manipulation. This report clearly illustrates a case where lumbar instability led to medically dangerous hypertension secondary to AD and was relieved by lumbar fusion. This case thus illustrates lumbar osteomyelitis and spinal instability as a previously unrecognized and surgically treatable cause of AD.
References
Milligan J . Autonomic dysreflexia: recognizing a common serious condition in patients with spinal cord injury. Can Fam Physician 2012; 58: 831–835.
Moeller BA Jr, Scheinberg D . Autonomic dysreflexia in injuries below the sixth thoracic segment. JAMA 1973; 224: 1295.
Vaidyanathan S . Autonomic dysreflexia in a tetraplegic patient due to a blocked urethral catheter: spinal cord injury patients with lesions above T-6 require prompt treatment of an obstructed urinary catheter to prevent life-threatening complications of autonomic dysreflexia. Int J Emerg Med 2012; 5: 1–5.
Morita M, Iwasaki M, Okuda S, Oda T, Miyauchi A . Autonomic dysreflexia associated with Charcot spine following spinal cord injury: a case report and literature review. Eur Spine J 2010; 19 (Suppl 2): S179–S182.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sieg, E., Zacko, J. & Hudson, T. Spinal fusion and antibiotic treatment illustrating lumbar osteomyelitis and spinal instability as a previously unrecognized and surgically treatable cause of autonomic dysreflexia. Spinal Cord Ser Cases 2, 16013 (2016). https://doi.org/10.1038/scsandc.2016.13
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.13