Abstract
Study design:
A literature review.
Objectives:
Our aim was to summarise the history, epidemiology, aetiological mechanism, pathological study, clinical and radiological evaluation, treatment and prognosis of subacute posttraumatic ascending myelopathy (SPAM).
Methods:
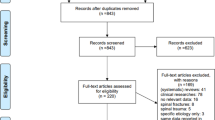
Medical literature on SPAM were searched in the PubMed, Medline, Ovid and Embase databases. The cases of SPAM reported in literature were analysed, and the history, epidemiology, aetiological mechanism, pathological study, clinical and radiological evaluation, treatment and prognosis of SPAM were summarised.
Results:
SPAM remains a relatively rare disorder occurring within the first few weeks after spinal cord injury (SCI). The incidence rate ranges from 0.42% to 1% among all SCI. SPAM is likely to occur in young and middle-aged male patients. Risk factors of SPAM include complete injury, low blood pressure, early postoperative mobilisation and nonsurgical treatment.
Conclusions:
SPAM is well recognised according to typical clinical manifestation and magnetic resonance imaging characteristics. There is no effective therapy for this neurological deterioration. The prognosis of SPAM is poor. There is usually a slight improvement of one or more level(s) below the maximal level of deterioration. The mortality rate is approximately 10%.
Similar content being viewed by others
Introduction
Neurological deterioration after acute spinal cord injury (SCI) is a dreaded complication. The most common type of neurological deterioration is acute deterioration, in which a rise of one or two levels usually occurs. Acute neurological deterioration is reported to occur in up to 5–10% patients with SCI.1, 2 This deterioration usually occurs within the first several hours or days after SCI and is usually temporary. Thus the final neurological lesion is lower or higher than the lesion found immediately after injury.1
Other less common forms of deterioration are subacute and late deterioration. Late deterioration after SCI occurs at least 2 months after injury.3, 4, 5 Posttraumatic syrinx formation and posttraumatic myelomalacia are the leading causes for late neurological deterioration.4, 5
Distinctly unlike acute and late neurological deterioration after SCI, subacute posttraumatic ascending myelopathy (SPAM) remains a relatively rare disorder after SCI, which can be defined as neurological deterioration ascending ⩾4 vertebral levels above the initial injured site and occurring within the first few weeks after SCI, unrelated to mechanical instability or syrinx formation.6, 7, 8, 9, 10, 11, 12, 13
Here we present a literature review of 33 patients with SPAM by reviewing 13 published articles1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 (Table 1) including the epidemiology, aetiological mechanism, pathological study, clinical and radiological evaluation, treatment and prognosis.
Methods
Medical literature on SPAM were searched for in the PubMed, Medline, Ovid and Embase databases. The cases of SPAM reported in literature were analysed and the history, epidemiology, aetiological mechanism, pathological study, clinical and radiological evaluation, treatment and prognosis of SPAM were summarised.
History
Frankel3 was the first to report this type of neurological deterioration in 1969. He first described a patient with a T12 fracture dislocation that led to paraplegia and ascended to C7 after initial injury.3 This case prompted Frankel to examine the records of all similar patients within a 14-year period, but there were only 7 other patients who had had neurological deterioration that ascended at least four segments. However, this type of neurological deterioration was not noticed by other spine and neurosurgeons for 30 years, until 1999 when Aito et al.6 reported a 30-year-old woman who sustained a fracture dislocation of T11/12 with complete Frankel A paraplegia below T11. She received a posterior surgical stabilisation 8 h after injury, and on the twelfth postoperative day, she had a neurological deterioration that was confirmed as SPAM by magnetic resonance imaging (MRI). In the past 20 years, with the development of MRI techniques, SPAM has been gradually recognised and more surgeons have reported cases of SPAM and described its characteristics of clinical manifestation and radiological examinations.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17
Epidemiology
An accurate incidence of SPAM is difficult to ascertain because there were only a few reports of this disorder, and there were no relative statistics on the incidence rate in most published case reports. Depending on the available studies, SPAM incidence ranges from 0.42% to ~1% of all SCI.2, 3, 11 The mortality rate after SPAM is 9%.11 Mortality aside, the relative morbidity associated with SPAM is also high, with many survivors requiring prolonged hospitalisation and even mechanical ventilation.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 14, 15, 16, 17
In the study by Frankel,3 the incidence of SPAM was 1% by reviewing 808 admissions with SCI. However, Frankel found that the incidence of SPAM was higher in the thoracolumbar junction, approximately 2%.3 Yablon et al.2 found one case that ascended four levels after SCI among 134 cases and reported that the incidence rate of SPAM was 0.7%. A study of SPAM evaluated over a 15-year period estimated the incidence to be approximately 0.42%.11
The age distribution of SPAM is shown in Table 2.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Typically, young and middle-aged patients comprise the majority of this disorder, accounting for 90.6% (29/32). In addition, there is a significant sex-related difference in SPAM; males are more likely to suffer from SPAM, and the ratio of males to females is approximately 5:1 (27:5).1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 14, 15, 16, 17
The stratification of SPAM by the original injury level is shown in Table 3.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 More than one-third of SPAM cases had an initial injury in the thoracolumbar spine. The initial injury was more likely to be fracture dislocation and burst fracture with a complete paraplegia or tetraplegia than other types of injury.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 14, 15, 16, 17 The majority of patients with SPAM did not have other significant injuries, such as traumatic brain injury or major chest injuries, except one patient who had a bilateral pulmonary injury.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 14, 15, 16, 17
Aetiological mechanisms of SPAM
Several hypotheses have been postulated to explain the aetiological mechanism of SPAM, including alteration of cerebrospinal fluid (CSF) circulation, great artery of Adamkiewicz (GAA) thrombosis, venous thrombosis and congestive ischaemia, hypotensive ischaemia, infection, apoptosis, secondary injury, arterial thrombosis, inflammatory or autoimmune reaction and meningitis or myelitis. The exact cause remains elusive, but the possible hypotheses are reviewed.
Alteration of CSF circulation
The theory of CSF flow alteration as a cause of SPAM was supported by many authors.10, 11, 15, 18 Obvious CSF pressure elevation after SCI has been shown in preclinical and clinical studies,19, 20, 21 and CSF pressure elevation may lead to neurological dysfunction.22 In a SCI animal model, Jones et al.23 found that the enlarged cord immediately occluded the subarachnoid space in severe SCI, and elevated CSF pressure was only partially decreased by epidural decompressive surgery.19 Although traditional epidural decompression seems adequate during operation, postoperative MRI often reveals that the swollen cord fills the subarachnoid space.24, 25 Planner et al.11 argued that decompression procedures in SPAM patients should normalise this altered CSF flow, making this cause less likely.
Meagher et al.10 postulated that intramedullary haemorrhage, oedema and debris following injury could occlude spinal cord canal drainage. Fischbein et al.18 described a presyrinx state and hypothesised that obstructed CSF flow leads to enlarged spinal cord accompanied by prolonged parenchymal T2 and that the condition was reversible with intervention. Additionally, the response of neurological recovery to cordectomy also supports the proposal that SPAM is secondary to altered CSF drainage.5, 10, 18
The theory of CSF flow alterations as a cause of SPAM correlates well with the time period of clinical symptoms and imaging findings.14 The delayed presentation of SPAM probably reflects the time for tethering of the arachnoid to develop and cause an imbalance in CSF drainage.10 Significant adhesion possibly ensues and the spinal canal is blocked. Then interstitial fluid builds in the cord interstitium and cord oedema ensues in conditions described as progressive posttraumatic myelomalacia, presyrinx or SPAM.10 Although SPAM is often thought to be partly reversible, the persisting increase of the intrathecal pressure may result in intramedullary ischaemia and irreversible neurological deterioration.
GAA thrombosis
The thoracolumbar junction corresponds to the region most frequently entered by the GAA, which is the largest single medullary artery supplying the spinal cord.26 Because most patients with SPAM were injured near the thoracolumbar junction, some authors assumed that a GAA thrombosis was potentially an aetiological factor of SPAM, such as fibrocartilage and nucleus pulposus.6, 16, 17 First, if this were the case, the neurological deterioration would occur abruptly without daily progression,8 and the posterior cord function would be preferentially spared. Second, a selective spinal angiogram of SPAM did not show any evidence of a thrombus in the GAA.8, 12 Third, the involvement pattern on an axial MRI of SPAM appears to be more central rather than anterior and thus does not appear to respect a classic GAA distribution. Finally, it was not supported by an autopsy study.7
Venous thrombosis and congestive ischaemia hypothesis
Venous thrombosis and congestive ischaemia are other possible aetiological mechanisms of SPAM.1, 6, 8, 12 After SCI, 68% of patients demonstrate reversal of the normal haemodynamic gradient, which, in healthy subjects, causes blood to flow from the paravertebral venous plexus to the inferior vena cava.27 The gradient reversal is thought to be due to increased vena caval pressure which, in turn, produces a retrograde elevation of pressure and decreases venous flow in the valveless paravertebral system.27 Impaired venous drainage of the cord after SCI may contribute to early neurological deterioration.1, 6 Additionally, in autopsied cases, venous stasis and infarction involve predominantly central and posterior cord regions,28, 29 which is in accordance with the MRI presentation.17
In cases of SPAM, the central involvement may be explained by the greater sensitivity in grey matter to ischaemia, and the ascending course may be explained by the progression of venous thrombosis. This theory is supported by a case presented by Schmidt12 in which the MRI demonstrated vascular markings consistent with venous congestion. Additionally, the patient appeared to deteriorate after being placed in a sitting position and while wearing a thoracolumbosacral orthotic brace, both of which could increase venous congestion.8, 12 These observations, in conjunction with the central distribution of the MRI signal abnormality and the presence of distended venous markings in the thecal sac, suggest that elevated venous pressures causing venous stasis and ischaemia may contribute to SPAM.12 The role of the venous system in the origin of progressive spinal myelopathy and the reversibility of the myelopathy is well illustrated by cases of spinal arteriovenous fistulas and venous hypertensive myelopathy.30, 31
However, if increased spinal venous pressure and stasis are relatively common among patients with SCI,27 then why is SPAM rarely reported? Furthermore, these associations are not found in all cases of SPAM, suggesting that another mechanism may be involved as well.
Hypotensive ischaemia
Ischaemia as a result of hypotension has been proposed as a mechanism for SPAM.6, 17 In a study of risk factors for neurological deterioration following SCI, Harrop et al.1 found delayed deterioration to be associated with sustained hypotension in patients with fracture dislocations. These changes then cause a decrease in perfusion pressure and ischaemic insult.12, 27 The sitting position may be associated with increased intra-abdominal pressure and an orthostatic blood pressure drop, which may further impair venous return from the paravertebral plexus.6 This may impair cord perfusion leading to an ischaemic insult. This hypothesis is perpetuated by supportive evidence in a few cases where the patient developed symptoms when they began to sit.6, 12
However, this will not explain the progressive nature of SPAM unless there are repeated or sustained episodes of hypotension. Moreover, most patients with SPAM are haemodynamically stable.
Infection
Findings that support the theory of infection include the following: (1) the temporal progression of the ascending myelopathy, (2) pyrexia, and (3) lack of significant recovery,3, 8 which is similar to the manifestation of acute transverse myelitis. Other supportive evidence showed an association between a high blood leucocyte count and neurological deterioration in the first 4 days after SCI.32 Whether these changes in body temperature and the leucocyte count were an association or a cause is hard to establish. Kumar et al.9 declared that an infection, such as acute transverse myelitis, was not the cause of SPAM according to the patient’s response to steroid treatment with clinical and radiological improvement. Furthermore, in the reported CSF and autopsy studies, there was no evidence of infection.8
Apoptosis
As an active form of programmed cell death, apoptosis has a role in the mechanism of central nervous system injury.33, 34, 35 Apoptosis of oligodendrocytes will induce myelin degeneration and cause additional axonal function disturbances.36 Al-Ghatany et al.7 found that apoptotic cells, even at distances remote from the area of the initial injury, can be observed, which provided indirect evidence of a significant role played by apoptosis in the progression of SPAM. However, Al-Ghatany et al.7 acknowledged that apoptosis is unlikely to be the only cause of SPAM. For instance, patients with SPAM frequently improve both clinically and radiographically after subacute deterioration, suggesting that apoptosis may be the end point but not the initiator of SPAM.7
Other hypotheses
Inflammatory reactions and secondary injury after primary SCI have been suggested as possible causes of SPAM.8 However, abundant evidence both from experiments in animals and from studies in humans have demonstrated that inflammatory reactions and processes of secondary injury are most robust immediately after injury.37, 38 Considering that SPAM is not immediate after injury and that the frequency is extremely rare, the suggestion that inflammatory reactions and secondary injury cause SPAM lacks persuasiveness.
Pathological findings
There were only two articles on the pathohistological examination of SPAM published by Al-Ghatany et al.7 and Meagher et al.10
In the study by Al-Ghatany et al.,7 the gross and microscopic findings of the brain and brainstem were normal. No abnormal arterial or venous channels were observed, and the GAA was normal. There was no evidence of fibrocartilaginous emboli or thromboemboli.
Gross examination of the spinal cord with its meninges revealed focal epidural haemorrhage above the injured site (T4). The upper thoracic and cervical spinal cord was soft and had a dusky and patchy haemorrhagic appearance. An inspection of the cross-sections of the lower cervical and thoracic spinal cord revealed patchy to diffuse haemorrhagic softening involving both grey and white matters.7
Microscopy showed infarction and swelling of the entire upper thoracic and lower cervical spinal cord. The infarction was characterised by extensive necrotic dissolution of the spinal cord with active macrophage infiltration and residual oedema. The necrosis was most prominent in the upper thoracic cord at and adjacent to the injured site, but it was also observed in the lower cervical spinal cord. Immunostaining for caspase-3 revealed many apoptotic cells in the upper thoracic cord and even the cervical spinal cord.7
In the study by Meagher et al.,10 they found that there was a cyst formation and the spinal cord had adhered to the dural sac at the injured site. Additionally, cord histology revealed a loss of myelin with vacuolation of the remaining myelin. There was no parenchymal B- or T-cell cord inflammatory change, but there was perivascular cuffing by foamy macrophages within the cord parenchyma and signs of mild T-cell inflammation and fibrosis around the nerve roots.10
Risk factors for SPAM
Risk factors for SPAM include complete SCI,13 injury at the thoracolumbar junction,13 asymptomatic low blood pressure,6, 12 early postoperative orthostatic mobilisation6, 12 and nonsurgical treatment.2
In reported cases with SPAM, the initial injury was almost complete SCI and more likely to be a fracture dislocation and burst fracture with complete paraplegia or tetraplegia than another type of injury.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 According to stratification of SPAM by the original injured level, more than one-third of SPAM cases had an initial injury in the thoracolumbar spine.1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17
In the case described by Aito et al.,6 the patient had an asymptomatically low blood pressure and developed symptoms of SPAM when the patient began to sit upright. In the patient reported by Schmidt,12 there was a low baseline blood pressure noted, and whenever the patient sat upright for physiotherapy, scapular pain and paraesthesia in the upper limbs occurred before the onset of SPAM.12
Early postoperative mobilisation may also induce an orthostatic drop in blood pressure, including spinal arterial pressure, especially in patients with SCI.6, 12 The spinal arterial pressure may impair cord perfusion sufficiently enough to produce an ischaemic insult.6, 12
Yablon et al.2 found that the patients who received surgical treatment by thorough decompression of the cord with rigid internal fixation had a lower incidence of neurological deterioration by comparing the clinical results of 134 patients with SCI.
Clinical evaluation
Although SPAM is a rare neurological deterioration, it is well recognised according to typical clinical manifestation and MRI characteristics. Depending on the extent and function of the spinal cord involved, SPAM may cause motor and sensory deficits varying from partial to complete loss of limb functions, and the higher the level ascended, the more catastrophic the impediments would be. And if the brainstem is involved, patients might suffer from dyspnoea and even death.
Typical characteristics of SPAM are that the patients suffered from neurological deterioration after a few days or weeks of latent clinical stability (Table 4). Some patients complained of pain in the arms, shoulder, scapula, neck, chest or trunk before the appearance of motor weakness.6, 7, 8, 11, 12, 15 Additionally, some patients might complain of paraesthesia, weakness in the upper limbs and arms6, 7, 10, 15 and ascended numbness in the trunk.12, 16 Patients usually had a different degree of fever from low-grade fever to hyperpyrexia.3, 8, 11, 16 Sometimes it might be asymptomatic in some patients with MRI features of SPAM.11 Neurological deficits can ease over time but do not restore to the neurological level before deterioration; the symptoms can also rapidly deteriorate to complete tetraplegia and even dyspnoea, requiring mechanical ventilation in a matter of hours or days8, 10, 11, 15 from the beginning of symptom onset. In some patients, pain subsided over several days without specific treatment.12
A careful neurological assessment, including motor function, sensory evaluation, deep tendon reflexes and perineal evaluation, is critical and required to make the diagnosis of SPAM.
Because each level of spinal cord is associated with unique functional capacity and neurological characteristics, subsequent neurological dysfunction caused by SPAM can have a specific sign. According to the involved levels, patients can have dysesthesia of the trunk, arm and hand,8, 15 ascended paraplegic level7, 11, 12 and decreased muscle strength in the upper limbs and hands.7, 8, 9, 15 Reflexes in the upper limb were sometimes absent.10, 15
Radiological evaluation
Magnetic resonance imaging
MRI is the golden standard of diagnosis of SPAM. Common MRI characteristics of SPAM are as follows:1, 2, 3, 6, 7, 8, 9, 10, 11, 12, 14, 15, 16, 17 MRI usually demonstrates a central area of high-intensity signal on T2-weighted sequences that ascended at least four segments cephalad to the initially injured segment; a maximum of 19 levels ascended has been reported,9 and sometimes the abnormal signal can ascend into the medulla oblongata. The high-intensity signal is tapered at the end of the lesion. There is usually a minimal heterogeneous intramedullary signal on T1-weighted sequences. There is a mild-to-moderate cord expansion with preservation of a normal rim of cord beyond the cord changes, with a syringe that is usually absent. In some cases, diffuse intrathecal haemorrhage can be observed on MRI.
Here we provide a series of typical radiographic dates of a 32-year-old male who suffered from SPAM on posttraumatic day 21 in our hospital (Figures 1, 2, 3).13
Preoperative plain radiography, computerised tomography (CT) scan and MRI showed a T12 burst fracture with severe canal compromise (a–e). (a) X-ray of the thoracolumbar in a lateral view; (b) MRI sagittal view of the thoracolumbar T2-weighted sequence; (c) MRI sagittal view of the thoracolumbar T1-weighted sequence; (d) MRI axial view at the injured site; (e) Axial CT scan at injured site. Postoperative CT scan revealed there was still a canal compromise (f).
Cervical spine MRI performed on posttraumatic day 23. (a) The T2-weighted sequence showed increased signalling and swelling between C2 and the upper thoracic cord. (b) The T1-weighted sequence showed heterogeneous intramedullary signal. (c) Axial T2-weighted image obtained at the C5 level showing an obvious swelling of the cord.
Changes observed on MRI usually did not coincide with the clinical neurological deterioration. MRI changes could occur without a detectable neurological deterioration.11, 15 MRI scans showed improved condition over time.14, 16 Additionally, follow-up imaging of the cord appears atrophic,8, 12 with significant reduction in the cord signal, and swelling with clean borders can be observed in the ascending region on T2W sequences.6, 9, 12 Over 1 year, myelomalacic changes can be observed on MRI, which is characterised by sharply circumscribed areas of high signal intensity in the central and posterior cord on T2-weighted sequences and low signal intensity on T1-weighted sequences.11, 15
After internal fixation, the level of the initial SCI could not be visualised well because of the metal artefact, so some authors stressed the importance of adopting MRI-compatible instruments.6 There was no difference of MRI of SPAM with and without gadolinium.6, 12, 16
Computerised tomography scan
Computerised tomography myelography suggested swelling of the spinal cord, without extrinsic compression at the level above the initial injured site.7
CSF examination
When lumbar puncture was performed, there was usually a complete or incomplete block below the injured site and no block injured site, and the patients also had an increased protein percent and neutrophils.3, 7, 8 CSF might have a remarkable appearance, similar to dishwater, and debris can be observed by microscopy.3 Cultures of the patient’s CSF revealed no bacterium, parasite, virus or tuberculosis.8
Other investigations
On myelography, diffuse swelling of the cord that extended approximately two segments above and below the injured vertebrae2 and a block at the level of the fracture3 could be observed, and there was no significant extrinsic spinal cord compression above the injured site.8
Signs of motor denervation of the muscles innervated by involved level could be detected by electromyography and motor-evoked potentials.6
A selective spinal angiogram demonstrated good opacification of the arterial system and no evidence of thrombosis, vascular anomaly or dural arteriovenous fistula.8, 12
Other investigations, such as colour-coded Doppler ultrasonography of the neck and vertebral vessels, chest radiograph, lung scan, MRI or computerised tomography of the brain and dynamic X-rays of the cervical spine, were carried out during the early stages of deterioration and were all normal.6, 8, 12, 15
Treatment
For the elusive aetiological mechanisms of SPAM and the rarity of this disorder, there was no evidence for the efficacy or superiority of any particular intervention. In addition, it makes the treatment of SPAM a challenge because of poor prognosis.
Supportive treatment
Supportive treatment is addressed by many authors3, 6, 8, 11, 15 including careful monitoring of blood pressure and maintaining blood pressure at a normal level during the acute phase of SCI, close observation of neurological function and paraplegic level to detect neurological deterioration, bedrest to prevent orthostatic hypotension, administration of oxygen and mechanical ventilation if the patients have symptoms of dyspnoea.
Medication therapy
In the literature published to date, a number of conservative treatments have been carried out to treat this condition, including anticoagulation, steroids, broad spectrum antibiotics and osmolar therapy.3, 6, 7, 8, 9, 12, 14, 15, 16, 17 Al-Ghatany et al.7 thought that antiapoptotic pharmacotherapy might be a promising treatment for SPAM, but there was no report about anti-apoptotic treatment in SPAM.
Slight neurological improvement can occur in the majority of cases over time after therapy.3, 6, 8, 9, 11, 14, 17 There was no evidence showing that such medications can improve functional outcomes.3, 7, 12 Therefore, it is difficult to draw a conclusion for or against the use of current treatment in SPAM. There is no consensus on dose or length of treatment12 or correlation with response. The disorder could not be prevented by steroid therapy before the onset of clinical signs.17
Operative therapy
Surgical treatment has been applied to reduce an increased CSF pressure according to the theory of CSF flow alteration in SPAM. Described interventions include epidural decompression by laminectomy,3 untethering of the spinal cord and nerve roots with an expansive duraplasty5 and cordectomy with untethering,10 and all of the interventions have been shown to be effective. Laminectomy can improve the block of CSF at the injured site; cord untethering and cordectomy would allow drainage of interstitial fluid into the epidural space if the central spinal canal is compromised.
One of the patients described by Frankel3 received a laminectomy and was treated with heparin and stopped ascending. In a case of SPAM reported by Meagher et al.,10 a cordectomy with cord untethering was performed at the initial injured site; after 4 weeks, a neurological examination revealed a complete resolution of SPAM. Lee et al.5 described 40 cases with neurological deterioration where all patients had a good response following untethering of the spinal cord and nerve roots with an expansive duraplasty.
However, another author reported that an early surgical decompressive procedure performed in a patient with SPAM failed to reverse the neurological deterioration.17 Additionally, we had a case of SPAM who received a cervical durotomy.13 Unfortunately, the patient failed to show recovery of autonomous respiration and entered coma with a Glasgow coma score of five and died of cerebral hernia.13
Prognosis
The prognosis associated with SPAM varies greatly according to the cord level of ascended myelopathy. In general, after weeks or months of treatment, there is usually a slight improvement of ⩾1 level(s) below the maximal level of deterioration in most patients,3, 8, 9, 10, 11, 14, 16 but sometimes SPAM may be neurologically devastating or even fatal if the level of cord involved ascends, which can result in aspiration of vomitus or respiratory failure7, 11; the mortality rate is approximately 10%.11 Additionally, patients rarely recover to the neurological level before deterioration.10 The clinical recovery was not in accordance with improvement on MRI.9, 11, 14 MRI demonstrated obvious resolution of abnormal cord signal and appeared normal in signal and size cephalad to the injured site, sometimes with a small focal region of myelomalacia cephalad to the injury.10, 11
Conclusion
SPAM remains a relatively rare disorder after SCI, defined as neurological deterioration ascending ⩾4 levels above the initial injured site and occurring within the first few weeks after SCI. The incidence of SPAM ranges from 0.42% to ~1% among all SCI. Typically, young and middle-aged patients comprise the majority of this disorder, accounting for 90.6%. And there is a significant sex-related difference, such that the ratio of males to females is approximately 5:1. Several hypotheses have been postulated to explain the aetiological mechanism of SPAM, but the exact cause remains elusive. Risk factors for SPAM include asymptomatic low blood pressure, early postoperative orthostatic mobilisation and nonsurgical treatment. Although SPAM is rare, it is well recognised according to typical clinical manifestation and MRI characteristics. There is no evidence for the efficacy or superiority of any particular intervention. In addition, it makes the treatment of SPAM a challenge because of its poor prognosis. The prognosis associated with SPAM varies greatly according to the cord level of ascended myelopathy. In general, there was usually a slight improvement of ⩾1 level(s) below the maximal level of deterioration in most patients, but sometimes SPAM may be neurologically devastating or even fatal. The mortality rate is approximately 10%.
Data Archiving
There were no data to deposit.
References
Harrop JS, Sharan AD, Vaccaro AR, Przybylski GJ . The cause of neurologic deterioration after acute cervical spinal cord injury. Spine 2001; 26: 340–346.
Yablon IG, Ordia J, Mortara R, Reed J, Spatz E . Acute ascending myelopathy of the spine. Spine 1989; 14: 1084–1089.
Frankel HL . Ascending cord lesion in the early stages following spinal injury. Paraplegia 1969; 7: 111–118.
Fehlings MG, Austin JW . Posttraumatic syringomyelia. J Neurosurg Spine 2011; 14: 570–572.
Lee TT, Arias JM, Andrus HL, Quencer RM, Falcone SF, Green BA . Progressive posttraumatic myelomalacic myelopathy- treatment with untethering and expansive duraplasty. J Neurosurg 1997; 86: 624–628.
Aito S, EI Masry WS, Gerner HJ, Lorenzo ND, Pellicanò G, D'Andrea M et al. Ascending myelopathy in the early stage of spinal cord injury. Spinal Cord 1999; 37: 617–623.
AI-Ghatany M, AI-Shraim M, Levi AD, Midha R . Pathological features including apoptosis in subacute posttraumatic ascending myelopathy. Case report and review of the literature. J Neurosurg Spine 2005; 2: 619–623.
Belanger E, Picard C, Lacerte D, Lavallee P, Levi AD . Subacute posttraumatic ascending myelopathy after spinal cord injury. Report of three cases. J Neurosurg Spine 2000; 93 (2 Suppl): 294–299.
Kumar A, Kumar J, Garg M, Farooque K, Gamanagatti S, Sharma V . Posttraumatic subacute ascending myelopathy in a 24-year-old male patient. Emerg Radiol 2010; 17: 249–252.
Meagher TM, Belci M, López de Heredia L, Ansorge O, Jamous A, Saif M et al. Resolution of SPAM following cordectomy: implications for understanding pathophysiology. Spinal Cord 2012; 50: 638–640.
Planner AC, Pretorius PM, Graham A, Meagher TM . Subacute progressive ascending myelopathy following spinal cord injury: MRI appearances and clinical presentation. Spinal Cord 2008; 46: 140–144.
Schmidt BJ . Subacute delayed ascending myelopathy after low spine injury: case report and evidence of a vascular mechanism. Spinal Cord 2006; 44: 322–325.
Zhang J, Wang HL, Liu HY, Wang GS . Subacute post-traumatic ascending myelopathy after T12 burst fracture in a 32-year-old male: case report and surgical result of cervical durotomy. Spinal Cord Ser Cases, (e-pub ahead of print 7 July 2016; doi:10.1038/scsandc.2016.4).
Kovanda TJ, Horn EM . Subacute posttraumatic ascending myelopathy in a 15-year-old boy. J Neurosurg Spine 2014; 21: 454–457.
Okada S, Saito T, Kawano O, Hayashida M, Matsumoto Y, Harimaya K et al. Sequential changes of ascending myelopathy after spinal cord injury on magnetic resonance imaging: a case report of neurologic deterioration from paraplegia to tetraplegia. Spine J 2014; 14: e9–e14.
Tan AC, Ng K, Newey A, Leong G . Subacute delayed ascending myelopathy: not just a post-traumatic disorder. Spinal Cord 2014; 52 (Suppl 2): S11–S13.
Visocchi M, Di Rocco F, Meglio M . Subacute clinical onset of postraumatic myelopathy. Acta Neurochir (Wien) 2003; 145: 799–804.
Fischbein NJ, Dillon WP, Cobbs C, Weinstein PR . The ‘presyrinx’ state: a reversible myelopathic condition that may precede syringomyelia. AJNR Am J Neuroradiol 1999; 20: 7–20.
Jones CF, Newell RS, Lee JH, Cripton PA, Kwon BK . The pressure distribution of cerebrospinal fluid responds to residual compression and decompression in ananimal model of acute spinal cord injury. Spine 2012; 37: E1422–E1431.
Horn EM, Theodore N, Assina R, Spetzler RF, Sonntag VK, Preul MC . The effects of intrathecal hypotension on tissue perfusion and pathophysiological outcome after acute spinalcord injury. Neurosurg Focus 2008; 25: E12.
Kwon BK, Curt A, Belanger LM, Bernardo A, Chan D, Markez JA et al. Intrathecal pressure monitoring and cerebrospinal fluid drainage in acute spinal cord injury: a prospective randomized trial. J Neurosurg Spin 2009; 10: 181–193.
Fedorow CA, Moon MC, Mutch WA, Grocott HP . Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: rationale and practical considerations for management. Anesth Analg 2010; 111: 46–58.
Jones CF, Cripton PA, Kwon BK . Gross morphological changes of the spinal cord immediately after surgical decompression in a large animal model of traumatic spinal cord injury. Spine 2012; 37: E890–E899.
Matsuyama Y, Kawakami N, Mimatsu K . Spinal cord expansion after decompression in cervical myelopathy. Investigation by computed tomography myelography and ultrasonography. Spine 1995; 20: 1657–1663.
Harada A, Mimatsu K . Postoperative changes in the spinal cord in cervical myelopathy demonstrated by magnetic resonance imaging. Spine 1992; 17: 1275–1280.
Sliwa JA, Maclean IC . Ischemic myelopathy: a review of spinal vasculature and related clinical syndromes. Arch Phys Med Rehabil 1992; 73: 365–372.
Cassar-Pullicino VN, Colhoun E, McLelland M, McCall IW, el Masry W . Hemodynamic alterations in the paravertebral venous plexus after spinal injury. Radiology 1995; 197: 659–663.
Hughes JT . Venous infarction of the spinal cord. Neurology 1971; 21: 794–800.
Kim RC, Smith HR, Henbest ML, Choi BH . Nonhemorrhagic venous infarction of the spinal cord. Ann Neurol 1984; 15: 379–385.
Pan L, Ma L, Gong J, Yu Z, Zhang X, Li J et al. Venous hypertensive myelopathy caused by narrowing of ascending lumbar vein. Zhonghua Wai Ke Za Zhi 2002; 40: 752–754.
Sugai F, Sumi H, Hara Y, Kajiyama K, Morino H, Fujimura H . An autopsy case of Degos' disease with ascending thoracic myelopathy. Rinsho Shinkeigaku 1998; 38: 1049–1053.
Katoh S, Ikata T, Tsubo M, Hamada Y, el Masry WS . Possible implication of leukocytes in secondary pathological changes after spinal cord injury. Injury 1997; 28: 215–217.
Beattie MS, Farooqui AA, Bresnahan JC . Review of current evidence for apoptosis after spinal cord injury. J Neurotrauma 2000; 17: 915–925.
Crowe MJ, Bresnahan JC, Shuman SL, Masters JN, Beattie MS . Apoptosis and delayed degeneration after spinal cord injury in rats and monkeys. Nat Med 1997; 3: 73–76.
Lu J, Ashwell KW, Waite P . Advances in secondary spinal cord injury: role of apoptosis. Spine 2000; 25: 1859–1866.
Hains BC, Black JA, Waxman SG . Primary cortical motor neurons undergo apoptosis after axotomizing spinal cord injury. J Comp Neurol 2003; 462: 328–341.
Donnelly DJ, Popovich PG . Inflammation and its role in neuroprotection, axonal regeneration and functional recovery after spinal cord injury. Exp Neurol 2008; 209: 378–388.
Fleming JC, Norenberg MD, Ramsay DA, Dekaban GA, Marcillo AE, Saenz AD et al. The cellular inflammatory response in human spinal cords after injury. Brain 2006; 129: 3249–3269.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Zhang, J., Wang, G. Subacute posttraumatic ascending myelopathy: a literature review. Spinal Cord 55, 644–650 (2017). https://doi.org/10.1038/sc.2016.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.175
This article is cited by
-
Post-traumatic syringomyelia resolution following surgical treatment: the moniliform syrinx with a better prognosis
Acta Neurologica Belgica (2023)
-
Very rare incidence of ascending paralysis in a patient of traumatic spinal cord injury: a case report
Spinal Cord Series and Cases (2022)
-
Subacute posttraumatic ascending myelopathy: a literature review
Spinal Cord Series and Cases (2017)