Abstract
Study design:
Cross-sectional study.
Objectives:
To determine the effect of injury duration on plantar-flexor elastic properties in individuals with chronic spinal cord injury (SCI) and spasticity.
Setting:
National Rehabilitation Center for Persons with Disabilities, Japan.
Methods:
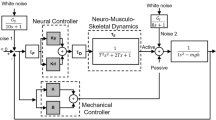
A total of 16 chronic SCI patients (age, 33±9.3 years; injury localization, C6-T12; injury duration, 11–371 months) participated. Spasticity of the ankle plantar-flexors was assessed using the Modified Ashworth Scale (MAS). The calf circumference and muscle thickness of the medial gastrocnemius (MG), lateral gastrocnemius and soleus were assessed using tape measure and ultrasonography. In addition, the ankle was rotated from 10° plantar-flexion to 20° dorsiflexion at 5 deg s−1 with a dynamometer, and the ankle angle and torque were recorded. After normalizing the data (the initial points of angle and torque were set to zero), we calculated the peak torque and energy. Furthermore, angle–torque data (before and after normalization) were fitted with a second- and fourth-order polynomial, and exponential (Sten–Knudsen) models, and stiffness indices (SISOP, SIFOP, SISK) and AngleSLACK (the angle at which plantar-flexor passive torque equals zero) were calculated. The stretch reflex gain and offset were determined from 0–10° dorsiflexion at 50, 90, 120 and 150 deg s−1. After logarithmic transformation, Pearson’s correlation coefficients were calculated.
Results:
MAS, calf circumference, MG thickness, peak torque and SIFOP significantly decreased with injury duration (r log-log=−0.63, −0.69, −0.63, −0.53 and −0.55, respectively, P<0.05). The peak torque and SIFOP maintained significant relationships even after excluding impacts from muscle morphology.
Conclusion:
Plantar-flexor elasticity in chronic SCI patients decreased with increased injury duration.
Similar content being viewed by others
Introduction
Motor paralysis following spinal cord injury (SCI) inevitably prevents daily activities such as upright standing and bipedal walking; consequently, physical activity declines in affected patients. Previous studies have indicated that SCI patients experience extreme muscle atrophy,1, 2, 3 fiber transformation towards a fast-fatigable type4, 5, 6 and decreased bone mineral density.7, 8 This musculoskeletal degeneration is attributed largely to the dramatically decreased muscle activity and mechanical stress in the paralyzed limbs, caused primarily by post-SCI motor paralysis.
Quantitative evaluation of the muscle viscoelasticity and tone is important in preventing secondary disorders after SCI. The Modified Ashworth Scale (MAS) is generally used to measure muscle tone and spasticity,9 but this score lacks adequate sensitivity to distinguish the contributions from the mechanical and neural components.10 In a study of the neural profile after SCI, we reported that spinal reflex excitability in participants experiencing both complete and incomplete SCI are significantly higher than the excitability in healthy young participants, but the Hmax/Mmax did not change significantly in incomplete SCI participants.11 In addition, the change in Hmax/Mmax was not associated with the chronicity of injury in SCI participants. Muscle viscoelasticity is a significant contributor to muscle tone, and it is therefore necessary to understand not only the neural but also the mechanical properties of the paralyzed region in SCI patients. To date, the relationship between the mechanical properties and the duration of injury has not been reported. This information could guide clinicians in determining the appropriate intervention for the patient’s pathologic condition.
The objective of the present study is to determine the effect of injury duration on plantar-flexor elastic properties in individuals with chronic SCI and spasticity.
Patients and methods
Participants
Sixteen participants diagnosed with SCI (age, 33±9 years; height, 172±7 cm; weight, 62±10 kg; injury localization, C6-T12; injury duration, 11–371 months) and spasticity (10 complete and 6 incomplete), five participants with complete SCI without spasticity (age, 30±7 years; height, 174±4 cm; weight, 67±14 kg; injury localization, T9–L3; injury duration, 12–213 months) and 13 healthy control participants (age, 27±5 years; height, 169±10 cm; weight, 62±10 kg; 10 male and 3 female) participated in this study. The population demographics are summarized in Table 1. There was no statistical age difference among the three groups (SCI participants with spasticity, SCI participants without spasticity and healthy participants; F-value=2.075, P=0.1422). Each participant provided written informed consent for the experimental procedure, which was approved by the National Rehabilitation Center for Persons with Disabilities (NRCD).
Measurements
The participants were seated with their hip and knee joints angled at 90°. The ankle joint was fixed onto the foot plate of a custom dynamometer.12 The calf circumference and muscle thickness of the plantar-flexors were measured at 30% of the calf length using a tape measure and ultrasonography (Prosound 2, Aloka, Tokyo, Japan) with a linear array probe (7.5 MHz). The calf circumference, medial gastrocnemius (Gas (MG)) and lateral Gas thicknesses of participants 5, 6 and 8, and four healthy control participants, as well as the soleus (Sol) thickness of participants 1, 5, 6 and 8, and five healthy control participants, were not obtained. We have stated that this lack of data might lead to type I error. The right ankle joint was rotated from 10° of plantar-flexion to 20° dorsiflexion at 5 deg s−1. During the measurement, ankle joint angle and plantar-flexion torque were recorded at a 1 kHz sampling frequency using a 16-bit analog-to-digital converter (Powerlab, AD Instruments, Bella Vista, NSW, Australia). The muscle activity of the Gas, Sol and tibialis anterior were also measured using surface electromyograms with a bipolar electrode (DE-2.3, Delsys, Boston, MA, USA) spaced 1 cm apart. The electromyograms signal was amplified (The Bagnoli-8 EMG System, Delsys) with band-pass filtering between 20 Hz and 450 Hz. Some participants (#1, 2, 3, 4 and 5 in Table 2) had clonus. In those participants, therefore, we took care not to miss the emergence of symptoms by visually monitoring the joint motion and the surface electromyography displayed on an oscilloscope, and if clonus occurred, the experiment was temporarily stopped. The trial was repeated 6–10 times, and five trials without muscle activity of the lower limb were selected and analyzed further. One participant (Table 1, participant 3) showed remarkable muscle activity exceeding±3 s.d. of baseline (Figure 1b), therefore the data from this participant was excluded.
(a) Representative angle and electromyograms (EMG; Gas, Sol, TA) waveform during passive motion test. Broken lines indicate ±3 s.d. of baseline. (b) Angle and EMG waveform of an excluded participant (participant 3 in Table 1).
The passive motion test was then followed by a stretch reflex test in the SCI participants with spasticity and healthy control participants only. Stretch reflexes were elicited by quick 10° toe-up rotations of the footplate from 0° with participants at rest. Four different angular velocities (60, 90, 120 and 150 deg s−1) were applied five times in each participant in a random order. The inter-stimulus intervals were not constant but were randomized within 4–9 s to avoid anticipation of forthcoming perturbations. After all trials, the MAS of the right plantar-flexor was assessed.
Analysis
Angle and torque data were averaged in five trials and digitally low-pass filtered using a fourth-order zero-lag Butterworth filter13 with a 10-Hz cut-off frequency.14, 15, 16 Three different mathematical models were fitted to the angle (θ)–torque (τ) data as previously described:16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27
(i) Second-order polynomial (SOP) model (Equation 1)

where a is experimental constant;
(ii) Fourth-order polynomial (FOP) model (Equation 2)

where m, n, o, p and q are experimental constants;
(iii) Exponential model similar to the Sten–Knudsen (SK) model (Equation 3)

where α and θslack are experimental constants.
Prior to fitting Equation 1, the angle (θ) and torque (τ) data reference points were set to zero. The plantar-flexor, peak torque (torque waveform peak), and energy (the area between the angle–torque curve and the line torque equaling zero) were calculated from the normalized angle–torque data. In Equations 2 and 3, the raw angle–torque data were used. Equation 3 fitting parameters were determined by the non-linear least square method (Levendberg-Marquardt algorithm28) using the optimization toolbox from MATLAB (The Mathworks, Natick, MA, USA). A total of 120016 data points were used in each fitting. The stiffness indices (SISOP, SIFOP, SISK) and AngleSLACK were determined from these equations as follows:




SIFOP is the average of the derivative of the fourth-order polynomial regression of angle–torque curve across all angle ranges (10° plantar-flexion to 20° dorsiflexion). The determination coefficient (R2) of the angle–torque curve fitting using SOP, FOP and SK models was also calculated. The reflex responses were analyzed as the peak-to-peak amplitude for 35 ms after perturbation. The SR gain and offset were calculated as the slope and interception of the regression line in the plotted stretch response to angular velocity.
Statistics
One-way analysis of variance was used to compare the determination coefficients (R2) between the three models, and post hoc analysis was performed using Tukey’s HSD test. All variables were logarithmically transformed29 except the Gas and Sol offsets, which have negative magnitudes. Then, the Spearman’s rank-correlation coefficient for the MAS and the Pearson’s product-moment correlation coefficient for the other variables were calculated to determine the relationship between the injury duration and mechanical parameters. In addition, the relationships between all variables and injury localization were determined using the same procedure. Before logarithmic transformation, MAS values were corrected by designating the minimum data value as one. The partial correlation coefficient, excluding morphological parameters, was also calculated for the mechanical parameters. The statistical significances of the correlation coefficients were assessed for SCI participants with spasticity. Statistical significance was set at P<0.05.
Results
Representative angle–torque data (raw and normalized) and fitting data using the three models are illustrated in Figure 2. In both examples (Figure 2a: participant 12 in Table 1; Figure 2b: participant 13 in Table 1), the FOP model fits the angle–torque data well. However, data fitting using the SOP and SK models is poor in some participants (Figure 2b: participant 13 in Table 1). Similarly, the collective determination coefficient data fitting using the FOP model was very good (R2=0.999±0.001) and significantly higher than in both the SOP (R2=0.869±0.135) and SK (0.904±0.130) models in all the participants (n=33). This trend also occurred and was significant in SCI participants with spasticity (FOP model: R2=0.999±0.001; SOP model: R2=0.850±0.120; SK model: R2=0.883±0.114, n=15). MAS negatively correlated with the injury duration in the SCI participants with spasticity (Figure 3). In addition, the calf circumference and MG thickness were negatively correlated to the injury duration (n=13 excluding the missing data described previously; Figure 3). However, there were no statistically significant relationships between the neural parameters (Gas gain and offset, Sol gain and offset) and injury duration in the group.
Representative angle–torque data fitting using three mathematical models (SOP, FOP and SK). (a) The fitting was good in all models, which were fitted to angle–torque data from participant 12 in Table 1. (b) The SOP and SK model fittings were inferior compared with the FOP model, based on angle–torque data from participant 13 in Table 1.
Relationship between mechanical variables and injury duration (months). Complete SCI participants with spasticity (filled circles), incomplete SCI participants with spasticity (open circles), complete SCI participants without spasticity (x), and healthy participants (horizontal bar) are shown. The horizontal dashed line indicates the mean value in healthy participants.
Angle–torque representative curves of all participants (excluding participant 3) are shown in Figure 4a. After the polynomial and exponential regression, the SIFOP, SISK and AngleSLACK were calculated, and Figure 4b was generated by designating the angle and torque reference points in Figure 4a as zero. Using the data in Figure 4a, we calculated the peak torque, energy and SISOP, and found that the peak torque and SIFOP (stiffness index calculated from the fourth-order polynomial regression) were inversely correlated with the injury duration (n=15).
(a) Angle–torque curves of plantar-flexor muscles for all complete SCI participants with spasticity (chain), incomplete SCI participants with spasticity (solid), complete SCI participants without spasticity (dashed) and healthy control participants (dotted), excluding participant 3. (b) The angle and torque reference points in a were set at zero. (c) Angle–torque curve for SCI participants with spasticity (both complete and incomplete) from a, with grayscale intensities of lines indicating injury duration (months). (d) The angle and torque reference points in c were set at zero.
Muscle morphology theoretically affects passive tension in the muscles and tendons. The effects of these morphologic variables (calf circumference and MG, lateral Gas, and Sol thicknesses) were excluded by calculating the partial correlation coefficients between the mechanical properties (peak torque, energy, SISOP, SIFOP, SISK and AngleSLACK) and the injury duration (Table 2). The peak torque and SIFOP were negatively correlated, even after excluding the effects of the calf circumference and MG thickness, which significantly decreased with the injury duration. In addition, we confirmed that the injury severity was not correlated with these results (Figure 5).
Discussion
We investigated the effect of injury duration on plantar-flexor elasticity in individuals with chronic SCI and found negative correlations between the clinical index of spasticity (MAS), morphologic parameters (calf circumference and MG thickness), mechanical parameters (peak torque and stiffness index) and injury duration in SCI participants with spasticity. In addition, there were significant partial correlation coefficients between the mechanical parameters and the injury duration excluding morphologic parameters.
Alteration of the ankle joint stiffness after SCI
As clearly shown in Figure 3, the decline in calf circumference and MG thickness with injury duration indicates that muscle atrophy continues in SCI even during the chronic stage. Castro et al.2 measured the cross-sectional area of the lower musculature (Gas, Sol and tibialis anterior) during the 6 months following spinal injury and showed that the CSA of Gas decreased significantly. The present result showing a selectively decreased MG thickness is consistent with previous findings.2 Notably, involuntary muscle activity resulting from clonus and spasm with spasticity might contribute to attenuate atrophy,30 therefore the decreasing spasticity observed in this study, coupled with the immobilization, likely accelerated the muscle atrophy.
The Ashworth scale31 remains a major clinical scale for evaluating spasticity,32, 33, 34 but its validity and reliability are questioned by some reports.35, 36 A positive correlation has been reported between the Ashworth scale and indices of clonus and spasm,37 therefore the negative correlation between MAS and the injury duration observed in this study suggest that the frequency of involuntary muscle contraction because of spasm gradually decreases over time after SCI. In evaluating the extent of spasticity over time, we found no statistically significant correlation between the stretch reflex gain and offset in the lower muscles (MG, Sol) and injury duration. This result is consistent with our previous study11 that found that the stretch reflex peak-to-peak amplitude and stretch reflex peak-to-peak amplitude/Mmax in complete and incomplete SCI participants were not correlated to the time post-injury, suggesting that spinal circuit excitability in SCI patients does not change during the chronic stage. However, several reports showed that Mmax was decreased more in the chronic SCI participants than in the age-matched healthy control participants,38, 39, 40, 41, 42, 43, 44 presumably because of the changes in proprioceptor function or muscle atrophy. In these studies, the time-dependent decline in Mmax may be caused by muscle atrophy, but because we did not measure Mmax in our study, we cannot conclude that the spinal reflex excitability in chronic SCI is maintained. Further research is needed to clarify this relationship.
Characteristics of the mechanical properties of the paralyzed ankle joint in SCI
Previous research16 indicates that the mathematical models used to calculate the mechanical parameters greatly impact the experimental result. Essentially, the change in a mechanical parameter (for example, stiffness) varied depending on the selected mathematical model applied to the angle–torque relation; thus, we evaluated several mathematical models (SOP, FOP and SK) to calculate each mechanical parameter. In this study, the peak torque and stiffness index (SIFOP) calculated from the FOP model were inversely correlated with the injury duration. The determination coefficients for the angle–torque data fitted with the FOP model were significantly higher than the coefficients based on the alternative models (SOP, SK), therefore the result (SIFOP) calculated using the FOP model was deemed to be the most reliable. Notably, SISOP, SISK and AngleSLACK calculated using the SOP and SK models were not significantly correlated with the injury duration. This observation likely reflects the inappropriate data fitting observed in some participants and the insufficient sample size; however, the underlying mechanism is unclear.
In addition, work was not significantly correlated with injury duration, which is consistent with a prior study asserting that work is not a spasticity indicator.45 Furthermore, the decreased peak torque and SIFOP over time suggest that plantar-flexor elasticity decreases with injury duration. However, several studies have found that the plantar-flexor passive-elasticity in the chronic SCI patients was higher than observed in the healthy age-matched participants.24, 26, 46 We speculate that plantar-flexor elasticity in SCI patients increases with immobilization during the acute stage of injury (<1 year), and thereafter, elasticity gradually decreases over time due in part to the muscle atrophy observed in this study. In theory, muscle morphology influences passive tension. Thus, we calculated the partial correlation coefficient between mechanical parameters and injury duration to exclude effects from morphological parameters (Table 2); significant relationships persisted, therefore we concluded that tissue elasticity in the plantar-flexor was involved in the mechanical parameter changes.
We cannot determine whether the muscle or tendon caused the plantar-flexor elasticity change. Theoretically, both muscle and tendon arranged in series can affect the total tissue stiffness,47 a relationship that has been experimentally confirmed in the plantar-flexors of healthy participants.17 In contrast, Diong et al.24 observed that the Gas muscle stiffness is increased in SCI participants, whereas Olson et al.6 found that the muscle changes occur at the cell level and reflect muscle fiber transformation from Type I to Type II. In addition, Maganaris48 showed that patellar tendon CSA, stiffness, and Young’s modulus decreased significantly in chronic (18–288 months after injury) complete SCI patients. Overall, these studies suggest that the tendon rather than the muscle has a primary role in the decreasing plantar-flexor elasticity. Further research is needed to clarify the different changes in muscle and tendon function over time following a SCI.
Limitations
We did not measure the range of motion of plantar-dorsiflexion in the SCI participants. Therefore, it is unclear whether contracture occurred in SCI participants. However, we visually confirmed that all participants achieved a 20° dorsiflexion while keeping the heel in contact with the dynamometer footplate during the passive motion test. In addition, we confirmed that muscle activity in the calf muscles (MG, Sol) and antagonist (tibialis anterior) were low (within the baseline mean±3 s.d.) during the passive motion test (representative participant in Figure 2a). Thus, the influence of articular alternation and muscle activity on the plantar-flexor torque was minimal, and the passive motion test was conducted appropriately.
In conclusion, the degree of spasticity (MAS), morphologic (circumference and MG muscle thickness) and mechanical (muscle-tendon elasticity) properties of the plantar-flexors in chronic SCI patients with spasticity decreased with the injury duration. Therapeutic intervention, such as FES or BWST, may be needed to prevent these sequelae in chronic SCI patients.
DATA ARCHIVING
There were no data to deposit.
References
Lotta S, Scelsi R, Alfonsi E, Saitta A, Nicolotti D, Epifani P et al. Morphometric and neurophysiological analysis of skeletal muscle in paraplegic patients with traumatic cord lesion. Paraplegia 1991; 29: 247–252.
Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA . Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol 1999; 80: 373–378.
Castro MJ, Apple DF, Staron RS, Campos GE, Dudley GA . Influence of complete spinal cord injury on skeletal muscle within 6 mo of injury. J Appl Physiol 1999; 86: 350–358.
Grimby G, Broberg C, Krotkiewska I, Krotkiewski M . Muscle fiber composition in patients with traumatic cord lesion. Scand J Rehabil Med 1976; 8: 37–42.
Martin TP, Stein RB, Hoeppner PH, Reid DC . Influence of electrical stimulation on the morphological and metabolic properties of paralyzed muscle. J Appl Physiol 1992; 72: 1401–1406.
Olsson MC, Krüger M, Meyer LH, Ahnlund L, Gransberg L, Linke WA et al. Fibre type-specific increase in passive muscle tension in spinal cord-injured subjects with spasticity. J Physiol 2006; 577: 339–352.
Frey-Rindova P, de Bruin ED, Stüssi E, Dambacher MA, Dietz V . Bone mineral density in upper and lower extremities during 12 months after spinal cord injury measured by peripheral quantitative computed tomography. Spinal Cord 2000; 38: 26–32.
Szollar SM, Martin EM, Sartoris DJ, Parthemore JG, Deftos LJ . Bone mineral density and indexes of bone metabolism in spinal cord injury. Am J Phys Med Rehabil 1998; 77: 28–35.
Biering-Sørensen F, Nielsen JB, Klinge K . Spasticity-assessment: a review. Spinal Cord 2006; 44: 708–722.
Grippo A, Carrai R, Hawamdeh Z, Falsini C, Aito S, Pinto F et al. Biomechanical and electromyographic assessment of spastic hypertonus in motor complete traumatic spinal cord-injured individuals. Spinal Cord 2011; 49: 142–148.
Nakazawa K, Kawashima N, Akai M . Enhanced stretch reflex excitability of the soleus muscle in persons with incomplete rather than complete chronic spinal cord injury. Arch Phys Med Rehabil 2006; 87: 71–75.
Kawashima N, Suzuki R, Nakazawa K, Ohta Y . Novel home-based rehabilitation device to prevent secondary diseases for patients with spinal cord injury. 2009 IEEE Int Conf Rehabil Robot 2009, 349–353.
Winter DA . Biomechanics and Motor Control of Human Movement. John Wiley & Sons. 1990.
Fouré A, Nordez A, Cornu C . Effects of plyometric training on passive stiffness of gastrocnemii muscles and Achilles tendon. Eur J Appl Physiol 2012; 112: 2849–2857.
Fouré A, Nordez A, Cornu C . Effects of eccentric training on mechanical properties of the plantar flexor muscle-tendon complex. J Appl Physiol 2013; 114: 523–537.
Nordez A, Cornu C, McNair PJ . Acute effects of static stretching on passive stiffness of the hamstring muscles calculated using different mathematical models. Clin Biomech 2006; 21: 755–760.
Kawakami Y, Kanehisa H, Fukunaga T . The relationship between passive ankle plantar flexion joint torque and gastrocnemius muscle and achilles tendon stiffness: implications for flexibility. J Orthop 2008; 38: 269–276.
Sten-Knudsen O . Torsional elasticity of the isolated cross striated muscle fibre. Acta Physiol Scand 1953; 28: 1–240.
Nordez A, Fouré A, Dombroski EW, Mariot JP, Cornu C, McNair PJ et al. Improvements to Hoang et al.'s method for measuring passive length-tension properties of human gastrocnemius muscle in vivo. J Biomech 2010; 43: 379–382.
Nordez A, Casari P, McNair PJ, Cornu C . Characterization and modelling of the musculoarticular complex mechanical behavior in passive conditions. Effects of cyclic and static stretching. IRBM 2009; 30: 20–29.
Diong J, Harvey LA, Kwah LK, Clarke JL, Bilston LE, Gandevia SC et al. Gastrocnemius muscle contracture after spinal cord injury: a longitudinal study. Am J Phys Med Rehabil 2012; 92: 1–10.
Hoang PD, Gorman RB, Todd G, Gandevia SC, Herbert RD . A new method for measuring passive length-tension properties of human gastrocnemius muscle in vivo. J Biomech 2005; 38: 1333–1341.
Hoang PD, Herbert RD, Todd G, Gorman RB, Gandevia SC . Passive mechanical properties of human gastrocnemius muscle tendon units, muscle fascicles and tendons in vivo. J Exp Biol 2007; 210: 4159–4168.
Diong JH, Herbert RD, Harvey LA, Kwah LK, Clarke JL, Hoang PD et al. Passive mechanical properties of the gastrocnemius after spinal cord injury. Muscle Nerve 2012; 46: 237–245.
Magnusson SP, Simonsen EB, Aagaard P, Kjaer M . Biomechanical responses to repeated stretches in human hamstring muscle in vivo. Am J Sports Med 1996; 24: 622–628.
Kwah LK, Herbert RD, Harvey LA, Diong J, Clarke JL, Martin JH et al. Passive mechanical properties of gastrocnemius muscles of people with ankle contracture after stroke. Arch Phys Med Rehabil 2012; 93: 1185–1190.
Diong JHL, Herbert RD, Kwah LK, Clarke JL, Harvey LA . Mechanisms of increased passive compliance of hamstring muscle-tendon units after spinal cord injury. Clin Biomech 2012; 27: 893–898.
Marquardt D . An algorithm for least-squares estimation of nonlinear parameters. J Soc Ind Appl 1963; 151: 859–860.
Erni T, Dietz V . Obstacle avoidance during human walking: learning rate and cross-modal transfer. J Physiol 2001; 534: 303–312.
Gorgey AS, Dudley GA . Spasticity may defend skeletal muscle size and composition after incomplete spinal cord injury. Spinal Cord 2008; 46: 96–102.
Ashworth B . Preliminary trial of carisoprodol in multiple sclerosis. Practitioner 1964; 192: 540–542.
Bohannon R, Smith M . Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987; 67: 206–207.
Ghotbi N, Ansari NN, Naghdi S, Hasson S, Jamshidpour B, Amiri S . Inter-rater reliability of the Modified Modified Ashworth Scale in assessing lower limb muscle spasticity. Brain Inj 2009; 23: 815–819.
Rekand T . Clinical assessment and management of spasticity: a review. Acta Neurol Scand 2010; 122: 62–66.
Malhotra S, Pandyan AD, Day CR, Jones PW, Hermens H . Spasticity, an impairment that is poorly defined and poorly measured. Clin Rehabil 2009; 23: 651–658.
Fleuren KS, Voerman GE, Erren-Wolters CV, Snoek GJ, Rietman JS, Hermens HJ et al. Stop using the Ashworth Scale for the assessment of spasticity. J Neurol Neurosurg Psychiatry 2010; 81: 46–52.
Benz EN, Hornby TG, Bode RK, Scheidt RA, Schmit BD . A physiologically based clinical measure for spastic reflexes in spinal cord injury. Arch Phys Med Rehabil 2005; 86: 52–59.
Pelletier CA, Hicks AL . The length-tension relationship of human dorsiflexor and plantarflexor muscles after spinal cord injury. Spinal Cord 2010; 48: 202–206.
Stein RB, Gordon T, Jefferson J, Sharfenberger A, Yang JF, de Zepetnek JT et al. Optimal stimulation of paralyzed muscle after human spinal cord injury. J Appl Physiol 1992; 72: 1393–1400.
Thomas C . Contractile properties of human thenar muscles paralyzed by spinal cord injury. Muscle Nerve 1997; 20: 788–799.
Huang C-Y, Wang C-H, Hwang I-S . Characterization of the mechanical and neural components of spastic hypertonia with modified H reflex. J Electromyogr Kinesiol 2006; 16: 384–391.
Calancie B, Broton JG, Klose KJ, Traad M, Difini J, Ayyar DR . Evidence that alterations in presynaptic inhibition contribute to segmental hypo- and hyperexcitability after spinal cord injury in man. Electroencephalogr Clin Neurophysiol 1993; 89: 177–186.
Murillo N, Kumru H, Vidal-Samso J, Benito J, Medina J, Navarro X et al. Decrease of spasticity with muscle vibration in patients with spinal cord injury. Clin Neurophysiol 2011; 122: 1183–1189.
Boorman GI, Lee RG, Becker WJ, Windhorst UR . Impaired ‘natural reciprocal inhibition’ in patients with spasticity due to incomplete spinal cord injury. Electroencephalogr Clin Neurophysiol 1996; 101: 84–92.
Akman MN, Bengi R, Karatas M, Kilinç S, Sözay S, Ozker R . Assessment of spasticity using isokinetic dynamometry in patients with spinal cord injury. Spinal Cord 1999; 37: 638–643.
Mirbagheri MM, Barbeau H, Ladouceur M, Kearney RE . Intrinsic and reflex stiffness in normal and spastic, spinal cord injured subjects. Exp Brain Res 2001; 141: 446–459.
Cook CS, McDonagh MJ . Measurement of muscle and tendon stiffness in man. Eur J Appl Physiol Occup Physiol 1996; 72: 380–382.
Maganaris CN, Reeves ND, Rittweger J, Sargeant AJ, Jones DA, Gerrits K et al. Adaptive response of human tendon to paralysis. Muscle Nerve 2006; 33: 85–92.
Acknowledgements
This study was partially supported by the KAKENHI (24700581) and the Japanese Ministry of Health, Labour, and Welfare (201224026A and 201317009A).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yaeshima, K., Negishi, D., Yamamoto, S. et al. Mechanical and neural changes in plantar-flexor muscles after spinal cord injury in humans. Spinal Cord 53, 526–533 (2015). https://doi.org/10.1038/sc.2015.9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.9