Abstract
Premenstrual symptoms are common, with premenstrual syndrome and premenstrual dysphoric disorder associated with decreased wellbeing and increased suicidality. Apps can offer convenient support for premenstrual mental health symptoms. We aimed to understand app preferences and Health Belief Model (HBM) constructs driving app use intention. An online survey was delivered. Structural equation modelling (SEM) explored HBM constructs. Data from 530 United Kingdom based participants who reported their mental health was impacted by their menstrual cycle (mean age = 35.85, SD = 7.28) were analysed. In terms of preferred app features, results indicated that symptom monitoring (74.72%, n = 396) and psychoeducation (57.92%, n = 307) were sought after, with 52.64% (n = 279) indicating unwillingness to pay for an app for mental health symptoms related to the menstrual cycle. Regarding HBM results, Satorra–Bentler-scaled fit statistics indicated a good model fit (χ2(254) = 565.91, p < 0.001; CFI = 0.939, RMSEA = 0.048, SRMR = 0.058). HBM constructs explained 58.22% of intention to use, driven by cues to action (β = 0.49, p < 0.001), perceived barriers (β = −0.22, p < 0.001), perceived severity (β = 0.16, P = 0.012), and perceived benefits (β = 0.10, p = 0.035). Results indicate that app developers should undertake co-design, secure healthcare professional endorsement, highlight therapeutic benefits, and address barriers like digital discomfort, privacy concerns, and quality.
Similar content being viewed by others
Introduction
Premenstrual symptoms are a collection of psychological, behavioural, and physical symptoms occurring during the luteal phase of the menstrual cycle, typically improving following the onset of menstrual bleeding1. Premenstrual symptoms are common, with most women experiencing at least one2. Moreover, premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD), which are characterised by more severe symptom presentation and functional impairment, are reportedly experienced by around 50%3 and up to 18% of women4, respectively. PMS and PMDD are cyclical disorders that are associated with poorer wellbeing and occupational functioning2, with PMDD further linked to an increased risk for suicidality5.
Digital avenues of help-seeking appear to be well-accepted by women in the United Kingdom generally (UK6) as well as specifically for premenstrual mental health symptoms7,8. Additionally, smartphone ownership was estimated to be at 92% in the UK population as of March 20219, making digital delivery of healthcare via apps scalable for healthcare services and commissioners and convenient for users. Applications (apps) offering support for mental health concerns (e.g., depression, anxiety conditions) in the general population have demonstrated evidence of efficacy10 and appear to be a well-accepted method of delivery for assessment, monitoring, and treatment both outside of and as an adjunct to formal mental health services11,12. Given the overlapping symptom profiles of common mental health disorders, for which effective apps are already available, and premenstrual symptoms, there is an opportunity to develop similar apps for PMS and PMDD. Currently, to our knowledge, there are few apps available specifically for PMS and PMDD. Many period tracking apps also offer mood and premenstrual symptom tracking13 which can be leveraged for insights, but offerings of a dedicated platform are minimal with few examples. One such example is the app “Me vs. PMDD” developed by the International Association for Premenstrual Disorders14. There is some limited evidence of the efficacy of apps for premenstrual symptoms and disorders, with period tracking apps being reportedly effective for management of PMS symptoms, including improving the understanding of the relationship between the menstrual cycle and mood15,16. Additionally, there is evidence that a period tracking app which additionally offers health information and lifestyle change recommendations was associated with reductions in depressive symptoms17. The authors hypothesised this improvement was due to an improved understanding of premenstrual symptoms which may have encouraged help-seeking, in combination with positive lifestyle changes17.
There are also opportunities to develop apps which can deliver more sophisticated management and support alongside symptom tracking. There is early evidence of the effectiveness of internet delivered cognitive behavioural therapy (CBT18,19). Internet delivered CBT has been shown to improve the symptoms of PMS and PMDD, with no evidence of negative long-term side-effects18,19. Moreover, there is evidence of online spaces being leveraged for peer support for PMS and PMDD8. Both CBT and peer support delivered via the internet are prime candidates for translation into app-based delivery. There are likely more app features which are sought by individuals with premenstrual symptoms, and so insights into this is important for delivering highly relevant apps to the symptoms of interest.
Given that the efficacy of apps for premenstrual mental health symptoms will hinge on the acceptability and by extension the engagement rate20, identifying preferred app features and health behaviour factors implicated in intention to use is crucial21. However, to our knowledge little has been recorded in the literature regarding user preferences for, and factors influencing usage of, such apps. Considering the potential value of these insights, the current study aimed to fill this research gap by applying the health belief model (HBM22).
The HBM attempts to predict engagement with health behaviours (e.g., medication adherence, engaging with psychological therapies) through six constructs including: 1) perceived benefits (i.e., the perceived benefits associated with using a mental health app for mental health symptoms related to the menstrual cycle (e.g., prevent interpersonal problems, improve performance in the workplace)), 2) perceived barriers (i.e., perceived obstacles associated with using a digital mental health app for mental health symptoms related to the menstrual cycle (e.g., potential financial costs, the risk of potential loss of sensitive data)), 3) perceived susceptibility (i.e., the perceived likelihood or vulnerability of experiencing mental health problems related to the menstrual cycle), 4) perceived severity (i.e., the perceived severity of mental health symptoms related to the menstrual cycle (e.g., mental health symptoms are serious, mental health symptoms have a negative impact on day-to-day life)), 5) self-efficacy (i.e., belief in possessing the resources (e.g., a smartphone, a computer), and the skills (e.g., able to download an app, able to navigate an app) to use an app for mental health symptoms related to the menstrual cycle), and 6) cues to action (i.e., a prompt which would encourage use of an app for mental health symptoms related to the menstrual cycle (e.g., recommended by a HCP, advertised on social media)). In the current study, the health behaviour of interest was intention to use an app for premenstrual mental health symptoms. The HBM has been previously used in studies evaluating the impact and potential uptake of mobile health interventions. Such studies include investigating the impact of text messages and phone calls on health behaviours (e.g., medication adherence) for physical health conditions (e.g., stroke, hypertension, HIV/AIDs23) as well as intention to use and engage in continued use of apps for COVID-19 contact tracing24,25. Outside of mobile health, the HBM has also been used to identify factors implicated in mental health help-seeking in young people26. Additionally, the HBM has been employed to evaluate health belief constructs associated with promoting preventative health behaviours for women’s health conditions associated with menstruation such as iron deficiency anaemia and menstrual pain27. Given that the use of the HBM in these studies are highly relevant to the current focus of the study, it was deemed that the HBM would be an appropriate measure of intention to use an app for premenstrual mental health symptoms.
The current study employed an exploratory approach, with the aims of: (1) understanding preferences for apps designed for premenstrual mental health symptoms and (2) exploring the HBM constructs implicated in intention to use an app for premenstrual mental health symptoms using a structural equation modelling (SEM) approach.
Results
Sociodemographic and premenstrual characteristics
578 participants who had completed at least 97% of the survey indicated that they had experienced premenstrual mental health concerns. 91.70% (n = 530) of these had complete data. Data from these participants were analysed (N = 530), meeting the sample size requirements for SEM.
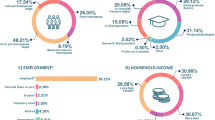
The majority of participants identified as female (95.66%, n = 507) and were white (94.15%, n = 499). The mean age of participants was 35.85 (SD = 7.28). See Table 1 for sociodemographic characteristics.
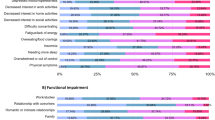
100% of the sample (N = 530) endorsed at least one premenstrual symptom to at least a mild severity. The most frequently endorsed premenstrual symptoms (Fig. 1) were physical symptoms (e.g., breast tenderness, headaches; 96.42%; n = 511) followed by increased anger and irritability (95.85%, n = 508). Fatigue/lack of energy was the symptom most frequently reported as severe (36.23%, n = 192). 97.17% (n = 515) reported their premenstrual symptoms impacted functioning to at least a mild extent in at least one area. The most frequently impaired aspect of domain of functioning was work/studies (83.40%, n = 442). Romantic or intimate relationships was the domain of functioning reported as most severely impacted by premenstrual symptoms (15.85%, n = 84).
Preferences for and interest in an app designed for premenstrual mental health symptoms
When respondents were asked to select three features to be included in their ideal mental health app, the most sought-after feature was monitoring symptoms over time (74.72%, n = 396; Fig. 2) followed by psychoeducation (i.e., resources to improve understanding of one’s mental health; 57.92%, n = 307). 52.64% (n = 279) said they would not be willing to pay for an app for premenstrual mental health symptoms. Of those who were willing to pay (47.36%, n = 251), there was a preference for a one-off payment (65.74%, n = 165) over subscription payments (34.26%, n = 86).
Structural model
HBM descriptives and correlations are displayed in Tables 2 and 3. Internal consistency (α) of the HBM questionnaire was 0.76 (Table 2). The mean behavioural intention score was 4.67 (on a scale from 1 = “strongly disagree” to 6 = “Strongly agree”; Table 2), indicating interest in using an app for premenstrual mental health symptoms.
In order to explore the association between individual HBM items and behavioural intention, Spearman rank-order correlation coefficients were calculated (Table 3). Cues to action (r = 0.45, p < 0.001), perceived benefits (r = 0.45, p < 0.001), perceived severity (r = 0.33, p < 0.001) and perceived susceptibility (r = 0.22, p < 0.001) were all significantly and positively correlated with behavioural intention. The perceived barriers construct was significantly, negatively correlated with behavioural intention (r = −0.36, p < 0.001). No significant correlation was revealed between self-efficacy and behavioural intention (r = 0.83, p = 0.057).
Differences in HBM item scoring based on sociodemographic characteristics were explored (Table 4, Supplementary Materials Table 1). Differences were observed in HBM item scoring between those in current paid employment (i.e., full-time or part-time employment, self-employed) and those who were not in paid employment. Specifically, both perceived susceptibility (in paid employment: mean = 3.78, SD = 1.01; not in paid employment: mean = 4.06, SD = 0.90; U = 5.88, p = 0.015) and perceived severity (in paid employment: mean = 3.94, SD = 1.24; not in paid employment: mean = 4.51, SD = 1.07; U = 18.76, p < 0.001) had lower mean scores than those engaged in paid employment. Age was significantly negatively correlated with perceived severity (i.e., as age increases perceived symptom severity decreases; r = −0.15, p = 0.001). Highest educational attainment was significantly negatively correlated with perceived benefits (r = −0.11, p = 0.013), perceived severity (r = −0.12, p = 0.007), and behavioural intention (r = −0.10, p = 0.031; i.e., lower academic achievement was associated with lower perceived benefits, lower perceived symptom severity, and with lower behavioural intention). Highest educational attainment was additionally significantly positively associated with self-efficacy (r = 0.15, p = 0.001; i.e., perception of self-efficacy increases with increased academic achievement). Annual household income was significantly negatively correlated with perceived benefits (r = −0.11, p = 0.014), perceived barriers (r = −0.10, p = 0.033), perceived susceptibility (r = −0.19, p = 0.001), and behavioural intention (r = −0.09, p = 0.046; i.e., as household income increases, perceived benefits, perceived barriers, perceived susceptibility, and behavioural intention decrease). Annual household income was also significantly positively associated with self-efficacy (r = 0.12, p = 0.012; i.e., perceived self-efficacy increases with increased annual household income).
A structural equation model was constructed to establish the consistency of the observed variables with the proposed latent variables of the HBM (i.e., perceived benefits, perceived barriers, perceived susceptibility, perceived severity, self-efficacy, cues to action). Additionally, the model intended to explore the relationships between these HBM variables and the outcome variable (behavioural intention). The results of the Satorra–Bentler-scaled fit statistics indicate a good model fit (χ2(254) = 565.91, P < 0.001; CFI = 0.939, RMSEA = 0.048, SRMR = 0.058). See Fig. 3 for the model schema (please note, to optimise readability, covariates are not presented in this figure). See the Supplementary Materials for the model schema with all covariates. All factor loadings between our observed and latent variables were significant, and above 0.27.
To see the original model schema from Stata with no covariates as well as the model schema with all covariates please see the Supplementary Material.) *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
Analyses revealed that the constructs of the HBM explained 58.22% of the variance in behavioural intention. The most important predictor of intention was cues to action (β = 0.49, P < 0.001), followed by perceived barriers (β = −0.22, P < 0.001), severity (β = 0.16, P = 0.012), and benefits (β = 0.10, P = 0.035). Self-efficacy (β = −0.01, P = 0.667) and perceived susceptibility (β = 0.07, P = 0.332) were not significantly associated with behavioural intention.
Discussion
The current study aimed to understand preferences for and factors influencing intention to use an app for premenstrual mental health symptoms. These findings have the potential to inform the design of apps for premenstrual mental health symptoms by understanding factors implicated in engagement.
In terms of preferred app features, the most sought-after feature was mental health symptom monitoring. Symptom monitoring can enable increased self-awareness of one’s mental health28, with the potential to improve symptoms28. Previous research has shown that period tracking apps are utilised to identify, monitor, and manage patterns between the menstrual cycle and mental health15. This functionality instils a sense of empowerment in those with PMS, provided it is not deemed overly intrusive or commercial16. Period tracking apps additionally offer a convenient method for establishing the presence of premenstrual symptoms in consecutive cycles, a requirement for a formal diagnosis of PMS or PMDD29. Despite these therapeutic benefits, mood-tracking apps are often lacking in functionality to support users’ interpretation of symptom data28. Therefore, blending period and mental health symptom tracking with supplementary psychoeducation, which was identified as an attractive app feature in the current study, into a single app would offer holistic monitoring, education, self-help, and act as an aid to diagnosis. Indeed, psychoeducation has demonstrated efficacy in increasing PMS knowledge and reducing PMS symptom severity30.
Regarding cost, participants in the current study showed a strong preference for free apps, reflecting previous work demonstrating that paywalls are a barrier to uptake31,32. Interestingly, as the majority of the current sample had a higher annual household income than the median household income of the UK of £32,300 as of 202233 a paywall may be a barrier to uptake for reasons other than affordability. One potential explanation is that users do not perceive apps to offer a reasonable return on investment32,34. An avenue to address this is to provide a free version of the app with basic features, allowing users to upgrade for access to more sophisticated features, a strategy adopted by many publicly available mental health apps35. Critically, user reviews of apps that have adopted the “freemium” model demonstrate negative experiences associated with poor descriptions of features behind a paywall, restricted access to data and therapeutic features, and incomplete treatment programmes35. Therefore, whilst creating free apps should be prioritised from a user engagement, experience, and clinical outcomes standpoint, if apps require payment, we encourage app developers to engage in transparent communication of the features available behind the paywall.
The HBM constructs of cues to action, perceived barriers, perceived severity, and perceived benefits were identified as significant predictors of behavioural intention, with the model explaining almost 60% of variance. These findings should be considered in light of the fact that the HBM items were pre-selected and presented to the participants. Therefore, there could be other factors which may have better captured participants’ health beliefs. Future work may wish to incorporate a Delphi component36 in the design of HBM items to identify key factors related to each construct which may contribute to intention to use. Cues to action was identified as the strongest predictor of intention. Within this construct, as defined by the current study, there appears to be an interest in apps that are co-designed with mental healthcare professionals or trusted institutions. Co-design is essential for the development and delivery of high-quality care37, and expert input into app design and content will likely assuage concerns about low-quality content or misinformation. Additionally, the app being recommended by a HCP was another strong component driving cues to action in the current study. This corroborates previous findings demonstrating the influence of a HCP in engaging with digital mental health interventions38, with endorsement of an app from a HCP, particularly if the HCP is a mental healthcare specialist, increasing interest in the app39. In light of this, app developers should, as standard, co-design tools with experts from healthcare and academia to ensure relevancy and quality of content. Additionally, promoting the app directly to HCPs will raise awareness of available digital resources enabling digital signposting and referral options for patients who present with premenstrual mental health symptoms.
Another significant predictor of intention was perceived barriers. Perceived barriers being identified as highly important to behavioural intention in the current study is in-line with the results of a meta-analysis of the effectiveness of the four core constructs of the HBM (i.e., excluding cues to action and self-efficacy40). This meta-analysis demonstrated that this construct consistently had the largest impact on the likelihood of engaging with a health behaviour40. Among the items presented to participants related to perceived barriers in the current study, a lack of comfort and concerns regarding quality were both highly implicated. Lack of comfort with digital tools is likely multifaceted; firstly, there is reported apprehension related to using digital tools for mental health due to the perceived lack of human connection41. Secondly, mental health apps potentially collect and analyse sensitive data, resulting in concerns about data privacy12. Few publicly available apps address these concerns, with many mental health and women’s health apps not including a privacy policy42,43,44, and few seeking consent from user44, driving mistrust. Privacy policies in apps that do include them typically score low on readability42, reducing users’ ability to provide consent44. Given this, app developers should endeavour to provide an accessible privacy policy which provides details on how the data they provide is analysed and stored. Using language which is clear and jargon-free may reassure users and increase trust. Moreover, adopting opt-in data sharing wherein users are explicitly asked to provide consent for specific types of data to be collected will likely further build trust.
App quality was additionally identified as a component of perceived barriers as defined by the current study, with participants indicating concerns that an app would not be able to understand their mental health symptoms. Concerns about app quality are frequent, with beliefs about efficacy influencing engagement31 to the extent that not providing evidence of an app’s efficacy potentially constitutes a barrier to app usage38. Taken together, the perceived barriers constructs as defined by the current study indicated that intention to use may be increased through addressing potential barriers to app uptake. App developers may achieve this through including features that support human connection (e.g., peer support, data sharing with HCPs), engaging in transparent communication regarding app privacy as described above, and sharing evidence of quality.
Perceived severity was identified as another key predictor of behavioural intention. This mirrors previous work demonstrating that increased symptom severity is associated with increased formal help-seeking45 and interest in digital mental health tools31. However, despite higher symptom severity being associated with increased interest in digital tools for mental health, this interest does not necessarily translate to real-world usage31. For example, higher baseline symptom severity prior to digital treatment is associated with lower engagement measured by uptake and programme completion46. Therefore, further work is required to understand the impact of severe premenstrual mental health symptoms on real-world app adoption and sustained use.
The final predictor of intention to adopt an app for premenstrual mental health symptoms was perceived benefits, emphasising the need for effective communication of benefits the app can confer to potential users. In the current study, a burden being lifted with increased understanding of mental health symptoms was highly implicated as a benefit. This is a common sentiment in those who have received a diagnosis of PMDD, with reports of patients feeling relieved and perceiving increased self-worth by reframing their symptoms through the lens of improved understanding offered by their diagnosis47. Moreover, alleviating problems with loved ones, which is frequently reported by those with PMDD47, was identified as a candidate for driving perceived benefits and thus app uptake. App developers should evaluate the benefits their tool can deliver, ensure these are valuable to the population of interest, and ensure benefits are well communicated.
Notably, contrary to the HBM both self-efficacy and perceived susceptibility were not significantly predictive of intention to use. Regarding self-efficacy, this is likely a reflection of the high digital access and literacy of the study population. Whilst self-efficacy was not implicated in intention to use in the current study, we strongly urge that this is not interpreted as it being unimportant, given the characteristics of the sample. Access to and competency in using technology is essential for engaging with mental health apps, with a risk of digital healthcare excluding already disadvantaged groups48. As such, app developers should ensure they are not contributing to the digital divide in terms of narrowing access to support. This may be achieved through adapting digital resources for non-digital delivery where possible, such as printable psychoeducation.
Similar to self-efficacy, perceived susceptibility was not a significant predictor of intention to use an app for mental health symptoms related to the menstrual cycle. Importantly, perceived susceptibility has been shown to not always correlate with intended behaviour, such as with breast self-examination in Iranian women49. In fact, despite perceived susceptibility being a core construct of the HBM, a meta-analysis of the effectiveness of the model found that it is the weakest predictor of behaviour (excluding cues to action and self-efficacy, which were not evaluated40). Moreover, as premenstrual symptoms are common13 and cyclical, alleviating outside the luteal phase, susceptibility may not be the main driver for seeking help. Instead, symptom severity or impaired functioning are more likely to motivate help-seeking. Perceived susceptibility may also be affected by social constructs that normalise premenstrual symptoms.
Given that these constructs were not implicated and the model can only explain around 60% of behavioural intention, further work is required to determine what other factors explain the remaining 40% of variance. As the constructs of self-efficacy and perceived susceptibility have been identified as not being predictive of behavioural intention in this sample, future work may wish to explore the same research question with a different behavioural model. One such model is the theory of planned behaviour which has previously been used to examine mental health help-seeking intention50 and interventions designed to improve menstrual health51. Likewise, as the current study explored only factors predicting intention to use, more work is necessary to understand how this intention to use translates to real-world usage, and moreover how app developers can promote sustained usage in this population given that drop-out from mental health apps is frequent52.
Some variations in HBM constructs related to sociodemographic characteristics were identified, particularly in regard to highest educational attainment and annual household income. Both educational attainment and annual household income were positively correlated with self-efficacy, suggesting that individuals with higher educational attainment and incomes felt more confident in their ability to engage with digital tools. This reflects previous evidence demonstrating the apparent association between higher education and acceptance of digital mental health interventions31,53. Annual household income was additionally negatively correlated with perceived barriers, this may be explained by concerns regarding cost as outlined above31,32,33,34. Of note, perceived severity appears to be influenced by education, income, and age with negative associations identified. Additionally, significant differences were also observed in perceived severity on the basis of current paid employment status with those in current paid employment perceiving lower severity. There is some evidence that lower educational achievement and lower income are associated with higher prevalence of common mental health disorders54,55. Given the potential influence of these characteristics on these factors implicated in intention to use, it is vital to ensure the design of user friendly and intuitive apps at low or no cost, to widen access to all possible users irrespective of educational attainment, employment status or income. It also further highlights the importance of co-design with individuals from diverse educational and socioeconomic backgrounds to capture attitudes and concerns towards, and preferences for, digital tools from different groups.
The findings of the current study should be considered alongside some limitations. The current sample was highly educated with a high annual income, out-earning the median UK household income. There is evidence that individuals who are highly educated with a high-income are more willing to engage with online health tools53. Notably however, the current study found that education and income were negatively associated with behavioural intention, contradicting such evidence31,53. However, the size of this association in the current study was small, and there are likely other potential confounding or unmeasured variables that may influence the observed associations between these sociodemographic characteristics and behavioural intention. Moreover, as the sample was recruited via social media and the survey was delivered online, participants are more likely have access to and experience interacting with digital technologies. Additionally, given that the recruitment materials advertised the study’s focus as healthcare for mental health symptoms related to the menstrual cycle it is likely that individuals with more severe premenstrual symptoms or whose mental health is more impacted by their menstrual cycle were more inclined to participate. Therefore, the findings of the current study should be framed within the context of the sample and future work should be undertaken in a more diverse sample.
Whilst the HBM items were co-designed with a psychiatrist and reviewed by individuals with lived experience of mental health concerns, there is a risk that some HBM items may not be relevant for some individuals experiencing mental health symptoms related to their menstrual cycle or that some important HBM items could be missing. Moreover, it should be noted that as the HBM items were created specifically for the current study, they were not previously validated. Consequently, there is a risk of this having introduced measurement inaccuracies and potential biases into the study findings, and as such the results should be interpreted with consideration of this limitation. Further work is required to validate the items in the population of interest.
Additionally, participants in the current study will likely have had different assumptions regarding what an app for mental health symptoms related to the menstrual cycle entails. In this regard, future research may wish to leverage the insights gained from the present study to incorporate preferred app features identified into developing HBM items with more tangible and specific app examples. Doing so would further evaluate intention to use an app for premenstrual mental health symptoms and provide further recommendations for evidence-based design of high-quality apps.
To summarise, there is an interest in apps designed for premenstrual mental health symptoms, with the inclusion of symptom monitoring and psychoeducation encouraging early interest, particularly if there is no cost to the user. Moreover, from a HBM perspective, advertising co-design practices with patients, trusted institutions, and clinicians, as well as securing endorsement from HCPs, may be highly influential in driving app uptake. Addressing potential barriers by including features that support human connection, transparently communicating app privacy, and sharing evidence of app quality, as well as highlighting the therapeutic benefits of the app, will likely drive intention to use.
Methods
Participants
Participants were recruited between January and March 2023 via email, word of mouth, paid advertisements, and organic posts on social media. Inclusion criteria for the study were: 1) ≥18 years, 2) UK residence, 3) have had a period, 4) not currently pregnant or breastfeeding, and 5) not in the perimenopause or menopause. Upon completion of the survey, respondents could enter their email for the chance to win one of three £50 Highstreet vouchers. The recruitment materials and participant information sheet emphasised the study’s focus on healthcare (including the developmental of mobile health solutions such as apps) for mental health symptoms related to the menstrual cycle.
Materials and procedure
The data analysed in the current study was taken from a larger survey. An anonymous online survey was created using Qualtrics XM® and sought to explore help-seeking characteristics and attitudes towards apps for premenstrual symptoms in a sample of individuals who experience mental health concerns related to their menstrual cycle. The current paper includes data on sociodemographic characteristics, premenstrual symptoms, preferences for an app for premenstrual mental health symptoms, and questions to evaluate interest in using an app for mental health symptoms related to the menstrual cycle from a HBM perspective. Premenstrual symptoms were measured with the Premenstrual Symptom Screening Tool (PSST56). The PSST includes 19 items scored on a 4-point scale, scored from ‘Not at all’ to ‘Severe’ to assess premenstrual symptoms and associated functional impairment. An additional item was added to capture impaired romantic or intimate relationships, as this is commonly associated with premenstrual conditions such as PMDD57. Therefore, the total number of items was 20. Questions regarding preferences for an app for mental health symptoms related to the menstrual cycle focused on app features and cost, with a view to understand which features and price point would be conducive to a highly attractive app offering. To determine which app features were preferred, participants were given a list of possible mental health app features (e.g., psychoeducation, symptom monitoring, help to obtain a diagnosis or get a referral to a HCP) and asked to select their top three preferred features. The list of possible mental health app features was taken from a previous study58 and were co-designed with relevant stakeholders. To determine preferences for cost, participants were asked whether they would be willing to pay for an app with their most desired features. 25 items were co-designed with a psychiatrist (SB) to assess the constructs of the HBM. Previous work using the HBM to evaluate intention to use an app for COVID-19 contact tracing24 and factors implicated in engaging in health-promoting behaviours related to menstruation27 were also considered as reference studies to inform item creation. Additionally, some HBM items were based on barriers and facilitators to mental health app interest and uptake identified in interviews with individuals with lived experience of mental health concerns59. HBM items in the current study were scored on a 6-point scale: 1 = “Strongly disagree”, 2 = “Disagree”, 3 = “Slightly disagree”, 4 = “Slightly agree”, 5 = “Agree”, 6 = “Strongly agree”. Items were reviewed by individuals with lived experience of mental health concerns and amended for the population of interest. The survey took 15-20 minutes to complete and was adaptive, meaning that only relevant questions were displayed based on previous answers.
Data analysis
Survey sections not included in the current paper containing free-text responses were reviewed, revealing three participants were in the perimenopause or menopause. This data was subsequently excluded from the analysis. Descriptive data analyses were performed in Excel, version 22006 (Microsoft Office 365). Cronbach’s alphas for internal consistency of HBM constructs were calculated. Spearman rank-order correlation coefficients between HBM constructs (calculated using the mean of items in each construct) were calculated. To assess group differences in HBM constructs related to employment, employment data were recoded as either “in current paid employment” (i.e., full-time, part-time, self-employed) or “not in current paid employment” (i.e., voluntary work, taking time off work to care for children or others, retired) and Mann–Whitney U tests were performed. To assess for associations between age, annual household income, and highest educational attainment and HBM constructs, Spearman rank-order correlation coefficients were calculated. Annual household income and highest educational attainment were treated as ordinal variables (with answer options “other” and “prefer not to say” removed for analysis). Please note, that group differences in ethnicity and gender were not explored given the insufficient number of participants in subgroups and overall homogeneity of the sample.
Cronbach’s alphas, Spearman rank-order correlations, and Mann–Whitney U’s were performed using SPSS, version 28.0.1.1
Figures were created using Excel version 2206 and PowerPoint version 2206 (Microsoft Office 365). Stata ver. 17.0 was used for the SEM. Confirmatory factor analysis (CFA) was conducted to investigate whether the factor structure of the HBM is a good fit for assessing intention to use an app for premenstrual mental health symptoms. There is no widely-accepted minimum acceptable sample size for SEM, with the proposed number of observations including a minimum of 20060 or 10 observations per variable61. Therefore, it was determined the required sample was at least 250 to meet the proposed minimum acceptable number of observations, given the number of HBM items.
A Doornik-Hansen test revealed data were non-normally distributed, and so there was a risk of underestimation of relationships between variables. Therefore, model goodness of fit evaluation was reported as a Satorra–Bentler scaled chi-squared test. A structural equation model was constructed to confirm the consistency of the observed variables with the proposed latent variables (perceived benefits, perceived barriers, perceived susceptibility, perceived severity, self-efficacy, and cues to action). The relationships between these variables and the outcome variable (behavioural intention) was then evaluated. All exogeneous latent variables were assumed to be correlated.
While χ2 is the commonly reported statistic to evaluate fit, and a good model should present with a p-value above 0.05 threshold62, χ2 is very sensitive to sample size, and in large samples, the model is nearly always rejected63. As such, χ2 is not necessarily a reliable basis for acceptance or rejection of the model63,64,65. Therefore, model fit was also evaluated using comparative fit index (CFI), root mean square error of approximation (RMSEA), and the standardised root mean square residual (SRMR), as recommended by Kline60. A CFI value of 0.90 or above indicates a good model fit66, and RMSEA values lower than 0.60 fit66 or 0.7067 signifies a good model fit. The SRMR represents the square-root of the difference between the residuals of the sample covariance matrix and the hypothesised model, where a relatively good model fit is indicated when the SRMR is below 0.08 fit66.
Data availability
The data that support the findings of this study are available from the corresponding author, SB, upon reasonable request.
References
Rapkin, A. J. & Winer, S. A. Premenstrual syndrome and premenstrual dysphoric disorder: quality of life and burden of illness. Expert Rev. Pharmacoecon. Outcomes Res. 9, 157–170 (2009).
Dennerstein, L., Lehert, P. & Heinemann, K. Epidemiology of premenstrual symptoms and disorders. Menopause Int. 18, 48–51 (2012).
Direkvand-Moghadam, A., Sayehmiri, K., Delpisheh, A. & Kaikhavandi, S. Epidemiology of Premenstrual Syndrome (PMS)-A Systematic Review and Meta-Analysis Study. J. Clin. Diagn. Res. 8, 106–109 (2014).
Halbreich, U., Borenstein, J., Pearlstein, T. & Kahn, L. S. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology 28, 1–23 (2003).
Prasad, D., Wollenhaupt-Aguiar, B., Kidd, K. N., De Azevedo Cardoso, T. & Frey, B. N. Suicidal Risk in Women with Premenstrual Syndrome and Premenstrual Dysphoric Disorder: A Systematic Review and Meta-Analysis. J. Womens Health 30, 1693–1707 (2021).
Department of Health & Social Care. Women’s Health Strategy for England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1100721/Womens-Health-Strategy-England-web-accessible.pdf. (2022). Accessed 05 October 2023.
Funnell, E., Martin-Key, N. A., Spadaro, B. & Bahn, S. Help-seeking behaviours and experiences for mental health symptoms related to the menstrual cycle: a UK-wide exploratory survey. (Under review). NPJ Womens Health https://doi.org/10.21203/rs.3.rs-3235467/v1 (2021).
Winslow, A., Hooberman, L. & Rubin, L. Werewolves and Two-Headed Monsters: An Exploration of Coping, Sharing, and Processing of Premenstrual Distress Among Individuals With PMDD on an Anonymous Internet Message Board. Womens Reprod. Health 10, 420–435 (2023).
Hiley, C. UK mobile phone statistics, 2023. https://www.uswitch.com/mobiles/studies/mobile-statistics/ (2023). Accessed 05 October 2023.
Chandrashekar, P. Do mental health mobile apps work: evidence and recommendations for designing high-efficacy mental health mobile apps. Mhealth 4, 6 (2018).
Schueller, S. M. & Torous, J. Scaling evidence-based treatments through digital mental health. Am Psychol 75, 1093–1104 (2020).
Chan, A. H. Y. & Honey, M. L. L. User perceptions of mobile digital apps for mental health: Acceptability and usability - An integrative review. J. Psychiatric Mental Health Nurs. 29, 147–168 (2022).
Hantsoo, L. et al. Premenstrual symptoms across the lifespan in an international sample: data from a mobile application. Arch. Womens Ment. Health 25, 903–910 (2022).
International Association for Premenstrual Disorders. Tracking Your Cycle & Symptoms. https://iapmd.org/symptom-tracker/ (2023). Accessed 05 January 2023.
Ford, A., Togni, G., de & Miller, L. Hormonal Health: Period Tracking Apps, Wellness, and Self-Management in the Era of Surveillance Capitalism. Engaging Sci. Technol. Soc. 7, 48–66 (2021).
Riley, S. & Paskova, K. A post-phenomenological analysis of using menstruation tracking apps for the management of premenstrual syndrome. Digital Health 8, 20552076221144199 (2022).
Song, M. & Kanaoka, H. Effectiveness of mobile application for menstrual management of working women in Japan: randomized controlled trial and medical economic evaluation. J. Med. Econ. 21, 1131–1138 (2018).
Borji-Navan, S., Mohammad-Alizadeh-Charandabi, S., Esmaeilpour, K., Mirghafourvand, M. & Ahmadian-Khooinarood, A. Internet-based cognitive-behavioral therapy for premenstrual syndrome: a randomized controlled trial. BMC Womens Health 22, 5 (2022).
Weise, C. et al. Internet-Based Cognitive-Behavioural Intervention for Women with Premenstrual Dysphoric Disorder: A Randomized Controlled Trial. Psychotherapy Psychosomatics 88, 16–29 (2019).
Gan D. Z. Q., McGillivray L., Han J., Christensen H., Torok M. Effect of Engagement With Digital Interventions on Mental Health Outcomes: A Systematic Review and Meta-Analysis. Front. Digital Health. 2021;3. https://doi.org/10.3389/fdgth.2021.764079.
Spadaro, B., Martin-Key, N. A. & Bahn, S. Building the Digital Mental Health Ecosystem: Opportunities and Challenges for Mobile Health Innovators. J. Med. Internet Res. 23, e27507 (2021).
Rosenstock, I. M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 2, 354–386 (1974).
Cho, Y. M., Lee, S., Islam, S. M. S. & Kim, S. Y. Theories Applied to m-Health Interventions for Behavior Change in Low- and Middle-Income Countries: A Systematic Review. Telemed. e-Health 24, 727–741 (2018).
Walrave, M., Waeterloos, C. & Ponnet, K. Adoption of a Contact Tracing App for Containing COVID-19: A Health Belief Model Approach. JMIR Public Health Surveill. 6, e20572 (2020).
Zhang, Z. & Vaghefi, I. Continued Use of Contact-Tracing Apps in the United States and the United Kingdom: Insights From a Comparative Study Through the Lens of the Health Belief Model. JMIR Formative Res. 6, e40302 (2022).
O’Connor, P. J., Martin, B., Weeks, C. S. & Ong, L. Factors that influence young people’s mental health help-seeking behaviour: a study based on the Health Belief Model. J. Adv. Nurs. 70, 2577–2587 (2014).
Ghorbani-Dehbalaei, M., Loripoor, M., Nasirzadeh, M. The role of health beliefs and health literacy in women’s health promoting behaviours based on the health belief model: a descriptive study. BMC Women Health. 21, https://doi.org/10.1186/s12905-021-01564-2 (2021).
Schueller, S. M., Neary, M., Lai, J. & Epstein, D. A. Understanding People’s Use of and Perspectives on Mood-Tracking Apps: Interview Study. JMIR Mental Health 8, e29368 (2021).
National Institute for Health and Care Excellence. Premenstrual syndrome: How should I diagnose premenstrual syndrome? https://cks.nice.org.uk/topics/premenstrual-syndrome/diagnosis/diagnosis/ (2019). Accessed 05 October 2023.
Kancheva Landolt, N. & Ivanov, K. Short report: cognitive behavioral therapy - a primary mode for premenstrual syndrome management: systematic literature review. Psychol. Health Med. 26, 1282–1293 (2021).
Borghouts, J. et al. Barriers to and Facilitators of User Engagement With Digital Mental Health Interventions: Systematic Review. J. Med. Internet Res. 23, e24387 (2021).
Krebs, P. & Duncan, D. T. Health App Use Among US Mobile Phone Owners: A National Survey. JMIR mHealth uHealth 3, e4924 (2015).
Office for National Statistics. Average household income, UK: financial year ending 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/bulletins/householddisposableincomeandinequality/financialyearending2022 (2023). Accessed 05 October 2023.
Oyebode, O., Alqahtani, F. & Orji, R. Using Machine Learning and Thematic Analysis Methods to Evaluate Mental Health Apps Based on User Reviews. IEEE Access 8, 111141–111158 (2020).
Eagle, T., Mehrotra, A., Sharma, A., Zuniga, A. & Whittaker, S. “Money Doesn’t Buy You Happiness”: Negative Consequences of Using the Freemium Model for Mental Health Apps. Proc. ACM Hum. Comput. Interact 6, 1–38 (2022).
Barrett, D. & Heale, R. What are Delphi studies? Evid. Based Nurs. 23, 68–69 (2020).
NHS Institute for Innovation and Improvement. The ebd approach: experience based design Using patient and staff experience to design better healthcare services. https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Experience-Based-Design-Guide-and-Toolkit.pdf. (2009). Accessed 05 October 2023.
Lipschitz, J. et al. Adoption of Mobile Apps for Depression and Anxiety: Cross-Sectional Survey Study on Patient Interest and Barriers to Engagement. JMIR Mental Health 6, e11334 (2019).
Simblett, S. et al. Barriers to and Facilitators of Engagement With mHealth Technology for Remote Measurement and Management of Depression: Qualitative Analysis. JMIR mHealth uHealth 7, e11325 (2019).
Carpenter, C. J. A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior. Health Commun. 25, 661–669 (2010).
Robillard, J. M. et al. Availability, readability, and content of privacy policies and terms of agreements of mental health apps. Internet Interventions 17, 100243 (2019).
Parker, L., Halter, V., Karliychuk, T. & Grundy, Q. How private is your mental health app data? An empirical study of mental health app privacy policies and practices. Int. J. Law Psychiatry 64, 198–204 (2019).
Alfawzan, N., Christen, M., Spitale, G. & Biller-Andorno, N. Privacy, Data Sharing, and Data Security Policies of Women’s mHealth Apps: Scoping Review and Content Analysis. JMIR mHealth uHealth 10, e33735 (2022).
Jilka, S. et al. Terms and conditions apply: Critical issues for readability and jargon in mental health depression apps. Internet Interventions 25, 100433 (2021).
Robinson, R. L. & Swindle, R. W. Premenstrual Symptom Severity: Impact on Social Functioning and Treatment-Seeking Behaviors. J. Womens Health Gender Based Med. 9, 757–768 (2000).
Cross, S. P. et al. Factors associated with treatment uptake, completion, and subsequent symptom improvement in a national digital mental health service. Internet Interventions 27, 100506 (2022).
Osborn, E., Wittkowski, A., Brooks, J., Briggs, P. E. & O’Brien, P. M. S. Women’s experiences of receiving a diagnosis of premenstrual dysphoric disorder: a qualitative investigation. BMC Women Health 20, 242 (2020).
Friis-Healy, E. A., Nagy, G. A. & Kollins, S. H. It Is Time to REACT: Opportunities for Digital Mental Health Apps to Reduce Mental Health Disparities in Racially and Ethnically Minoritized Groups. JMIR Mental Health 8, e25456 (2021).
Tavafian, S. S., Hasani, L., Aghamolaei, T., Zare, S. & Gregory, D. Prediction of breast self-examination in a sample of Iranian women: an application of the Health Belief Model. BMC Women Health 9, 37 (2009).
Adams, C., Gringart, E. & Strobel, N. Explaining adults’ mental health help-seeking through the lens of the theory of planned behavior: a scoping review. Syst. Rev. 11, 160 (2022).
Darabi, F. & Yaseri, M. Intervention to Improve Menstrual Health Among Adolescent Girls Based on the Theory of Planned Behavior in Iran: A Cluster-randomized Controlled Trial. J. Prev. Med. Public Health 55, 595–603 (2022).
Torous, J., Lipschitz, J., Ng, M. & Firth, J. Dropout rates in clinical trials of smartphone apps for depressive symptoms: A systematic review and meta-analysis. J. Affect. Disord. 263, 413–419 (2020).
Luo, A. et al. The Effect of Online Health Information Seeking on Physician-Patient Relationships: Systematic Review. J. Med. Internet Res. 24, e23354 (2022).
Fryers, T., Melzer, D. & Jenkins, R. Social inequalities and the common mental disorders. Soc. Psychiatry Psychiatric Epidemiol. 38, 229–237 (2003).
Sareen, J., Afifi, T. O., McMillan, K. A. & Asmundson, G. J. G. Relationship Between Household Income and Mental Disorders: Findings From a Population-Based Longitudinal Study. Arch. Gen. Psychiatry 68, 419–427 (2011).
Steiner, M., Macdougall, M. & Brown, E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch Womens Ment Health 6, 203–209 (2003).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed., text rev. (American Psychiatric Publishing, Inc, 2022).
Spadaro, B., Martin-Key, N. A., Funnell, E., Benáček, J. & Bahn, S. Opportunities for the Implementation of a Digital Mental Health Assessment Tool in the United Kingdom: Exploratory Survey Study. JMIR Formative Res. 7, e43271 (2023).
Funnell, E. L., Spadaro, B., Martin-Key, N. A., Benacek, J. & Bahn, S. Perceived acceptability of apps for mental health assessment and triage with recommendations for future design: a UK semi-structured interview study. JMIR formative research 8, e48881 (2024).
Kline R. B. Principles and Practice of Structural Equation Modeling. 4th ed. (Guildford Press, 2015).
Thompson B. Exploratory and confirmatory factor analysis: Understanding concepts and applications (American Psychological Association, 2004).
Barrett, P. Structural equation modelling: Adjudging model fit. Personal. Ind. Differ. 42, 815–824 (2007).
Schermelleh-Engel, K., Moosbrugger, H. & Müller, H. Evaluating the Fit of Structural Equation Models: Tests of Significance and Descriptive Goodness-of-Fit Measures. Methods Psychol. Res. 8, 23–74 (2003).
Vandenberg, R. J. Introduction: Statistical and Methodological Myths and Urban Legends: Where, Pray Tell, Did They Get This Idea? Org. Res. Methods 9, 194–201 (2006).
Joreskog, K. & Sorbom D. Structural equation modelling: Guidelines for determining model fit (University Press of America, 1993).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscipl. J. 6, 1–55 (1999).
Steiger, J. H. Understanding the limitations of global fit assessment in structural equation modeling. Personal. Ind. Differ. 42, 893–898 (2007).
Acknowledgements
We wish to extend our thanks to all the participants for taking the time to contribute to the current study. We also wish to thank Stanley Medical Research Institute for their funding which made the current study possible (grant 07R-1888).
Author information
Authors and Affiliations
Contributions
Authors E.F., B.S., N.M.-K., and S.B. conceived the study focus and materials. Recruitment was conducted by Author E.F. Data analysis and figure creation was performed by Authors J.B. and E.F. Author E.F. prepared the manuscript with support from Authors N.M.-K. and J.B. and revisions from Authors B.S. and S.B. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
Author S.B. holds shares in Psynova Neurotech Ltd and Psyomics Ltd but declares no non-financial competing interests. Author E.F. is a paid consultant for Psyomics Ltd but declares no non-financial competing interests. Authors N.A.M.-K., J.B., and B.S. declare no financial or non-financial competing interests.
Ethical approval and informed consent
The study was approved by the University of Cambridge Human Biology Research Ethics Committee (approval number PRE.2022.110). All participants provided informed consent. Informed consent was collected electronically in the survey software prior to the survey questions being delivered.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Funnell, E.L., Martin-Key, N.A., Benacek, J. et al. Preferences for and intention to use an app for premenstrual mental health symptoms using the Health Behaviour Model (HBM). npj Womens Health 2, 18 (2024). https://doi.org/10.1038/s44294-024-00014-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44294-024-00014-2