Abstract
Major depressive disorder and exposure to antidepressants during pregnancy have been previously associated with preterm birth (PTB). However, the reported results are inconsistent. In this study, we aimed to estimate the effects of antidepressants and maternal depression on the risk of PTB using data from electronic health records (EHRs). This is a population-based retrospective cohort study, utilizing data from primary care EHRs. The cohort included 216,070 deliveries of 176,866 patients from the UK between January 1996 and February 2019. We analyzed the effects of antidepressant exposure during pregnancy on the risk of PTB and additional control outcomes in subgroups of patients with a history of depression, and with recent pre-pregnancy treatment. We also assessed the effect of depression alone, in untreated patients. The analysis utilized large-scale propensity score matching that included all demographic and clinical covariates, and effect estimation using a Cox model. The main cohort included 17,615 (8.2%) PTBs. Among patients who were not exposed to antidepressants during pregnancy, a history of depression was associated with an increased risk of PTB (HR 1.10, CI [1.04,1.15], P < 0.01]. Patients exposed to SSRIs during the first 22 weeks of gestation were not at a significantly higher risk of PTB compared to unexposed patients (HR 1.08 CI [0.98,1.18], P = 0.11). Moreover, treatment continuation during pregnancy did not affect the risk of PTB among patients with pre-pregnancy treatment (HR 1.03 CI [0.92,1.15], P = 0.61), and among patients with a history of depression (HR 1.00 CI [0.90,1.11], P = 0.98). Additionally, exposure to antidepressants was associated with a reduced risk of some common medical conditions during the outcome follow-up period. Our findings indicate that the concern of PTB should not affect the clinical decision of medical treatment for pregnant women suffering from depression, since antidepressant treatment by itself does not increase the risk of PTB.
Similar content being viewed by others
Introduction
Depressive disorders during pregnancy are common, with estimated prevalence ranging from 11% to 16%1. Accordingly, antidepressant drugs, most commonly selective serotonin reuptake inhibitors (SSRI), are used by approximately 3–4% of pregnant women worldwide, with a higher prevalence in the United States compared to Europe2. As antidepressants cross the placenta and the fetal blood-brain barrier3, exposure during pregnancy raises concerns of potential risks of adverse pregnancy outcomes and postnatal effects.
Observational studies have shown associations between exposure to antidepressants during pregnancy and increased risk of preterm birth (PTB), although reported results have been inconsistent. Particularly, these associations may be confounded by exposure to maternal psychiatric illness and by illness severity, making it difficult to disentangle the effects of the condition and the treatment4,5,6,7. Meta-analysis studies reported an overall increased risk of PTB in women exposed to antidepressants during pregnancy, with relative risk ranging from 1.17 to 1.698,9,10,11,12; however, there was high heterogeneity across studies. It has been suggested that depression, rather than antidepressant treatment, may have a causal relation to PTB5,13,14 and that psychological stress during pregnancy is a risk factor of PTB15, although other studies have reported that among women with depression, consumption of antidepressants during pregnancy was associated with a higher risk of PTB6,16. The conclusion of most of these previous studies was that the clinical decision about the pharmacological treatment of depression during pregnancy should carefully weigh the risk-benefit potential17.
Patients are often cautious about continuing their antidepressant treatment during pregnancy due to potential side effects. A UK study found that antidepressants were 5 times more likely to be stopped in pregnant women than in nonpregnant women, particularly during the first 6 weeks of pregnancy18. However, as treatment discontinuation may be harmful to the mother, as well as to the developing fetus, it is important to produce reliable evidence to facilitate evidence-based decision-making.
The motivation for this study was to address the above-mentioned gaps in understanding the relations between antidepressants and PTB and to contribute evidence to support the clinical recommendations. We aimed to estimate the effects of antidepressants and maternal depression on the risk of PTB and to disentangle the two effects using abundant data from over 200,000 deliveries recorded in electronic health records (EHRs). We used a rigorous matching methodology on a large cohort of pregnant women, along with subgroup and sensitivity analyses, in order to address the clinical concern of whether antidepressants, and SSRIs in particular, should be continued or discontinued during pregnancy.
Results
Study population
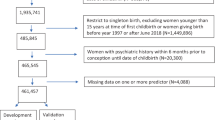
The study population selection process is depicted in Fig. 1. The analysis included 216,070 pregnancies of 176,866 mothers. There were 17,615 (8.2%) PTBs of 16,946 mothers (9.6%) in the baseline cohort. The mean period of observation before the beginning of pregnancy was 5.3 ± 3.9 years, and the mean follow-up time after delivery was 7.0 ± 4.8 years. The characteristics of the main cohort are presented in Table 1. There was no significant difference in the mother’s age or pre-pregnancy BMI between term and preterm deliveries. Mothers who gave birth prematurely had a significantly higher average quantile of Townsend deprivation index, higher prevalence of smoking, chronic and mental health conditions, and more frequent use of medications in selected major drug classes, including antidepressants, within the year before pregnancy.
The main cohort included live births from January 1996 to February 2019. Three subgroups were defined for further sensitivity analysis: patients with a history of depression diagnosis (SG1), patients with pre-pregnancy SSRI prescriptions (SG2) and patients who were not exposed to antidepressants during the pregnancy (SG3).
Effects of depression and antidepressants on preterm birth
Patients exposed to SSRIs during the first 22 weeks of pregnancy had an unadjusted higher risk of preterm delivery, compared to those unexposed to any antidepressants (HR 1.28, CI [1.20,1.37], P < 0.01). Following confounder adjustment with large-scale propensity score matching (LS-PSM), the effect was attenuated (HR 1.08, CI [0.98,1.18], P = 0.11) and no longer significant (Fig. 2). In the subgroup of patients with a past diagnosis of depression (SG1) there was an unadjusted increased risk of preterm delivery (HR 1.15, CI [1.07,1.24], P < 0.01) but no difference in the adjusted risk (HR 1.00, CI [0.90,1.11], P = 0.98) between the patients exposed and unexposed to antidepressants during pregnancy. Similarly, in the subgroup of patients with pre-pregnancy SSRI prescriptions (SG2), the unadjusted effect of pregnancy exposure was positive (HR 1.11, CI [1.01,1.21], P = 0.03), but following LS-PSM adjustment, there was no statistically significant difference in the risk of preterm delivery between the exposed and unexposed groups (HR 1.03, CI [0.92,1.15], P = 0.61). Similar effects were observed when considering exposure to any antidepressant during the first 22 weeks of pregnancy, with an adjusted HR of 1.09 (CI [1.01,1.19], P = 0.03) for comparison of all patients, and adjusted HRs of 1.08 (CI [0.98,1.18], P = 0.12) and 1.04 (CI [0.95,1.15], P = 0.40) for subgroups SG1 and SG2, respectively. When restricting the exposure to any antidepressant during the first trimester, the adjusted HRs for SG1 and SG2 were 0.98 (CI [0.90,1.08], P = 0.74) and 1.01 (CI [0.92,1.12], P = 0.78), respectively.
In the subgroup of patients without antidepressant prescriptions during pregnancy (SG3), patients with a previous diagnosis of depression were at a higher risk of preterm delivery compared to patients without such a diagnosis. In this comparison, the positive unadjusted effect (HR 1.17 CI [1.13,1.21], P < 0.01) persisted after LS-PSM adjustment (HR 1.10, CI [1.04,1.15], P < 0.01).
Effects of depression and antidepressants on additional outcomes
In SG3, a history of depression was associated with an increased adjusted risk of UTI (HR [CI] 1.14 [1.05,1.24], P < 0.01), URI (1.08 [1.00,1.16], P = 0.06), constipation (1.28 [1.14,1.44], P < 0.01), heartburn (1.18 [1.10,1,28], P < 0.01), diarrhea (1.30 [1.15,1.47], P < 0.01) and headache (1.27 [1.15,1.40], P < 0.01) during the follow-up period. In SG1 and SG2, exposure to SSRIs during the first 22 weeks of pregnancy was associated with a reduced risk of URI (0.79 [0.65,0.94] P = 0.01 and 0.84 [0.71,1.00] P = 0.05, respectively), constipation (0.73 [0.57,0.94] P = 0.02 and 0.83 [0.66,1.03] P = 0.10) and headache (0.85 [0.69,1.04] P = 0.12 and 0.84 [0.70,1.01] P = 0.07), while no risk differences were observed for UTI, heartburn, and diarrhea (Fig. 3).
Similar results were obtained for SG1 and SG2 when considering exposure to any antidepressants during the first 22 weeks of pregnancy or during the first trimester: the adjusted risks of URI and constipation were significantly lower in exposed patients. The risk of headache tended to decrease for SG2, with borderline statistical significance. For the outcomes of URI, heartburn, and diarrhea, there was no risk difference associated with the exposure.
Discussion
We used EHRs of a large population-based cohort to examine the effect of both maternal depression and the use of antidepressants (SSRIs in particular) on the risk of PTB, aiming to disentangle the effect of the illness from the treatment.
We observed that patients exposed to antidepressants during the first 22 weeks of gestation were at increased risk for PTB, compared to those who were not pharmacologically treated. However, as these two groups differ significantly in their history of mental illness, the observed effects may stem from the underlying depression rather than the medications. Therefore, we conducted subgroup analyses demonstrating that patients with a history of depression who were not exposed to antidepressants during pregnancy were at increased risk of PTB, compared to those without depression. This effect remained significant after adjusting for various potentially confounding factors, indicating that the increased risk of PTB may be attributed to the depression itself rather than the treatment. Moreover, when assessing the effect of exposure to antidepressants in subgroups of patients with a history of depression or with pre-pregnancy antidepressant treatment, we did not observe a risk difference between exposed and non-exposed patients. These results were invariant to the type of antidepressant (any antidepressant or SSRIs) and to the exposure time window (first 22 weeks of gestation or first trimester).
We also assessed the effects of depression and antidepressants on other common medical conditions and symptoms that have been shown to be associated with depression19,20, including infectious diseases such as UTI and URI, constipation, diarrhea, headache, and heartburn. Our analysis confirmed that the risk for all of these outcomes is increased in patients with a history of depression compared to patients without depression. Interestingly, antidepressant treatment during pregnancy reduced the risk for some of the outcomes (URI, constipation, and headache), and did not increase the risk for the others. The mechanism by which antidepressants affect the risk of comorbidities is unclear. Possibly, the risk reduction is secondary to the treatment-induced improvement of depression. Alternatively, antidepressants may act as immunomodulators, which may lead to a reduction in the prevalence of concurrent medical conditions. This explanation stems from the theory that depression induces a pro-inflammatory immune reaction, resulting in increased susceptibility to other accompanying medical conditions21,22,23,24,25,26,27,28.
The clinical question remains whether pregnant women suffering from depression should cease their existing treatment or withhold initiation of a new treatment due to the increased risk of PTB18. Our findings indicate that the concern of PTB should not affect the clinical decision of pharmacological treatment for pregnant women suffering from depression, since antidepressant treatment by itself is not associated with increased risk of PTB. Moreover, antidepressant treatment reduces the risk of unbalanced depression implications, such as suicidal behavior, poor nutrition secondary to anorexia, and nonadherence to medical and prenatal care, as well as adverse pregnancy and neonatal outcomes like postpartum depression and abnormal child development27,28,29.
As depression may lead to suboptimal maternal and fetal outcomes, the medical decision regarding antidepressant treatment during pregnancy should be based upon personalized clinical judgment, considering the best interest of both the mother and the developing fetus, by weighing the potential risks and benefits of drug treatment against the possible complications arising from untreated maternal depression30.
Consistent with our results, several previous studies have demonstrated an association between maternal depression and PTB, irrespective of antidepressant use5,13,14,31. Nordeng et al. showed that after adjusting for the maternal level of depression as well as various socio-demographic and lifestyle factors, the effect of antenatal antidepressants on PTB became insignificant32. Moreover, recent studies that examined the association between PTB and maternal depression stratified by the depression severity, suggested a potential dose-effect interaction, with increased risk of PTB among patients suffering from severe depression14.
Inconsistently, other studies described an effect of antenatal antidepressants on the risk of PTB, which persisted following an adjustment for maternal depression6,8,9,10,11,12,16,33. Yonkers et al. reported that the use of SSRIs was associated with an increased risk of PTB regardless of major depressive disorder, while depression alone, without drug therapy had no clear effect6.
The conflicting results may stem from differences in study design and in particular the selection of the comparator group for the effect estimation. In Yonkers et al. the reference group included patients with neither major depressive episodes nor SSRI treatment6. This group differs significantly from the exposed group, especially with respect to mental health-related covariates that are highly correlated with the exposure and cannot be properly adjusted for between the reference and exposed groups. Our analysis overcomes this limitation by comparing subgroups of patients with a history of depression diagnosis or treatment, which differ only in their antidepressant exposure during pregnancy. Other differences between studies include the selection criteria of the cohort, the phenotype of maternal depression, the classification of its severity, and the timing of the covariate assessment, exposure, and follow-up windows. Additionally, the studies vary in the methods used to adjust for potential confounders and in the outcome models used to estimate the effects5,6,8,9,10,11,12,13,14,16,31,33.
Our study has several strengths that differentiate it from previous work. It is based on an exceptionally large dataset from primary care EHR, which provides a reliable holistic representation of a patient’s medical history, as opposed to self-reported data that may be incomplete or biased. We used a meticulous matching methodology, considering numerous potentially confounding factors, including known risk factors, maternal characteristics, baseline medical status, and lifestyle features. Additionally, we conducted a unique subgroup analysis that enabled us to disentangle the possible effects of depression and antidepressants, and demonstrated these effects on additional health outcomes with known associations to depression that served as positive controls.
Nevertheless, this work also has some limitations. The recording of depression symptoms in the EHR may be incomplete. Exposure to antidepressants was derived from prescription information, which lacks certainty about actual compliance to treatment. Moreover, the severity of the depression, which is not reliably captured in the EHR, is a potential confounder that could not be fully adjusted for in our analyses. The patients that continued their treatment during pregnancy may have suffered from more severe symptoms than those who discontinued. However, as depression is associated with preterm birth, a more severe depression in the exposed group would contribute to a larger positive effect size. Therefore, our results that exposure to antidepressants does not increase the risk of preterm birth may be an overestimation of the real effect, but not an underestimation.
Due to the clinical significance of depression treatment in general and especially during the antenatal period, we believe that additional reliable data is needed to facilitate evidence-based clinical decision-making. An important consideration in this process is the possible consequences for the future health outcomes of the newborn, which require additional, large-scale, longitudinal studies. Furthermore, exploring nonpharmacological treatments in the context of depression and adverse pregnancy outcomes would be a desirable extension of this work.
In conclusion, in this study, we have analyzed the effects of depression and antidepressants on preterm birth. Our results suggest that the risk of PTB is associated with depression, rather than the treatment by antidepressants. In patients with a history of depression or with recent pre-pregnancy treatment, exposure during pregnancy did not affect the risk of preterm birth. Furthermore, we observed that exposure to antidepressants during pregnancy was associated with a reduced risk of some common medical conditions that are known to be associated with depression. These observations may support the clinical decision of continuing antidepressant treatment during pregnancy while weighing the patient-specific risk-benefit potential.
Methods
This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline. The design was a population-based propensity score-matched cohort study, utilizing data from EHRs.
Dataset
We used primary care EHRs from IQVIA Medical Research Data (IMRD), incorporating data from The Health Improvement Network (THIN, a Cegedim database). This dataset contains records of over 12.5 million patients, covers approximately 5% of the UK population, and is representative of the population in terms of demographics and condition prevalence34. The data includes patient demographics, medical diagnoses, drug prescriptions, anthropometric measurements, and lab tests, which were standardized into the Observational Medical Outcomes Partnership (OMOP) common data model35.
Study population
The initial population included all patients who had a live birth between January 1996 and February 2019 and information about gestational age at birth in their medical records. Pregnancies resulting in a live birth were identified by searching for recorded medical codes, using the algorithm to infer pregnancy episodes and their outcomes from observational data developed by Mathco et al.36. Start dates were estimated using a derived hierarchy of available pregnancy markers, including records of gestational age at birth and last menstrual period. Patients were also required to be continuously observed for at least one year prior to the beginning of pregnancy, to ensure availability of sufficient medical history. Multiple births (N = 2389) and patients with a history of severe mental illness (psychotic disorder and bipolar disorder, N = 736) were excluded. The patient selection flowchart is shown in Fig. 1. The final cohort included 216,070 deliveries of 176,866 patients.
Out of this main cohort, we defined the following subgroups:
-
1.
SG1: Patients with a previous diagnosis of depression at any time prior to pregnancy (N = 53,809).
-
2.
SG2: Patients with SSRI prescription within 1 year prior to pregnancy (N = 20,544).
-
3.
SG3: Patients who were not exposed to antidepressants during pregnancy (N = 203,335).
Exposures and outcomes
Exposure to antidepressants was determined by identifying prescriptions of drugs with WHO’s Anatomical Therapeutic Chemical (ATC) code N06A. SSRI prescriptions were identified by ATC code N06AB. Diagnosis of depression was determined by identifying visits with SNOMED-CT codes for depressive disorder, symptoms of depression, or depressed mood (codes 35489007, 394924000, and 366979004, respectively).
The PTB outcome was defined as birth before gestational age (GA) of 37 weeks. To identify the beginning of the pregnancy we used either the recorded observation of length of gestation at birth (code 412726003) within 90 days after the delivery or, in cases where GA was not directly available, the date of the last menstrual period (code 161713000) within 22 to 43 weeks before the delivery.
As positive controls for our study, we assessed the effects of depression and antidepressants on six common medical conditions and symptoms that are known to be associated with depression19,20,37,38. These additional maternal outcomes included urinary tract infection (UTI, code 68566005), upper respiratory infection (URI, code 54150009), constipation (code 14760008), diarrhea (code 62315008), heartburn (code 16331000), and headache (code 25064002).
Study design
The study design is illustrated in Fig. 4, which follows the framework of graphical representation recommended by Schneeweiss et al.39. The baseline analysis (BL) compared patients exposed to SSRIs during the first 22 weeks (days 0 to 154) of gestation to patients unexposed to any antidepressants. The covariate assessment window was set as one year prior to the index date (the beginning of the pregnancy). The exposure assessment window (anytime before gestational week 22) preceded a PTB follow-up window, which ranged from gestational weeks 23 to 37 during which a preterm delivery of a viable fetus can occur. Patients who initiated antidepressant treatment during the PTB follow-up window were censored at the time of their first prescription. The additional maternal outcomes were assessed during the same follow-up window as PTB.
The boxes on the timeline represent the exclusion assessment windows (light blue), exposure assessment windows (dark blue) and outcome follow-up window (green-white). Window timings are given in brackets, relative to the cohort entry date. Subgroup labels on the windows indicate a relation to specific analyses. The vertical gray lines mark the beginning of pregnancy, end of 37 weeks of gestation and delivery day (DD). SMI: severe mental illness; GA: gestational age; Dx: diagnosis.
The analyses of the subgroups SG1 and SG2 were based on the same design, with additional exclusion criteria (Fig. 4). For analyzing subgroup SG3, patients with antidepressant prescriptions during pregnancy were excluded, and the exposure was defined as depression diagnosis any time before the pregnancy.
Propensity models
To balance the compared groups on the confounding variables, we used large-scale propensity score matching (LS-PSM)40. We fitted a regularized logistic regression propensity model that predicted the probability of the exposure, based on a set of all available demographic and clinical covariates - conditions (including comorbidities), drug prescriptions, observations, and procedures during the year before the pregnancy. Covariates that are linked to the exposure were omitted from the propensity model (for example, pre-pregnancy prescriptions of antidepressants). We performed one-to-one matching of the target and comparator groups, based on the propensity score with a caliper width of 0.2. The matching quality was assessed by measuring the per-feature standardized difference (SD), requiring SD ≤ 0.1 for acceptable matching41.
Effect estimation
We estimated the effect size of the exposure on PTB and the additional outcomes by calculating hazard ratios (HR) using Cox proportional hazards model, conditioned on the matched sets. All estimations were supplemented with 95% confidence intervals (CI).
The analysis was performed using the Health Analytics Data-to-Evidence Suite (HADES), a set of open-source R packages developed by the Observational Health Data Sciences and Informatics (OHDSI) community42.
Ethical approval
Use of IQVIA Medical Research Data (IMRD) was approved by the NHS London - South East Research Ethics Committee (REC reference: 18/LO/0441); in accordance with this approval, the study protocol was reviewed and approved by an independent Scientific Review Committee (SRC) of IQVIA Inc. (reference number: 20SRC018). Patients’ written informed consent was waived by the London - South East Research Ethics Committee as the study used data from anonymized electronic health records.
Data availability
The data that support the findings of this study are available from IQVIA Inc. but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Code availability
The underlying code for this study is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author.
References
Howard, L. M. et al. Non-psychotic mental disorders in the perinatal period. Lancet 384, 1775–1788 (2014).
Molenaar, N. M. et al. The international prevalence of antidepressant use before, during, and after pregnancy: A systematic review and meta-analysis of timing, type of prescriptions and geographical variability. J. Affect. Disorders 264, 82–89 (2020).
Ewing, G., Tatarchuk, Y., Appleby, D. & Kim, D. Placental Transfer of Antidepressant Medications: Implications for Postnatal Adaptation Syndrome. Clin. Pharmacokinet 54, 359–370 (2015).
Byatt, N., Deligiannidis, K. M. & Freeman, M. P. Antidepressant use in pregnancy: a critical review focused on risks and controversies. Acta. Psychiatr. Scand 127, 94–114 (2013).
Staneva, A., Bogossian, F., Pritchard, M. & Wittkowski, A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 28, 179–193 (2015).
Yonkers, K. A. et al. Depression and serotonin reuptake inhibitor treatment as risk factors for preterm birth. Epidemiology 23, 677–685 (2012).
Yonkers, K. A. et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen. Hosp. Psychiatry 31, 403–413 (2009).
Huang, H., Coleman, S., Bridge, J. A., Yonkers, K. & Katon, W. A meta-analysis of the relationship between antidepressant use in pregnancy and the risk of preterm birth and low birth weight. Gen. Hosp. Psychiatry 36, (2014).
Ross, L. E. et al. Selected pregnancy and delivery outcomes after exposure to antidepressant medication: a systematic review and meta-analysis. JAMA Psychiatry 70, 436–443 (2013).
Chang, Q. et al. Antidepressant Use in Depressed Women During Pregnancy and the Risk of Preterm Birth: A Systematic Review and Meta-Analysis of 23 Cohort Studies. Front. Pharmacol. 11, (2020).
Huybrechts, K. F., Sanghani, R. S., Avorn, J. & Urato, A. C. Preterm birth and antidepressant medication use during pregnancy: a systematic review and meta-analysis. PLoS One 9, e92778 (2014).
Eke, A. C., Saccone, G. & Berghella, V. Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG: Int J. of Obstet. Gynaecol. 123, 1900–1907 (2016).
Cantarutti, A., Merlino, L., Monzani, E., Giaquinto, C. & Corrao, G. Is the Risk of Preterm Birth and Low Birth Weight Affected by the Use of Antidepressant Agents during Pregnancy? A Population-Based Investigation. PLoS One 11, e0168115 (2016).
Li, D., Liu, L. & Odouli, R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: a prospective cohort study†. Human Reprod. 24, 146–153 (2009).
Shapiro, G. D., Fraser, W. D., Frasch, M. G. & Séguin, J. R. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms. J. Perinatal Med. 41, 631–645 (2013).
Chen, L.-F., Lin, C.-E., Chung, C.-H., Lai, C.-H. & Chien, W.-C. Association between the use of antidepressants and the risk of preterm birth among pregnant women with depression: a retrospective cohort study in Taiwan. J. Investig. Med. 69, 999–1007 (2021).
Pearlstein, T. Depression during Pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 29, 754–764 (2015).
Petersen, I., Gilbert, R. E., Evans, S. J. W., Man, S.-L. & Nazareth, I. Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from The Health Improvement Network. J. Clin. Psychiatry 72, 979–985 (2011).
Smith, D. J. et al. Depression and multimorbidity: a cross-sectional study of 1,751,841 patients in primary care. J. Clin. Psychiatry 75, 1202–1208 (2014). quiz 1208.
Zhang, Q., Shao, A., Jiang, Z., Tsai, H. & Liu, W. The exploration of mechanisms of comorbidity between migraine and depression. J. Cell. Mol. Med. 23, 4505–4513 (2019).
Anisman, H. Cascading effects of stressors and inflammatory immune system activation: implications for major depressive disorder. J. Psychiatry. Neurosci. 34, 4–20 (2009).
O’Brien, S. M., Scott, L. V. & Dinan, T. G. Cytokines: abnormalities in major depression and implications for pharmacological treatment. Human Psychopharmacol. Clin. Exp. 19, 397–403 (2004).
Vismari, L., Alves, G. J. & Palermo-Neto, J. Depression, antidepressants and immune system: a new look to an old problem. Arch. Clin. Psychiatry (São Paulo) 35, 196–204 (2008).
Szabo, A. et al. Immunomodulatory capacity of the serotonin receptor 5-HT2B in a subset of human dendritic cells. Sci. Rep. 8, 1765 (2018).
Strawbridge, R. et al. Inflammation and clinical response to treatment in depression: A meta-analysis. Euro. Neuropsychopharmacol. 25, 1532–1543 (2015).
Eyre, H. A., Lavretsky, H., Kartika, J., Qassim, A. & Baune, B. T. Modulatory Effects of Antidepressant Classes on the Innate and Adaptive Immune System in Depression. Pharmacopsychiatry 26, 85–96 (2016).
Leonard, B. E. The immune system, depression and the action of antidepressants. Progr. Neuro-Psychopharmacol. Biol. Psychiatry 25, 767–780 (2001).
Szałach, L. P., Lisowska, K. A. & Cubała, W. J. The Influence of Antidepressants on the Immune System. Arch. Immunol. Ther. Exp. 67, 143–151 (2019).
Grigoriadis, S. et al. The Impact of Maternal Depression During Pregnancy on Perinatal Outcomes: A Systematic Review and Meta-Analysis. J. Clin. Psychiatry 74, 8615 (2013).
Koren, G. & Nordeng, H. Antidepressant use during pregnancy: the benefit-risk ratio. Am. J. Obstet. Gynecol. 207, 157–163 (2012).
Fransson, E., Örtenstrand, A. & Hjelmstedt, A. Antenatal Depressive Symptoms and Preterm Birth: A Prospective Study of a Swedish National Sample. Birth 38, 10–16 (2011).
Nordeng, H. et al. Pregnancy Outcome After Exposure to Antidepressants and the Role of Maternal Depression: Results From the Norwegian Mother and Child Cohort Study. J. Clin. Psychopharmacol. 32, 186 (2012).
Udechuku, A., Nguyen, T., Hill, R. & Szego, K. Antidepressants in pregnancy: a systematic review. Aust. N Z J Psychiatry 44, 978–996 (2010).
Blak, B. T., Thompson, M., Dattani, H. & Bourke, A. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform. Prim. Care 19, 251–255 (2011).
The Book of OHDSI. https://ohdsi.github.io/TheBookOfOhdsi/.
Matcho, A. et al. Inferring pregnancy episodes and outcomes within a network of observational databases. PLoS ONE 13, e0192033 (2018).
Andersson, N. W. et al. Depression and the risk of severe infections: prospective analyses on a nationwide representative sample. Int. J. Epidemiol. 45, 131–139 (2016).
Ballou, S. et al. Chronic Diarrhea and Constipation are More Common in Depressed Individuals. Clin. Gastroenterol. Hepatol. 17, 2696–2703 (2019).
Schneeweiss, S. et al. Graphical Depiction of Longitudinal Study Designs in Health Care Databases. Ann. Intern. Med. 170, 398–406 (2019).
Tian, Y., Schuemie, M. J. & Suchard, M. A. Evaluating large-scale propensity score performance through real-world and synthetic data experiments. Int. J. Epidemiol. 47, 2005–2014 (2018).
Austin, P. C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav. Res. 46, 399–424 (2011).
HADES. https://ohdsi.github.io/Hades/.
Acknowledgements
This study was partly funded by the March of Dimes. The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
G.A. contributed to the study conception and design, material preparation, data analysis, and manuscript writing. CY contributed to the study conception and design, material preparation, data analysis and commented on previous versions of the manuscript. MB, IG, PA, TH, VB, AT, BL, JR, SW, TO, IK and MS contributed to the study conception and design and commented on previous versions of the manuscript. TS contributed to manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amit, G., Yanover, C., Bivas-Benita, M. et al. Antidepressant use during pregnancy and the risk of preterm birth – a cohort study. npj Womens Health 2, 5 (2024). https://doi.org/10.1038/s44294-024-00008-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44294-024-00008-0