Abstract
Background
Being breastfed has established benefits for infant health, but its long-term effects on adult diseases, including cancer, remain underexplored. We examined associations between being breastfed in infancy and the risks of common cancers.
Methods
Data from 339,115 participants (191,117 women) enrolled in the UK Biobank with self-reported breastfeeding data were linked to national cancer registries. Cox models estimated sex-specific hazard ratios (HR) and 95% confidence intervals (CI) for the associations between being breastfed (ever/never) and risks of overall cancer as well as common cancer sites.
Results
In total, 34,392 incident cancers (17,895 in women) were registered. The HR of overall cancer associated with being breastfed was 1.05 (95% CI 1.01–1.09) in women and 1.00 (95% CI 0.96–1-04) in men. In site-specific analysis being breastfed was associated with an increased risk of breast and ovarian cancer in women and a reduced risk of oesophageal cancer in men.
Discussion
We found that having been breastfed was associated with a marginally increased risk of adult cancer in women, but we found no evidence of an association in men. These findings should be viewed within the study limitations, and do not outweigh the many benefits that breastfeeding provides.
Similar content being viewed by others
Introduction
Cancer is a leading cause of morbidity and premature mortality worldwide [1]. Despite regional heterogeneity, global cancer incidence is rising [1, 2]. These increases likely reflect demographic shifts, and improvements in cancer screening and detection, alongside changes in the distribution of modifiable risk factors and, potentially, changes in breastfeeding [3]. Breastfeeding provides substantial short and long-term health benefits for both the mother and child [4]. Compared to infants who are not breastfed, breastfed infants have lower morbidity from infectious disease, score higher in intelligence tests, and may be protected against overweight and diabetes in later life [5]. Despite these benefits, breastfeeding rates in both the United Kingdom (UK) and Europe remain substantially below the World Health Organization’s (WHO) recommendations to initiate breastfeeding within the first hour of birth and maintain exclusive breastfeeding for the first six months of life [4, 6, 7]. In the UK, the proportion of infants who were ever breastfed dropped from 80% to 60% between 1934 and 1970 [8, 9]. Estimates suggest that in the early 1990s, fewer than 1% of UK infants received 6 months of exclusive breastfeeding and that despite improvements in breastfeeding initiation, this was still the case in 2010 [7, 10].
Despite the well-described benefits of having been breastfed, associations with cancer risks are less well-described. Having been breastfed has been associated with a reduced risk of childhood cancer, including leukaemia and neuroblastomas [11]. Although adult cancers often differ from childhood cancers in underlying pathology and behaviour, the fundamental processes of malignant change likely share common features [12]. Consequently, there is reason to examine whether having been breastfed also protects against adult cancers. Current evidence of associations between having been breastfed and adult cancer risk is scarce and inconsistent. In the largest study to date, the UK-based Million Women Study, an increased risk of colorectal cancer among women who had been breastfed was described [13]. Other studies have observed an inverse association between having been breastfed and pre-menopausal breast cancer, but not other cancer sites [14]. Notably, a substantial knowledge gap remains for evidence of associations of having been breastfed with cancer in men, and for studies powered to detect associations at separate cancer sites.
Having been breastfed as an infant may be linked to adult cancer risks through its associations with obesity and inflammation, which are established risk factors for many cancer forms [15,16,17]. For example, having been breastfed is associated with appetite regulation, energy balance and metabolism throughout life [17, 18]. These associations may affect the development of risk factors for cancer such as childhood growth patterns, child and adult obesity and in turn obesity-related cancers [19, 20]. Breastfeeding may also be linked to adult cancer risks through effects on the early-life immune system [21]. Breastmilk is rich in bioactive components essential for both protection from environmental pathogens and the development of the initially insufficient, immature and ineffective infant immune system [22]. Connected to its immunological properties, being breastfed is associated with the pattern of microbial colonisation in the child, which persists into later life, and could affect cancer risk [23,24,25].
Consequently, we hypothesised that having been breastfed may be associated with reduced cancer risk in later life. To assess this, we utilised data from the UK Biobank to examine sex-specific associations between self-reported breastfeeding status and the risk of adult cancer overall. Following this, we examined the associations with the 10 most common cancer forms in each sex to further describe potential site-specific effects.
Methods
Data resource and study population
The UK Biobank is a prospective cohort study that enrolled participants at ages 40–49 years. A full study protocol is described online [26]. In brief, between 2006–2010, participants were invited to an assessment centre at one of 21 sites across the UK [27]. At the assessment centres, participants completed a touchscreen questionnaire providing information on early life, socio-demographic, lifestyle, environmental, and reproductive factors. Anthropometric measurements were taken by technicians following standardised protocols [26]. Breastfeeding data were collected with the question “Were you breastfed when you were a baby” (yes/no/do not know/prefer not to answer).
All information was collected at the recruitment centre. Variables requested from the data resource included if the participants’ mother smoked (yes/no), participant year of birth, ethnicity (re-categorised into Black, Asian, White, mixed, other), birthweight (kg), relative body size at age 10 (smaller, about average, larger), the participants’ educational level achieved (recategorized into low, intermediate, high), location of the assessment centre, participant age at enrolment (years), body mass index (BMI; kg/m2) at enrolment, smoking status (never-smoked, ex-smoker, current smoker), hormone replacement therapy use (ever vs. never used) and Townsend Deprivation score (numerical measure of relative material deprivation at study entry assigned based on national census output areas).
Biobank data were electronically linked to the UK’s national cancer and death registries. These registers contain data starting from the early 1970s [28]. Cancer forms were defined by International Classification of Diseases 10th edition (ICD-10) codes and the 10 most common incident cancer forms in each sex were retained for exploratory site-specific analysis (Supplementary Table 1). Where non-sex-specific cancers appeared in the top 10 of only one sex, they were assessed in both sexes to facilitate comparisons. Following this criteria, 13 cancers were included (cancer of the bladder, breast, colon, endometrium, kidney, lung, malignant melanomas of the skin, non-Hodgkin’s lymphoma, oesophagus, ovaries, pancreas, prostate, and rectum). Models for overall cancer included all malignant neoplasms (ICD-10 codes: C00–C97). Non-melanoma skin cancer was not included in any analysis. Participants with non-melanoma skin cancer were either included in the non-cancer group or, if diagnosed with a second cancer form, they contributed to the analyses of this cancer form. Only incident cancer cases (from the date of enrolment into UK Biobank) were included.
Study population
Participants were excluded from all analyses if they answered, “do not know”, “prefer not to answer” or had missing data for if they were breastfed as an infant. Participants who had missing information for or who reported being part of a multiple births or adopted were also excluded (Fig. 1). For the analyses of endometrial and ovarian cancer, women with self-reported hysterectomy or oophorectomy were excluded from the analysis, respectively. Participants with their first cancer diagnosis before enrolment into the UK Biobank, other than non-melanoma skin cancer (C44), hydatidiform moles (O01), benign tumours (D10-D36), or in situ neoplasms (D00-D09), were excluded.
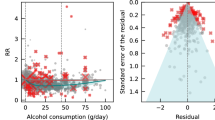
Statistical analyses
Participant characteristics were described as percentages within a given category or median and interquartile range (IQR) by breastfeeding status. Where present, missing data for each variable were categorised as a new “missing” category. The characteristics of those with and without breastfeeding data were also compared. The occurrence of each cancer form was counted by breastfeeding status and sex. To examine if having been breastfed as an infant was associated with cancer risk in later life, associations between having been breastfed and incident cancer overall, alongside site-specific cancers were examined using sex-specific Cox proportional hazard models with age as the underlying time scale. Sex-specific models were constructed owing to the considerable sex differences in cancer susceptibility between sexes [29]. In the constructed models, follow-up began at the date of enrolment into the UK Biobank and ended at the date of first cancer, death or at the end of follow-up in the linked cancer registry (25th June 2021), whichever came first.
Potential confounders of the association between having been breastfed and cancer risks were identified based on availability in the UK Biobank and a priori, literature-driven hypotheses. Maternal smoking and participant ethnicity were considered confounders and were included as covariates in adjusted models. For the analyses of breast and endometrial cancers, we included self-reported use of hormone replacement therapy as an additional covariate. Cox models were stratified by age category at enrolment (38–44, 45–49, 50–54, 55–59, 60–64, 65–73 years), year of birth, and location of the assessment centre. Both crude and adjusted hazard ratios (HR) and their respective 95% confidence intervals (CI) are reported. For the reader’s interest, p values for each model are presented in the supplementary materials. Although identified as a potential confounder, birthweight had a high level of missingness (> 30% compared with < 5% for other included variables) and was therefore not included as a covariate.
Models for breast cancer were divided into pre-menopausal and post-menopausal periods. In the pre-menopause model, women who did not report having experienced menopause contributed person years of follow-up from age at assessment to 55 years of age. In the post-menopausal analysis, women contributed person years of follow-up from age 55 years or age at enrolment if they self-reported having experienced menopause at the assessment. Fifty-five years of age was selected as the cut-off for menopause as in a wide range of international studies, almost all women had reached menopause by this age [30]. Women who self-reported having not had menopause but were over the age of 55 were excluded from the post-menopausal analysis (n = 1317).
To account for the number of outcomes analysed in the exploratory site-specific analysis, we presented the Bonferroni corrected site-specific family error rate (α). The adjustment factor for this correction was determined by the number of sites analysed for each sex.
To assess the proportionality of hazards over time, potential differences in associations between having been breastfed and cancer risks by categories of age at risk (38–58, 59–62, 63–66, 67–73, years) were tested in nested models with and without cross-product terms. Age categories were selected to approximate an equal number of participants in each category. Similarly, potential interactions with birth cohorts (1934–1944, 1945–1949, 1950–1954, 1955–1959, 1960–1971) were tested in nested models with and without cross-product terms.
All analyses were performed in R (Version 4.1.0). Code will be made available on request to the corresponding author. This project was registered with the UK Biobank on 19-10-2022 (approved research ID: 95095) and approved by the Danish Data Protection Agency (P-2022-445).
Results
From a total of 502,369 UK Biobank participants, 339,115 matched the inclusion criteria and were included in this study (Fig. 1). Characteristics of participants with and without breastfeeding data are presented in Supplementary Table 2. Participants without breastfeeding data were older, had more missing data and had lower birthweight than those with breastfeeding data. Of the participants with breastfeeding data, 191,117 (56.4%) were women. Most participants (247,404 [73%]) responded “yes” to having been breastfed as a baby. Participants who reported having been breastfed were born earlier, were older, less socioeconomically deprived at enrolment, and were more likely to be male when compared to those who reported having not been breastfed (Table 1).
During a median follow-up of 12.2 years (IQR = 11.4–13.0), 17,865 and 16,497 first-incident cancers were recorded in women and men, respectively. The number of cases at different cancer sites by breastfeeding status and sex are provided in Table 2.
Having been breastfed as an infant was associated with a slightly increased risk of overall cancer in women (HR = 1.05 [95% CI, 1.01–1.09]) (Fig. 2). Among men, there was no evidence that having been breastfed was associated with overall cancer (HR = 1.00 [95% CI, 0.96–1.04]) (Fig. 3). In exploratory site-specific analyses, no associations were observed for 10 of the 13 sites assessed in women. Having been breastfed was associated with an increased risk of pre-menopausal breast cancer (HR = 1.12 [95% CI, 1.00–1.24]), post-menopausal breast cancer (HR = 1.08 [95% CI, 1.02–1.16]) and ovarian cancer (HR = 1.20 [95% CI, 1.00–1.44]) compared to those who were not breastfed (Fig. 2, Supplementary Table 3). The inclusion of the use of hormone replacement therapy in the models for breast and endometrial cancer minimally affected the associations described (Supplementary Table 3). For site-specific analyses in women, after correction for multiple testing, no p-value was below the Bonferroni-adjusted family error rate α (0.0042 [0.05/12]) (Supplementary Table 3). In men, no site-specific associations were observed for 9 of the 10 cancer sites assessed. Men who were breastfed as infants had a reduced risk of oesophageal cancer (HR = 0.71 [95% CI, 0.57–0.89]) (Fig. 3). The p-value for oesophageal cancer in men was below the Bonferroni-adjusted family error rate α of 0.005 [0.05/10]) (Supplementary Table 3).
No clear increasing or decreasing birth-cohort effects were observed for the majority of cancers. Birth-cohort effects were observed for kidney cancer in women and lung and skin cancer in men (Supplementary Table 4). Violations of the proportional hazards assumptions were observed for kidney cancer and non-Hodgkin’s lymphoma in women. (Supplementary Fig. 1). There was no evidence of proportional hazard assumption violations in men.
Discussion
In this study, based on a large UK population, having been breastfed was associated with a slightly increased risk of overall cancer in women, but no evidence of an association was observed in men. An exploratory analysis across common cancer sites provided weak evidence that these findings may be driven by an increased risk of breast and ovarian cancer in women who were breastfed. In men, site-specific models identified a reduced risk of oesophageal cancer in men who were breastfed. Notably, the overall association in women is driven by sex-specific hormonal cancer forms, potentially explaining the sex differences observed in the overall cancer estimates. These findings should be interpreted cautiously owing to the limitations of the study.
We initially hypothesised that the association of breastfeeding with healthy growth, development and reduced risk of childhood obesity would protect breastfed infants from cancer in later life. The increased risk of overall cancer in women who were breastfed is the opposite of the protective effect we expected. One possible explanatory hypothesis is that the increased risk of cancer could have been related to the timing of weight gain and how this is associated with breastfeeding [20]. Early-life BMI has been inversely associated with the risk of breast cancer, independently of adult BMI [31, 32], and breastfed children have a lower BMI compared to those who are not breastfed. Consequently, breastfed women may have an increased risk of breast cancer in adulthood, compared to those who are not breastfed, owing to their lower early-life BMI. Despite this, we would expect adult BMI to be more important for adult cancer risk as a less time-distanced exposure. Furthermore, the inverse association of breastfeeding with BMI may not track fully into adulthood, but more evidence is required to understand the relationship between breastfeeding and adult BMI [33]. Moreover, the association between breastfeeding and early-life BMI relies on individuals being breastfed long and intensely enough to affect growth outcomes. The exposure variable (ever vs. never breastfed) available in this data cannot capture these important aspects of breastfeeding. Consequently, from the data available, we cannot conclude that the increased risk of cancer is driven by reduced childhood BMI in breastfed infants. Furthermore, and contrary to the hypothesis that the increased risk of cancer in women having been breastfed is explained through inverse associations with body size, childhood overweight and higher BMI have been shown to be positively associated with the risk of ovarian cancer [34]. The differences in the direction of the relationship between childhood BMI and these two cancer sites serve to highlight the difficulty of linking the effect of breastfeeding on early-life growth to subsequent cancer risk and reflect the complex web of early-life exposures that may influence later cancer risk [35].
The increased risk we observed between having been breastfed and both breast and ovarian cancer is not consistent with the previous literature. Both the Million Women study (n = 395,363) and an analysis of 89,385 pre-menopausal and 50,586 post-menopausal American women born between 1921 and 1965 and recruited into one of the two Nurses Health Studies described no evidence of an association between having been breastfed (ever vs. never breastfed) and either breast or ovarian cancer [13, 36]. In the Million Women Study, findings across other cancer sites (endometrial, lung, non-Hodgkin’s lymphoma, oesophageal, pancreatic, skin, and stomach cancer) were consistent with our findings [13]. The authors did report an increased risk of colon and rectal cancer (relative risk (RR) = 1.19 [95% CI, 1.12–1.25], RR = 1.14 [95% CI, 1.02–1.26], respectively), which was not replicated in our study. It is plausible that differences in the study populations may explain these differences. For example, women recruited into the Million Women Study were born earlier and were older on average than the UK Biobank participants, but the exact reasons for intra-study variation across cancer sites are challenging to explain.
In our study, there was no evidence of an association between having been breastfed and overall cancer in men as well as for 9 out of 10 cancer sites examined. We did observe a relatively strong inverse association between being breastfed and the risk of oesophageal cancer. Interestingly, although sex differences in oesophageal cancer are widely reported and thought to be driven by hormonal and genomic factors, the measure of association for women in this study (HR = 0.78 [95% CI, 0.57–1.08]) and the Million Women Study (crude RR = 0.87 [95% CI, 0.76–0.99]) suggest that breastfed women might also have been protected from oesophageal cancer [13]. In our study, the wider confidence intervals for the association with oesophageal cancer reflected a lower oesophageal cancer incidence in women, and although the association reported in the Million Women Study was attenuated when covariates were included (many of which were likely to mediate the association), there appears to be evidence of a signal [13]. Although it is hard to hypothesise why breastfeeding would have a protective association with only oesophageal cancer, which shares common risk factors with many other cancer sites, it would be interesting to see if this association is replicated in future studies.
The strengths of this study include the large sample size and linkage of UK Biobank participants to the high-quality and high-coverage National Health Service cancer registries. Although UK Biobank participants are healthier than the general population, the size of the resource and the number of cancer cases likely provide a good assessment of aetiological associations between having been breastfed and cancer risk, which can be generalised [37]. The size of the cohort and long-term follow-up also facilitated assessment across many cancer sites in women and men separately, which few resources are capable of facilitating.
This study has important limitations. The precision in the measure of the exposure is limited owing to the categorising of breastfeeding into “ever” or “never” groups. This fails to account for individual heterogeneity in the duration, intensity, and exclusivity of breastfeeding. Detailed information on breastfeeding would allow a better assessment of how this may be associated with cancer, including investigation of dose-dependent associations and insight into the optimal duration of breastfeeding. The dichotomous nature of the exposure variable limits our interpretation as we are unable to examine a quantitative exposure to breastmilk. As we hypothesise that breastfeeding influences cancer risk through established cancer risk factors, the amount and length of exposure to breastfeeding are essential to describe. The measurement of the exposure variable is also a limitation of this study because the collection of breastfeeding data by participant recall potentially introduces non-differential misclassification bias, thus, we cannot preclude a potential underestimation of the results. Nevertheless, previous studies have described high levels of concordance between prospectively collected and recalled data on ever breastfeeding (yes/no), although agreement is higher if individuals are breastfed for at least 1 month [38].
The relatively large number of excluded individuals with missing breastfeeding data is a further limitation. We suggest that differences between those with and without breastfeeding data are driven by the missing data population being born earlier. As such, we cannot preclude some selection bias in the study. Despite this, those with breastfeeding data still represented a broad range of birth years. Among these, we found few interactions between breastfeeding and the birth-cohort in the associations with cancer, and thus, we find it unlikely that our analysis underestimates the effect of breastfeeding. For individual cancer sites with birth-cohort effect, they were limited and showed no consistent pattern or replication across cancer sites. Consequently, we conclude that the described birth-cohort effects were spurious and resulted from low numbers of cancers, which was reflected in the wide confidence intervals.
The associations between breastfeeding and many factors across the life course present methodological challenges, such as the identification of potential confounders. A critical data gap in the UK Biobank is the lack of information on maternal factors, such as maternal socioeconomic position, age, and obesity, which could potentially confound the observed associations, alongside influencing the duration and intensity of breastfeeding [36]. Models constructed also did not include birthweight as a potential confounder, as it was poorly recorded in the available data. Consequently, there is a risk of bias due to not controlling for birthweight. Moreover, the models did not include later life determinants of cancer, such as the family history of cancer, adult body size and body composition, socioeconomic factors, diet, or physical activity since these factors are mediators rather than confounders, and it was not the aim of this study to assess mediation through these factors. Other potentially important data such as information on complementary feeding or infant diet were not collected and are likely to have changed over the four decades over which the participants were born. This absence of this data restricts the interpretation of the results and relevance to contemporary populations where the availability of breastfeeding alternatives, as well as societal pressure and norms, will markedly differ.
There are also limitations to our interpretation of the findings resulting from the design of this study. As a result of the age profile of participants in the UK Biobank, we are unable to extend our findings to lifetime cancer risk, especially for cancers with earlier ages of onset. Examination of these associations in a younger population would be an important addition to future studies. The UK Biobank is susceptible to survival bias as participants had to survive into middle age to be included. If having been breastfed is associated with cancer or survival before enrolment, which we expect, these effects could lead to under- or over-estimation of the effect sizes. We also investigated associations with many cancer forms, increasing the family-wise error rate. The cancer site-specific associations have been interpreted conservatively as these could be spurious findings that require further validation.
In conclusion, we found limited evidence of an association between having been breastfed and adult cancer risk in men and women. Having been breastfed was associated with a marginally increased risk of adult cancer in women, but no evidence of an association was reported in men. Site-specific analyses indicated that women who were breastfed had an increased risk of both breast and ovarian cancer, although these associations were not maintained after adjustment for multiple tests. Men who were breastfed as infants had a reduced risk of oesophageal cancer. For the interpretation of these results, we stress that the deleterious effects reported here are far outweighed by the immeasurable benefits of being breastfed for both mother and child. As the UK and European countries struggle to achieve the WHO recommendations on breastfeeding, these findings should not undermine efforts to create the conditions for initiation of and sustained breastfeeding.
Data availability
All data is publicly available from the UK Biobank. All code used for the completion of this manuscript will be made available as highlighted in the text.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53.
Kanavos P. The rising burden of cancer in the developing world. Ann Oncol 2006;17:viii15–23.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–90.
Horta BL, Loret de Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:30–7.
Theurich MA, Davanzo R, Busck-Rasmussen M, Díaz-Gómez NM, Brennan C, Kylberg E, et al. Breastfeeding rates and programs in Europe: a survey of 11 National Breastfeeding Committees and representatives. J Pediatr Gastroenterol Nutr. 2019;68:400–7.
McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey, UK Data Service. 2010.
Wang X, Yan M, Zhang Y, Wang W, Zhang W, Luo J, et al. Breastfeeding in infancy and mortality in middle and late adulthood: a prospective cohort study and meta‐analysis. J Intern Med. 2023;293:624–35.
Martin RM. Association between breast feeding and growth: the Boyd-Orr cohort study. Arch Dis Child Fetal Neonatal Ed. 2002;87:193F–201.
Pontin D, Emmett P, Steer C, Emond A, the ALSPAC Study Team. Patterns of breastfeeding in a UK longitudinal cohort study. Matern Child Nutr. 2007;3:2–9.
Su Q, Sun X, Zhu L, Yan Q, Zheng P, Mao Y, et al. Breastfeeding and the risk of childhood cancer: a systematic review and dose-response meta-analysis. BMC Med. 2021;19:90.
Murphy MFG, Bithell JF, Stiller CA, Kendall GM, O’Neill KA. Childhood and adult cancers: contrasts and commonalities. Maturitas. 2013;76:95–8.
Yang TO, Cairns BJ, Green J, Reeves GK, Floud S, Bradbury KE, et al. Adult cancer risk in women who were breastfed as infants: large UK prospective study. Eur J Epidemiol. 2019;34:863–70.
Martin RM, Middleton N, Gunnell D, Owen CG, Smith GD. Breast-feeding and cancer: the Boyd Orr cohort and a systematic review with meta-analysis. J Natl Cancer Inst. 2005;97:1446–57.
Gillman MW, Rifas-Shiman SL, Berkey CS, Frazier AL, Rockett HRH, Camargo CA, et al. Breast-feeding and overweight in adolescence: within-family analysis. Epidemiol Camb Mass. 2006;17:112–4.
Rudnicka AR, Owen CG, Strachan DP. The effect of breastfeeding on cardiorespiratory risk factors in adult life. Pediatrics. 2007;119:e1107–115.
Dewey KG, Güngör D, Donovan SM, Madan EM, Venkatramanan S, Davis TA, et al. Breastfeeding and risk of overweight in childhood and beyond: a systematic review with emphasis on sibling-pair and intervention studies. Am J Clin Nutr. 2021;114:1774–90.
Cottrell EC, Ozanne SE. Developmental programming of energy balance and the metabolic syndrome. Proc Nutr Soc. 2007;66:198–206.
Dewey KG. Growth characteristics of breast-fed compared to formula-fed infants. Biol Neonate. 1998;74:94–105.
Arenz S, Rückerl R, Koletzko B, von Kries R. Breast-feeding and childhood obesity-a systematic review. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2004;28:1247–56.
Mason AL, Gilady SY, Mackey JR. Mouse mammary tumor virus in human breast cancer. Am J Pathol. 2011;179:1588–90.
Yu JC, Khodadadi H, Malik A, Davidson B, Salles ÉDSL, Bhatia J, et al. Innate immunity of neonates and infants. Front Immunol. 2018;9:1759.
Gregory KE, Samuel BS, Houghteling P, Shan G, Ausubel FM, Sadreyev RI, et al. Influence of maternal breast milk ingestion on acquisition of the intestinal microbiome in preterm infants. Microbiome. 2016;4:68.
Ximenez C, Torres J. Development of microbiota in infants and its role in maturation of gut mucosa and immune system. Arch Med Res. 2017;48:666–80.
Sarkar A, Yoo JY, Valeria Ozorio Dutra S, Morgan KH, Groer M. The Association between early-life gut microbiota and long-term. Health Dis J Clin Med. 2021;10:459.
Collins, R. UK Biobank Protocol, 2007. https://www.ukbiobank.ac.uk/media/gnkeyh2q/study-rationale.pdf.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Henson KE, Elliss-Brookes L, Coupland VH, Payne E, Vernon S, Rous B, et al. Data resource profile: National Cancer Registration Dataset in England. Int J Epidemiol. 2020;49:16–16h.
Dorak MT, Karpuzoglu E. Gender differences in cancer susceptibility: an inadequately addressed issue. Front Genet. 2012;3:268.
Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13:1141–51.
Baer HJ, Tworoger SS, Hankinson SE, Willett WC. Body fatness at young ages and risk of breast cancer throughout life. Am J Epidemiol. 2010;171:1183–94.
Yang TO, Cairns BJ, Pirie K, Green J, Beral V, Floud S, et al. Body size in early life and the risk of postmenopausal breast cancer. BMC Cancer. 2022;22:232.
Martin RM, Kramer MS, Patel R, Rifas-Shiman SL, Thompson J, Yang S, et al. Effects of promoting long-term, exclusive breastfeeding on adolescent adiposity, blood pressure, and growth trajectories: a secondary analysis of a randomized clinical trial. JAMA Pediatr. 2017;171:e170698.
Ding N, Zhan J, Shi Y, Qiao T, Li P, Zhang T. Obesity in children and adolescents and the risk of ovarian cancer: a systematic review and dose‒response meta-analysis. PLoS ONE. 2022;17:e0278050.
Clarke MA, Joshu CE. Early life exposures and adult cancer risk. Epidemiol Rev. 2017;39:11–27.
Michels KB, Trichopoulos D, Rosner BA, Hunter DJ, Colditz GA, Hankinson SE, et al. Being breastfed in infancy and breast cancer incidence in adult life: results from the two nurses’ health studies. Am J Epidemiol. 2001;153:275–83.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Cairns BJ, Liu B, Clennell S, Cooper R, Reeves GK, Beral V, et al. Lifetime body size and reproductive factors: comparisons of data recorded prospectively with self reports in middle age. BMC Med Res Methodol. 2011;11:7.
Acknowledgements
The authors would like to thank the UK Biobank for approving the project and maintaining the data resource.
Funding
This work was supported by a grant from the Novo Nordisk Foundation awarded to LGB (NNF21OC0071349). The funders were not involved in the design of the study, analysis of data or interpretation of results.
Author information
Authors and Affiliations
Contributions
LGB, JLB and KMR contributed to the study’s inception. DHB, LGB, BWJ, JA, JLB and DCP contributed to the analysis strategy and design. DHB conducted the analysis and drafted the manuscript. All authors were involved in the data interpretation. All authors critically revised the manuscript for important intellectual content and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent
This research has been conducted using the UK Biobank resource under application number 95095. The UK Biobank Research Tissue Bank approval covers this research. The Research Ethics Committee approval number for the UK Biobank is 16/NW/0274. This work uses data provided by patients and collected by the NHS as part of their care and support.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hameiri-Bowen, D., Pedersen, D.C., Jensen, B.W. et al. The association between being breastfed in infancy and risks of cancer in adulthood—a UK Biobank study. BJC Rep 2, 40 (2024). https://doi.org/10.1038/s44276-024-00061-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44276-024-00061-x