Abstract
Background
Transglutaminase 2 (TGM2) is a protein expressed in several isoforms in both intra- and extra-cellular tissue compartments. It has multiple functions that are important in cancer biology and several small studies have suggested expression of TGM2 in breast cancers is associated with a poorer prognosis. The aim of this study was to evaluate the role of intra-cellular and extra-cellular TGM2 expression in breast cancer and to determine whether there were any differences by hormone receptor status.
Methods
We carried out TGM2 immunostaining of tissue micro-arrays comprising 2169 tumour cores and scored these for both intra- and extra-cellular and expression.
Results
Intra-cellular (tumour cell) TGM2 positivity was associated with a better prognosis (HR = 0.74, 95% CI 0.59–0.92) with a larger effect stronger in hormone-receptor-negative cases (HR = 0.56, 95% CI 0.37–0.85). Extra-cellular (stromal) TGM2 expression was associated with a poorer prognosis (HR = 1.47, 95% CI 1.06–2.03) with a stronger association in hormone-receptor-positive cases (HR = 1.60, 95% CI 1.09–2.34).
Conclusion
Tissue compartment and hormone receptor status differences in the effect of TGM2 expression on clinical outcomes of breast cancer may reflect the different functions of TGM2.
Similar content being viewed by others
Background
Breast cancer is a heterogeneous disease, and the prognosis of early breast cancer varies substantially depending on clinico-pathological features and molecular characteristics. These factors are used to guide treatment decisions. The PREDICT breast prognostication and treatment benefit model is based on age at diagnosis, mode of detection, tumour size, tumour grade, number of positive lymph nodes and expression of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2) and the marker of proliferation Kiel 67 (KI67) [1, 2]. Many other tumour proteins have been evaluated as prognostic biomarkers. For example, cytokeratin 5/6 (CK5/6) and epidermal growth factor receptor (EGFR) are markers of disease that originated from basal cells [3].
Transglutaminase 2 (TGM2), a member of a family of calcium-dependent transglutaminase enzymes, is a multifunctional protein, under the control of intracellular GTP and calcium levels. TGM2 modifies proteins by catalysing the formation of ε(γ-glutamyl)-lysine bonds; it is instrumental in protein polymerisation and incorporation of diamines and polyamines into proteins [4]. This multiply-spliced gene product of TGM2 is expressed both intra- and extracellularly and its diverse roles are conformation and isoform dependent [5]. TGM2 is expressed in many tissues, but it not expressed in normal breast epithelium [6]. However, TGM2 and TGM2 are up-regulated in breast cancer [6] and TGM2 has been shown to play multiple roles in the biology of breast cancer including cell adhesion, invasion and survival [7], programmed cell death [8], cell signalling [9], and metabolic reprogramming [10]. TGM2 has also been suggested to limit metastasis of colon cancer cells by effectively forming restrictive fibrillar networks in the stroma [11]. The two major isoforms of TGM2, TGM2-long and the truncated TGM2-short, are proposed to have opposing roles in cancer, being pro-cell-survival and pro-apoptotic, respectively [12].
Thus, tumour TGM2 expression is a good candidate as a biomarker of prognosis in breast cancer. Several studies have reported on the association between TGM2 expression and prognosis in breast cancer [6, 13, 14] with increased expression being associated with a poorer prognosis. However, the largest of these studies [13] was based on just 412 patients and no study has evaluated the role of TGM2 expression according to tumour hormone receptor status or has evaluated both intra-cellular expression and extra-cellular expression. The aim of this work was to assess the association between expression of TGM2 in both tumour and stromal compartment in invasive hormone receptor positive and hormone receptor negative female breast cancer in a cohort of 2169 women with early invasive breast cancer.
Materials and methods
Study population
The Study of Epidemiology and Risk in Cancer Heredity (SEARCH), is population-based and consists of two study populations. The populations were prevalent cases (diagnosed at under 55 years of age from 1991 to 1996 and still alive when the study started in 1996), and incident cases (diagnosed at under 70 years of age after 1996). Cases were identified through the East Anglia Cancer Registry until 2003 and subsequently through the Eastern Cancer Registry and Information Service (ECRIC). Follow-up by the Cancer Registry was carried out through national death registration. Participants with breast cancer (ICD10 code C50) recorded on Part I of the death certificate were considered to have died from breast cancer. SEARCH is approved by the National Research Ethics Service Cambridgeshire Committee and all participants provided written, informed consent.
Tissue microarray (TMA) construction
Pathology blocks from 2169 patients were retrieved for tissue micro-array construction. Tissue microarray blocks were constructed using donor pathology blocks taken at the time of primary surgery before any treatment. The position for core selection was guided by slides stained with haematoxylin and eosin with areas of invasive carcinoma marked by a pathologist. Each tumour is represented by a single 0.6 mm core in a TMA constructed from paraffin-embedded tissue blocks.
Assigning hormone-receptor-status to cases
Sections from each TMA were previously stained for ER and PR and scored using the Allred system [15]. Allred scores of three or more were considered positive. ER status data from the clinical record were also available for some cases with missing data from the TMAs. Cases were designated hormone-receptor-positive if either oestrogen receptor (ER) or progesterone receptor (PR) status was positive. Where data were missing for one of the markers, as was the case in 65 cases (2 lacked ER status and 63 lacked PR status), hormone-receptor status was based on the single marker – some of the hormone-receptor-negative cases may thus be misclassified. However, where both ER and PR status was known there was agreement in 84% of cases, thus misclassification is suggested to have happened only in approximately 10 cases.
IHC staining of TGM2
Antigen retrieval was performed using an antigen access unit, supplied by Menarini Diagnostics, with Menarini access tris buffer. The slides were transferred to an IntelliPATH autostainer; all of the incubations were at ambient temperature and the following reagents and timings were applied: five minutes with Menarini peroxidase block; five minutes with Menarini casein block; one hour with Abcam TGM2 antibody (ab2386) diluted to a concentration of 1:500; ten minutes with Menarini universal probe; and fifteen minutes with horseradish peroxidase. These steps were all followed by one wash with Menarini buffer 1, a ten-minute incubation with diaminobenzidine (DAB), two washes with water, one minute with Mayers haematoxylin, and finally one wash with water.
When present in tumour cells, TGM2 expression was almost exclusively in the cytoplasm. The tissue sections had the expected features of breast tumour tissue, including blood vessels, ducts, stroma and fibroblasts. Where cytoplasmic staining of TGM2 occurred, it was generally present in some, but not all, of the tumour cells in the sample. Where there was a mixture of stained and unstained cells, there were often small clusters of stained cells; in general, they were moderately well-distributed throughout the section.
Scoring TGM2 expression
Intra-cellular TGM2 expression in tumour cells and extra-cellular expression in stromal tissue was scored by a pathologist (EP) and a trained technician and PhD candidate (FMB). TGM2 staining intensity was scored on a four-point scale (0 = no staining, 1 = weak staining, 2 = medium staining and 3 = strong staining) and the percentage of tumour cells positive was estimated to the nearest ten per cent. Only invasive tumour cells were scored. Where the intensity was not consistent the most prevalent intensity was used. Scores of 10% or more were considered positive (Fig. 1). TGM2 was generally evenly distributed when present in the stroma; cases with medium or strong staining of 10% or more of the stroma were considered positive (Fig. 2).
a No staining (score of 0). b No staining, weak staining (representative score of 1 indicated with a green arrow) and medium staining. c Mainly medium (representative score of 2 indicated with a green arrow) staining with a few areas of strong staining. d Strong staining (representative score of 3 indicated with a black arrow).
Statistical analyses
All analyses were performed using R Statistical Software v4.1.2 [16], implemented in R studio v2022.7.1.554 [17]. Packages used were gap [18], tidyverse [19], survival [20], survminer [21] and tableone [22]. Associations between TGM2 expression and categorical variables were evaluated using standard χ2 tests. Associations between TGM2 expression and death from breast cancer were investigated using Cox proportional hazards regression. Follow-up time was taken from the date of diagnosis. As participants were recruited after diagnosis (left truncation), time at risk was taken from the date of entry into the study. Follow-up was censored on the date of death or on the date last known to be alive or at 15 years after diagnosis, whichever came first. The proportional hazards assumption was tested by assessing the correlation of the weighted Schoenfeld residuals with time. Analyses were carried out for all cases and for hormone-receptor-positive and hormone-receptor-negative cases separately.
Results
Tumours from 2169 cases were stained for TGM2. The numbers of cases by intra-cellular (tumour cell) TGM2 expression status and age group, hormone-receptor-status, grade, stage and extra-cellular (stromal) TGM2 expression are shown in Table 1. Intracellular and extracellular TGM2 status were only weakly correlated (Kappa = 0.095, P = 0.003). Outcome data were not available for 13 cases and so 2156 cases were included in the final set for time-to-event analyses. Of these, 431 (17%) died of breast cancer within 15 years of diagnosis. The fully adjusted models were based on a complete case analysis n = 1925 with complete data).
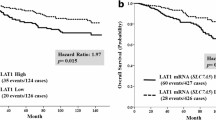
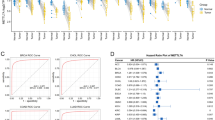
In univariable analysis intra-cellular (tumour cell) TGM2 positivity was associated with a better prognosis (HR = 0.75, 95% CI 0.61–0.92; P = 0.0053). The proportional hazards assumption was not violated (P = 0.27). There was little difference in the hazard ratio estimate after adjusting for stage and grade, which are known to affect patient survival, (Fig. 3a, HR = 0.74, 95% CI 0.59–0.92; P = 0.0059). However, the effect was stronger in hormone-receptor-negative cases (Fig. 3b, HR = 0.56, 95% CI 0.37–0.85; P = 0.0064) than in hormone-receptor-positive cases (Fig. 3c, HR = 0.87, 95% CI 0.67–1.12; P = 0.28). This difference was nominally statistically significant (P = 0.037).
TGM2 expression data in the stroma was obtainable for 901 cases. TGM2 stromal expression was associated with a poorer prognosis in univariable analysis (HRadj = 1.60, 95% CI 1.19–2.14, P = 0.0018) with some attenuation after adjusting for stage and grade ((HR = 1.47, 95% CI 1.06–2.03, P = 0.02). The association was stronger in hormone-receptor-positive cases (HRadj = 1.60, 95% CI 1.09–2.34, P = 0.015) with little evidence of any effect in hormone-receptor-negative cases (HR = 0.92, 95% CI 0.49–1.71, P = 0.78). However, the difference was not statistically significant (P = 0.15). In hormone receptor positive disease the association the effect was bigger in the intra-cellular TGM2 expression negative cases (HRadj = 1.88, 95% CI 1.17–3.02, P = 0.0092) than intra-cellular TGM2 expression positive cases (HRadj = 1.10, 95% CI 0.57–2.09, P = 0.78). Again, this difference was not statistically significant (P = 0.23).
Discussion
We have found modest evidence for an association between intra-cellular expression of TGM2 in the tumour cytoplasm and an improved prognosis in early breast cancer with a bigger effect in hormone-receptor-negative disease than in hormone-receptor positive disease. This is in contrast to previous studies that have evaluated the prognostic significance of TGM2 in breast tumours, all of which found that increased expression was associated with a poorer prognosis [6, 13, 14]. However, previous studies have not reported on the association stratified by hormone receptor status, nor did they report on the association with intra-cellular expression. One study reported only on the role of extra-cellular expression [14] and our findings support this observation as TGM2 expression in the stroma was associated with a poorer prognosis, an association that appeared to be restricted to hormone receptor positive disease. We used the Bayes False Discovery Probability (BDFP) to assist in the interpretation of each nominally significant association [23]. The BFDP is the probability that a reported significant association is a false positive given a specified prior probability that the alternative hypothesis is true. We have assumed that if the alternative hypothesis is true, the effect size is unlikely to be a hazard ratio greater than 1.5 or less than 0.67. As shown in Table 2, even under reasonably strong priors, the observed associations are quite likely to represent false positives. This is despite the large sample size of this study. Even larger sample sizes will be needed to confirm these associations with high confidence.
The observed associations are intriguing in their specificity. They suggest that the function of TGM2 in breast tumours depends on hormone-receptor-status and differs depending on whether it is expressed inside or outside of the cell. The weak correlation between intra-cellular expression in tumour cells and extra-cellular expression in the stroma suggests that cells other than the tumour are the source of the extracellular protein. Indeed, TGM2 may be produced in and secreted from various cell types including the fibroblasts that occur in the tissue stroma [24]. It is plausible that the differences between in effects of intra- and extra-cellular expression reflect the many different functions of TGM2 [5]. For example, TGM2 has been shown to promote inflammatory signalling which would be expected to be associated with poorer outcomes [13] and targeted depletion of TGM2 inhibits metastasis, while overexpression of TG2 enhances metastasis [25]. On the other hand, tumour progression was increased and survival rate reduced in TGM2 knockout mice compared to wild-type [11] and TGM2 activation induces programmed cell death [8]. Additional complexity comes from the fact that the different isoforms may be differentially expressed in different tumours and have different functions. However, the antibody used for the present work detects total TGM2 and is unable to distinguish isoforms; isoform specific antibodies are not currently available.
A limitation of this study is the use of TGM2 expression derived from a single 0.6 mm core of tumour tissue. All tumours will have some degree of spatial heterogeneity in their morphology and molecular characteristics, and a single sample may not be representative of the tumour. Thus, the TGM2 expression based on a single core can be considered a form of random measurement error. Consequently, there will be some attenuation of any true associations.
In conclusion, we have found evidence to support previous publications that have suggested breast cancers that express TGM2 in the stoma are associated a poorer than those that do not express TGM2. A possible association of intra-cellular TGM2 expression with a better prognosis in invasive breast cancer has not been reported previously and needs confirmation in independent data sets.
Data availability
The data and analysis code (R script) to reproduce the results reported in this manuscript are available from the corresponding author on request.
References
Candido Dos Reis FJ, Wishart GC, Dicks EM, Greenberg D, Rashbass J, Schmidt MK, et al. An updated PREDICT breast cancer prognostication and treatment benefit prediction model with independent validation. Breast Cancer Res. 2017;19:58.
Grootes I, Keeman R, Blows FM, Milne RL, Giles GG, Swerdlow AJ, et al. Incorporating progesterone receptor expression into the PREDICT breast prognostic model. Eur J Cancer. 2022;173:178–93.
Siziopikou KP, Cobleigh M. The basal subtype of breast carcinomas may represent the group of breast tumors that could benefit from EGFR-targeted therapies. Breast. 2007;16:104–7.
Sarkar NK, Clarke DD, Waelsch H. An enzymically catalyzed incorporation of amines into proteins. Biochim Biophys Acta. 1957;25:451–2.
Gundemir S, Colak G, Tucholski J, Johnson GV. Transglutaminase 2: a molecular Swiss army knife. Biochim Biophys Acta. 2012;1823:406–19.
Xu D, Xu N, Sun L, Yang Z, He M, Li Y. TG2 as a novel breast cancer prognostic marker promotes cell proliferation and glycolysis by activating the MEK/ERK/LDH pathway. BMC Cancer. 2022;22:1267.
Mangala LS, Fok JY, Zorrilla-Calancha IR, Verma A, Mehta K. Tissue transglutaminase expression promotes cell attachment, invasion and survival in breast cancer cells. Oncogene. 2007;26:2459–70.
Fok JY, Mehta K. Tissue transglutaminase induces the release of apoptosis inducing factor and results in apoptotic death of pancreatic cancer cells. Apoptosis. 2007;12:1455–63.
Brown KD. Transglutaminase 2 and NF-kappaB: an odd couple that shapes breast cancer phenotype. Breast Cancer Res Treat. 2013;137:329–36.
Kumar S, Donti TR, Agnihotri N, Mehta K. Transglutaminase 2 reprogramming of glucose metabolism in mammary epithelial cells via activation of inflammatory signaling pathways. Int J Cancer. 2014;134:2798–807.
Jones RA, Kotsakis P, Johnson TS, Chau DY, Ali S, Melino G, et al. Matrix changes induced by transglutaminase 2 lead to inhibition of angiogenesis and tumor growth. Cell Death Differ. 2006;13:1442–53.
Antonyak MA, Jansen JM, Miller AM, Ly TK, Endo M, Cerione RA. Two isoforms of tissue transglutaminase mediate opposing cellular fates. Proc Natl Acad Sci USA. 2006;103:18609–14.
Oh K, Ko E, Kim HS, Park AK, Moon HG, Noh DY, et al. Transglutaminase 2 facilitates the distant hematogenous metastasis of breast cancer by modulating interleukin-6 in cancer cells. Breast Cancer Res. 2011;13:R96.
Assi J, Srivastava G, Matta A, Chang MC, Walfish PG, Ralhan R. Transglutaminase 2 overexpression in tumor stroma identifies invasive ductal carcinomas of breast at high risk of recurrence. PLoS One. 2013;8:e74437.
Harvey JM, Clark GM, Osborne CK, Allred DC. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol. 1999;17:1474–81.
R Core Team. R: A language and environment for statistical computing. 2021. https://www.R-project.org/.
R Studio Team. R Studio: Integrated Development for R. 2020. http://www.rstudio.com/.
Zhao JH. gap: Genetic Analysis Package. 2023. https://CRAN.R-project.org/package=gap.
Wickham H, Averick M, Bryan J, Chang W, McGowan LD, François R, et al. Welcome to the tidyverse. J Open Source Softw. 2019;4:1686.
Therneau T. A package for survival analysis in R. 2023. https://CRAN.R-project.org/package=survival.
Kassambara A, Kosinski M, Biecek P. survminer: Drawing Survival Curves using ‘ggplot2’. 2021. https://CRAN.R-project.org/package=survminer.
Yoshida K, Bartel A. tableone: Create ‘Table 1’ to Describe Baseline Characteristics with or without Propensity Score Weights. 2022. https://CRAN.R-project.org/package=tableone.
Wakefield J. A Bayesian measure of the probability of false discovery in genetic epidemiology studies. Am J Hum Genet. 2007;81:208–27.
Philp CJ, Siebeke I, Clements D, Miller S, Habgood A, John AE, et al. Extracellular matrix cross-linking enhances fibroblast growth and protects against matrix proteolysis in lung fibrosis. Am J Respir Cell Mol Biol. 2018;58:594–603.
Shinde A, Paez JS, Libring S, Hopkins K, Solorio L, Wendt MK. Transglutaminase-2 facilitates extracellular vesicle-mediated establishment of the metastatic niche. Oncogenesis. 2020;9:16.
Acknowledgements
We thank the all the women who have taken part in the SEARCH study; the SEARCH team for recruitment and data management; the many general practitioners and nurses for patient recruitment; the Histopathology Core at the Cambridge Institute. SEARCH was funded by Cancer Research UK (C490/A10119 C490/A10124 C490/A16561). This work was supported by the National Institute for Health Research Biomedical Research Centre at the University of Cambridge.
Author information
Authors and Affiliations
Contributions
FMB carried out the immunohistochemistry, scoring of the stained TMA and wrote the initial draft of the manuscript. WC and HRA helped in the construction of the tissue micro-arrays. EP supervised the scoring of the stained tissue micro-arrays. PDPP carried out the biostatistical analysis. CP and PC conceived the project and supervised the work. All authors edited the initial draft of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
SEARCH ovary was approved by the National Research Ethics Service East of England - Cambridge South Committee (#99/5/07). All participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementery information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blows, F.M., Ali, H.R., Cope, W. et al. Expression of transglutaminase-2 (TGM2) in the prognosis of female invasive breast cancer. BJC Rep 2, 5 (2024). https://doi.org/10.1038/s44276-023-00030-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44276-023-00030-w