Abstract
Combining cells, biomaterials and bioactive factors with biophysical cues to engineer cell and tissue constructs can address various applications, such as regenerative and personalized medicine, in addition to drug discovery and testing. However, challenges associated with the assembly of large, complex tissues integrating multiple cell types and functions require established technologies such as 3D printing to be combined with cell-assembly and cell-stimulation methods. Ultrasound is a potential tool for advancing tissue engineering, conferring the advantages of cytocompatibility and deep tissue penetration. In this Review, we discuss the application of ultrasound to the remote manipulation and assembly of biological building blocks, as well as the direct and indirect triggering of cellular processes, in combination with ultrasound-sensitive additives. Furthermore, we examine the role of ultrasound in tissue maturation, and in affecting the microenvironment and cell programming. Finally, we outline the challenges facing the technology and considerations for the widespread use of ultrasound in tissue engineering.
Key points
-
Ultrasound is a versatile and biocompatible method to remotely apply forces and transfer energy, with diverse potential applications in tissue engineering.
-
Parallel and rapid assembly of cells can be achieved by using ultrasound techniques in standalone setups or in combination with bioprinting to yield multilayer constructs with high local cell density.
-
Ultrasound can spatiotemporally alter the biochemical and biomechanical properties of scaffold materials to influence the fate of engineered cells and tissues.
-
Ultrasound can couple to cellular and molecular processes, manipulating cell behaviour and tissue morphogenesis.
-
Ultrasound methodologies will benefit from standardized protocols and instruments to allow widespread adoption in the tissue-engineering community.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Berthiaume, F., Maguire, T. J. & Yarmush, M. L. Tissue engineering and regenerative medicine: history, progress, and challenges. Annu. Rev. Chem. Biomol. Eng. 2, 403–430 (2011).
Hoffman, T., Khademhosseini, A. & Langer, R. Chasing the paradigm: clinical translation of 25 years of tissue engineering. Tissue Eng. Part A 25, 679–687 (2019).
Kim, Y. S., Smoak, M. M., Melchiorri, A. J. & Mikos, A. G. An overview of the tissue engineering market in the United States from 2011 to 2018. Tissue Eng. A 25, 1–8 (2019).
Lancaster, M. A. & Knoblich, J. A. Organogenesis in a dish: modeling development and disease using organoid technologies. Science 345, 1247125 (2014).
Loewa, A., Feng, J. J. & Hedtrich, S. Human disease models in drug development. Nat. Rev. Bioeng. https://doi.org/10.1038/s44222-023-00063-3 (2023).
Langhans, S. A. Three-dimensional in vitro cell culture models in drug discovery and drug repositioning. Front. Pharmacol. 9, 6 (2018).
Pampaloni, F. & Stelzer, E. H. Three-dimensional cell cultures in toxicology. Biotechnol. Genet. Eng. Rev. 26, 117–138 (2009).
Nuwer, R. US agency seeks to phase out animal testing. Nature https://doi.org/10.1038/d41586-022-03569-9 (2022).
Moysidou, C. M., Barberio, C. & Owens, R. M. Advances in engineering human tissue models. Front. Bioeng. Biotechnol. 8, 620962 (2020).
Nichol, J. W. & Khademhosseini, A. Modular tissue engineering: engineering biological tissues from the bottom up. Soft Matter 5, 1312–1319 (2009).
Blatchley, M. R. & Anseth, K. S. Middle-out methods for spatiotemporal tissue engineering of organoids. Nat. Rev. Bioeng. 1, 329–345 (2023).
Cho, S., Discher, D. E., Leong, K. W., Vunjak-Novakovic, G. & Wu, J. C. Challenges and opportunities for the next generation of cardiovascular tissue engineering. Nat. Methods 19, 1064–1071 (2022).
Agarwal, T., Subramanian, B. & Maiti, T. K. Liver tissue engineering: challenges and opportunities. ACS Biomater. Sci. Eng. 5, 4167–4182 (2019).
Takebe, T. & Wells, J. M. Organoids by design. Science 364, 956–959 (2019).
Matejčić, M. & Trepat, X. Mechanobiological approaches to synthetic morphogenesis: learning by building. Trends Cell Biol. 33, 95–111 (2023).
Rademakers, T., Horvath, J. M., Blitterswijk, C. A. & LaPointe, V. L. S. Oxygen and nutrient delivery in tissue engineering: approaches to graft vascularization. J. Tissue Eng. Regen. Med. 13, 1815–1829 (2019).
Auger, F. A., Gibot, L. & Lacroix, D. The pivotal role of vascularization in tissue engineering. Annu. Rev. Biomed. Eng. 15, 177–200 (2013).
Armstrong, J. P. K. & Stevens, M. M. Using remote fields for complex tissue engineering. Trends Biotechnol. 38, 254–263 (2020).
Dholakia, K., Drinkwater, B. W. & Ritsch-Marte, M. Comparing acoustic and optical forces for biomedical research. Nat. Rev. Phys. 2, 480–491 (2020).
Primo, G. A. & Mata, A. 3D patterning within hydrogels for the recreation of functional biological environments. Adv. Funct. Mater. 31, 2009574 (2021).
Ouyang, L. L., Armstrong, J. P. K., Salmeron-Sanchez, M. & Stevens, M. M. Assembling living building blocks to engineer complex tissues. Adv. Funct. Mater. 30, 1909009 (2020).
Rufo, J., Cai, F., Friend, J., Wiklund, M. & Huang, T. J. Acoustofluidics for biomedical applications. Nat. Rev. Methods Primers 2, 30 (2022).
Armstrong, J. P. K. et al. Engineering anisotropic muscle tissue using acoustic cell patterning. Adv. Mater. 30, 1802649 (2018).
Deshmukh, D. V. et al. Continuous production of acoustically patterned cells within hydrogel fibers for musculoskeletal tissue engineering. Adv. Funct. Mater. 32, 2113038 (2022).
Armstrong, J. P. K. et al. Tissue engineering cartilage with deep zone cytoarchitecture by high-resolution acoustic cell patterning. Adv. Healthc. Mater. 11, 2200481 (2022).
Chen, P., Guven, S., Usta, O. B., Yarmush, M. L. & Demirci, U. Biotunable acoustic node assembly of organoids. Adv. Healthc. Mater. 4, 1937–1943 (2015).
Cai, H. et al. Intelligent acoustofluidics enabled mini-bioreactors for human brain organoids. Lab Chip 21, 2194–2205 (2021).
Gong, Z. et al. Acoustic droplet printing tumor organoids for modeling bladder tumor immune microenvironment within a week. Adv. Healthc. Mater. 10, 2101312 (2021).
Friend, J. Acoustofluidics. Front. Acoust. 1, 1261027 (2023).
Melde, K., Mark, A. G., Qiu, T. & Fischer, P. Holograms for acoustics. Nature 537, 518–522 (2016).
Ma, Z. et al. Acoustic holographic cell patterning in a biocompatible hydrogel. Adv. Mater. 32, 1904181 (2020).
Gu, Y. et al. Acoustofluidic holography for micro- to nanoscale particle manipulation. ACS Nano 14, 14635–14645 (2020).
Jain, P., Kathuria, H. & Dubey, N. Advances in 3D bioprinting of tissues/organs for regenerative medicine and in-vitro models. Biomaterials 287, 121639 (2022).
Tibbitt, M. W. & Anseth, K. S. Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol. Bioeng. 103, 655–663 (2009).
Brassard, J. A., Nikolaev, M., Hubscher, T., Hofer, M. & Lutolf, M. P. Recapitulating macro-scale tissue self-organization through organoid bioprinting. Nat. Mater. 20, 22–29 (2021).
Gopinathan, J. & Noh, I. Recent trends in bioinks for 3D printing. Biomater. Res. 22, 11 (2018).
Harley, W. S. et al. Advances in biofabrication techniques towards functional bioprinted heterogeneous engineered tissues: a comprehensive review. Bioprinting 23, 00147 (2021).
Mohan, T. S., Datta, P., Nesaei, S., Ozbolat, V. & Ozbolat, I. T. 3D coaxial bioprinting: process mechanisms, bioinks and applications. Prog. Biomed. Eng. 4, 022003 (2022).
Zhang, Y. S. et al. 3D extrusion bioprinting. Nat. Rev. Methods Primers 1, 75 (2021).
Jentsch, S. et al. Multiscale 3D bioprinting by nozzle-free acoustic droplet ejection. Small Methods 5, e2000971 (2021).
Fang, Y. et al. Rapid generation of multiplexed cell cocultures using acoustic droplet ejection followed by aqueous two-phase exclusion patterning. Tissue Eng. Part C 18, 647–657 (2012).
Guillotin, B. & Guillemot, F. Cell patterning technologies for organotypic tissue fabrication. Trends Biotechnol. 29, 183–190 (2011).
You, S. et al. High cell density and high-resolution 3D bioprinting for fabricating vascularized tissues. Sci. Adv. 9, eade7923 (2023).
Bernal, P. N. et al. Volumetric bioprinting of complex living-tissue constructs within seconds. Adv. Mater. 31, 1904209 (2019).
Ouyang, L. Pushing the rheological and mechanical boundaries of extrusion-based 3D bioprinting. Trends Biotechnol. 40, 891–902 (2022).
Banerjee, D. et al. Strategies for 3D bioprinting of spheroids: a comprehensive review. Biomaterials 291, 121881 (2022).
Xin, S. et al. Generalizing hydrogel microparticles into a new class of bioinks for extrusion bioprinting. Sci. Adv. 7, eabk3087 (2021).
Ou, Y. et al. Bioprinting microporous functional living materials from protein-based core–shell microgels. Nat. Commun. 14, 322 (2023).
Fennema, E., Rivron, N., Rouwkema, J., van Blitterswijk, C. & de Boer, J. Spheroid culture as a tool for creating 3D complex tissues. Trends Biotechnol. 31, 108–115 (2013).
Safaee, S., Schock, M., Joyee, E. B., Pan, Y. & Chen, R. K. Field-assisted additive manufacturing of polymeric composites. Addit. Manuf. 51, 102642 (2022).
Chansoria, P. & Shirwaiker, R. 3D bioprinting of anisotropic engineered tissue constructs with ultrasonically induced cell patterning. Addit. Manuf. 32, 101042 (2020).
Sriphutkiat, Y., Kasetsirikul, S., Ketpun, D. & Zhou, Y. Cell alignment and accumulation using acoustic nozzle for bioprinting. Sci. Rep. 9, 17774 (2019).
Shao, M. H., Cui, B., Zheng, T. F. & Wang, C. H. Ultrasonic manipulation of cells for alleviating the clogging of extrusion-based bioprinting nozzles. J. Phys. Conf. Ser. 1798, 012009 (2021).
Chansoria, P., Narayanan, L. K., Schuchard, K. & Shirwaiker, R. Ultrasound-assisted biofabrication and bioprinting of preferentially aligned three-dimensional cellular constructs. Biofabrication 11, 035015 (2019).
Guex, A. G., Di Marzio, N., Eglin, D., Alini, M. & Serra, T. The waves that make the pattern: a review on acoustic manipulation in biomedical research. Mater. Today Bio 10, 100110 (2021).
Wiklund, M. Acoustofluidics 12: biocompatibility and cell viability in microfluidic acoustic resonators. Lab Chip 12, 2018–2028 (2012).
Ayan, B. et al. Aspiration-assisted freeform bioprinting of prefabricated tissue spheroids in a yield-stress gel. Commun. Phys. 3, 183 (2020).
Olofsson, K., Hammarström, B. & Wiklund, M. Ultrasonic based tissue modelling and engineering. Micromachines 9, 594 (2018).
Athanassiadis, A. G. et al. Ultrasound-responsive systems as components for smart materials. Chem. Rev. 122, 5165–5208 (2022).
Hartono, D. et al. On-chip measurements of cell compressibility via acoustic radiation. Lab Chip 11, 4072–4080 (2011).
Olofsson, K., Hammarström, B. & Wiklund, M. Acoustic separation of living and dead cells using high density medium. Lab Chip 20, 1981–1990 (2020).
Jeger-Madiot, N. et al. Controlling the force and the position of acoustic traps with a tunable acoustofluidic chip: application to spheroid manipulations. J. Acoust. Soc. Am. 151, 4165–4179 (2022).
Olofsson, K. et al. Acoustic formation of multicellular tumor spheroids enabling on-chip functional and structural imaging. Lab Chip 18, 2466–2476 (2018).
Christakou, A. E., Ohlin, M., Onfelt, B. & Wiklund, M. Ultrasonic three-dimensional on-chip cell culture for dynamic studies of tumor immune surveillance by natural killer cells. Lab Chip 15, 3222–3231 (2015).
Olofsson, K., Carannante, V., Takai, M., Onfelt, B. & Wiklund, M. Ultrasound-based scaffold-free core–shell multicellular tumor spheroid formation. Micromachines 12, 329 (2021).
Bouyer, C. et al. A bio-acoustic levitational (BAL) assembly method for engineering of multilayered, 3D brain-like constructs, using human embryonic stem cell derived neuro-progenitors. Adv. Mater. 28, 161–167 (2016).
Comeau, E. S., Hocking, D. C. & Dalecki, D. Ultrasound patterning technologies for studying vascular morphogenesis in 3D. J. Cell Sci. 130, 232–242 (2017).
Kang, B. et al. High-resolution acoustophoretic 3D cell patterning to construct functional collateral cylindroids for ischemia therapy. Nat. Commun. 9, 5402 (2018).
Comeau, E. S. et al. In vivo acoustic patterning of endothelial cells for tissue vascularization. Sci. Rep. 13, 16082 (2023).
Baudoin, M. & Thomas, J. L. Acoustic tweezers for particle and fluid micromanipulation. Annu. Rev. Fluid Mech. 52, 205–234 (2019).
Chen, K. et al. Rapid formation of size-controllable multicellular spheroids via 3D acoustic tweezers. Lab Chip 16, 2636–2643 (2016).
Guo, F. et al. Three-dimensional manipulation of single cells using surface acoustic waves. Proc. Natl Acad. Sci. USA 113, 1522–1527 (2016).
Cai, H. et al. Trapping cell spheroids and organoids using digital acoustofluidics. Biofabrication 12, 035025 (2020).
Gao, Z. et al. A multifunctional acoustic tweezer for heterogenous assembloids patterning. Small Struct. 4, 2200288 (2023).
Baudoin, M. et al. Spatially selective manipulation of cells with single-beam acoustical tweezers. Nat. Commun. 11, 4244 (2020).
Cox, L., Croxford, A. & Drinkwater, B. W. Dynamic patterning of microparticles with acoustic impulse control. Sci. Rep. 12, 14549 (2022).
Cox, L., Melde, K., Croxford, A., Fischer, P. & Drinkwater, B. W. Acoustic hologram enhanced phased arrays for ultrasonic particle manipulation. Phys. Rev. Appl. 12, 064055 (2019).
Ma, Z. et al. Spatial ultrasound modulation by digitally controlling microbubble arrays. Nat. Commun. 11, 4537 (2020).
Melde, K. et al. Compact holographic sound fields enable rapid one-step assembly of matter in 3D. Sci. Adv. 9, eadf6182 (2023).
Athanassiadis, A. G. et al. Multiplane diffractive acoustic networks. IEEE Trans. Ultrason. Ferroelect. Freq. Contr. 70, 441–448 (2023).
Chen, P. et al. Microscale assembly directed by liquid-based template. Adv. Mater. 26, 5936–5941 (2014).
Ren, T., Chen, P., Gu, L., Ogut, M. G. & Demirci, U. Soft ring-shaped cellu-robots with simultaneous locomotion in batches. Adv. Mater. 32, 1905713 (2020).
Wang, J. et al. Acoustic fabrication of living cardiomyocyte-based hybrid biorobots. ACS Nano 16, 10219–10230 (2022).
Serpooshan, V. et al. Bioacoustic-enabled patterning of human iPSC-derived cardiomyocytes into 3D cardiac tissue. Biomaterials 131, 47–57 (2017).
Petta, D. et al. Sound-induced morphogenesis of multicellular systems for rapid orchestration of vascular networks. Biofabrication 13, 015004 (2020).
Di Marzio, N. et al. Sound-based assembly of a microcapillary network in a Saturn-like tumor model for drug testing. Mater. Today Bio 16, 100357 (2022).
Tognato, R. et al. Sound-based assembly of three-dimensional cellularized and acellularized constructs. Mater. Today Bio 22, 100775 (2023).
Gu, L. et al. Size- and density-dependent acoustic differential bioassembly of spatially defined heterocellular architecture. Biofabrication 15, 015019 (2023).
Wu, D. et al. Biomolecular actuators for genetically selective acoustic manipulation of cells. Sci. Adv. 9, eadd9186 (2023).
Bach, J. S. & Bruus, H. Suppression of acoustic streaming in shape-optimized channels. Phys. Rev. Lett. 124, 214501 (2020).
Karlsen, J. T., Qiu, W., Augustsson, P. & Bruus, H. Acoustic streaming and its suppression in inhomogeneous fluids. Phys. Rev. Lett. 120, 054501 (2018).
Qiu, W., Karlsen, J. T., Bruus, H. & Augustsson, P. Experimental characterization of acoustic streaming in gradients of density and compressibility. Phys. Rev. Appl. 11, 024018 (2019).
Hammarström, B., Laurell, T. & Nilsson, J. Seed particle-enabled acoustic trapping of bacteria and nanoparticles in continuous flow systems. Lab Chip 12, 4296–4304 (2012).
Bazou, D., Castro, A. & Hoyos, M. Controlled cell aggregation in a pulsed acoustic field. Ultrasonics 52, 842–850 (2012).
Hoyos, M. & Castro, A. Controlling the acoustic streaming by pulsed ultrasounds. Ultrasonics 53, 70–76 (2013).
Wolfenson, H., Yang, B. & Sheetz, M. P. Steps in mechanotransduction pathways that control cell morphology. Annu. Rev. Physiol. 81, 585–605 (2019).
Hofer, M. & Lutolf, M. P. Engineering organoids. Nat. Rev. Mater. 6, 402–420 (2021).
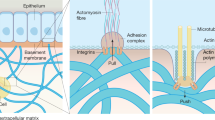
Saraswathibhatla, A., Indana, D. & Chaudhuri, O. Cell–extracellular matrix mechanotransduction in 3D. Nat. Rev. Mol. Cell Biol. 24, 495–516 (2023).
Chaudhuri, O., Cooper-White, J., Janmey, P. A., Mooney, D. J. & Shenoy, V. B. Effects of extracellular matrix viscoelasticity on cellular behaviour. Nature 584, 535–546 (2020).
Elosegui-Artola, A. et al. Matrix viscoelasticity controls spatiotemporal tissue organization. Nat. Mater. 22, 117–127 (2023).
Kim, T. et al. Deep brain stimulation by blood–brain-barrier-crossing piezoelectric nanoparticles generating current and nitric oxide under focused ultrasound. Nat. Biomed. Eng. 7, 149–163 (2023).
Carley, E., King, M. C. & Guo, S. Integrating mechanical signals into cellular identity. Trends Cell Biol. 32, 669–680 (2022).
Maresca, D. et al. Biomolecular ultrasound and sonogenetics. Annu. Rev. Chem. Biomol. Eng. 9, 229–252 (2018).
Norris, E. G., Dalecki, D. & Hocking, D. C. Using acoustic fields to fabricate ECM-based biomaterials for regenerative medicine applications. Recent Prog. Mater. 2, 1–24 (2020).
Blinc, A., Francis, C., Trudnowski, J. & Carstensen, E. Characterization of ultrasound-potentiated fibrinolysis in vitro. Blood 81, 2636–2643 (1993).
Garvin, K. A., VanderBurgh, J., Hocking, D. C. & Dalecki, D. Controlling collagen fiber microstructure in three-dimensional hydrogels using ultrasound. J. Acoust. Soc. Am. 134, 1491–1502 (2013).
Ray, A. & Provenzano, P. P. Aligned forces: origins and mechanisms of cancer dissemination guided by extracellular matrix architecture. Curr. Opin. Cell Biol. 72, 63–71 (2021).
Huebsch, N. et al. Ultrasound-triggered disruption and self-healing of reversibly cross-linked hydrogels for drug delivery and enhanced chemotherapy. Proc. Natl Acad. Sci. USA 111, 9762–9767 (2014).
Sun, Y., Chen, L.-G., Fan, X.-M. & Pang, J.-L. Ultrasound responsive smart implantable hydrogels for targeted delivery of drugs: reviewing current practices. Int. J. Nanomed. 17, 5001–5026 (2022).
Lutolf, M. P. et al. Synthetic matrix metalloproteinase-sensitive hydrogels for the conduction of tissue regeneration: engineering cell-invasion characteristics. Proc. Natl Acad. Sci. USA 100, 5413–5418 (2003).
Kloxin, A. M., Kasko, A. M., Salinas, C. N. & Anseth, K. S. Photodegradable hydrogels for dynamic tuning of physical and chemical properties. Science 324, 59–63 (2009).
Huo, S. et al. Mechanochemical bond scission for the activation of drugs. Nat. Chem. 13, 131–139 (2021).
Chandan, R., Mehta, S. & Banerjee, R. Ultrasound-responsive carriers for therapeutic applications. ACS Biomater. Sci. Eng. 6, 4731–4747 (2020).
Moreno‐Gomez, N., Athanassiadis, A. G., Poortinga, A. T. & Fischer, P. Antibubbles enable tunable payload release with low‐intensity ultrasound. Adv. Mater. 35, 2305296 (2023).
Kim, G. et al. High-intensity focused ultrasound-induced mechanochemical transduction in synthetic elastomers. Proc. Natl Acad. Sci. USA 116, 10214–10222 (2019).
Lampi, M. C. & Reinhart-King, C. A. Targeting extracellular matrix stiffness to attenuate disease: from molecular mechanisms to clinical trials. Sci. Transl. Med. 10, eaao0475 (2018).
Barriga, E. H., Franze, K., Charras, G. & Mayor, R. Tissue stiffening coordinates morphogenesis by triggering collective cell migration in vivo. Nature 554, 523–527 (2018).
Nele, V. et al. Ultrasound-triggered enzymatic gelation. Adv. Mater. 32, 1905914 (2020).
Sheeran, P. S., Luois, S. H., Mullin, L. B., Matsunaga, T. O. & Dayton, P. A. Design of ultrasonically-activatable nanoparticles using low boiling point perfluorocarbons. Biomaterials 33, 3262–3269 (2012).
Farrell, E. et al. Spatiotemporal control of myofibroblast activation in acoustically-responsive scaffolds via ultrasound-induced matrix stiffening. Acta Biomater. 138, 133–143 (2022).
McBeath, R., Pirone, D. M., Nelson, C. M., Bhadriraju, K. & Chen, C. S. Cell shape, cytoskeletal tension, and rhoa regulate stem cell lineage commitment. Dev. Cell 6, 483–495 (2004).
Connelly, J. T. et al. Actin and serum response factor transduce physical cues from the microenvironment to regulate epidermal stem cell fate decisions. Nat. Cell Biol. 12, 711–718 (2010).
Gjorevski, N. et al. Tissue geometry drives deterministic organoid patterning. Science 375, eaaw9021 (2022).
Paun, I. A. et al. Osteogenic cells differentiation on topological surfaces under ultrasound stimulation. J. Mater. Sci. 54, 11213–11230 (2019).
Higgins, S. G. et al. High‐aspect‐ratio nanostructured surfaces as biological metamaterials. Adv. Mater. 32, 1903862 (2020).
Lim, W. A. The emerging era of cell engineering: harnessing the modularity of cells to program complex biological function. Science 378, 848–852 (2022).
Iacoponi, F. et al. Optimal low-intensity pulsed ultrasound stimulation for promoting anti-inflammatory effects in macrophages. APL Bioeng. 7, 016114 (2023).
Fechheimer, M. et al. Transfection of mammalian cells with plasmid DNA by scrape loading and sonication loading. Proc. Natl Acad. Sci. USA 84, 8463–8467 (1987).
Bao, S., Thrall, B. D. & Miller, D. L. Transfection of a reporter plasmid into cultured cells by sonoporation in vitro. Ultrasound Med. Biol. 23, 953–959 (1997).
Qiu, Y. et al. The correlation between acoustic cavitation and sonoporation involved in ultrasound-mediated DNA transfection with polyethylenimine (PEI) in vitro. J. Control. Rel. 145, 40–48 (2010).
Stewart, M. P., Langer, R. & Jensen, K. F. Intracellular delivery by membrane disruption: mechanisms, strategies, and concepts. Chem. Rev. 118, 7409–7531 (2018).
Mizrahi, N. et al. Low intensity ultrasound perturbs cytoskeleton dynamics. Soft Matter 8, 2438–2443 (2012).
Blackmore, J., Shrivastava, S., Sallet, J., Butler, C. R. & Cleveland, R. O. Ultrasound neuromodulation: a review of results, mechanisms and safety. Ultrasound Med. Biol. 45, 1509–1536 (2019).
Jerusalem, A. et al. Electrophysiological–mechanical coupling in the neuronal membrane and its role in ultrasound neuromodulation and general anaesthesia. Acta Biomater. 97, 116–140 (2019).
Kamimura, H. A. S., Conti, A., Toschi, N. & Konofagou, E. E. Ultrasound neuromodulation: mechanisms and the potential of multimodal stimulation for neuronal function assessment. Front. Phys. 8, 150 (2020).
Rabut, C. et al. Ultrasound technologies for imaging and modulating neural activity. Neuron 108, 93–110 (2020).
Imashiro, C. et al. Travelling ultrasound promotes vasculogenesis of three‐dimensional‐monocultured human umbilical vein endothelial cells. Biotechnol. Bioeng. 118, 3760–3769 (2021).
Bashardoust Tajali, S., Houghton, P., MacDermid, J. C. & Grewal, R. Effects of low-intensity pulsed ultrasound therapy on fracture healing: a systematic review and meta-analysis. Am. J. Phys. Med. Rehabil. 91, 349–367 (2012).
Zhou, X. et al. Improved human bone marrow mesenchymal stem cell osteogenesis in 3D bioprinted tissue scaffolds with low intensity pulsed ultrasound stimulation. Sci. Rep. 6, 32876 (2016).
Palanisamy, P., Alam, M., Li, S., Chow, S. K. H. & Zheng, Y. Low‐intensity pulsed ultrasound stimulation for bone fractures healing: a review. J. Ultrasound Med. 41, 547–563 (2022).
Ikeda, K. et al. Effects of low-intensity pulsed ultrasound on the differentiation of C2C12 cells. Life Sci. 79, 1936–1943 (2006).
Lai, C.-H. et al. Effects of low-intensity pulsed ultrasound, dexamethasone/TGF-β1 and/or BMP-2 on the transcriptional expression of genes in human mesenchymal stem cells: chondrogenic vs. osteogenic differentiation. Ultrasound Med. Biol. 36, 1022–1033 (2010).
Ambattu, L. A., Gelmi, A. & Yeo, L. Y. Short‐duration high frequency megahertz‐order nanomechanostimulation drives early and persistent osteogenic differentiation in mesenchymal stem cells. Small 18, 2106823 (2022).
Duque, M. et al. Sonogenetic control of mammalian cells using exogenous transient receptor potential A1 channels. Nat. Commun. 13, 600 (2022).
Yoo, S., Mittelstein, D. R., Hurt, R. C., Lacroix, J. & Shapiro, M. G. Focused ultrasound excites cortical neurons via mechanosensitive calcium accumulation and ion channel amplification. Nat. Commun. 13, 493 (2022).
Collins, M. N. & Mesce, K. A. A review of the bioeffects of low-intensity focused ultrasound and the benefits of a cellular approach. Front. Physiol. 13, 1047324 (2022).
Zhang, M. et al. Cell mechanical responses to subcellular perturbations generated by ultrasound and targeted microbubbles. Acta Biomater. 155, 471–481 (2023).
Riehl, B. D., Park, J.-H., Kwon, I. K. & Lim, J. Y. Mechanical stretching for tissue engineering: two-dimensional and three-dimensional constructs. Tissue Eng. Part B 18, 288–300 (2012).
Brown, T. D. Techniques for mechanical stimulation of cells in vitro: a review. J. Biomech. 33, 3–14 (2000).
Terraciano, V. et al. Differential response of adult and embryonic mesenchymal progenitor cells to mechanical compression in hydrogels. Stem Cell 25, 2730–2738 (2007).
Datta, N. et al. In vitro generated extracellular matrix and fluid shear stress synergistically enhance 3D osteoblastic differentiation. Proc. Natl Acad. Sci. USA 103, 2488–2493 (2006).
Kapur, S., Baylink, D. J. & William Lau, K.-H. Fluid flow shear stress stimulates human osteoblast proliferation and differentiation through multiple interacting and competing signal transduction pathways. Bone 32, 241–251 (2003).
Ozcelik, A. et al. Acoustofluidic rotational manipulation of cells and organisms using oscillating solid structures. Small 12, 5120–5125 (2016).
Ahmed, D. et al. Rotational manipulation of single cells and organisms using acoustic waves. Nat. Commun. 7, 11085 (2016).
Coussios, C. C. & Roy, R. A. Applications of acoustics and cavitation to noninvasive therapy and drug delivery. Annu. Rev. Fluid Mech. 40, 395–420 (2008).
Shiraishi, K. et al. Biophysical forces mediated by respiration maintain lung alveolar epithelial cell fate. Cell 186, 1478–1492.e15 (2023).
Nitsan, I., Drori, S., Lewis, Y. E., Cohen, S. & Tzlil, S. Mechanical communication in cardiac cell synchronized beating. Nat. Phys. 12, 472–477 (2016).
Mishra, P., Hill, M. & Glynne-Jones, P. Deformation of red blood cells using acoustic radiation forces. Biomicrofluidics 8, 034109 (2014).
Bezer, J. H., Koruk, H., Rowlands, C. J. & Choi, J. J. Elastic deformation of soft tissue-mimicking materials using a single microbubble and acoustic radiation force. Ultrasound Med. Biol. 46, 3327–3338 (2020).
Zhang, Y. & Habibovic, P. Delivering mechanical stimulation to cells: state of the art in materials and devices design. Adv. Mater. 34, 2110267 (2022).
Cafarelli, A. et al. Piezoelectric nanomaterials activated by ultrasound: the pathway from discovery to future clinical adoption. ACS Nano 15, 11066–11086 (2021).
Yildiz, D., Göstl, R. & Herrmann, A. Sonopharmacology: controlling pharmacotherapy and diagnosis by ultrasound-induced polymer mechanochemistry. Chem. Sci. 13, 13708–13719 (2022).
Mitragotri, S. Healing sound: the use of ultrasound in drug delivery and other therapeutic applications. Nat. Rev. Drug Discov. 4, 255–260 (2005).
Rich, J., Tian, Z. & Huang, T. J. Sonoporation: past, present, and future. Adv. Mater. Technol. 7, 2100885 (2022).
Yu, H. & Xu, L. Cell experimental studies on sonoporation: state of the art and remaining problems. J. Control. Rel. 174, 151–160 (2014).
Aryal, M., Arvanitis, C. D., Alexander, P. M. & McDannold, N. Ultrasound-mediated blood–brain barrier disruption for targeted drug delivery in the central nervous system. Adv. Drug Deliv. Rev. 72, 94–109 (2014).
Fletcher, S.-M. P., Choi, M., Ogrodnik, N. & O’Reilly, M. A. A porcine model of transvertebral ultrasound and microbubble-mediated blood-spinal cord barrier opening. Theranostics 10, 7758–7774 (2020).
Bleker, S. et al. Modulation of the blood–retina-barrier permeability by focused ultrasound: computational and experimental approaches. J. Acoust. Soc. Am. 153, A68 (2023).
Oberli, M. A., Schoellhammer, C. M., Langer, R. & Blankschtein, D. Ultrasound-enhanced transdermal delivery: recent advances and future challenges. Ther. Deliv. 5, 843–857 (2014).
Lentacker, I., De Cock, I., Deckers, R., De Smedt, S. C. & Moonen, C. T. W. Understanding ultrasound induced sonoporation: definitions and underlying mechanisms. Adv. Drug Deliv. Rev. 72, 49–64 (2014).
Son, S. et al. Multifunctional sonosensitizers in sonodynamic cancer therapy. Chem. Soc. Rev. 49, 3244–3261 (2020).
Crum, L., Bailey, M., Hwang, J. H., Khokhlova, V. & Sapozhnikov, O. Therapeutic ultrasound: recent trends and future perspectives. Phys. Procedia 3, 25–34 (2010).
Yang, Y. et al. Sonothermogenetics for noninvasive and cell-type specific deep brain neuromodulation. Brain Stimul. 14, 790–800 (2021).
Shapiro, M. G. et al. Biogenic gas nanostructures as ultrasonic molecular reporters. Nat. Nanotechnol. 9, 311–316 (2014).
Lakshmanan, A. et al. Acoustic biosensors for ultrasound imaging of enzyme activity. Nat. Chem. Biol. 16, 988–996 (2020).
Ibsen, S., Tong, A., Schutt, C., Esener, S. & Chalasani, S. H. Sonogenetics is a non-invasive approach to activating neurons in Caenorhabditis elegans. Nat. Commun. 6, 8264 (2015).
Leskinen, J. J. & Hynynen, K. Study of factors affecting the magnitude and nature of ultrasound exposure with in vitro set-ups. Ultrasound Med. Biol. 38, 777–794 (2012).
Snehota, M., Vachutka, J., Ter Haar, G., Dolezal, L. & Kolarova, H. Therapeutic ultrasound experiments in vitro: review of factors influencing outcomes and reproducibility. Ultrasonics 107, 106167 (2020).
Izadifar, Z., Izadifar, Z., Chapman, D. & Babyn, P. An introduction to high intensity focused ultrasound: systematic review on principles, devices, and clinical applications. J. Clin. Med. 9, 460 (2020).
Miller, D. L. et al. Overview of therapeutic ultrasound applications and safety considerations. J. Ultrasound Med. 31, 623–634 (2012).
Qiu, Y. et al. Acoustic devices for particle and cell manipulation and sensing. Sensors 14, 14806–14838 (2014).
Jin, Y. et al. Magnetic control of axon navigation in reprogrammed neurons. Nano Lett. 19, 6517–6523 (2019).
Yun, S. et al. Design of magnetically labeled cells (mag-cells) for in vivo control of stem cell migration and differentiation. Nano Lett. 18, 838–845 (2018).
Kappes, M. et al. Superparamagnetic iron oxide nanoparticles for targeted cell seeding: magnetic patterning and magnetic 3D cell culture. Adv. Funct. Mater. 32, 2203672 (2022).
Bratt-Leal, A. M., Kepple, K. L., Carpenedo, R. L., Cooke, M. T. & McDevitt, T. C. Magnetic manipulation and spatial patterning of multi-cellular stem cell aggregates. Integr. Biol. 3, 1224–1232 (2011).
Rangarajan, S., Madden, L. & Bursac, N. Use of flow, electrical, and mechanical stimulation to promote engineering of striated muscles. Ann. Biomed. Eng. 42, 1391–1405 (2014).
Borchers, S., Himmelbach, M., Logothetis, N. & Karnath, H.-O. Direct electrical stimulation of human cortex — the gold standard for mapping brain functions? Nat. Rev. Neurosci. 13, 63–70 (2012).
Jimenez-Gambin, S., Jimenez, N., Benlloch, J. M. & Camarena, F. Holograms to focus arbitrary ultrasonic fields through the skull. Phys. Rev. Appl. 12, 014106 (2019).
Karatum, O., Han, M., Erdogan, E. T., Karamursel, S. & Nizamoglu, S. Physical mechanisms of emerging neuromodulation modalities. J. Neural Eng. 20, 031001 (2023).
Parfenov, V. A. et al. Biofabrication of a functional tubular construct from tissue spheroids using magnetoacoustic levitational directed assembly. Adv. Healthc. Mater. 9, 2000721 (2020).
Leighton, T. G. What is ultrasound? Prog. Biophys. Mol. Biol. 93, 3–83 (2007).
Bertin, N. et al. Bubble-based acoustic micropropulsors: active surfaces and mixers. Lab Chip 17, 1515–1528 (2017).
Wiklund, M., Green, R. & Ohlin, M. Acoustofluidics 14: applications of acoustic streaming in microfluidic devices. Lab Chip 12, 2438 (2012).
Salari, A. et al. Dancing with the cells: acoustic microflows generated by oscillating cells. Small 16, 1903788 (2020).
Rasouli, R., Villegas, K. M. & Tabrizian, M. Acoustofluidics — changing paradigm in tissue engineering, therapeutics development, and biosensing. Lab Chip 23, 1300–1338 (2023).
Friend, J. & Yeo, L. Y. Microscale acoustofluidics: microfluidics driven via acoustics and ultrasonics. Rev. Mod. Phys. 83, 647–704 (2011).
Drinkwater, B. W. Dynamic-field devices for the ultrasonic manipulation of microparticles. Lab Chip 16, 2360–2375 (2016).
Kinsler, L. E. et al. (eds) Fundamentals of Acoustics 149–170 (Wiley, 2000).
Kinsler, L. E. et al. (eds) Fundamentals of Acoustics 210–245 (Wiley, 2000).
Blaeser, A. et al. Controlling shear stress in 3D bioprinting is a key factor to balance printing resolution and stem cell integrity. Adv. Healthc. Mater. 5, 326–333 (2016).
Miri, A. K. et al. Effective bioprinting resolution in tissue model fabrication. Lab Chip 19, 2019–2037 (2019).
Adhikari, J. et al. Effects of processing parameters of 3D bioprinting on the cellular activity of bioinks. Macromol. Biosci. 21, 2000179 (2021).
Madrid-Wolff, J., Boniface, A., Loterie, D., Delrot, P. & Moser, C. Controlling light in scattering materials for volumetric additive manufacturing. Adv. Sci. 9, 2105144 (2022).
Gudapati, H., Dey, M. & Ozbolat, I. A comprehensive review on droplet-based bioprinting: past, present and future. Biomaterials 102, 20–42 (2016).
Li, X. et al. Inkjet bioprinting of biomaterials. Chem. Rev. 120, 10793–10833 (2020).
Duck, F. A. Medical and non-medical protection standards for ultrasound and infrasound. Prog. Biophys. Mol. Biol. 93, 176–191 (2007).
Baker, K. G., Robertson, V. J. & Duck, F. A. A review of therapeutic ultrasound: biophysical effects. Phys. Ther. 81, 1351–1358 (2001).
FDA. Marketing clearance of diagnostic ultrasound systems and transducers. U.S. Food and Drug Administration https://www.fda.gov/media/71100/download (2019).
Apfel, R. E. & Holland, C. K. Gauging the likelihood of cavitation from short-pulse, low-duty cycle diagnostic ultrasound. Ultrasound Med. Biol. 17, 179–185 (1991).
Hariharan, P., Myers, M. R. & Banerjee, R. K. HIFU procedures at moderate intensities — effect of large blood vessels. Phys. Med. Biol. 52, 3493–3513 (2007).
Ter Haar, G. et al. Guidance on reporting ultrasound exposure conditions for bio-effects studies. Ultrasound Med. Biol. 37, 177–183 (2011).
Preston, R. C. & Shaw, A. Recommended Ultrasound Field Safety Classification for Medical Diagnostic Devices. Measurement Good Practice Guide, 50. National Physical Laboratory https://eprintspublications.npl.co.uk/2113/ (2001).
Fontana, F. et al. Development and validation of low-intensity pulsed ultrasound systems for highly controlled in vitro cell stimulation. Ultrasonics 116, 106495 (2021).
Acknowledgements
The research was in part supported by the European Research Council under the ERC Advanced Grant Agreement HOLOMAN (no. 788296); and the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) under Germany’s Excellence Strategy through the Excellence Cluster 3D Matter Made to Order (EXC-2082/1-390761711) and the Carl-Zeiss-Stiftung (P2022-04-073).
Author information
Authors and Affiliations
Contributions
All authors contributed to the writing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
K.M. and P.F. are inventors on a patent related to this work granted by the European Patent Office (EP3034281 B1). K.M. and P.F. declare no other competing interests. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Bioengineering thanks Tony Huang, Feng Guo and Martin Wiklund for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Melde, K., Athanassiadis, A.G., Missirlis, D. et al. Ultrasound-assisted tissue engineering. Nat Rev Bioeng (2024). https://doi.org/10.1038/s44222-024-00166-5
Accepted:
Published:
DOI: https://doi.org/10.1038/s44222-024-00166-5