Abstract
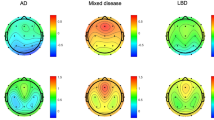
Cognitive decline and hallucinations are common and debilitating non-motor symptoms, usually occurring during later phases of Parkinson’s disease (PD). Minor hallucinations (MH) appear early in the disease course and have been suggested to predict cognitive impairment and decline in PD, however, this has not been well-established by clinical research. Here, we investigated whether, in the absence of dementia, patients with PD and MH (without differences in frontal–subcortical and posterior cognitive functions) show altered brain oscillations and whether such MH-related electrophysiological changes are associated with cognitive impairments that increase over time. Combining model-driven electroencephalography analysis with neuropsychiatric and neuropsychological examinations in 75 patients with PD, we reveal enhanced frontal theta oscillations in patients with PD suffering from MH and link these oscillatory changes with lower cognitive frontal–subcortical functions. Neuropsychological follow-up examinations five years later revealed a stronger decline in frontal–subcortical functions in patients with MH, anticipated by stronger frontal theta alterations measured during the first assessment, defining an MH- and theta-oscillation-based early marker of a cognitive decline in PD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data are available here: https://gitlab.epfl.ch/fbernasc/pd_mh_eeg_cognition.git.
Code availability
Codes for the analyses are available here: https://gitlab.epfl.ch/fbernasc/pd_mh_eeg_cognition.git.
References
Kalia, L. V. & Lang, A. E. Parkinson’s disease. Lancet 386, 896–912 (2015).
Dorsey, E. R. et al. Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17, 939–953 (2018).
Postuma, R. B. & Berg, D. Advances in markers of prodromal Parkinson disease. Nat. Rev. Neurol. 12, 622–634 (2016).
Fénelon, G., Soulas, T., Zenasni, F. & De Langavant, L. C. The changing face of Parkinson’s disease-associated psychosis: a cross-sectional study based on the new NINDS-NIMH criteria. Mov. Disord. 25, 755–759 (2010).
Lenka, A., Pagonabarraga, J., Pal, P. K., Bejr-Kasem, H. & Kulisvesky, J. Minor hallucinations in Parkinson disease: A subtle symptom with major clinical implications. Neurology https://doi.org/10.1212/WNL.0000000000007913 (2019).
Ffytche, D. H. et al. The psychosis spectrum in Parkinson disease. Nat. Rev. Neurol. 13, 81–95 (2017).
Aarsland, D. et al. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 7, 47 (2021).
Levin, J., Hasan, A. & Höglinger, G. U. Psychosis in Parkinson’s disease: identification, prevention and treatment. J. Neural Transm. 123, 45–50 (2016).
Diederich, N. J., Fénelon, G., Stebbins, G. & Goetz, C. G. Hallucinations in Parkinson disease. Nat. Rev. Neurol. 5, 331–342 (2009).
Forsaa, E. B., Larsen, J. P., Wentzel-Larsen, T. & Alves, G. What predicts mortality in Parkinson disease?: a prospective population-based long-term study. Neurology 75, 1270–1276 (2010).
Marinus, J., Zhu, K., Marras, C., Aarsland, D. & van Hilten, J. J. Risk factors for non-motor symptoms in Parkinson’s disease. Lancet Neurol. 17, 559–568 (2018).
Aarsland, D., Hutchinson, M. & Larsen, J. P. Cognitive, psychiatric and motor response to galantamine in Parkinson’s disease with dementia. Int. J. Geriatr. Psychiatry 18, 937–941 (2003).
Galvin, J. E., Pollack, J. & Morris, J. C. Clinical phenotype of Parkinson disease dementia. Neurology 67, 1605–1611 (2006).
Uc, E. Y. et al. Incidence of and risk factors for cognitive impairment in an early Parkinson disease clinical trial cohort. Neurology 73, 1469–1477 (2009).
Anang, J. B. M. et al. Predictors of dementia in Parkinson disease: a prospective cohort study. Neurology 83, 1253–1260 (2014).
Goetz, C. G., Emre, M. & Dubois, B. Parkinson’s disease dementia: definitions, guidelines, and research perspectives in diagnosis. Ann. Neurol. 64(Suppl 2), S81–S92 (2008).
Aarsland, D., Larsen, J. P., Tandberg, E. & Laake, K. Predictors of nursing home placement in Parkinson’s disease: a population-based, prospective study. J. Am. Geriatr. Soc. 48, 938–942 (2000).
Gonzalez, M. C., Dalen, I., Maple-Grødem, J., Tysnes, O.-B. & Alves, G. Parkinson’s disease clinical milestones and mortality. NPJ Parkinsons Dis. 8, 1–5 (2022).
Collerton, D., Perry, E. & McKeith, I. Why people see things that are not there: a novel perception and attention deficit model for recurrent complex visual hallucinations. Behav. Brain Sci. 28, 737–757 (2005).
Goldman, J. G. et al. Visuoperceptive region atrophy independent of cognitive status in patients with Parkinson’s disease with hallucinations. Brain J. Neurol. 137, 849–859 (2014).
Hobson, J. A., Pace-Schott, E. F. & Stickgold, R. Dreaming and the brain: toward a cognitive neuroscience of conscious states. Behav. Brain Sci. 23, 793–842 (2000).
Ibarretxe-Bilbao, N. et al. Differential progression of brain atrophy in Parkinson’s disease with and without visual hallucinations. J. Neurol. Neurosurg. Psychiatry 81, 650–657 (2010).
Shine, J. M., Halliday, G. M., Naismith, S. L. & Lewis, S. J. G. Visual misperceptions and hallucinations in Parkinson’s disease: dysfunction of attentional control networks? Mov. Disord. 26, 2154–2159 (2011).
Watanabe, H. et al. Cortical and subcortical brain atrophy in Parkinson’s disease with visual hallucination. Mov. Disord. 28, 1732–1736 (2013).
Ramirez-Ruiz, B., Junque, C., Marti, M.-J., Valldeoriola, F. & Tolosa, E. Cognitive changes in Parkinson’s disease patients with visual hallucinations. Dement. Geriatr. Cogn. Disord. 23, 281–288 (2007).
Obeso, J. A., Rodriguez-Oroz, M. C., Stamelou, M., Bhatia, K. P. & Burn, D. J. The expanding universe of disorders of the basal ganglia. Lancet 384, 523–531 (2014).
Shine, J. M. et al. The role of dysfunctional attentional control networks in visual misperceptions in Parkinson’s disease. Hum. Brain Mapp. 35, 2206–2219 (2014).
Fénelon, G., Mahieux, F., Huon, R. & Ziégler, M. Hallucinations in Parkinson’s disease: prevalence, phenomenology and risk factors. Brain J. Neurol. 123, 733–745 (2000).
Ravina, B. et al. Diagnostic criteria for psychosis in Parkinson’s disease: report of an NINDS, NIMH work group. Mov. Disord. Off. 22, 1061–1068 (2007).
Pagonabarraga, J. et al. Neural correlates of minor hallucinations in non-demented patients with Parkinson’s disease. Parkinsonism Relat. Disord. 20, 290–296 (2014).
Bernasconi, F. et al. Robot-induced hallucinations in Parkinson’s disease depend on altered sensorimotor processing in fronto-temporal network. Sci. Transl. Med. 13, eabc8362 (2021).
Bejr-Kasem, H. et al. Disruption of the default mode network and its intrinsic functional connectivity underlies minor hallucinations in Parkinson’s disease. Mov. Disord. Off. 34, 78–86 (2019).
Bejr-Kasem, H. et al. Minor hallucinations reflect early gray matter loss and predict subjective cognitive decline in Parkinson’s disease. Eur. J. Neurol. 28, 438–447 (2021).
Llebaria, G. et al. Neuropsychological correlates of mild to severe hallucinations in Parkinson’s disease. Mov. Disord. 25, 2785–2791 (2010).
Bosboom, J. L. W. et al. Resting state oscillatory brain dynamics in Parkinson’s disease: an MEG study. Clin. Neurophysiol. 117, 2521–2531 (2006).
Geraedts, V. J. et al. Clinical correlates of quantitative EEG in Parkinson disease: a systematic review. Neurology 91, 871–883 (2018).
Hassan, M. et al. Functional connectivity disruptions correlate with cognitive phenotypes in Parkinson’s disease. Neuroimage Clin. 14, 591–601 (2017).
Olde Dubbelink, K. T. E. et al. Cognitive decline in Parkinson’s disease is associated with slowing of resting-state brain activity: a longitudinal study. Neurobiol. Aging 34, 408–418 (2013).
Hinrichs, H. et al. Comparison between a wireless dry electrode EEG system with a conventional wired wet electrode EEG system for clinical applications. Sci. Rep. 10, 5218 (2020).
Hirschmann, J. et al. Distinct oscillatory STN-cortical loops revealed by simultaneous MEG and local field potential recordings in patients with Parkinson’s disease. Neuroimage 55, 1159–1168 (2011).
Hirschmann, J. et al. A direct relationship between oscillatory subthalamic nucleus-cortex coupling and rest tremor in Parkinson’s disease. Brain J. Neurol. 136, 3659–3670 (2013).
Kühn, A. A. et al. Pathological synchronisation in the subthalamic nucleus of patients with Parkinson’s disease relates to both bradykinesia and rigidity. Exp. Neurol. 215, 380–387 (2009).
Oswal, A. et al. Deep brain stimulation modulates synchrony within spatially and spectrally distinct resting state networks in Parkinson’s disease. Brain J. Neurol. 139, 1482–1496 (2016).
Tinkhauser, G. et al. The modulatory effect of adaptive deep brain stimulation on beta bursts in Parkinson’s disease. Brain J. Neurol. 140, 1053–1067 (2017).
Babiloni, C. et al. Abnormal cortical neural synchronization mechanisms in quiet wakefulness are related to motor deficits, cognitive symptoms, and visual hallucinations in Parkinson’s disease patients: an electroencephalographic study. Neurobiol. Aging 91, 88–111 (2020).
Bonanni, L. et al. EEG comparisons in early Alzheimer’s disease, dementia with Lewy bodies and Parkinson’s disease with dementia patients with a 2-year follow-up. Brain J. Neurol. 131, 690–705 (2008).
Donoghue, T. et al. Parameterizing neural power spectra into periodic and aperiodic components. Nat. Neurosci. 23, 1655–1665 (2020).
Goetz, C. G. et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170 (2008).
Pagonabarraga, J. et al. Minor hallucinations occur in drug-naive Parkinson’s disease patients, even from the premotor phase. Mov. Disord. 31, 45–52 (2016).
Fénelon, G., Soulas, T., Langavant, L. C., de, Trinkler, I. & Bachoud-Lévi, A.-C. Feeling of presence in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 82, 1219–1224 (2011).
Wood, R. A., Hopkins, S. A., Moodley, K. K. & Chan, D. Fifty percent prevalence of extracampine hallucinations in Parkinson’s disease patients. Front. Neurol. 6, 263 (2015).
Kataoka, H. & Ueno, S. Predictable risk factors for the feeling of presence in patients with Parkinson’s disease. Mov. Disord. Clin. Pract. 2, 407–412 (2015).
Stern, A. F. The Hospital Anxiety and Depression Scale. Occup. Med. 64, 393–394 (2014).
Starkstein, S. E. et al. Reliability, validity, and clinical correlates of apathy in Parkinson’s disease. J. Neuropsychiatry Clin. Neurosci. 4, 134–139 (1992).
Lenka, A., Hegde, S., Jhunjhunwala, K. R. & Pal, P. K. Interactions of visual hallucinations, rapid eye movement sleep behavior disorder and cognitive impairment in Parkinson’s disease: A review. Parkinsonism Relat. Disord. 22, 1–8 (2016).
Sasai, T., Matsuura, M. & Inoue, Y. Electroencephalographic findings related with mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorder. Sleep 36, 1893–1899 (2013).
Postuma, R. B. et al. A single-question screen for REMsleep behavior disorder: a multicenter validation study. Mov. Disord. 27, 913–916 (2012).
Stiasny-Kolster, K. et al. The REM sleep behavior disorder screening questionnaire–a new diagnostic instrument. Mov. Disord. 22, 2386–2393 (2007).
Fernández de Bobadilla, R. et al. Parkinson’s disease-cognitive rating scale: psychometrics for mild cognitive impairment. Mov. Disord. 28, 1376–1383 (2013).
Asch, N. et al. Independently together: subthalamic theta and beta opposite roles in predicting Parkinson’s tremor. Brain Commun. 2, fcaa074 (2020).
Beudel, M. et al. Oscillatory beta power correlates with akinesia-rigidity in the Parkinsonian subthalamic nucleus. Mov. Disord. 32, 174–175 (2017).
Burn, D. J. et al. Motor subtype and cognitive decline in Parkinson’s disease, Parkinson’s disease with dementia, and dementia with Lewy bodies. J. Neurol. Neurosurg. Psychiatry 77, 585–589 (2006).
Alonso-Frech, F. et al. Slow oscillatory activity and levodopa-induced dyskinesias in Parkinson’s disease. Brain J. Neurol. 129, 1748–1757 (2006).
Rodriguez-Oroz, M. C. et al. Initial clinical manifestations of Parkinson’s disease: features and pathophysiological mechanisms. Lancet Neurol. 8, 1128–1139 (2009).
He, W. et al. Co-increasing neuronal noise and beta power in the developing brain. Preprint at bioRxiv https://doi.org/10.1101/839258 (2019).
Tran, T. T., Rolle, C. E., Gazzaley, A. & Voytek, B. Linked sources of neural noise contribute to age-related cognitive decline. J. Cogn. Neurosci. 32, 1813–1822 (2020).
Voytek, B. et al. Age-related changes in 1/f neural electrophysiological noise. J. Neurosci. 35, 13257–13265 (2015).
Whitford, T. J. et al. Brain maturation in adolescence: concurrent changes in neuroanatomy and neurophysiology. Hum. Brain Mapp. 28, 228–237 (2007).
Cellier, D., Riddle, J., Petersen, I. & Hwang, K. The development of theta and alpha neural oscillations from ages 3 to 24 years. Dev. Cogn. Neurosci. 50, 100969 (2021).
Galtier, I., Nieto, A., Lorenzo, J. N. & Barroso, J. Subjective cognitive decline and progression to dementia in Parkinson’s disease: a long-term follow-up study. J. Neurol. 266, 745–754 (2019).
Chandler, J. M. et al. Characteristics of Parkinson’s disease in patients with and without cognitive impairment. J. Parkinsons Dis. 11, 1381–1392 (2021).
Leroi, I., McDonald, K., Pantula, H. & Harbishettar, V. Cognitive impairment in Parkinson disease: impact on quality of life, disability, and caregiver burden. J. Geriatr. Psychiatry Neurol. 25, 208–214 (2012).
Aarsland, D. et al. Risk of dementia in Parkinson’s disease: a community-based, prospective study. Neurology 56, 730–736 (2001).
Walker, Z., Possin, K. L., Boeve, B. F. & Aarsland, D. Lewy body dementias. Lancet 386, 1683–1697 (2015).
Morita, A., Kamei, S. & Mizutani, T. Relationship between slowing of the EEG and cognitive impairment in Parkinson disease. J. Clin. Neurophysiol. 28, 384–387 (2011).
Soikkeli, R., Partanen, J., Soininen, H., Pääkkönen, A. & Riekkinen, P. Slowing of EEG in Parkinson’s disease. Electroencephalogr. Clin. Neurophysiol. 79, 159–165 (1991).
Stoffers, D. et al. Slowing of oscillatory brain activity is a stable characteristic of Parkinson’s disease without dementia. Brain 130, 1847–1860 (2007).
Wiesman, A. I. et al. A sagittal gradient of pathological and compensatory effects of neurophysiological slowing in Parkinson’s disease. 2022.08.05.22278436 Preprint at medRxiv https://doi.org/10.1101/2022.08.05.22278436 (2022).
Buckner, R. L. Memory and executive function in aging and AD: multiple factors that cause decline and reserve factors that compensate. Neuron 44, 195–208 (2004).
Steriade, M., Datta, S., Paré, D., Oakson, G. & Curró Dossi, R. C. Neuronal activities in brain-stem cholinergic nuclei related to tonic activation processes in thalamocortical systems. J. Neurosci. 10, 2541–2559 (1990).
Jensen, O., Gelfand, J., Kounios, J. & Lisman, J. E. Oscillations in the alpha band (9-12 Hz) increase with memory load during retention in a short-term memory task. Cereb. Cortex 12, 877–882 (2002).
Raghavachari, S. et al. Gating of human theta oscillations by a working memory task. J. Neurosci. 21, 3175–3183 (2001).
Makeig, S., Debener, S., Onton, J. & Delorme, A. Mining event-related brain dynamics. Trends Cogn. Sci. 8, 204–210 (2004).
Dhanis, H. et al. Robotically-induced hallucination triggers subtle changes in brain network transitions. NeuroImage 248, 118862 (2021).
Chung, S. J. et al. Frontal atrophy as a marker for dementia conversion in Parkinson’s disease with mild cognitive impairment. Hum. Brain Mapp. 40, 3784–3794 (2019).
Chung, S. J. et al. Factor analysis-derived cognitive profile predicting early dementia conversion in PD. Neurology 95, e1650–e1659 (2020).
Lee, J. E. et al. Exploratory analysis of neuropsychological and neuroanatomical correlates of progressive mild cognitive impairment in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 85, 7–16 (2014).
Pagonabarraga, J. et al. Parkinson’s disease-cognitive rating scale: a new cognitive scale specific for Parkinson’s disease. Mov. Disord. 23, 998–1005 (2008).
Williams-Gray, C. H., Foltynie, T., Brayne, C. E. G., Robbins, T. W. & Barker, R. A. Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain J. Neurol. 130, 1787–1798 (2007).
Goetz, C. G. et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov. Disord. 19, 1020–1028 (2004).
Klassen, B. T. et al. Quantitative EEG as a predictive biomarker for Parkinson disease dementia. Neurology 77, 118–124 (2011).
Cozac, V. V. et al. Increase of EEG spectral theta power indicates higher risk of the development of severe cognitive decline in Parkinson’s disease after 3 years. Front. Aging Neurosci. 8, 284 (2016).
Bejr-Kasem, H. et al. The role of attentional control over interference in minor hallucinations in Parkinson’s disease. Parkinsonism Relat. Disord. 102, 101–107 (2022).
Bernasconi, F. et al. Neuroscience robotics for controlled induction and real-time assessment of hallucinations. Nat. Protoc. 17, 2966–2989 (2022).
Delorme, A. & Makeig, S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods 134, 9–21 (2004).
Chaumon, M., Bishop, D. V. M. & Busch, N. A. A practical guide to the selection of independent components of the electroencephalogram for artifact correction. J. Neurosci. Methods 250, 47–63 (2015).
Bédard, C., Kröger, H. & Destexhe, A. Does the 1/f frequency scaling of brain signals reflect self-organized critical states? Phys. Rev. Lett. 97, 118102 (2006).
Chiang, A. K. I., Rennie, C. J., Robinson, P. A., van Albada, S. J. & Kerr, C. C. Age trends and sex differences of alpha rhythms including split alpha peaks. Clin. Neurophysiol. 122, 1505–1517 (2011).
Dickson, D. W., Uchikado, H., Fujishiro, H. & Tsuboi, Y. Evidence in favor of Braak staging of Parkinson’s disease. Mov. Disord. 25(Suppl 1), S78–S82 (2010).
Ushey, K., Allaire, J. & Tang, Y. reticulate: interface to Python. R package v.1.16 (2020).
Ostlund, B. et al. Spectral parameterization for studying neurodevelopment: How and why. Dev. Cogn. Neurosci. 54, 101073 (2022).
Frossard, J. & Renaud, O. Permutation tests for regression, ANOVA, and comparison of signals: the permuco package. J. Stat. Software 99, 1–32 (2021).
Benjamini, Y. & Yekutieli, D. The control of the false discovery rate in multiple testing under dependency. Ann. Stat. 29, 1165–1188 (2001).
Singmann, H. & Klauer, K. C. Deductive and inductive conditional inferences: two modes of reasoning. Think. Reason. 17, 247–281 (2011).
Lex, A., Gehlenborg, N., Strobelt, H., Vuillemot, R. & Pfister, H. UpSet: visualization of intersecting sets. IEEE Transactions on Visualization and Computer Graphics 20, 983–1992 (2014).
Acknowledgements
We thank all patients for their participation to the study. We thank Prof. Andrea Serino and Prof. Gilles Allali for their comments on earlier version of the manuscript. This research was supported by two donors advised by CARIGEST SA (Fondazione Teofilo Rossi di Montelera e di Premuda and a second one wishing to remain anonymous) to O.B.; National Center of Competence in Research (NCCR) ‘Synapsy—The Synaptic Bases of Mental Diseases’ grant number 51NF40-185897 to O.B.; Parkinson Suisse to O.B.; Bertarelli Foundation to O.B.; CIBERNED (Carlos III Institute) and FIS grant PI18/01717 to J.K.; Instituto de Salud Carlos III (ISCIII), Spain, to J.K.; PERIS, expedient number SLT008/18/00088 Generalitat de Catalunya to J. Pagonabarraga.
Author information
Authors and Affiliations
Contributions
F.B. conceptualized idea, analyzed the data and wrote paper, J.P., H.B-K, S.M-H collected data and wrote paper, J.K, O.B wrote paper. J.M. and A.H-B. collected data. All authors approved the definitive version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Abhishek Lenka, Leonidas Stefanis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary methods, results, Figs. 1–7 and Tables 1–8.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bernasconi, F., Pagonabarraga, J., Bejr-Kasem, H. et al. Theta oscillations and minor hallucinations in Parkinson’s disease reveal decrease in frontal lobe functions and later cognitive decline. Nat. Mental Health 1, 477–488 (2023). https://doi.org/10.1038/s44220-023-00080-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00080-6
This article is cited by
-
Numerosity estimation of virtual humans as a digital-robotic marker for hallucinations in Parkinson’s disease
Nature Communications (2024)
-
Minor hallucinations in early Parkinson’s disease: are they benign?
Nature Mental Health (2023)