Abstract
Previous studies suggested the role of cellular senescence in late-life depression (LLD). However, it is unclear how this finding relates to common features of LLD, such as medical and cognitive problems. We applied factor analyses to an extensive battery of clinical variables in 426 individuals with LLD. Here we tested the relationship between these factors, age and sex, with an index of cellular senescence based on 22 senescence-associated secretory phenotype proteins. We found four factors: ‘depression and anxiety severity’, ‘cognitive functioning’, ‘cardiovascular and cardiometabolic health’ and ‘blood pressure’. A higher senescence-associated secretory phenotype index was associated with poorer ‘cognitive functioning’ and ‘cardiovascular and cardiometabolic health’ but not with ‘depression and anxiety severity’. These findings highlight the role of cellular senescence in poorer physical and cognitive health in LLD. They are consonant with the viewpoint that co-occurring medical burdens and their associated disabilities are part of a phenotype of accelerated ageing in LLD.
Similar content being viewed by others
Main
Late-life depression (LLD) is a major depressive disorder in older adults. LLD is common and poses a substantial burden for affected individuals, their families and society1. These burdens include worse quality of life, impaired activities of daily living2 and increased frailty3. Previous studies demonstrated a strong link among LLD, poor physical health4, cognitive impairment, an increased risk for dementia and mortality5. These clinico-epidemiological findings suggest that older adults with LLD may experience an accelerated ageing phenotype6.
Accelerated ageing processes in LLD may be driven by increased allostatic load, altered proteostasis control, pro-inflammatory mechanisms and systemic oxidative stress7,8. Research also suggests that accelerated ageing in LLD may occur on the cellular and subcellular level9 and be linked to enhanced senescence processes10. Cellular senescence11 has emerged as a pivotal hallmark of the biology of ageing. It is a complex stress response in which cells irreversibly lose their proliferative capacity, become resistant to apoptosis12 and develop a multicomponent secretory phenotype13, referred to as the senescence-associated secretory phenotype (SASP)12. The SASP includes proteins involved in cycle control, intercellular communication, the immune-inflammatory response and tissue remodelling14. Under non-pathological conditions, SASP proteins are essential for embryonic development and tissue patterning throughout life15. However, the accumulation of senescent cells and the increased secretion of SASP proteins with age is linked to tissue deterioration and the emergence of physical disorders prevalent in older adults16. Human and animal studies found that the increased expression of SASP proteins drives multiple age-related phenotypes, such as atherosclerosis17, osteoarthritis18, cancer19, kidney dysfunction20 and a shortened health span21. In humans, an increase in SASP proteins is related to obesity, cardiometabolic dysregulation22 and frailty14. Several studies characterized the role of cellular senescence and SASP proteins in the brain. Aged microglia, astrocytes and neurons exhibit various features of senescence, including the expression of SASP proteins23,24,25. In Alzheimer’s disease, an upregulation of SASP proteins has been found in hippocampal neurons and astrocytes26.
These findings support that cellular senescence underlies body-wide accelerated ageing and that SASP proteins are markers for these processes. Since the SASP proteins reflect multiple interrelated biological functions, examining them as a biomarker-composite index (SASP index) might be more robust than investigating single proteins. While the SASP is cell dependent, there are common SASP proteins expressed by senescent cells. On the basis of these SASP markers27, our group developed a peripheral SASP index comprising 22 proteins. We validated the SASP index in several studies28,29 and consistently found a higher SASP index in individuals with LLD compared with healthy individuals28,30,31, suggesting that the SASP index might be a marker for accelerated ageing in LLD.
While these previous studies report an increase in the SASP index in LLD, it is unclear which clinical characteristics of LLD are linked to cellular senescence and the SASP index. We hypothesize that cognitive and physical health variables (for example, medical comorbidities and general physical health) are correlated with the increased SASP index and thus might drive accelerated ageing in LLD. Alternatively, psychopathology itself (for example, the severity of depression and psychiatric comorbidities) may drive the increased SASP. Testing this hypothesis may deepen our understanding of biological ageing abnormalities in LLD and help identify individuals who are particularly vulnerable to accelerated ageing and may benefit from targeted prevention and treatment strategies. In this Article, as a step towards this goal, we aimed to identify which clinical variables are related to the peripheral SASP index in LLD. We leveraged a relatively large LLD sample (n = 426) with SASP protein measurements. Following previous studies demonstrating the utility of integrating various variables32,33,34, we used factor analyses to group clinical variables. We then tested our hypothesis that the resulting clinical factors would be associated with the SASP index.
Results
Participants were recruited as part of a clinical trial (the Incomplete Response in Late-Life Depression: Getting to Remission (IRL-GREY) study) conducted between August 2009 and August 2014, as detailed previously35 (Supplementary Table 1). We included 426 participants, aged 60 years or older, with a diagnosis of current non-psychotic major depressive disorder and a score ≥15 on the Montgomery–Asberg Depression Rating Scale (MADRS)36. All participants included in this analysis had complete demographic and protein data. Their mean age ± standard deviation (s.d.) was 68.94 ± 7.10 years, and 64% were female. For demographic and clinical information, see Tables 1 and 2, and for medication information, see Supplementary Table 2.
Clinical variables
For an overview of our analytic strategy, see Fig. 1. We examined an extensive battery of clinical variables to characterize mental health, including MADRS36, Anxiety Sensitivity Index (ASI)37, Scale of Suicidal Ideation (SSI)38 and the Medical Outcomes Survey—mental39. To examine cognitive functioning, we recorded self-reported years of education, Mini-Mental Status Examination (MMSE)40, Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)41 and the Delis–Kaplan Executive Function System (DKEFS)42. Last, we obtained anthropometric data, blood pressure, fasting glucose levels, Cumulative Illness Rating Scale—geriatrics (CIRS-G)43 and the Medical Outcomes Survey—physical39.
First, we conducted three independent factor analyses to group clinical variables. Next, we calculated a regression to determine the effects of age and sex on the SASP index. We then utilized correlation and regression analyses to explore the association between the SASP index and the factors. Finally, we split the sample into participants with early-onset depression (age of onset before 65 years) or late-onset depression (age of onset at or after 65 years) and repeated the regression analyses for these two subgroups. References: MADRS36, ASI37, SSI38, Medical Outcomes Survey—mental39, MMSE40, RBANS41, DKEFS42, BMI, Medical Outcomes Survey—physical39 and SASP.
As presented in Supplementary Table 3, the factor analyses revealed one ‘depression and anxiety severity’ factor, one ‘cognitive functioning’ factor and two physical health-related factors. The first physical health-related factor is termed the ‘cardiovascular and cardiometabolic health’ factor. This explained the most variance and comprised body mass index (BMI), fasting glucose levels, CIRS-G and Medical Outcomes Survey—physical scales. The second physical health factor is termed ‘blood pressure’ because it comprises systolic and diastolic blood pressure.
Relationship between the SASP and demographic variables
On the basis of previous pre-clinical studies focused on the changes in the secretome pattern of senescent cells27 and our previous publications28,30, we determined 22 SASP proteins and calculated a SASP index. We conducted a regression analysis with the SASP index as the dependent variable and age and sex as independent variables (F(2, 423) = 21.31, P < 0.001, adjusted R2 = 0.087 and power >0.99). This demonstrated a significant effect of age (standardized β = 0.24, T = 5.24, P < 0.001 and variance inflation factor of 1.00) and sex (standardized β = −0.19, T = −4.11, P < 0.001 and variance inflation factor of 1.00) so that older and male participants presented with a higher SASP index (Supplementary Fig. 1).
Relationship between the SASP index and clinical variables
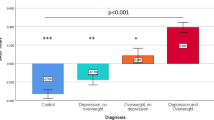
We used correlation and regression analyses to calculate the association between the SASP index and the factors determined above. A higher SASP index was correlated with worse cognitive functioning (r = −0.18, P < 0.001 and power 0.90) and worse cardiovascular and cardiometabolic health (r = 0.42, P < 0.001 and power >0.99) (Supplementary Table 4). Sex-specific correlations demonstrated a positive correlation between the SASP index and the cardiovascular and cardiometabolic health factor, both for males (r = 0.53, P < 0.001 and power >0.99) and females (r = 0.37, P < 0.001 and power >0.99), and a negative correlation between the SASP index and the cognitive functioning factor for females (r = −0.17, P = 0.005 and power 0.63).
As shown in Table 3, the linear regression analysis with the SASP index as the dependent variable and age, sex and the four factors as independent variables showed a significant effect of age (P < 0.001), sex (P < 0.001) and cardiovascular and cardiometabolic health (P < 0.001). Cardiovascular and cardiometabolic health was also the most significant independent variable when splitting our sample into males and females. This finding was supported when we repeated the regression analysis six times, excluding one of the covariates. As shown in Supplementary Table 6, the cardiovascular and cardiometabolic health factor contributed the most to the explained variance in the regression analysis. Including site as an additional covariate in the linear regression analysis did not significantly change the regression results (Supplementary Table 7).
Influence of age of onset
We conducted additional exploratory analyses to test the influence of age of onset on the relationship between the SASP index and demographic and clinical variables. We split the sample into participants with early-onset depression (n = 356) or late-onset depression (n = 69). The information was missing for one participant. As displayed in Table 4, results were qualitatively similar for early-onset versus late-onset depression.
Discussion
Previous work suggested a critical role of cellular senescence and an increased SASP index in LLD compared with non-depressed older adults28,30,44. The present study extended these findings by examining the variables related to the SASP index within individuals with LLD. Our results highlighted an association between an elevated SASP index and poor physical health. In addition, the SASP index was associated with age and sex, and cognitive functioning in females. In contrast, the SASP index was not associated with the severity of depression or anxiety (Fig. 2).
In individuals with LLD, the SASP index was most strongly associated with the cardiovascular and cardiometabolic health factor. Previous studies have demonstrated a robust bidirectional relationship between LLD and physical health6 and the mediating effect of medical conditions on treatment outcomes45. One previous study in young and middle-aged adults with major depressive disorder demonstrated that the SASP index was most strongly correlated to BMI31. In addition, pre-clinical studies have shown that fat cells express SASP proteins, which in turn cause a pro-oxidant, pro-inflammatory and pro-tumourigenic environment46. Obesity and diabetes mellitus have been linked to an increased expression of SASP proteins, and intervention studies have demonstrated that caloric restriction and exercise could delay cellular senescence and decrease SASP proteins47. Animal studies have shown that clearing senescent cells from obese mice restored neurogenesis, alleviating anxiety-related behaviour and chronic stress-induced cognitive decline48.
We observed a significant impact of age and biological sex on the SASP index. While cellular senescence occurs throughout life, senescent cells accumulate with age44 and contribute to tissue degradation. Therefore, our finding of a positive association between age and the SASP index is congruent with the description of biological senescence status as one of the hallmarks of ageing. While no studies have examined sex differences in SASP proteins, research on telomere length has reported sexual dimorphism49, and studies applying the allostatic load model to quantify physiological costs of stress found higher allostatic load in males than females50. In line with our findings, cardiovascular diseases develop later in females than males, and the association between LLD and increased mortality is particularly relevant for males51.
We found a significant but relatively weak correlation between the SASP index and cognitive functioning in females. Cognitive functioning—specifically executive functioning—has been identified as a predictor or moderator of treatment response in LLD52. In addition, one previous study on LLD reported a relationship between the SASP index and processing speed, executive functioning and general cognitive performance30. In another study, the SASP index was higher in individuals with comorbid LLD and mild cognitive impairments than in those with LLD without mild cognitive impairments28. These findings are expected, given the role of cellular senescence in brain functioning and neurological and neurodegenerative disorders53. While our sex-specific analyses must be interpreted with caution due to our larger number of female participants, they suggest that the association between the SASP index and cognition may be more robust in females.
Contrary to our hypothesis, the SASP index was not associated with the severity of depression or anxiety characteristics. When interpreting this finding, it is critical to note that it does not contradict our previous studies that have consistently demonstrated an increased SASP index in individuals with a major depressive disorder compared with non-depressed older adults28,30,31. However, it suggests that the SASP index is more closely associated with physical health and cognitive functioning than with the severity of depression and anxiety symptoms within individuals with LLD. The question of how depressive symptoms interact with the pathophysiology of major depression is fiercely discussed. For example, the severity and duration of depression are related to mortality54. Neuroimaging studies have reported a relationship between the age of onset and structural brain changes but not between symptom severity and structural abnormalities55. Some smaller studies examining telomere length have suggested a relationship between symptom severity and telomere length56, but other studies fail to report this association57 or only find it for younger adults. In one large longitudinal study of depressive symptoms, epigenetic changes and telomere length58, telomere length was shorter in individuals with depression. However, the authors did not find a relationship among changes in depressive symptoms, epigenetic markers or telomere length within an individual. They concluded that other features, such as inflammation, might drive the biological markers in depressed individuals. While this interpretation is also compelling for our findings, we acknowledge that differences in methods (for example, factor analyses versus single scores) might contribute to our findings. Additionally, previous studies suggested that other depression scales, such as the Geriatric Depression Scale or the Perceived Stress Scale, might be more sensitive to monitoring changes and treatment responses in LLD59. Therefore, longitudinal and more extensive studies are needed to explore the association between the SASP index and depression and anxiety characteristics within one individual.
Our findings highlight the interactive effect between LLD and physical burden. Previous research has demonstrated that depression frequently occurs in individuals with chronic illness and amplifies the disability and disablement associated with co-occurring physical illness and cognitive impairment60. In addition, depression undermines adherence to co-prescribed pharmacotherapy for medical diseases and reduces healthy lifestyle choices. Therefore, evidence-based treatment of depression may also reduce mortality risk secondary to physical illness, such as cancer61. On the other hand, co-occurring physical burden moderates the long-term response to antidepressant treatment and renders the individual’s response more brittle45. Last, the interaction of physical conditions and depression enhances the long-term risk for cognitive impairment and dementia. For these reasons, depression foreshortens life expectancy, while appropriate maintenance treatment may reduce mortality risk and increase life quality. Our findings suggest that future treatment efforts should include interventions and lifestyle modifications that target general health, such as weight loss and exercise programmes62, and optimized control of chronic medical conditions such as diabetes, hypertension and hypercholesterolaemia. Prescribed physical activity has been shown to prevent depression and has neuronal benefits63. In addition, geroscience-guided treatments that clear senescent cells or modify senescence and SASP-mediated pathways might provide promising avenues to improve LLD outcomes64. Future studies that examine the SASP longitudinally as a biomarker of ageing should examine if the SASP moderates long-term outcomes and if treatment of depression can modify the expression of SASP in a way that reduces the likelihood of physical and cognitive disabilities.
As highlighted, our study’s main limitation is that we did not include a healthy control group and did not collect longitudinal data. Therefore, we cannot test for causal relationships. Furthermore, future studies should build on our findings and use causal statistical models to examine the relationship among LLD, physical health and the SASP index. In addition, our analyses were limited by the nature of our data. For instance, the number of participants from under-represented groups was too small, and we could not assess the influence of race or ethnicity on the SASP index. However, previous studies have suggested associations between race/ethnicity and physical health or LLD65. Also, we did not have information on socioeconomic status except for the indirect measure of years of education. Similarly, we did not have information on childhood adversity or past traumas, which might mediate the relationship between neuropsychiatric symptoms and ageing. While we included a large selection of carefully pre-selected clinical measures, other variables might be relevant to capture the clinical heterogeneity of LLD. In particular, more detailed information on smoking and alcohol consumption, other physical comorbidities (for example, cerebrovascular disease) and general markers of quality of life, activities of daily living and physical activities should be included in future studies66.
In this study, we used the SASP index as a systemic measure of biological cellular senescence status. We have used the SASP index in several previous depression studies involving over 1,000 individuals and a longitudinal follow-up28,29,30,31,67. In addition, several other groups have used a subset of the SASP proteins and reported a relationship between these proteins and frailty, negative post-surgery outcomes or concussions68,69. However, senescence is a heterogeneous phenotype, probably dependent on the cell type13,70. While the cellular source of SASP proteins is unknown, some evidence suggests that the SASP index is relevant to brain health and that brain cells express SASP proteins23,24,25. In ageing and psychiatric disorders, the blood–brain barrier permeability is increased71, leading to an enhanced passage of proteins. Some studies suggest that plasma from old mice accelerates brain ageing in young mice72, and senolytic interventions targeting the periphery alleviate the effect of SASP proteins on the brain71. However, comparable studies in humans are missing. Future studies are needed to validate the SASP index and to compare its predictive accuracy with other indices of physical morbidity or biomarkers related to senescence and ageing. In addition, studies are needed to examine the relationship between the central and peripheral expression of SASP proteins.
Conclusion
The present study aimed to understand the variables associated with biological senescence status and an increased SASP index in LLD. Physical health demonstrated the strongest association with the SASP index. In addition, age, sex and cognitive functioning were associated with the SASP index. The severity of depression and anxiety was unrelated to the SASP index. Thus, our findings highlight the importance of physical health for cellular senescence and ageing in LLD. Longitudinal studies are needed to examine the complex relationship among LLD, physical health and ageing.
Methods
Study sample
We included 426 participants, 60 years old or older, with a diagnosis of current non-psychotic major depressive disorder and a score ≥15 on the MADRS36. The present study presents a secondary data analysis of the baseline data of a completed study ((IRL-GREY), ClinicalTrials.gov Identifier: NCT00892047). The present study was a secondary data analysis of the parent IRL-GREY study35. Therefore, we did not carry out power calculations for this secondary data analysis but included all participants with plasma samples from the parent study (426 out of 468).
Participant’s assessment took place from 20 July 2009 to 30 December 2013 in research offices at three sites: the University of Pittsburgh, Pittsburgh, PA; Washington University at St Louis, St Louis, MO; and the Centre for Addiction and Mental Health, Toronto, ON, Canada. The study protocol can be found at https://www.clinicaltrials.gov/ct2/show/NCT02960763?term=Eric+Lenze&draw=2&rank=3. Ethics approval was obtained from the institutional review boards at the Washington University at St Louis, the University of Pittsburgh Medical Center and the Centre for Addiction and Mental Health. Additional approval was obtained from the institutional review board at the University of Connecticut Health Center for biomarker analyses. All participants provided written informed consent and were compensated for participating in the IRL-GREY study.
The diagnosis of major depressive disorder and the presence of a major depressive episode was based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR) diagnostic criteria73 and confirmed with the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-IV-TR)74. Exclusion criteria were lifetime diagnosis of bipolar disorder, schizophrenia, schizoaffective disorder, other psychotic disorders, current psychotic symptoms, clinical history of dementia, alcohol or substance abuse in the past 6 months, imminent suicide risk, unstable physical illness or contraindication to venlafaxine XR. Ethics approval was obtained from the institutional review boards at the three participating sites (no. 201712078), and all participants provided written informed consent. In this paper, we included only data related to the baseline assessment before the initiation of venlafaxine XR.
Clinical assessments
We obtained age, self-reported sex and self-reported race for all individuals.
Depression and anxiety characteristics
Characteristics of LLD, including the length of the current depressive episode, age of onset of the first depressive episode, recurrence, previous suicide attempts and comorbid anxiety disorders, were obtained during the SCID-IV-TR interview. The severity of depressive symptoms was evaluated by the total score on the MADRS36. Anxiety symptoms and severity were assessed by the ASI37. We evaluated suicidality with the SSI38. We also included the Medical Outcomes Survey—mental39 to assess mental well-being and quality of life.
Cognitive functioning
We recorded self-reported years of education for all individuals. Global cognitive performance was evaluated with the MMSE40 and the RBANS (global cognitive performance domain)41. Given that the RBANS does not include executive functioning, we also included the DKEFS Trail Making Test (condition 4 versus condition 5) and the DKEFS Color Word Inference (final condition 3) (executive function domain). We utilized the mean of these two variables for further analyses42.
Physical health status
We obtained anthropometric data and calculated BMI (kg m2). Blood pressure was measured while sitting after resting for at least 5 min, with systolic and diastolic blood pressure values being the mean of two measurements taken 5 min apart. We determined fasting glucose levels for all individuals. We assessed the burden of physical illness with the CIRS-G43 and the Medical Outcomes Survey—physical39.
Medication
We classified self-reported medication following the first level category of the Anatomical Therapeutic Chemical Classification. We provide a more detailed overview of psychoactive drugs, including anticonvulsants, antidepressants, antipsychotics, anxiolytics/sedatives/hypnotics, opiates and stimulants.
Laboratory analyses of the SASP proteins
Blood was collected by venipuncture with ethylenediaminetetraacetic acid tubes after overnight fasting and processed within 3 h of collection using standard procedures. Plasma was obtained from the blood by centrifugation at 3,000g for 10 min at 4 °C, aliquoted and stored in a −80 °C freezer until the laboratory analyses.
The SASP proteins were analysed by a customized multiplex assay (R&D Systems) using the Luminex platform LX 100/200 (Luminex). All laboratory personnel responsible for the analyses were blinded to demographic and clinical data. We performed all experiments according to the manufacturer’s instructions. All samples were analysed using the same assay batch on the same day to reduce variability, and the coefficient of variation was <10% for all analyses.
Given the heterogeneity of senescence and its lack of dependence on specific cells, there is no established SASP panel. However, previous research suggests that senescence markers are related to inflammation, extracellular matrix, signalling and growth factors75. On the basis of this work, we have developed a SASP index comprising 22 proteins and validated it in several studies30, including 527 individuals with depression and 638 healthy individuals31, and another study of 371 older individuals to examine the influence of depression and mild cognitive impairments on the SASP index28. We have also reported that the SASP index in depression relates to brain structural abnormalities67. Finally, in a longitudinal study of a subsample of the participants included in the present analysis, we have shown that a higher SASP index at baseline independently predicted a lower remission rate to venlafaxine treatment29.
As in our previous studies28,30, the 22 proteins included in the SASP index used in the present study are IGFBP-6, IGFBP-2, MIP-1β, IL-1β, GMC-SF, PLGF, Angiogenin, MIF-1, MIP-1α, Gro-α, IL-6, MCP-4, Gp130, ICAM-1, MCP-1, IL-8, MIP-3 α, Osteoprotegerin, TIMP-1, uPAR, TNFRI and TNFRII. The raw values were log transformed and standardized to z scores, and the SASP index for each participant was calculated based on the following regression formula:
where β is the individual weight and x is the standardized z score of each protein included in the SASP index. The weights for each biomarker were derived from our previous study in an independent sample of older adults with and without a history of major depressive disorder (Supplementary Table 8) (ref. 28).
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics 27 and GraphPad Prism 9. We only included participants for whom we could calculate the SASP index. We had complete demographic data for all participants. However, some participants were missing some clinical variables. Therefore, we used linear imputations for missing data procedures provided in IBM SPSS Statistics 27 and included all participants in our primary analyses. The last value before and the first after the missing value are used for the interpolation. If the first or last case in the series has a missing value, the missing value is not replaced.
Our analytic strategy consisted of four steps:
-
(1)
Clinical variables: following previous studies32, we conducted factor analyses to group clinical variables into different domains. It has been suggested that integrating multiple variables using factor analyses is more reliable when estimating disease trajectories33 and determining treatment outcomes34 than using single variables. Here, we conducted separate factor analyses, including variables related to (1) depression and anxiety characteristics, (2) cognitive functioning and (3) physical health. The assumptions for conducting factor analyses were tested using Bartlett’s sphericity tests. We utilized the Anderson–Rubin method to extract factors and Varimax rotation to ensure the orthogonality of the estimated factors. Only factors with an eigenvalue above one were extracted.
-
(2)
Relationship between the SASP index and demographic variables: we conducted a regression analysis with the SASP index as the dependent variable and age and sex as independent variables. We tested for normality using a normal probability plot of regression standardized residual. We calculated the variance inflation factor to detect multicollinearity between the independent variables. A P value less than 0.025 was considered significant.
-
(3)
Relationship between the SASP index and clinical variables: first, we used correlation analyses to explore the association between the SASP index and the factors determined in step one. In addition, we computed correlation analyses separately for males and females to test for a sex-specific association between the SASP index and the factors. We computed Pearson and Spearman correlations because not all variables were normally distributed. P values were Bonferroni corrected for the number of correlations computed, and a P value less than 0.0013 was considered significant. Next, we conducted a linear regression analysis with the SASP index as the dependent variable, and age, sex and all factors as independent variables. We tested for normality using a normal P-P plot of regression standardized residual. We calculated the variance inflation factor to detect multicollinearity between the independent variables. To determine if an independent variable had a significant effect on the SASP, a Bonferroni-corrected P value less than 0.0083 was considered significant. We repeated the regression analysis for males and females separately. In sensitivity analyses, we first repeated the regression analysis six times, each time excluding one of the covariates to estimate the contribution of each independent variable separately. Finally, we repeated the regression analyses, including the site (Pittsburgh, Toronto or Washington) as an additional covariate.
-
(4)
Influence of age of onset on the relationship between the SASP index and clinical variables: We conducted additional exploratory analyses to assess whether the age of onset influences the relationships above. We repeated the regression analysis for participants with early-onset (before 65 years) versus late-onset (65 years and older) depression separately.
Please note that all reported tests were two tailed.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The current data related to the biomarkers analyses from the IRL-GREY study can be shared upon request from investigators and after approval from all investigators associated with the IRL-GREY Biomarkers Study. Please contact B.S.D. at diniz@uchc.edu.
Code availability
As indicated in Methods, all statistical analyses were performed using IBM SPSS Statistics 27 and GraphPad Prism 9. We did not use custom code.
References
Diniz, B. S. et al. The effect of gender, age, and symptom severity in late-life depression on the risk of all-cause mortality: the Bambuí Cohort Study of Aging. Depress. Anxiety 31, 787–795 (2014).
Lin, J. H. et al. Late-life depression and quality of life in a geriatric evaluation and management unit: an exploratory study. BMC Geriatr. 14, 77 (2014).
Almeida, O. P. et al. Depression, frailty, and all-cause mortality: a cohort study of men older than 75 years. J. Am. Med. Dir. Assoc. 16, 296–300 (2015).
Ditmars, H. L. et al. Associations between depression and cardiometabolic health: a 27-year longitudinal study. Psychol. Med. https://doi.org/10.1017/s003329172000505x (2021).
Diniz, B. S., Butters, M. A., Albert, S. M., Dew, M. A. & Reynolds, C. F. 3rd Late-life depression and risk of vascular dementia and Alzheimer’s disease: systematic review and meta-analysis of community-based cohort studies. Br. J. Psychiatry 202, 329–335 (2013).
Qiao, Y. et al. Role of depressive symptoms in cardiometabolic diseases and subsequent transitions to all-cause mortality: an application of multistate models in a prospective cohort study. Stroke Vasc. Neurol. 6, 511–518 (2021).
Mendes-Silva, A. P. et al. Shared biologic pathways between Alzheimer disease and major depression: a systematic review of microRNA expression studies. Am. J. Geriatr. Psychiatry 24, 903–912 (2016).
Kuo, C. Y., Lin, C. H. & Lane, H. Y. Molecular basis of late-life depression. Int. J. Mol. Sci. 22, 7421 (2021).
Wolkowitz, O. M., Epel, E. S., Reus, V. I. & Mellon, S. H. Depression gets old fast: do stress and depression accelerate cell aging? Depress. Anxiety 27, 327–338 (2010).
Laks, J. Invited perspective on ‘the molecular intersection between senescence and major depression in the elderly’. Am. J. Geriatr. Psychiatry 26, 1106–1107 (2018).
Hayflick, L. & Moorhead, P. S. The serial cultivation of human diploid cell strains. Exp. Cell. Res. 25, 585–621 (1961).
Herranz, N. & Gil, J. Mechanisms and functions of cellular senescence. J. Clin. Invest. 128, 1238–1246 (2018).
Basisty, N. et al. A proteomic atlas of senescence-associated secretomes for aging biomarker development. PLoS Biol. 18, e3000599 (2020).
Tchkonia, T., Zhu, Y., van Deursen, J., Campisi, J. & Kirkland, J. L. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J. Clin. Invest. 123, 966–972 (2013).
Tominaga, K. The emerging role of senescent cells in tissue homeostasis and pathophysiology. Pathobiol. Aging Age Relat. Dis. 5, 27743 (2015).
Karin, O., Agrawal, A., Porat, Z., Krizhanovsky, V. & Alon, U. Senescent cell turnover slows with age providing an explanation for the Gompertz law. Nat. Commun. 10, 5495 (2019).
Childs, B. G. et al. Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science 354, 472–477 (2016).
Jeon, O. H., David, N., Campisi, J. & Elisseeff, J. H. Senescent cells and osteoarthritis: a painful connection. J. Clin. Invest. 128, 1229–1237 (2018).
Demaria, M. et al. Cellular senescence promotes adverse effects of chemotherapy and cancer relapse. Cancer Discov. 7, 165–176 (2017).
Valentijn, F. A., Falke, L. L., Nguyen, T. Q. & Goldschmeding, R. Cellular senescence in the aging and diseased kidney. J. Cell Commun. Signal 12, 69–82 (2018).
Baker, D. J. et al. Naturally occurring p16(Ink4a)-positive cells shorten healthy lifespan. Nature 530, 184–189 (2016).
Takahashi, A. et al. Downregulation of cytoplasmic DNases is implicated in cytoplasmic DNA accumulation and SASP in senescent cells. Nat. Commun. 9, 1249 (2018).
Flanary, B. E., Sammons, N. W., Nguyen, C., Walker, D. & Streit, W. J. Evidence that aging and amyloid promote microglial cell senescence. Rejuvenation Res. 10, 61–74 (2007).
Salminen, A. et al. Astrocytes in the aging brain express characteristics of senescence-associated secretory phenotype. Eur. J. Neurosci. 34, 3–11 (2011).
Ishikawa, S. & Ishikawa, F. Proteostasis failure and cellular senescence in long-term cultured postmitotic rat neurons. Aging Cell 19, e13071 (2020).
Saez-Atienzar, S. & Masliah, E. Cellular senescence and Alzheimer disease: the egg and the chicken scenario. Nat. Rev. Neurosci. 21, 433–444 (2020).
Coppé, J. P. et al. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol. 6, 2853–2868 (2008).
Diniz, B. S. et al. Mild cognitive impairment and major depressive disorder are associated with molecular senescence abnormalities in older adults. Alzheimers Dement. 7, e12129 (2021).
Diniz, B. S. et al. Association of molecular senescence markers in late-life depression with clinical characteristics and treatment outcome. JAMA Netw. Open 5, e2219678 (2022).
Diniz, B. S. et al. Enhanced molecular aging in late-life depression: the senescent-associated secretory phenotype. Am. J. Geriatr. Psychiatry 25, 64–72 (2017).
Diniz, B. S., Reynolds Iii, C. F., Sibille, E., Bot, M. & Penninx, B. Major depression and enhanced molecular senescence abnormalities in young and middle-aged adults. Transl. Psychiatry 9, 198 (2019).
Shiovitz-Ezra, S., Leitsch, S., Graber, J. & Karraker, A. Quality of life and psychological health indicators in the national social life, health, and aging project. J. Gerontol. B Psychol. Sci. Soc. Sci. 64, i30–i37 (2009).
Lemke, H. et al. Association of disease course and brain structural alterations in major depressive disorder. Depress. Anxiety 39, 441–451 (2022).
Wallace, M. L., Frank, E. & Kraemer, H. C. A novel approach for developing and interpreting treatment moderator profiles in randomized clinical trials. JAMA Psychiatry 70, 1241–1247 (2013).
Lenze, E. J. et al. Efficacy, safety, and tolerability of augmentation pharmacotherapy with aripiprazole for treatment-resistant depression in late life: a randomised, double-blind, placebo-controlled trial. Lancet 386, 2404–2412 (2015).
Montgomery, S. A. & Asberg, M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry 134, 382–389 (1979).
Reiss, S., Peterson, R. A., Gursky, D. M. & McNally, R. J. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav. Res. Ther. 24, 1–8 (1986).
Beck, A. T., Kovacs, M. & Weissman, A. Assessment of suicidal intention: the scale for suicide ideation. J. Consulting Clin. Psychol. 47, 343–352 (1979).
Ware, J. E. SF-36 Health Survey: Manual and Interpretation Guide (The Health Institute, New England Medical Center, 1997); https://www.researchgate.net/profile/John-Ware-6/publication/313050850_SF-36_Health_Survey_Manual_Interpretation_Guide/links/594a5b83aca2723195de5c3d/SF-36-Health-Survey-Manual-Interpretation-Guide.pdf
Folstein, M. F., Folstein, S. E. & McHugh, P. R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Randolph, C., Yierney, M. C., Mohr, E. & Chase, T. N. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J. Clin. Exp. Neuropsych. 20, 310–319 (1998).
Delis, D. C., Kaplan, E. & Kramer, J. H. Delis-Kaplan Executive Function System (APA PsycTests, 2001); https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Cognition-%26-Neuro/Delis-Kaplan-Executive-Function-System/p/100000618.html
Miller, M. D. et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res. 41, 237–248 (1992).
Diniz, B. S. The molecular intersection between senescence and major depression in the elderly. Am. J. Geriatr. Psychiatry 26, 1097–1105 (2018).
Reynolds, C. F. 3rd et al. Maintenance treatment of major depression in old age. N. Engl. J. Med. 354, 1130–1138 (2006).
Oliva-Olivera, W. et al. Neovascular deterioration, impaired NADPH oxidase and inflammatory cytokine expression in adipose-derived multipotent cells from subjects with metabolic syndrome. Metab. Clin.Exp. 71, 132–143 (2017).
Schafer, M. J. et al. Exercise prevents diet-induced cellular senescence in adipose tissue. Diabetes 65, 1606–1615 (2016).
Lin, Y. F., Wang, L. Y., Chen, C. S., Li, C. C. & Hsiao, Y. H. Cellular senescence as a driver of cognitive decline triggered by chronic unpredictable stress. Neurobiol. Stress 15, 100341 (2021).
Gu, D., Li, J., Little, J., Li, H. & Zhang, X. Associations between serum sex hormone concentrations and telomere length among U.S. adults, 1999–2002. J. Nutr. Health Aging 24, 48–54 (2020).
Juster, R. P. et al. Sex and gender roles in relation to mental health and allostatic load. Psychosom. Med. 78, 788–804 (2016).
Anstey, K. J. & Luszcz, M. A. Mortality risk varies according to gender and change in depressive status in very old adults. Psychosom. Med. 64, 880–888 (2002).
Cristancho, P. et al. Executive function predicts antidepressant treatment noncompletion in late-life depression. J. Clin. Psychiatry https://doi.org/10.4088/JCP.16m11371 (2018).
Chinta, S. J. et al. Cellular senescence and the aging brain. Exp. Gerontol. 68, 3–7 (2015).
Vyas, C. M. & Okereke, O. I. Late-life depression: a narrative review on risk factors and prevention. Harv. Rev. Psychiatry 28, 72–99 (2020).
Schmaal, L. et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Mol. Psychiatry 22, 900–909 (2017).
Mendes-Silva, A. P. et al. Telomere shortening in late-life depression: a potential marker of depression severity. Brain Behav. 11, e2255 (2021).
Schaakxs, R., Verhoeven, J. E., Oude Voshaar, R. C., Comijs, H. C. & Penninx, B. Leukocyte telomere length and late-life depression. Am. J. Geriatr. Psychiatry 23, 423–432 (2015).
Verhoeven, J. E. et al. Depression, telomeres and mitochondrial DNA: between- and within-person associations from a 10-year longitudinal study. Mol. Psychiatry 23, 850–857 (2018).
Lin, C. H., Wang, S. H. & Lane, H. Y. Effects of sodium benzoate, a D-amino acid oxidase inhibitor, on perceived stress and cognitive function among patients with late-life depression: a randomized, double-blind, sertraline- and placebo-controlled trial. Int. J. Neuropsychopharmacol. 25, 545–555 (2022).
Evans, D. L. et al. Mood disorders in the medically ill: scientific review and recommendations. Biol. Psychiatry 58, 175–189 (2005).
Gallo, J. J. et al. Long term effect of depression care management on mortality in older adults: follow-up of cluster randomized clinical trial in primary care. BMJ 346, f2570 (2013).
Mason, A. E. et al. Weight loss maintenance and cellular aging in the supporting health through nutrition and exercise study. Psychosom. Med. 80, 609–619 (2018).
Gujral, S. et al. Exercise for depression: a feasibility trial exploring neural mechanisms. Am. J. Geriatr Psychiatry 27, 611–616 (2019).
Sharma, R. & Padwad, Y. In search of nutritional anti-aging targets: TOR inhibitors, SASP modulators, and BCL-2 family suppressors. Nutrition 65, 33–38 (2019).
Vyas, C. M. et al. Association of race and ethnicity with late-life depression severity, symptom burden, and care. JAMA Netw. Open 3, e201606 (2020).
Kim, C. J., Park, J., Kang, S. W. & Schlenk, E. A. Factors affecting aging cognitive function among community-dwelling older adults. Int. J. Nurs. Pract. https://doi.org/10.1111/ijn.12567 (2017).
Mendes-Silva, A. P. et al. Molecular senescence is associated with white matter microstructural damage in late-life depression. Am. J. Geriatr. Psychiatry 27, 1414–1418 (2019).
Schafer, M. J. et al. The senescence-associated secretome as an indicator of age and medical risk. JCI Insight https://doi.org/10.1172/jci.insight.133668 (2020).
Schwab, N., Grenier, K. & Hazrati, L. N. DNA repair deficiency and senescence in concussed professional athletes involved in contact sports. Acta Neuropathol. Commun. 7, 182 (2019).
Saul, D. et al. A new gene set identifies senescent cells and predicts senescence-associated pathways across tissues. Nat. Commun. 13, 4827 (2022).
Sikora, E. et al. Cellular senescence in brain aging. Front. Aging Neurosci. 13, 646924 (2021).
Villeda, S. A. et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature 477, 90–94 (2011).
Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR 4th edn, text revision (American Psychiatric Association, 2000).
First, M., Spitzer, R. L., Gibbon, M. & Williams, J. B. W. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) (Biometrics Research, New York State Psychiatric Institute, 2002).
Evans, S. A., Horrell, J. & Neretti, N. The three-dimensional organization of the genome in cellular senescence and age-associated diseases. Semin. Cell Dev. Biol. 90, 154–160 (2019).
Acknowledgements
This work was funded by NIH grants R01MH118311 (B.S.D. and G.T.) and R01 MH083660 (C.F.R., B.H.M., E.J.L.) the Harvard Medical School Livingston Fellowship Award and the Young Investigator Grant sponsored by Mary and John Osterhaus and the Brain & Behavior Research Foundation (J.S.-H.). Additional support came from P50MH122351 and the Taylor Family Institute for Innovative Psychiatric Research at Washington University (E.L.V.).
Author information
Authors and Affiliations
Contributions
J.S.-H.: study hypothesis formulation, statistical data analyses and the draft of the paper. B.H.M., C.F.R., D.M.B., J.F.K., M.A.B. and E.J.L.: clinical trial study design and execution. A.P.M.-S. and E.L.V.: design of customized biomarkers assays and biomarker laboratory analyses. G.T.: statistical data analyses. B.S.D.: study hypothesis formulation, design of the customized biomarkers assay, statistical data analyses and the draft of the paper. In addition, all authors provided intellectual contributions to all aspects of the current work, and they revised and approved the submission of the paper for peer review.
Corresponding authors
Ethics declarations
Competing interests
E.J.L. is a consultant for Prodeo, IngenioRx, Pritikin ICR and Boehringer-Ingelheim, has a patent application for sigma-1 agonists in COVID-19 treatment and receives research support from PCORI, COVID Early Treatment Fund, Emergent Venture FastGrants and MagStim. J.F.K. reports receiving an honorarium from Otsuka for the preparation and presentation of a webinar (disease-state, not product focused), from NightWare and Biogen for scientific advising and potential equity from Aifred Health for scientific advising. B.H.M. holds and receives support from the Labatt Family Chair in Biology of Depression in Late-Life Adults at the University of Toronto. He also receives compensation from the Centre for Addiction and Mental Health (CAMH) and the University of Toronto, Ontario. He currently receives research support from Brain Canada, the Canadian Institutes of Health Research, the CAMH Foundation, the US National Institute of Health (NIH), Capital Solution Design LLC (software used in a study funded by CAMH Foundation) and HAPPYneuron (software used in a study funded by Brain Canada). Within the past 3 years, he has received research support from the Patient-Centered Outcomes Research Institute (PCORI), and he has been an unpaid consultant to Myriad Neuroscience. D.M.B. receives research support from CIHR, NIH, Brain Canada and the Temerty Family through the CAMH Foundation and the Campbell Research Institute. He received research support and in-kind equipment support for an investigator-initiated study from Brainsway Ltd. He has been the site principal investigator for sponsor-initiated studies for Brainsway Ltd. He also receives in-kind equipment support from Magventure for investigator-initiated studies. He received medication supplies for an investigator-initiated trial from Indivior. The other co-authors do not have a conflict of interest related to this study.
Peer review
Peer review information
Nature Mental Health thanks Martino Belvederi Murri, Federico Triolo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Table 1: CONSORT 2010 checklist of information to include when reporting a randomized trial. Supplementary Table 2: Medication. Supplementary Table 3: Factor analyses. Supplementary Table 4: Correlations between SASP index and factors. Supplementary Table 5: Correlations between factors. Supplementary Table 6: Explained variance in regression analyses, dependent variable SASP. Supplementary Table 7: Regression analyses with the site as an additional covariate, dependent variable SASP. Supplementary Table 8: Weights to construct the SASP index. Supplementary Fig. 1: Relationship between the SASP index and demographic and clinical variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seitz-Holland, J., Mulsant, B.H., Reynolds III, C.F. et al. Major depression, physical health and molecular senescence markers abnormalities. Nat. Mental Health 1, 200–209 (2023). https://doi.org/10.1038/s44220-023-00033-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00033-z
This article is cited by
-
Cellular senescence and frailty: a comprehensive insight into the causal links
GeroScience (2023)
-
The heterogeneity of late-life depression and its pathobiology: a brain network dysfunction disorder
Journal of Neural Transmission (2023)