Abstract
Low-density lipoprotein (LDL) indubitably contributes causally to atherosclerosis, a leading challenge to health worldwide. Interventions that lower LDL cholesterol (LDL-C) have made remarkable inroads against this global scourge. Recent therapeutic advances have achieved ever lower levels of LDL-C. Improved cardiovascular outcomes continue to accrue from these interventions. In particular, the discovery of the role of proprotein convertase subtilisin/kexin type 9 (PCSK9) as the causal gene in autosomal-dominant hypercholesterolemia has led with remarkable speed to the development of novel agents to lower LDL-C concentrations beyond prior measures, and to alleviate further cardiovascular risk. We review how this story, and its position in the broader landscape of therapy to prevent atherosclerotic events, represents a notable victory of contemporary cardiovascular medicine and reflects successful partnerships between basic scientists, the pharmaceutical and biotechnology sectors, and clinical investigators. Continued cooperation in this manner promises to yield further progress in combating cardiovascular diseases beyond interventions on LDL-C.
Similar content being viewed by others
Main
In the wake of the epidemiologic transition, as communicable diseases have receded, atherosclerotic cardiovascular disease has become a global scourge. Developing nations bear the greatest burden of atherosclerotic risk in the current era. Unfortunately, unhealthy lifestyle behaviors remain rampant. Healthful diets, engaging in regular physical activity, not becoming obese, and avoiding tobacco smoking could make major inroads into this modern epidemic. Yet, societal and individual measures to foster healthy lifestyles remain difficult to institute and sustain. But we fortunately possess a growing palette of pharmacologic tools to repel the ravages of atherosclerosis and to supplement efforts to improve lifestyle. Moreover, we have an increasing appreciation for genetic contributors to atherosclerosis, both rarer monogenic mutations and more-common variants that provoke smaller effect sizes. In individuals with inherited heightened risk of atherosclerotic cardiovascular disease, even a pristine lifestyle cannot obviate cardiovascular risk. This review describes the current landscape of management of atherogenic lipoproteins, notably low-density lipoprotein (LDL), with an emphasis on the role of strategies that target proprotein convertase subtilisin/kexin type 9 (PCSK9).
LDL causes human atherothrombosis
The introduction of the ultracentrifuge to analytical biochemistry led to the categorization of different fractions of blood lipids1 (Fig. 1). One of these fractions associated particularly with atherosclerotic cardiovascular events: LDL. Hydrophobic lipids, such as triglyceride and cholesterol, and its esters require a water-soluble coating to circulate in an aqueous medium, such as blood. Lipoprotein particles package the water-insoluble lipids in a shell of more polar lipids decorated by a series of proteins designated apolipoproteins. The apolipoproteins can serve as molecular addresses that can direct various lipoprotein particles to specific receptors on particular cells. The signature apolipoprotein of LDL, apolipoprotein B (ApoB), roughly encircles the equator of the LDL particle. LDL can also bear ApoE. In this Review, we make a distinction between ‘LDL cholesterol, LDL-C’ and ‘LDL,’ referring to the particle. As LDL particles can contain a different mix of apolipoproteins and varying quantities of other constituents, such as phospholipids, fat-soluble vitamins, and so on, we refer to the particle as LDL and its payload of cholesterol/cholesteryl ester as LDL-C.
Both ApoB and ApoE serve as ligands for the canonical LDL receptor characterized originally by Brown and Goldstein2 (Fig. 1). The discovery of the LDL receptor, and study of its expression in fibroblasts obtained from individuals with familial hypercholesterolemia and hence elevated cardiovascular risk, affirmed that mutations in the LDL receptor are the genetic basis of this common form of familial hypercholesterolemia (FH, now classified as FH1). Heterozygous LDL receptor mutations constitute one of the most common genetic diseases in humans, affecting as many 1 in 300 individuals. Those with homozygous null or hypofunctioning LDL receptors or compound heterozygotes have an extraordinarily elevated risk of premature atherothrombotic events. Such individuals with genetically determined elevations in LDL-C can experience myocardial infarction as early as the first decade of life in the homozygous condition.
A phenocopy of familial hypercholesterolemia (FH2), described by Innerarity and colleagues, results from a mutation at residue 3500 in ApoB that interferes with its recognition by the LDL receptor3. The molecular basis of a third form of familial hypercholesterolemia, autosomal dominant hypercholesterolemia, remained obscure until recently, as will be discussed in detail below. A rare autosomal recessive form of familial hypercholesterolemia (FH4) arises from mutations in the LDL protein receptor adaptor 1 (LDLRAP1) that associate with reduced LDL-receptor-dependent LDL catabolism, through mechanisms that remain indistinct4,5.
Beyond these four monogenic forms of hypercholesterolemia, advances in human genetics have identified myriad more-common variants that each produce small increments in LDL over the lifetime of the individual. We all carry a palette of such variants. Those who accumulate a greater burden of variants that elevate LDL-C have increased cardiovascular risk. Successive generations of polygenic risk scores allow us to gauge the burden of elevations in LDL due to these more-common genetic variants6. This concordant human genetic evidence strengthens the case for causality of LDL in human atherosclerosis (Box 1).
The astute physician Carl Müller in 1938 observed the relationship between angina pectoris, xanthomata, and hypercholesterolemia7. This clinical association, subsequently supported by decades of observational epidemiologic research, coupled with the characterization of lipoproteins, demonstrated strong circumstantial evidence for the participation of LDL-C in human atherosclerosis. Studies with pharmacologic interventions that lower LDL-C provide further evidence supporting the causality of LDL in human atherothrombosis8.
Approaches to therapy for elevated LDL
One of the first large-scale randomized trials of pharmacologic treatment of hypercholesterolemia, the Lipid Research Clinics (LRC) study, supported by the US National Heart, Lung, and Blood Institute, used bile-acid sequestrants9,10. These unpalatable resins, taken orally, bind bile acids in the intestine and promote their excretion in feces. As bile acids derive from cholesterol, this led to a modest lowering of LDL-C. Bile acid sequestrants can also raise triglyceride concentrations in the blood, an unwanted action in atherosclerotic individuals. The LRC study showed a modest decrease in cardiovascular events, but no improvement in mortality. The relatively modest benefits of a very hard-to-tolerate medication led many prominent physicians and lay critics alike to denigrate the value of LDL-C lowering in clinical practice11,12,13.
The introduction of the HMG-CoA reductase inhibitors helped to deter this perception. The Japanese scientist Akira Endo sought inhibitors of the rate-limiting enzyme in cholesterol synthesis, hydroxymethylglutaryl coenzyme A, in natural products of soil bacteria14. This work reflected the extensive experience with fermentation in Japan and the quest for new antibiotics following Fleming’s discovery of penicillin, a product of a microorganism. Endo’s success led to rapid exploration of other inhibitors of this key enzyme and led to the development of the first generation of statins. The landmark Scandinavian Simvastatin Survival Study (4S) demonstrated with rigor the ability of a statin to reduce cardiovascular events in high-risk individuals15. These data caused some doubters to recant.
Successive studies with statins have addressed individuals with progressively lower risks, and the development of more potent statins has led to the ability to drive LDL concentrations even lower. The ensemble of large-scale clinical trials with statins firmly established the benefits of LDL lowering. The results fostered the concept of ‘lower is better.’ Moreover, the safety profile of this class of agents demonstrated that low concentrations of LDL, more akin to those of a human neonate or many animal species, did not entail adverse consequences16.
LDL lowering beyond statins
The quest for inhibitors of another enzyme involved in lipid metabolism, acyl-coenzyme A, cholesterol acyltransferase (ACAT), led to the identification of a molecule, ezetimibe, that produced a 15–20% reduction in LDL-C. A brilliant series of experiments showed that the target of this molecule was not ACAT, but rather a cholesterol transporter in the small intestine responsible for uptake of dietary and biliary cholesterol: Niemann-Pick C1-like protein 1 (NPC1L1)17. Coadministration of simvastatin with ezetimibe produced a decrease in adverse cardiovascular events after a 7-year observation period in a large-scale clinical trial (IMPROVE-IT), which demonstrated the ability of a non-statin to contribute to reduced cardiovascular risk in individuals already receiving an evidence-based statin regimen18. Although significant, the modest absolute risk reduction of a few percent indicates diminishing returns of the additional LDL-C lowering of some 17 mg/dL that the addition of ezetimibe to the evidence-based dose of simvastatin affords (40 mg daily)18,19.
Another therapeutic, bempedoic acid, a dicarboxylic acid with 15-carbon chain length and derivatized in the alpha and omega sites by methyl groups and a hydroxy group at carbon 8, inhibits another enzyme a few steps upstream of HMG-CoA reductase in the cholesterol biosynthetic pathway: ATP-citrate lyase20. This compound can lower LDL-C by 15–20%, similar to the extent of reduction achieved by ezetimibe treatment. It produces incremental drops in LDL-C when combined with a statin or ezetimibe. Bempedoic acid is a prodrug that requires activation by an enzyme principally present in hepatocytes to attain its inhibitory activity. This feature may permit it to evade some of the unwanted muscle-related actions or symptoms associated with statin use. Skeletal muscle does not contain the enzyme SLC27A2, which derivatizes the parent molecule to the active thioester.
Both ezetimibe and bempedoic acid have received regulatory approval in most jurisdictions and can be used as monotherapy or in combination with statins or each other to achieve LDL-C lowering. A large-scale randomized trial in individuals who are unable to tolerate statins is tracking cardiovascular outcomes following treatment with bempedoic acid21. Cholesteryl ester transfer protein (CETP) inhibitors were initially developed for their ability to raise HDL cholesterol in hope of decreasing cardiovascular events, but these have shown no or little efficacy, and sometimes even harm, in clinical trials. Obicetrapib, a potent CETP inhibitor, can lower LDL-C by about 50% when given in addition to high-intensity statins and undergoing testing in a cardiovascular outcome trial.
The PCSK9 story
As noted above, identifying the genetic defects linked to autosomal dominant hypercholesterolemia lagged behind such identification for other common forms of familial hypercholesterolemia (Fig. 1). Careful study of kindreds with autosomal dominant hypercholesterolemia by two talented female scientists, Marianne Abifadel and Catherine Boileau, working in Paris, delineated a candidate locus for the defective gene. Meanwhile, Nabil Seidah, working at the Institute for Clinical Research in Montreal, developed great expertise in proteolytic enzymes that process proteins, following the initial discoveries of Michel Crétien. Through felicitous conjunction, the Paris group and the Montreal group identified a candidate, proprotein convertase subtilisin/kexin type 9 (PCSK9), as the causal gene in autosomal dominant hypercholesterolemia22. Gain-of-function mutations in this gene yielded elevations in LDL-C. Thereafter, Helen Hobbs and Jonathan Cohen found that individuals with loss of function in PCSK9 identified in the Dallas Heart Study seemed to enjoy protection from atherosclerotic cardiovascular disease23.
PCSK9 functions as a chaperone to channel the LDL receptor for intracellular catabolism, preventing its recycling to the cell surface (Fig. 2). The increased LDL receptor expression augments LDL clearance and lowers plasma LDL-C. PCSK9 is an unusual proteinase24. Although it is a member of the proprotein convertase family, it resembles proteinase K, distinct from other family members. It also exhibits peculiar biochemical properties. Like other family members, it undergoes auto-catalytic cleavage. But PCSK9 is secreted with its pro-piece attached and is thus catalytically inactive, as the pro-piece remains associated with the cleaved protein and hinders the enzyme’s active site. Furthermore, PCSK9 also undergoes processing by furin to a smaller product that leads to release of the pro-domain, but this cleavage yields a dead enzyme. Indeed, several lines of biochemical evidence suggest that the ability of PCSK9 to reduce the LDL receptor does not depend on its catalytic activity. Although the design of proteinase inhibitors by medicinal chemistry is a well-trodden path to drug development, the independence of PCSK9’s regulation of the LDL receptor from enzymatic activity has frustrated this approach. That is why the first effective therapeutic agents to reduce PCSK9 concentrations used antibody neutralization instead of the more usual small-molecule approach.
This figure depicts the mechanisms by which PCSK9 influences the number of LDL receptors on the cell surface. The depiction of the hepatocyte on the left shows how, under conditions of lower PCSK9 concentrations, the LDL receptor recycles to the cell surface. In the presence of higher concentrations of PCSK9, the complex with the LDL receptor targets the receptor for lysosomal degradation.
This alternative approach, the development of biologicals, has proved more promising. Monoclonal antibodies that can neutralize PCSK9 have proven efficacy in large-scale clinical trials. The rapid development of antibody therapeutics represents a true victory of science and translational medicine. Progressing from study of families with a relatively rare trait to the identification of a target protein and the rapid evolution and validation of a therapeutic approach in the span of less than 15 years illustrates the power of partnerships between human geneticists, biochemists, and the pharmaceutical industry. The two therapeutics that have proven useful in large-scale clinical trials, evolocumab and alirocumab, have received regulatory approval worldwide25,26. A third antibody, bococizumab, which retained approximately 3% of mouse sequences, generated anti-drug antibodies that led to diminished efficacy with time and halted its development27. The pivotal outcome trials with evolocumab and alirocumab enrolled individuals who were, for the most part, treated effectively with statins, affirming the efficacy of adding PCSK9 inhibition to this treatment. The degree of LDL lowering achieved by administering a PCSK9-neutralizing antibody to statin-treated individuals considerably exceeds that which is achievable with ezetimibe or bempedoic acid combined with statins.
Two major studies in very high-risk individuals have demonstrated that PCSK9 monoclonal antibody inhibitors reduce LDL-C by 60% and cardiovascular events by 15–20% when added to statin and/or ezetimibe treatment. Current guidelines recommend PCSK9 monoclonal antibody inhibitors as an add-on therapy for very high-risk patients to achieve LDL-C goals28. Imaging studies have given us some insight into the effects of PCSK9 monoclonal antibody on the atherosclerotic plaque. GLAGOV used intravascular ultrasound to show that the addition of evolocumab to a statin could result in plaque regression29. Newer imaging studies using OCT have demonstrated that the addition of PCSK9 inhibitor to statin therapy alters plaque composition, reflected by increased fibrous cap thickness and decreased lipid arc30,31,32. The PACMAN-AMI study used this approach to establish a reduction in atheroma volume and an increase in the thickness of the plaques’ protective fibrous cap in individuals with recent acute coronary syndrome receiving the PCSK9 antibody alirocumab in addition to statin32. Such alterations could render a plaque less susceptible to rupturing and provoking thrombus formation. A secondary analysis of the FOURIER trial demonstrated a significant reduction in the risk of acute arterial events across all arterial territories33. Women have higher circulating PCSK9 levels than men; however, a recent pooled analysis of PCSK9 inhibition trials showed no sex difference in clinical benefit34,35.
Cardiovascular medicine has entered an era of RNA therapeutics (Fig. 3 and Tables 1 and 2). It is now possible to selectively target genes that have key roles in lipid metabolism by antisense oligonucleotides and small interfering RNA (siRNA). New-generation nucleic-acid-based therapies conjugated with N-acetylgalactosamine (GalNAc) target them to the liver by binding the asialoglycoprotein receptor on hepatocytes, thus maintaining efficacy with the administration of much lower doses than those used for untargeted agents and decreasing unwanted actions36.
(i) Monoclonal anti-PCSK9 antibodies bind their target in the extracellular space. This neutralization prevents PCSK9 from binding to the LDL receptor, and it thus enters the cytoplasm joined to this cell surface receptor, directing the LDL receptor to the phagolysosome for degradation and limiting its recycling to the membrane. Thus, PCSK9 inhibition augments LDL receptors on the cell surface, where they can bind and clear LDL from the circulation. (ii) siRNA agents engineered to bind to the mRNA that encodes PCSK9 and direct catabolism of this mRNA, and can do so in a serial manner. Thus, one molecule of anti-PCSK9 siRNA can direct the degradation of many messages that encode PCSK9, limiting the translation and protein expression of this chaperone. (iii) Antisense RNAs promote destruction of the PCSK9 messenger RNA, but do so with a one-to-one stoichiometry. (iv) Small-molecule blockers of PCSK9 function in development mimic the action of the biologicals and provide a potential oral route of administration, rather than requiring parenteral administration, as is the case for the anti-PCSK9 antibodies. (v) CRISPR–Cas9-mediated gene or base editing alters the nucleotide sequence in the nuclear DNA, inhibiting the transcription of the messenger RNA that encodes PCSK9.
An siRNA that causes catabolism of PCSK9 messenger RNA has been developed; it acts intracellularly to block the synthesis of PCSK9. Owing to the recycling of siRNA, inclisiran, the siRNA agent that targets PCSK9, has more-prolonged LDL-lowering efficacy than that of the monoclonal antibodies that require administration every 2–4 weeks37. Inclisiran’s duration of action permits it to be given just twice, or even once, yearly. Inclisiran has received approval in European countries and in the United States for heterozygous familial hypercholesterolemia. A large-scale outcome trial is testing the efficacy of LDL lowering by targeting PCSK9 with this siRNA.
Research has continued into alternative methods to inhibit PCSK9, which may cost less and have easier administration (Fig. 3 and Table 1). The development of an oral PCSK9 inhibitor has proven challenging owing to decreased bioavailability after ingestion. Recently, an orally bioavailable cyclic peptide, PCSK9i, has entered clinical development. Phase 1 studies have shown that this agent on top of statin therapy reduced LDL-C levels by ~65% at day 14 compared with baseline levels, and was well tolerated38. A small, non-biological, synthetic ligand that binds PCSK9 with low-nanomolar affinity can reduce PCSK9 activity and increase hepatic LDLR expression in mice39. This approach might also provide a tool for oral PCSK9 inhibition.
Other approaches to target the mRNA to prevent the formation of PCSK9 have begun being evaluated. A recently developed liver-targeted antisense oligonucleotide that inhibits the expression of PCSK9 decreased LDL-C by 73% in 12 weeks and was well tolerated at the higher dose in a multiple ascending-dose study in people receiving statin treatment40. To achieve long-term LDL-C lowering, the quest for an effective PCSK9 vaccine continues. These efforts aim to trigger the generation of host anti-PCSK9 antibodies. Preclinical studies have shown the effectiveness of a peptide-based active vaccination against PCSK9 in hypercholesterolemic mice. This vaccine is undergoing testing in non-human primates, but the long-term efficacy and safety in humans still requires demonstration41. A phase I study assessing the safety, tolerability, immunogenicity, and LDL-lowering activity of a vaccine targeting PCSK9 has shown induction of a strong PCSK9-reactive antibody response that reduces LDL-C levels in healthy participants by 11.2% and 13.3% at weeks 20 and 70. Booster immunization enhanced this immune response42.
The advent of gene editing using CRISPR–Cas9 has opened the possibility of permanent alteration in genes, including that which encodes PCSK9. In an exciting study, Musunuru and Kathiresan’s team and Rothgangl et al. used a base-editing approach to permanently block PCSK9 gene expression in non-human primates43,44. Base editing, a later-generation CRISPR technique, permits a more precise alteration in genomic DNA, altering just one base rather than depending on DNA-repair processes, which may be more prone to off-target genetic alterations. Moreover, base editing has the potential of reversibility, providing an ‘antidote’ to otherwise lifelong genetic alteration. The base-editing approach in cynomolgus monkeys (Macaca fascicularis) showed a striking decrease in plasma PCSK9 and a concordant 60% decrease in blood LDL-C over at least an approximate eight-month period of observation. Extensive care to avoid off-target genetic alteration and exploration of potential off-target effects provided initial reassurance regarding the safety of this approach.
The clinical application of gene editing will require considerable ethical and regulatory surveillance. Yet, the power of these evolving technologies of genomic intervention is such that their use is inevitable. We must confront the ethical issues and evaluate potential off-target or enduring unwanted actions of such approaches in a steadfast manner. With appropriate safeguards, the application of gene- or base-editing technology could prove revolutionary for diseases caused by elevated LDL-C, such as atherosclerosis. Base-editing interference in PCSK9 gene expression could provide a lifetime lowering of LDL-C. Human genetic studies indicate that long duration of exposure to lower levels of LDL-C can confer considerable cardiovascular benefit over a lifetime45. Such a durable therapeutic approach could avoid issues of compliance and access, obviating some of the major obstacles to the therapeutic lowering of LDL-C encountered in practice.
The PCSK9 antibodies act extracellularly. Base-editing or siRNA approaches act intracellularly. Safety issues due to other or unknown actions of PCSK9 might pertain to the intracellular manipulations to a greater extent than extracellular anti-PCSK9 antibody administration. For example, certain studies have raised the specter of dysglycemia associated with reduced function of PCSK9 (refs. 46,47). Although no signal has emerged from the large-scale therapeutic application of monoclonal antibodies that target PCSK9, the intracellular interventions will require careful consideration in this regard.
Some of the beneficial effects of statins on cardiovascular events do not depend on LDL lowering. The so-called ‘pleiotropic’ effects of statins have well-founded molecular bases: interference in prenylation of small G proteins and induction of transcription factors such as Krüppel-like factor 2 (KLF2)48,49. These targets of statins can mute inflammatory and thrombotic pathways and boost availability of nitric oxide, an endogenous vasodilator with multiple anti-atherothrombotic actions. Analyses of clinical trials with statins have provided observational evidence that up to 50% of the benefit of statins results from a direct anti-inflammatory action independent of LDL lowering50. In this regard, PCSK9 inhibition does not appear to share strong and consistent anti-inflammatory actions, aside from the lowering of LDL-C. Thus, theoretically, a combination of an anti-inflammatory therapy with PCSK9 reduction could amplify cardiovascular benefit.
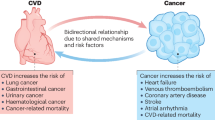
Recent observations have demonstrated altered cardiac lipid and mitochondrial metabolism in PCSK9-deficient mice in an LDLR-independent manner, leading to the development of heart failure with preserved ejection fraction51. Furthermore, some PCSK9 loss-of-function variants are associated with altered cardiac functions in humans. However, in experiments that mimicked PCSK9-inhibitor therapy, a complete lack of circulating PCSK9 did not have this effect. This observation provides reassurance that PCSK9 inhibitors do not likely alter cardiac metabolism in humans in a clinically important manner51. One unexpected favorable effect of PCSK9 inhibition is the possible potentiation of the anti-tumor efficacy of immune checkpoint therapy. Like the LDL receptor, PCSK9 can block recycling of major histocompatibility antigen class I (MHC I) to the cell surface by chaperoning it to the lysosome. Experimentally, PCSK9 inhibition raises MHC I expression on cancer cells52. As cytotoxic T cells require interaction with MHC I, this action could boost the ability of CD8+ T cells to lyse tumor cells53.
Newer lipid therapeutics on the horizon
The application of human genetics has identified several newer targets for treating dyslipidemia. These include angiopoietin-like factors 3, 8, and 4 (ANGPTL3, ANGPTL8 and ANGPTL4) and apolipoprotein C3. However, both efficacy and liver-toxicity concerns led to halting the clinical development of vupanorsen, a GalNAc-targeted anti-ANGPTL3 antisense oligonucleotide. Reducing apolipoprotein CIII with olezarsen, a GalNAc-targeted antisense oligonucleotide, yielded dose-dependent reductions in triglycerides and VLDL cholesterol in a phase 2 study54. Although no signal for hepatotoxicity emerged, fewer than 100 individuals were treated with olezarsen in the study. One mechanism of altered lipid metabolism with these newer targets involves regulation of the activity of lipoprotein lipase55. This enzyme, associated with the surface of endothelial cells, can trim fatty acids from triglycerides, promoting the clearance of triglyceride-rich lipoprotein particles, now considered causal in human atherothrombosis. Newer therapeutics involving both antibody neutralization and siRNA or antisense RNA technologies are currently under investigation. Early clinical-trial results have shown very promising effects on the lipid profile of such strategies. Targeting triglycerides or triglyceride-rich lipoproteins could provide additional benefit beyond LDL lowering to optimize cardiovascular outcomes in patients with dyslipidemia.
Management of dyslipidemia in the current era
As noted at the outset of this Review, lifestyle remains the foundation of all cardiovascular prevention, particularly primordial prevention (addressing risk factors early in life) or primary prevention (treating risk factors to prevent disease). After lifestyle, statins remain the bulwark of our therapeutic armamentarium to combat cardiovascular risk due to elevated LDL-C. In individuals intolerant of statins or in whom statin monotherapy does not achieve the desired degree of LDL-C lowering, the addition of ezetimibe and/or bempedoic acid can provide decrements in LDL-C. PCSK9-directed therapeutics remain an additional option for controlling LDL-C, particularly after lifestyle and non-biological approaches have not sufficed to achieve desired LDL-C goals.
Issues that remain in the clinical management of dyslipidemia include statin intolerance and reluctance. Some issues with statins may result from a nocebo effect, but lipid specialists certainly encounter individuals who have genuine statin intolerance. Hence, non-statin LDL-C-lowering agents are additional tools for cardiovascular risk management. Issues of cost and accessibility remain with the proprietary and ethical pharmaceuticals that target dyslipidemia. Moreover, the parenteral administration of some of the newer therapeutic agents versus oral administration of some of the small-molecule agents presents a barrier to some individuals. The development of orally active inhibitors of PCSK9 may provide an option going forward.
The goal of globally equitable access to effective therapies
Despite the great success of the medical enterprise in the rapid development of PCSK9-directed therapeutics, access to these potentially life-saving therapeutics remains limited. The expensive processes that produce the biological agents have led to pricing that represents a challenge to healthcare systems and individuals alike. Multiple guidelines specify target goals for achieving LDL lowering with therapeutics. But achieving such goals currently remains aspirational owing to restricted availability of newer agents. Thus, we should strive to achieve broader and equitable access to such recently developed biological and other therapeutics.
This concern applies not only to wealthier nations, but also to the developing world, regions that bear the greatest overall burden of atherosclerotic risk. Moreover, considerable disparities in access to therapies exist within wealthier nations, as demonstrated poignantly during the COVID-19 pandemic, which affected certain communities and ethnicities disproportionately. A challenge for members of the medical enterprise is working together to assure equitable access to beneficial medications on a global basis. The PEPFAR program provided better access to drugs for treating HIV in developing nations (https://www.hiv.gov/federal-response/pepfar-global-aids/pepfar). We should, as a medical and scientific community, strive to solve the problem of accessibility and assure more equitable access of cardiovascular therapeutics worldwide. Only then will we realize the full benefit of the advances in cardiovascular therapeutics, exemplified by the case of LDL-C and of PCSK9 inhibition in particular. In this regard, despite considerable initial skepticism regarding the efficacy of LDL-C lowering in women, in primary prevention, and in older people, the current clinical trial database supports the use of statins and of ezetimibe in selected individuals in these categories56,57,58.
Discussion
We can derive several important lessons from the saga of LDL biology and the successive development of ever more potent, effective, and acceptable therapeutic measures. This notable victory of cardiovascular medicine reflects successful partnerships between basic scientists, the pharmaceutical and biotechnology sectors, and clinical investigators. The discovery of the role of PCSK9 as the causal gene in autosomal-dominant hypercholesterolemia led rapidly to the development of additional agents to lower LDL-C concentrations and alleviate cardiovascular risk. This achievement required close and concerted cooperation between basic biochemists, human geneticists, cell biologists, the pharmaceutical and biotechnology industries, and clinical trialists. Such cooperation provides a model for paving the way to wielding the powerful palette of contemporary scientific and clinical tools to speed the application of fundamental discoveries to clinical medicine and improvement in patient outcomes and public health.
Challenges remain to surmount. Societies must prioritize efforts to instill healthy lifestyle measures in youth (primordial prevention) and in all stages of the human lifecycle to minimize reliance on pharmacotherapies. We must strive to make the fruits of therapeutic advances affordable and accessible to all who can benefit. Cardiovascular disease has after all become a worldwide epidemic, with the greatest burden of disease in low- and middle-income regions. The application of PCSK9 therapeutics has plumbed the depths of LDL-C achievable in practice. Thus, further lowering of LDL-C beyond that achievable by combinations of current treatments, including PCSK9-blocking strategies, may not yield appreciable increments in cardiovascular benefits19. Hence, we welcome the development and clinical evaluation of orthogonal approaches to cardiovascular-risk reduction, such as targeting other atherogenic lipids or quelling inflammation. We can use biomarkers, including polygenic risk scores, to target individuals at particular risk in primary prevention. We should seek to emulate the advances in cancer therapy afforded by genetically directed allocation of treatments. Cardiovascular risk reduction remains a work in progress. The example of LDL and the latest chapter of harnessing discoveries related to PCSK9 afford a model for moving forward, to furnish further advances in the quest to conquer cardiovascular diseases.
Change history
23 June 2022
In the version of this article initially published, in the last sentence of the “LDL lowering beyond statins” section, the text now reading “Obicetrapib, a potent CETP inhibitor, can lower LDL-C by about 50%” originally read “5%” in the HTML version of the article. This technical error has been amended in the HTML version of this article.
References
Lindgren, F. T., Elliott, H. A. & Gofman, J. W. The ultracentrifugal characterization and isolation of human blood lipids and lipoproteins, with applications to the study of atherosclerosis. J. Phys. Colloid Chem. 55, 80–93 (1951).
Goldstein, J. L. & Brown, M. S. A century of cholesterol and coronaries: from plaques to genes to statins. Cell 161, 161–172 (2015).
Innerarity, T. L. et al. Familial defective apolipoprotein B-100: low density lipoproteins with abnormal receptor binding. Proc. Natl Acad. Sci. USA 84, 6919–6923 (1987).
Wilund, K. R. et al. Molecular mechanisms of autosomal recessive hypercholesterolemia. Hum. Mol. Genet. 11, 3019–3030 (2002).
Sánchez-Hernández, R. M. et al. Autosomal recessive hypercholesterolemia in Spain. Atherosclerosis 269, 1–5 (2018).
Aragam, K. G. & Natarajan, P. Polygenic scores to assess atherosclerotic cardiovascular disease risk. Circ. Res. 126, 1159–1177 (2020).
Müller, C. Xanthomata, hypercholesterolemia, angina pectoris. Acta Med. Scand. 95, 75–84 (1938).
Collaboration, C. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174 000 participants in 27 randomised trials. Lancet 385, 1397–1405 (2015).
The lipid research clinics coronary primary prevention trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. J. Am. Med. Assoc. 251, 365–374 (1984).
The lipid research clinics coronary primary prevention trial results. I. Reduction in incidence of coronary heart disease. J. Am. Med. Assoc. 251, 351–364 (1984).
Oliver, M. F. Serum cholesterol—the knave of hearts and the joker. Lancet 2, 1090–1095 (1981).
Moore, T. J. The cholesterol myth. The Atlantic Monthly 264, 37–70 (1989).
Oliver, M. F. Might treatment of hypercholesterolaemia increase non-cardiac mortality? Lancet 337, 1529–1531 (1991).
Endo, A., Kuroda, M. & Tanzawa, K. Competitive inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase by ML-236A and ML-236B fungal metabolites, having hypocholesterolemic activity. FEBS Lett. 72, 323–326 (1976).
Group, S. S. S. S. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandanavian Simvastatin Survival Study (4S). Lancet 344, 1383–1389 (1994).
Collins, R. et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 388, 2532–2561 (2016).
Altmann, S. W. et al. Niemann-Pick C1 like 1 protein is critical for intestinal cholesterol absorption. Science 303, 1201–1204 (2004).
Cannon, C. P. et al. Ezetimibe added to statin therapy after acute coronary syndromes. N. Engl. J. Med. 372, 2387–2397 (2015).
Laufs, U., Descamps, O. S., Catapano, A. L. & Packard, C. J. Understanding IMPROVE-IT and the cardinal role of LDL-C lowering in CVD prevention. Eur. Heart J. 35, 1996–2000 (2014).
Pinkosky, S. L. et al. Liver-specific ATP-citrate lyase inhibition by bempedoic acid decreases LDL-C and attenuates atherosclerosis. Nat. Commun. 7, 13457 (2016).
Nicholls, S. J. et al. Rationale and design of the CLEAR-outcomes trial: evaluating the effect of bempedoic acid on cardiovascular events in patients with statin intolerance. Am. Heart J. 235, 104–112 (2021).
Abifadel, M. et al. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat. Genet. 34, 154–156 (2003).
Cohen, J. et al. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat. Genet. 37, 161–165 (2005).
Seidah, N. G. The PCSK9 discovery, an inactive protease with varied functions in hypercholesterolemia, viral infections, and cancer. J. Lipid Res. 62, 100130 (2021).
Sabatine, M. S. et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 376, 1713–1722 (2017).
Schwartz, G. G. et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N. Engl. J. Med. 379, 2097–2107 (2018).
Ridker, P. M. et al. Lipid-reduction variability and antidrug-antibody formation with bococizumab. N. Engl. J. Med. 376, 1517–1526 (2017).
Mach, F. et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 41, 111–188 (2020).
Nicholls, S. J. et al. Effect of evolocumab on progression of coronary disease in statin-treated patients: The GLAGOV randomized clinical trial. J. Am. Med. Assoc. 316, 2373–2384 (2016).
Gao, F. et al. Effect of alirocumab on coronary plaque in patients with coronary artery disease assessed by optical coherence tomography. Lipids Health Dis. 20, 106 (2021).
Nicholls, S. J. et al. Assessing the impact of PCSK9 inhibition on coronary plaque phenotype with optical coherence tomography: rationale and design of the randomized, placebo-controlled HUYGENS study. Cardiovasc. Diagn. Ther. 11, 120–129 (2021).
Räber, L. et al. Effect of alirocumab added to high-intensity statin therapy on coronary atherosclerosis in patients with acute myocardial infarction. J. Am. Med. Assoc. 327, 1771–1781 (2022).
Oyama, K. et al. Effect of evolocumab on acute arterial events across all vascular territories: results from the FOURIER trial. Eur. Heart J. 42, 4821–4829 (2021).
Cannata, A., Cantoni, S., Sciortino, A., Bruschi, G. & Russo Claudio, F. Mechanical hemolysis complicating transcatheter interventions for valvular heart disease. J. Am. Coll. Cardiol. 77, 2323–2334 (2021).
Ferri, N. et al. Sex-specific predictors of PCSK9 levels in a European population: the IMPROVE study. Atherosclerosis 309, 39–46 (2020).
Biessen, E. A. L. & Berkel, T. J. C. V. N-acetyl galactosamine targeting: paving the way for clinical application of nucleotide medicines in cardiovascular diseases. Arterioscler. Thromb. Vasc. Biol. 41, 2855–2865 (2021).
Ray, K. K. et al. Inclisiran in patients at high cardiovascular risk with elevated LDL cholesterol. N. Engl. J. Med. 376, 1430–1440 (2017).
Tucker, T. J. et al. A series of novel, highly potent, and orally bioavailable next-generation tricyclic peptide PCSK9 inhibitors. J. Med. Chem. 64, 16770–16800 (2021).
Brousseau, M. E. et al. Identification of a PCSK9-LDLR disruptor peptide with in vivo function. Cell Chem. Biol. 29, 249–258(2021).
Hofherr, A. et al. Safety, pharmacokinetics and pharmacodynamics of multiple ascending doses of AZD8233, Targeting PCSK9, in patients with dyslipidemia (Abstract). Circulation 144, A9747 (2022).
Momtazi-Borojeni, A. A., Jaafari, M. R., Afshar, M., Banach, M. & Sahebkar, A. PCSK9 immunization using nanoliposomes: preventive efficacy against hypercholesterolemia and atherosclerosis. Arch. Med. Sci. 17, 1365–1377 (2021).
Zeitlinger, M. et al. A phase I study assessing the safety, tolerability, immunogenicity, and low-density lipoprotein cholesterol-lowering activity of immunotherapeutics targeting PCSK9. Eur. J. Clin. Pharmacol. 77, 1473–1484 (2021).
Musunuru, K. et al. In vivo CRISPR base editing of PCSK9 durably lowers cholesterol in primates. Nature 593, 429–434 (2021).
Rothgangl, T. et al. In vivo adenine base editing of PCSK9 in macaques reduces LDL cholesterol levels. Nat. Biotechnol. 39, 949–957 (2021).
Borén, J. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 41, 2313–2330 (2020).
Ference, B. A. et al. Variation in PCSK9 and HMGCR and risk of cardiovascular disease and diabetes. N. Engl. J. Med. 375, 2144–2153 (2016).
Schmidt, A. F. et al. PCSK9 genetic variants and risk of type 2 diabetes: a mendelian randomisation study. Lancet Diabetes Endocrinol. 5, 97–105 (2016).
SenBanerjee, S. et al. KLF2 is a novel transcriptional regulator of endothelial proinflammatory activation. J. Exp. Med. 199, 1305–1315 (2004).
Wang, C. Y., Liu, P. Y. & Liao, J. K. Pleiotropic effects of statin therapy: molecular mechanisms and clinical results. Trends Mol. Med. 14, 37–44 (2008).
Ridker, P. M. et al. C-reactive protein levels and outcomes after statin therapy. N. Engl. J. Med. 352, 20–28 (2005).
Da Dalt, L. et al. PCSK9 deficiency rewires heart metabolism and drives heart failure with preserved ejection fraction. Eur. Heart J. 42, 3078–3090 (2021).
Liu, X. et al. Inhibition of PCSK9 potentiates immune checkpoint therapy for cancer. Nature 588, 693–698 (2020).
Patrono, C. & Volpe, M. PCSK9 inhibition: not just LDL-cholesterol knock down: a glimmer for cancer. Eur. Heart J. 42, 1130–1131 (2021).
Tardif, J. -C. et al. Apolipoprotein C-III reduction in subjects with moderate hypertriglyceridaemia and at high cardiovascular risk. Eur. Heart J. 43, 1401–1412 (2022).
Tokgözoğlu, L. & Libby, P. The dawn of a new era of lipid-lowering therapies. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehab841 (2022).
Shepherd, J. et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet 360, 1623–1630 (2002).
Ridker, P. M. et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N. Engl. J. Med. 359, 2195–2207 (2008).
Ouchi, Y. et al. Ezetimibe lipid-lowering trial on prevention of atherosclerotic cardiovascular disease in 75 or older (EWTOPIA 75). Circulation 140, 992–1003 (2019).
Ference, B. A. et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38, 2459–247 (2017).
Acknowledgements
P.L. receives funding support from the National Heart, Lung, and Blood Institute (RO1HL134892 and RO1HL163099), the American Heart Association (18CSA34080399), the Fondation Leducq, the RRM Charitable Fund, and the Simard Fund.
Author information
Authors and Affiliations
Contributions
P.L. wrote the initial draft, and L.T. made critical edits and additions. Both authors contributed to generating the figures.
Corresponding author
Ethics declarations
Competing interests
L.T. reports consulting fees from Abbott, Amgen, Bayer, MSD, Mylan, Novartis, Sanofi, and Daiichi-Sankyo; payment or honoraria from Abbott, Janssen, Amgen, Bayer, Daiichi-Sankyo, MSD, Mylan, Novartis, Novo Nordisk, Sanofi, Servier, Pfizer, Recordati Abdi-İbrahim; support for attending meetings for Servier; participation on a data safety monitoring board or advisory board for Abbott, Amgen, Novartis, Sanofi, Daiichi-Sankyo, Mylan, Pfizer. L.T. was the Past President European Atherosclerosis Society and the Past President Turkish Society of Cardiology. P.L. is an unpaid consultant to, or involved in clinical trials for Amgen, AstraZeneca, Baim Institute, Beren Therapeutics, Esperion Therapeutics, Genentech, Kancera, Kowa Pharmaceuticals, Medimmune, Merck, Norvo Nordisk, Novartis, Pfizer, and Sanofi-Regeneron. P.L. is a member of the scientific advisory board for Amgen, Caristo Diagnostics, Cartesian Therapeutics, CSL Behring, DalCor Pharmaceuticals, Dewpoint Therapeutics, Kancera, Kowa Pharmaceuticals, Olatec Therapeutics, Medimmune, Novartis, PlaqueTec, Soley Therapeutics, TenSixteen Bio, and XBiotech, Inc. P.L.’s laboratory has received research funding in the last 2 years from Novartis. P.L. is on the Board of Directors of XBiotech, Inc. P.L. has a financial interest in Xbiotech, a company developing therapeutic human antibodies, and in TenSixteen Bio, a company targeting somatic mosaicism and clonal hematopoiesis of indeterminate potential (CHIP) to discover and develop novel therapeutics to treat age-related diseases. P.L.’s interests were reviewed and are managed by Brigham and Women’s Hospital and Partners HealthCare in accordance with their conflict-of-interest policies.
Peer review
Peer review information
Nature Cardiovascular Research thanks François Mach, Shizuya Yamashita and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Libby, P., Tokgözoğlu, L. Chasing LDL cholesterol to the bottom — PCSK9 in perspective. Nat Cardiovasc Res 1, 554–561 (2022). https://doi.org/10.1038/s44161-022-00085-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44161-022-00085-x