Abstract
Hypertrophic cardiomyopathy (HCM) is a common inherited cardiovascular disease with heterogeneous clinical presentations, governed by multiple molecular mechanisms. Metabolic perturbations underlie most cardiovascular diseases; however, the metabolic alterations and their function in HCM are unknown. Here, we describe the metabolome and lipidome of heart and plasma samples from individuals with and without HCM. Correlation analyses showed strong association between metabolic alterations and cardiac function and prognosis of patients with HCM. Using machine learning we identified metabolite panels as potential HCM diagnostic markers or predictors of survival. Clustering based on metabolome and lipidome of heart enabled stratification of patients with HCM into three subgroups with distinct cardiac function and survival. Integration of metabolomics and proteomics data identified metabolic pathways significantly altered in patients with HCM, with the pentose phosphate pathway and oxidative stress being particularly upregulated. Thus, targeting the pentose phosphate pathway and oxidative stress may serve as potential therapeutic strategies for HCM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
The clinical information of each HCM patient is provided in Supplementary Table 1. The baseline clinical characteristics for DCM and non-HCM controls are included in Supplementary Table 2. As public sharing of the raw genomic data is restricted by the regulation of the Human Genetic Resources Administration of China, detailed results of WES are included in Supplementary Table 3. Raw metabolomics and lipidomics data are included in Supplementary Tables 4–6. The MS proteomics raw data is deposited in the ProteomeXchange Consortium (http://proteomecentral.proteomexchange.org) via the iProX partner repository with dataset identifier PXD032097. Source data are provided with this paper.
Code availability
Codes for data analysis are available at https://github.com/WenminWang15/HCM_Nat-Cardiovasc-Res.
References
Maron, B. J. Clinical course and management of hypertrophic cardiomyopathy. New Engl. J. Med. 379, 655–668 (2018).
Semsarian, C., Ingles, J., Maron, M. S. & Maron, B. J. New perspectives on the prevalence of hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 65, 1249–1254 (2015).
Virani, S. S. et al. Heart disease and stroke statistics 2021 update: a report from the American heart association. Circulation 143, e254–e743 (2021).
Maron, B. J. & Maron, M. S. Hypertrophic cardiomyopathy. Lancet 381, 242–255 (2013).
Sen-Chowdhry, S., Jacoby, D., Moon, J. C. & McKenna, W. J. Update on hypertrophic cardiomyopathy and a guide to the guidelines. Nat. Rev. Cardiol. 13, 651–675 (2016).
Marian, A. J. & Braunwald, E. Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 121, 749–770 (2017).
Alfares, A. A. et al. Results of clinical genetic testing of 2,912 probands with hypertrophic cardiomyopathy: expanded panels offer limited additional sensitivity. Genet. Med. 17, 880–888 (2015).
Frey, N., Luedde, M. & Katus, H. A. Mechanisms of disease: hypertrophic cardiomyopathy. Nat. Rev. Cardiol. 9, 91–100 (2011).
Ormerod, J. O., Frenneaux, M. P. & Sherrid, M. V. Myocardial energy depletion and dynamic systolic dysfunction in hypertrophic cardiomyopathy. Nat. Rev. Cardiol. 13, 677–687 (2016).
Maron, B. J., Maron, M. S., Maron, B. A. & Loscalzo, J. Moving beyond the sarcomere to explain heterogeneity in hypertrophic cardiomyopathy: JACC review topic of the week. J. Am. Coll. Cardiol. 73, 1978–1986 (2019).
Maurizi, N. et al. Clinical course and significance of hypertrophic cardiomyopathy without left ventricular hypertrophy. Circulation 139, 830–833 (2019).
Elliott, P. M. et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 35, 2733–2779 (2014).
Kurilshikov, A. et al. Gut microbial associations to plasma metabolites linked to cardiovascular phenotypes and risk. Circ. Res. 124, 1808–1820 (2019).
Nicholson, G. et al. Human metabolic profiles are stably controlled by genetic and environmental variation. Mol. Syst. Biol. 7, 525 (2011).
Pang, H., Jia, W. & Hu, Z. Emerging applications of metabolomics in clinical pharmacology. Clin. Pharmacol. Ther. 106, 544–556 (2019).
Liang, L., Sun, F., Wang, H. & Hu, Z. Metabolomics, metabolic flux analysis and cancer pharmacology. Pharmacol. Ther. 224, 107827 (2021).
Wishart, D. S. Emerging applications of metabolomics in drug discovery and precision medicine. Nat. Rev. Drug Discov. 15, 473–484 (2016).
Bertero, E. & Maack, C. Metabolic remodelling in heart failure. Nat. Rev. Cardiol. 15, 457–470 (2018).
Ussher, J. R., Elmariah, S., Gerszten, R. E. & Dyck, J. R. The emerging role of metabolomics in the diagnosis and prognosis of cardiovascular disease. J. Am. Coll. Cardiol. 68, 2850–2870 (2016).
Zhu, J. & Thompson, C. B. Metabolic regulation of cell growth and proliferation. Nat. Rev. Mol. Cell Biol. 20, 436–450 (2019).
Davis, J. et al. A tension-based model distinguishes hypertrophic versus dilated cardiomyopathy. Cell 165, 1147–1159 (2016).
Lopaschuk, G. D., Ussher, J. R., Folmes, C. D., Jaswal, J. S. & Stanley, W. C. Myocardial fatty acid metabolism in health and disease. Physiol. Rev. 90, 207–258 (2010).
Madeo, F., Eisenberg, T., Pietrocola, F. & Kroemer, G. Spermidine in health and disease. Science 359, eaan2788 (2018).
Percudani, R. & Peracchi, A. A genomic overview of pyridoxal-phosphate-dependent enzymes. EMBO Rep. 4, 850–854 (2003).
Marian, A. J., Senthil, V., Chen, S. N. & Lombardi, R. Antifibrotic effects of antioxidant N-acetylcysteine in a mouse model of human hypertrophic cardiomyopathy mutation. J. Am. Coll. Cardiol. 47, 827–834 (2006).
Lombardi, R. et al. Resolution of established cardiac hypertrophy and fibrosis and prevention of systolic dysfunction in a transgenic rabbit model of human cardiomyopathy through thiol-sensitive mechanisms. Circulation 119, 1398–1407 (2009).
Gibb, A. A. & Hill, B. G. Metabolic coordination of physiological and pathological cardiac remodeling. Circ. Res. 123, 107–128 (2018).
Ritterhoff, J. & Tian, R. Metabolism in cardiomyopathy: every substrate matters. Cardiovasc. Res. 113, 411–421 (2017).
Ritterhoff, J. et al. Metabolic remodeling promotes cardiac hypertrophy by directing glucose to aspartate biosynthesis. Circ. Res. 126, 182–196 (2020).
Dyar, K. A. et al. Atlas of circadian metabolism reveals system-wide coordination and communication between clocks. Cell 174, 1571–1585 (2018).
Gottlieb, E. & Tomlinson, I. P. Mitochondrial tumour suppressors: a genetic and biochemical update. Nat. Rev. Cancer 5, 857–866 (2005).
Hilvo, M. et al. Development and validation of a ceramide- and phospholipid-based cardiovascular risk estimation score for coronary artery disease patients. Eur. Heart J. 41, 371–380 (2020).
Nordestgaard, B. G. & Varbo, A. Triglycerides and cardiovascular disease. Lancet 384, 626–635 (2014).
Russo, S. B. et al. Ceramide synthase 5 mediates lipid-induced autophagy and hypertrophy in cardiomyocytes. J. Clin. Invest. 122, 3919–3930 (2012).
Haq, S. et al. Deletion of cytosolic phospholipase A2 promotes striated muscle growth. Nat. Med. 9, 944–951 (2003).
Ommen, S. R. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 142, e533–e557 (2020).
Heggermont, W. A. et al. Inhibition of MicroRNA-146a and overexpression of its target dihydrolipoyl succinyltransferase protect against pressure overload-induced cardiac hypertrophy and dysfunction. Circulation 136, 747–761 (2017).
Li, Q. et al. PKM1 exerts critical roles in cardiac remodeling under pressure overload in the heart. Circulation 144, 712–727 (2021).
Stanley, W. C., Recchia, F. A. & Lopaschuk, G. D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 85, 1093–1129 (2005).
Huang, J. M., Xian, H. & Bacaner, M. Long-chain fatty acids activate calcium channels in ventricular myocytes. PNAS 89, 6452–6456 (1992).
Stincone, A. et al. The return of metabolism: biochemistry and physiology of the pentose phosphate pathway. Biol. Rev. Camb. Philos. Soc. 90, 927–963 (2015).
Dimitrow, P. P., Undas, A., Wołkow, P., Tracz, W. & Dubiel, J. S. Enhanced oxidative stress in hypertrophic cardiomyopathy. Pharmacol. Rep. 61, 491–495 (2009).
McGarrah, R. W., Crown, S. B., Zhang, G. F., Shah, S. H. & Newgard, C. B. Cardiovascular metabolomics. Circ. Res. 122, 1238–1258 (2018).
Taegtmeyer, H. et al. Assessing cardiac metabolism: a scientific statement from the American Heart Association. Circ. Res. 118, 1659–1701 (2016).
Murashige, D. et al. Comprehensive quantification of fuel use by the failing and nonfailing human heart. Science 370, 364–368 (2020).
Lionetti, V., Stanley, W. C. & Recchia, F. A. Modulating fatty acid oxidation in heart failure. Cardiovasc. Res. 90, 202–209 (2011).
Carracedo, A., Cantley, L. C. & Pandolfi, P. P. Cancer metabolism: fatty acid oxidation in the limelight. Nat. Rev. Cancer 13, 227–232 (2013).
Abozguia, K. et al. Metabolic modulator perhexiline corrects energy deficiency and improves exercise capacity in symptomatic hypertrophic cardiomyopathy. Circulation 122, 1562–1569 (2010).
Liao, R. et al. Cardiac-specific overexpression of GLUT1 prevents the development of heart failure attributable to pressure overload in mice. Circulation 106, 2125–2131 (2002).
Shao, D. et al. Glucose promotes cell growth by suppressing branched-chain amino acid degradation. Nat. Commun. 9, 2935 (2018).
Umbarawan, Y. et al. Glucose is preferentially utilized for biomass synthesis in pressure-overloaded hearts: evidence from fatty acid-binding protein-4 and -5 knockout mice. Cardiovasc. Res. 114, 1132–1144 (2018).
Rajasekaran, N. S. et al. Human αB-crystallin mutation causes oxido-reductive stress and protein aggregation cardiomyopathy in mice. Cell 130, 427–439 (2007).
Contrepois, K. et al. Molecular choreography of acute exercise. Cell 181, 1112–1130 (2020).
Rhee, E. P. et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J. Clin. Invest. 121, 1402–1411 (2011).
Stegemann, C. et al. Lipidomics profiling and risk of cardiovascular disease in the prospective population-based Bruneck study. Circulation 129, 1821–1831 (2014).
Schwartz, P. J. et al. Inherited cardiac arrhythmias. Nat. Rev. Dis. Primers. 6, 58 (2020).
Gong, Y. et al. Metabolic-pathway-based subtyping of triple-negative breast cancer reveals potential therapeutic targets. Cell Metab. 33, 51–64 (2021).
Hakimi, A. A. et al. An integrated metabolic atlas of clear cell renal cell carcinoma. Cancer Cell 29, 104–116 (2016).
Landstrom, A. P. & Ackerman, M. J. Mutation type is not clinically useful in predicting prognosis in hypertrophic cardiomyopathy. Circulation. 122, 2441–2449 (2010).
Ball, W. et al. Long-term survival in patients with resting obstructive hypertrophic cardiomyopathy comparison of conservative versus invasive treatment. J. Am. Coll. Cardiol. 58, 2313–2321 (2011).
Gersh, B. J. et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation 124, 2761–2796 (2011).
Wu, G. et al. Variant spectrum of formin homology 2 domain-containing 3 gene in chinese patients with hypertrophic cardiomyopathy. J. Am. Heart Assoc. 10, e018236 (2021).
Wang, J. et al. Malignant effects of multiple rare variants in sarcomere genes on the prognosis of patients with hypertrophic cardiomyopathy. Eur. J. Heart Fail. 16, 950–957 (2014).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Sarafian, M. H. et al. Objective set of criteria for optimization of sample preparation procedures for ultra-high throughput untargeted blood plasma lipid profiling by ultra performance liquid chromatography–mass spectrometry. Anal. Chem. 86, 5766–5774 (2014).
Huang, F. et al. Inosine monophosphate dehydrogenase dependence in a subset of small cell lung cancers. Cell Metab. 28, 369–382 (2018).
Xiao, N. et al. Integrated cytokine and metabolite analysis reveals immunometabolic reprogramming in COVID-19 patients with therapeutic implications. Nat. Commun. 12, 1618 (2021).
Han, J., Gagnon, S., Eckle, T. & Borchers, C. H. Metabolomic analysis of key central carbon metabolism carboxylic acids as their 3-nitrophenylhydrazones by UPLC/ESI-MS. Electrophoresis 34, 2891–2900 (2013).
Meng, X. et al. Simultaneous 3-nitrophenylhydrazine derivatization strategy of carbonyl, carboxyl and phosphoryl submetabolome for LC–MS/MS-based targeted metabolomics with improved sensitivity and coverage. Anal. Chem. 93, 10075–10083 (2021).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. Omics 16, 284–287 (2012).
Rohart, F., Gautier, B., Singh, A. & KA, L. C. mixOmics: an R package for ‘omics feature selection and multiple data integration. PLoS Comput. Biol. 13, e1005752 (2017).
Shannon, P. et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 13, 2498–2504 (2003).
Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. B Methodol. 58, 267–288 (1996).
Breiman, L. Random forests. Mach. Learn. 45, 5–32 (2001).
Ishwaran, H., Kogalur, U. B., Blackstone, E. H. & Lauer, M. S. Random survival forests. Ann. Appl. Stat. 2, 841-860 (2008).
Wilkerson, M. D. & Hayes, D. N. ConsensusClusterPlus: a class discovery tool with confidence assessments and item tracking. Bioinformatics 26, 1572–1573 (2010).
van Heesch, S. et al. The translational landscape of the human heart. Cell 178, 242–260 (2019).
Nie, M. et al. Evolutionary metabolic landscape from preneoplasia to invasive lung adenocarcinoma. Nat. Commun. 12, 6479 (2021).
Acknowledgements
We thank the members of the Hu laboratory for critiquing the manuscript and N. Xiao, J. Li, B. Peng, S. Mao and T. Xu for their helpful discussion. This study is supported by grants from the National Natural Science Foundation of China (32150024, 92057209) (received by Z.H.), (81870286) (received by L.S.), the CAMS Fund for Young Talents of Medical Science (2018RC310006) (received by J.W.), the CAMS Innovation Fund for Medical Sciences (CAMS-2020-I2M-C&T-A-006) (received by L.S.), National Key R&D Program of China (2020YFA0803300) (received by Z.H.), and Tsinghua-Peking Center for Life Sciences, Beijing Frontier Research Center for Biological Structure (received by Z.H.).
Author information
Authors and Affiliations
Contributions
W.W. and Z.H. designed the study and wrote the manuscript. W.W. performed data analyses, data integration and western blot experiments. K.Y. and W.W. performed targeted metabolomics experiments and data processing. K.Y. and J.X. performed lipidomics experiments and data processing. J.W., G.W. and M.L. performed WES and proteomics experiments. M.N., Y.Z., B.W., H.P. and P.L. assisted in data interpretation and manuscript editing. N.T., C.Q., Y.L., Q.S., X.W., D.J., J.W., G.W., S.W. and L.S. provided clinical samples and information. Y.Z., H.P., X,L., D.L. and T.Y. performed machine learning. Z.H. conceived and supervised the project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cardiovascular Research thanks Nicholas Larson and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CMR image of HCM and quality assessments for metabolomics and lipidomics data.
a, Representative cardiovascular magnetic resonance (CMR) images of non-HCM (Ctrl) and patients with HCM. The white arrow indicates the maximum thickness of cardiac interventricular septum. LA, left atrium; LV, left ventricular; RA, right atrium; RV, right ventricular. Bar: 20 mm. b, Principal component analysis (PCA) across omics assay. Each sample is colored by batch information. c–e, Coefficient of variation for metabolites detected by targeted metabolomics in cardiac tissues (n = 44) (c) and plasma (n = 22) (d) and lipidomics (for TAG, n = 30; for other lipid classes, n = 59) (e) of quality control samples. The box plots visualized as median and 25th and 75th percentiles, with whiskers indicating maximal and minimal values.
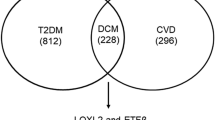
Extended Data Fig. 2 Overview of metabolomics data in the heart tissues from patients with HCM, related to Fig. 2.
a, Heatmap of metabolites relative abundance in non-HCM controls (Ctrl), HCM and DCM patients. b, PCA score plot of targeted metabolomics data on non-HCM controls, HCM and DCM patients. c, Venn diagram depicting the number of upregulated (left) and downregulated (right) metabolites in HCM and DCM group. d, Log2 fold change of differential metabolites in the HCM (x axis) or DCM (y axis) compared to non-HCM controls. e, Relative intensity of metabolites involved in TCA cycle in non-HCM controls (n = 16), HCM (n = 349) and DCM patients (n = 46). The box plots visualized as median and 25th and 75th percentiles, with whiskers indicating maximal and minimal values. f, Heatmap of spearman correlation coefficient of differential metabolites between HCM patients and non-HCM controls. Only pair metabolites with P value < 0.05 were colored and spearman correlation coefficient are labeled in the relevant box. g, Spearman correlation networks of differential metabolites with absolute correlation coefficient greater than 0.5. The solid line represents positive correlation and the dash line represents negative correlation. Statistical analyses were performed by two-sided Mann–Whitney U-test (e). (exact P values are provided in the source data). Asterisks indicate significance as follows: ns P ≥ 0.05, *P < 0.05, **P < 0.01.
Extended Data Fig. 3 Overview of lipidomics data in the heart tissues from HCM patients, related to Fig. 3.
a, PLS-DA score plot of lipidomics data on HCM patients and non-HCM controls (Ctrl). b-d, Volcano plots of sphingolipids (b), glycerophospholipids (c) and neutral lipids (d) alterations between HCM and non-HCM controls. Significantly upregulated, downregulated (FDR-corrected P value < 0.05, fold change > 1.5 or < 0.67) and unchanged metabolites were colored in red, blue, and gray, respectively. Top 10 most significantly increased or decreased metabolites of fold change in each group are labeled. The horizontal line denotes a FDR cutoff of 0.05, and the vertical lines denote a fold change of 1.5 or 0.67. e, Relative intensity of PG, PI and PS in HCM (n = 349) and non-HCM controls (n = 16). The box plots visualized as median and 25th and 75th percentiles, with whiskers indicating maximal and minimal values. f, Fold change of TAG with different numbers of carbon between HCM and non-HCM controls. Statistical analyses were performed by two-sided Mann–Whitney U-test (e) and followed by Benjamini–Hochberg correction (b-d).
Extended Data Fig. 4 Metabolic alterations in the plasma of HCM patients, related to Fig. 4.
a, Heatmap of metabolites relative abundance in the plasma of non-HCM controls (Ctrl) and HCM patients. b, PCA score plot of metabolomics data on the plasma of HCM patients and non-HCM controls. c, Venn diagram depicting the number of plasma and tissue differential metabolites between HCM and non-HCM controls group.
Extended Data Fig. 5 Metabolic subtyping of HCM and their associations with clinical characteristics, related to Fig. 6.
a, b, Groups were identified based on metabolomics data of HCM cohort by K-means consensus clustering upon their abundance. Consensus results show consistency for k = 2 (a) and k = 4 (b), the abundance of TAGs was defined as the ratio of each TAG to total TAG abundance in each patient. c, Cumulative distribution function (CDF) plot of consensus clustering for HCM patients metabolomics data. d, Delta area (change in CDF area) plot of consensus clustering for HCM patients metabolomics data. e, f, The distribution of HCM patients with different NYHA class (e) and MWT (f) in each individual metabolic subtype. g, h, Kaplan–Meier curves for overall survival of HCM patients stratified by the relative intensity of isocitrate, fumarate (g), Uracil, GMP, dUMP and R5P (h) (two-sided log-rank test with no multiple comparisons adjustment). The median of metabolite abundances as the cutoff for expression dichotomization. i, j, Subgroups were identified based on lipidomics data of HCM cohort by K-means consensus clustering upon their abundance. Consensus results show consistency for k = 2 (i) and k = 4 (j). k, CDF plot of consensus clustering for HCM patients lipidomics data. l, Delta area (change in CDF area) plot of consensus clustering for HCM patients lipidomics data. m, n, The distribution of clinical parameters: NYHA class (m) and MWT (n) in each individual metabolic cluster. o, Bubble plot of significance between TAGs with different numbers of carbon and overall survival. Each dot represents a lipid species. Color coded per TAG with different numbers of carbon. Dot size indicates significance. The abundance of TAGs was defined as the ratio of each TAG to total TAG abundance in each patient. A two-sided log-rank test was used with no multiple comparisons adjustment. p, Kaplan–Meier curves for overall survival of HCM patients stratified by the relative intensity of HexCer d18:1/22:2 (two-sided log-rank test). The median of metabolite abundances as the cutoff for expression dichotomization.
Supplementary information
Supplementary Information
Description of Additional supplementary files, Supplementary Fig. 1
Source data
Source Data Fig. 1
Statistical Source Data.
Source Data Fig. 2
Statistical Source Data.
Source Data Fig. 3
Statistical Source Data.
Source Data Fig. 4
Statistical Source Data.
Source Data Fig. 5
Statistical Source Data.
Source Data Fig. 6
Statistical Source Data.
Source Data Fig. 7
Unprocessed western blots.
Source Data Extended Data Fig. 1
Statistical Source Data.
Source Data Extended Data Fig. 2
Statistical Source Data.
Source Data Extended Data Fig. 3
Statistical Source Data.
Source Data Extended Data Fig. 4
Statistical Source Data.
Source Data Extended Data Fig. 5
Statistical Source Data.
Rights and permissions
About this article
Cite this article
Wang, W., Wang, J., Yao, K. et al. Metabolic characterization of hypertrophic cardiomyopathy in human heart. Nat Cardiovasc Res 1, 445–461 (2022). https://doi.org/10.1038/s44161-022-00057-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44161-022-00057-1
This article is cited by
-
Metabolomic machine learning predictor for diagnosis and prognosis of gastric cancer
Nature Communications (2024)
-
Characterization of the circulating transcriptome expression profile and identification of novel miRNA biomarkers in hypertrophic cardiomyopathy
European Journal of Medical Research (2023)