Abstract
Only a minority of patients derive long-term clinical benefit from anti-programmed cell death protein 1 (anti-PD-1) or anti-programmed death-ligand 1 (anti-PD-L1) monoclonal antibodies. The presence of tertiary lymphoid structures (TLSs) has been associated with improved survival in several tumor types. Here, using a large-scale retrospective analysis of three independent cohorts of patients with cancer who were treated with anti-PD-1 or anti-PD-L1 antibodies, we show that the presence of mature TLSs was associated with improved objective response rates, progression-free survival and overall survival, independent of PD-L1 expression status and CD8+ T cell density. These results pave the way for using TLS detection to select patients who are more likely to benefit from immune checkpoint blockade.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets that support the findings of this study are not publicly available due to information that could compromise research participant consent. According to French/European regulations, any re-use of the data must be approved by the ethics committee. Each request for access to the dataset (including the images) will be granted after a request sent to the corresponding author (A.I.) and approval by the ethics committee. Source data are provided with this paper.
References
Vaddepally, R. K., Kharel, P., Pandey, R., Garje, R. & Chandra, A. B. Review of indications of FDA-approved immune checkpoint inhibitors per NCCN guidelines with the level of evidence. Cancers (Basel). 12, 738 (2020).
Davis, A. A. & Patel, V. G. The role of PD-L1 expression as a predictive biomarker: an analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors. J. Immunother. Cancer 7, 278 (2019).
Cassetta, L. & Kitamura, T. Targeting tumor-associated macrophages as a potential strategy to enhance the response to immune checkpoint inhibitors. Front. Cell Dev. Biol. 6, 38 (2018).
Schalper, K. A. et al. Elevated serum interleukin-8 is associated with enhanced intratumor neutrophils and reduced clinical benefit of immune-checkpoint inhibitors. Nat. Med. 26, 688–692 (2020).
Sautès-Fridman, C., Petitprez, F., Calderaro, J. & Fridman, W. H. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat. Rev. Cancer 19, 307–325 (2019).
Ladányi, A. et al. Prognostic impact of B-cell density in cutaneous melanoma. Cancer Immunol. Immunother. 60, 1729–1738 (2011).
Messina, J. L. et al. 12-Chemokine gene signature identifies lymph node-like structures in melanoma: potential for patient selection for immunotherapy? Sci. Rep. 2, 765 (2012).
Goc, J. et al. Dendritic cells in tumor-associated tertiary lymphoid structures signal a TH1 cytotoxic immune contexture and license the positive prognostic value of infiltrating CD8+ T cells. Cancer Res. 74, 705–715 (2014).
Behr, D. S. et al. Prognostic value of immune cell infiltration, tertiary lymphoid structures and PD-L1 expression in Merkel cell carcinomas. Int. J. Clin. Exp. Pathol. 7, 7610–7621 (2014).
Caro, G. D. et al. Occurrence of tertiary lymphoid tissue is associated with T-cell infiltration and predicts better prognosis in early-stage colorectal cancers. Clin. Cancer Res. 20, 2147–2158 (2014).
Petitprez, F. et al. B cells are associated with survival and immunotherapy response in sarcoma. Nature 577, 556–560 (2020).
Cabrita, R. et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature 577, 561–565 (2020).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Tsou, P., Katayama, H., Ostrin, E. J. & Hanash, S. M. The emerging role of B cells in tumor immunity. Cancer Res. 76, 5597–5601 (2016).
Bruno, T. C. New predictors for immunotherapy responses sharpen our view of the tumour microenvironment. Nature 577, 474–476 (2020).
Kroeger, D. R., Milne, K. & Nelson, B. H. Tumor-Infiltrating plasma cells are associated with tertiary lymphoid structures, cytolytic T-cell responses, and superior prognosis in ovarian cancer. Clin Cancer Res. 22, 3005–3015 (2016).
Germain, C. et al. Presence of B cells in tertiary lymphoid structures is associated with a protective immunity in patients with lung cancer. Am. J. Respir. Crit. Care Med. 189, 832–844 (2014).
Montfort, A. et al. A strong B-cell response is part of the immune landscape in human high-grade serous ovarian metastases. Clin. Cancer Res. 23, 250–262 (2017).
Kalergis, A. M. & Ravetch, J. V. Inducing tumor immunity through the selective engagement of activating Fcγ receptors on dendritic cells. J. Exp. Med. 195, 1653–1659 (2002).
Fridman, W. H. et al. B cells and cancer: To B or not to B? J. Exp. Med. 218, e20200851 (2020).
Lu, Y. et al. Complement signals determine opposite effects of B cells in chemotherapy-induced immunity. Cell 180, 1081–1097 (2020).
Schwartz, L. H. et al. RECIST 1.1—update and clarification: from the RECIST committee. Eur. J. Cancer 62, 132–137 (2016).
Vigliar, E. et al. PD-L1 expression on routine samples of non-small cell lung cancer: results and critical issues from a 1-year experience of a centralised laboratory. J. Clin. Pathol. 72, 412–417 (2019).
Balar, A. V. et al. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): a multicentre, single-arm, phase 2 study. Lancet Oncol. 18, 1483–1492 (2017).
Koeppel, F. et al. Added value of whole-exome and transcriptome sequencing for clinical molecular screenings of advanced cancer patients with solid tumors. Cancer J. 24, 153–162 (2018).
Acknowledgements
This study was funded by AstraZeneca.
Author information
Authors and Affiliations
Contributions
A.I., A. Bessede, W.H.F. and F.L.L. conceived of and designed the study. L.V. and F.L.L. performed the histological analyses. S.C., S.L.M., I.S., M.T., G.R., S.P., M.C., F.C., C.L., K.B., M.K., F.C., B.B., Y.L., A.M., J.-C.S. and A.I. provided study materials or treated patients. All authors collected and assembled data. A.I., A. Bessede, L.V. and F.L.L. developed the tables and figures. A.I., A. Bessede, M.B., F.L.L., W.H.F. and C.S.-F. conducted the literature search and wrote the manuscript. All authors were involved in the critical review of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
A. Bessede, J.-P.G. and C.R. are employees of ImmuSmol/Explicyte. E.O. and A.S. are employees of AstraZeneca. A.I. received research grants from AstraZeneca, Bayer, Bristol Myers Squibb, Chugai, Merck, MSD, PharmaMar, Novartis and Roche and received personal fees from Epizyme, Bayer, Lilly, Roche and SpringWorks. B.B. received grants from AstraZeneca, Pfizer, Eli Lilly, Onxeo, Bristol Myers Squibb, Inivata, AbbVie, Amgen, Blueprint Medicines, Celgene, GlaxoSmithKline, Ignyta, Ipsen, Merck KGaA, MSD Oncology, Nektar, PharmaMar, Sanofi, Spectrum Pharmaceuticals, Takeda, Tiziana Therapeutics, Cristal Therapeutics, Daiichi Sankyo, Janssen Oncology, OSE Immunotherapeutics, BeiGene, Boehringer Ingelheim, Genentech, Servier and Tolero Pharmaceuticals. Y.L. received grants from Janssen, Sanofi and MSD, personal fees from Janssen, Sanofi, Astellas, Roche, AstraZeneca, Bristol Myers Squibb, Seattle Genetics, MSD, Clovis, Incyte and Pfizer and non-financial support from Astellas, Roche, AstraZeneca, Bristol Myers Squibb, Seattle Genetics and MSD. A.M. received research grants from Merus, Bristol Myers Squibb, Boehringer Ingelheim, Transgene and MSD and personal fees from Bristol Myers Squibb, AstraZeneca, MedImmune, Oncovir and Merieux. J.-C.S. received consultancy fees from AstraZeneca, Astex, Clovis, GlaxoSmithKline, GamaMabs, Lilly, MSD, Mission Therapeutics, Merus, Pfizer, PharmaMar, Pierre Fabre, Roche/Genentech, Sanofi, Servier, Symphogen and Takeda. L.V., M.B., S.C., S.L.M., M.L., I.S., M.T., G.R., S.P., M.C., F.C., C.L., K.B., M.K., I.G., C.S.-F., V.V., F.C., W.H.F. and F.L.L. declare no competing interests.
Additional information
Peer review information Nature Cancer thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Assessment of the presence of TLS and their maturation stage in tumors.
a: This is a TLS-positive primary pancreatic adenocarcinoma associated with a T CD8 + lymphocyte density of 154/mm² and negative for PD-L1. The TLS are delineated with the black lines on the HES slide, highlighting their vicinity to tumor cells. Scale bar indicates 300 µm in size. Representative of 540 tumors analyzed (Discovery cohort n = 328, validation cohort A n = 131, validation cohort B n = 81). b: This panel shows representative examples of immature and mature TLS observed in tumor samples. Upper panel: This mature TLS is detected in a primary pancreatic adenocarcinoma associated with a T CD8 + lymphocyte density of 154/mm² and negative for PD-L1. Mature TLS are defined by the presence of a network of CD23-positive dendritic cells on immunofluorescence (note that in this case, the presence of a germinal center visible on the HES was already diagnostic of a mature TLS). Lower panel: The picture shows an immature TLS detected in a primary adenocarcinoma of the lung concomitantly showing a high T CD8 + lymphocyte infiltrate of 372/mm² and a PD-L1 TPS score of 1%. The tumor was only associated with immature TLS displaying no germinal center and no network of CD23-positive dendritic cells on immunofluorescence. Representative of 540 tumors analyzed (Discovery cohort n = 328, validation cohort A n = 131, validation cohort B n = 81). The pictures from the left to right column correspond to 1) Hematoxylin Eosin Saffron (HES) staining, 2) Double immunohistochemistry staining of CD3/CD20 (CD3 in brown, CD20 in purple), 3) Double immunohistochemistry staining of CD8/PD-L1 (CD8 in brown, PD-L1 in purple), 4) Multiplex immunofluorescence assay of CD4 (blue), CD8 (yellow), CD20 (orange), CD21 (green) and CD23 (pink). The scale bars on the HES images indicate 50 µm and 100 µm for the upper and lower panels, respectively. Black cropped arrows highlight the tumor cells in the samples.
Extended Data Fig. 2 Predictive value of TLS status according to CPS PD-L1 scores.
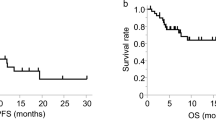
Objective response rates (OR: objective response, SD: stable disease; PD: progressive disease; chi squared (χ²) test) and Kaplan-Meier curves of progression-free survival (log-rank test) and overall survival (log-rank test) of 328 cancer patients treated with anti-PD1/PD-L1 antagonists according to CPS PD-L1 scores (a: CPS PD-L1 < 1, N = 223 patients; b: CPS PD-L1 ≥ 1, N = 105 patients) and TLS status (red curve: mature-TLS positive tumors; blue line: mature-TLS negative tumors).
Extended Data Fig. 3 Predictive value of TLS status according to T CD8 cell density.
Objective Response rates (OR: objective response, SD: stable disease, PD: progressive disease; chi squared (χ²) test) and Kaplan-Meier curves of progression-free (log-rank test) and overall survival (log-rank test) of 328 cancer patients treated with anti-PD1/PD-L1 antagonists according to T CD8 + cell density (a: low density, N = 165 patients; b: high density, N = 163 patients) and TLS status (red curve: mature-TLS positive tumors; blue line: mature-TLS negative tumors).
Extended Data Fig. 4 Outcome of cancer patients (non-small cell lung cancer excluded) according to TLS status.
a) Objective Response rates (OR: objective response, SD: stable disease, PD: progressive disease; chi squared (χ²) test) and Kaplan-Meier curves (log-rank test) of progression-free (b) and overall survival (c) of 201 cancer patients (all tumor types except non-small cell lung cancer) treated with anti-PD1/PD-L1 antagonists according to TLS status (red curve: mature-TLS positive tumors; blue line: mature-TLS negative tumors).
Extended Data Fig. 5 Comparison of the TLS screening with pathology and immunohistochemistry pathology versus the screening with immunofluorescence (method by Petitprez et al).
First line: conspicuous mature TLS with CD23 + follicular dendritic cells network. Second line: mature TLS defined by isolated CD23 + cell displaying dendritic morphology. Pictures from the left to right column correspond to 1) Hematoxylin Eosin Saffron (HES) staining, 2) Multiplex immunofluorescence assay of CD23 (pink) and CD20 (orange), 3) Double immunohistochemistry staining of CD23/CD20 (CD23 in brown, CD20 in red). The scale bars on the HES images indicate 50 µm in size. Representative of 540 tumors analyzed (Discovery cohort n = 328, validation cohort A n = 131, validation cohort B n = 81).
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2.
Supplementary Tables
Supplementary Tables 3–5.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Rights and permissions
About this article
Cite this article
Vanhersecke, L., Brunet, M., Guégan, JP. et al. Mature tertiary lymphoid structures predict immune checkpoint inhibitor efficacy in solid tumors independently of PD-L1 expression. Nat Cancer 2, 794–802 (2021). https://doi.org/10.1038/s43018-021-00232-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-021-00232-6
This article is cited by
-
Enhancing immune responses of ESC-based TAA cancer vaccines with a novel OMV delivery system
Journal of Nanobiotechnology (2024)
-
Reshaping the tumor microenvironment of cold soft-tissue sarcomas with oncolytic viral therapy: a phase 2 trial of intratumoral JX-594 combined with avelumab and low-dose cyclophosphamide
Molecular Cancer (2024)
-
Single-cell sequencing reveals the heterogeneity of B cells and tertiary lymphoid structures in muscle-invasive bladder cancer
Journal of Translational Medicine (2024)
-
Tertiary lymphoid structural heterogeneity determines tumour immunity and prospects for clinical application
Molecular Cancer (2024)
-
Deciphering the correlation between metabolic activity through 18F-FDG-PET/CT and immune landscape in soft-tissue sarcomas: an insight from the NEOSARCOMICS study
Biomarker Research (2024)