Abstract
Immune checkpoint inhibitors have significantly improved the prognosis in patients with non-small cell lung cancer, compared with cytotoxic agents. However, the prediction of treatment response is often difficult, even after assessing the tumor programmed death-ligand 1 expression. We conducted this observational study to analyze the association between the differentiation of peripheral CD4 + T cells and the efficacy of immune checkpoint inhibitor therapy. We enrolled patients who were diagnosed with non-small cell lung cancer and received immune checkpoint inhibitor therapy between 2020 and 2022. Blood samples were collected at the start of immune checkpoint inhibitor therapy, and the expressions of PD-1, CCR7, and CD45RA in peripheral CD4 + T cells were analyzed by flow cytometry. The association between the findings of flow cytometry and survival after the initiation of the immune checkpoint inhibitor therapy was evaluated. Forty patients with non-small cell lung cancer were enrolled. The Cox proportional hazards model showed that an increased proportion of CD45RA-CD4 + T cells was associated with a reduced risk of progression after adjustment for performance status, tumor programmed death-ligand 1 expression level, mutation status of the epidermal growth factor receptor gene, and combined therapy with cytotoxic agents. The present study showed that the proportion of peripheral CD45RA- CD4 + T cells was associated with progression-free survival after the initiation of immune checkpoint inhibitor therapy, independent of several clinical factors.
Similar content being viewed by others
Introduction
Systemic therapy with a cytotoxic agent has been the standard treatment for advanced non-small cell lung cancer (NSCLC) with negative driver mutations. In a phase III trial comparing the effectiveness of cisplatin plus pemetrexed versus cisplatin plus gemcitabine in NSCLC, the 2-year survival rates were 18.9% and 14.0%, respectively1. However, immune checkpoint inhibitors (ICI) have conferred longer survival. Combination therapy with pembrolizumab and cytotoxic agents showed a 2-year survival rate of 45.7% in NSCLC2. Furthermore, pembrolizumab monotherapy demonstrated a 5-year survival rate of 31.9% in NSCLC patients with strong tumor programmed death-ligand 1 (PD-L1) expression3.
Tumor PD-L1 expression is related to the therapeutic efficacy of ICIs, with higher survival rates observed in patients with strong PD-L1 expression. However, early progression is observed even in patients with positive PD-L1 expression4, while some patients with negative PD-L1 expression show long-term survival5. Tumor PD-L1 expression is reported to be heterogeneous in tumor tissue, and it might be modified by treatment exposure, in addition to being caused by multiple mechanisms6. Moreover, it is problematic that tissue samples are required for the evaluation of PD-L1 expression. Therefore, investigation for biomarkers that complement tumor PD-L1 expression is underway. Peripheral immune cells are one of them, including lymphocytes7,8,9,10,11, monocytes12, and eosinophils13.
We previously reported that the proportion of peripheral PD-1 + CD4 + T cells evaluated within 1 week after the initiation of ICIs is associated with progression-free survival (PFS)14. Furthermore, previous studies have reported that peripheral PD-1 + CD4 + T lymphocytes might correspond to effector memory T cells15,16. Thus, we believe that T-cell differentiation, classified as naive T cells, effector memory T cells, central memory T cells, and effector T cells, is associated with the efficacy of ICI therapy. For example, Zuazo M et al. reported that differentiated CD4 + T cells in peripheral blood, defined as CD27-CD28-CD4 + T cells, were associated with longer PFS after the initiation of ICIs in patients with NSCLC.
We conducted this observational study to analyze the association between the differentiation of CD4 + T cells, including naive, effector memory, central memory, and effector T cells, in the peripheral blood of patients with NSCLC and the efficacy of ICI therapy.
Methods
Patients
Patients diagnosed with NSCLC and receiving ICI therapy at Toyama University Hospital between 2020 and 2022 were prospectively enrolled in this study. Selection criteria were established as follows: (1) Patients who were cytologically or histologically diagnosed with NSCLC, including adenocarcinoma or squamous cell lung cancer; (2) Patients who were eligible for systemic therapy and would receive ICI therapy, including ICI monotherapy or combination therapy with cytotoxic anticancer agents. Patients who had been treated with ICI therapy before the study period were also eligible. However, patients diagnosed with neuroendocrine cancer, sarcomatoid carcinoma, or poorly differentiated NSCLC were excluded.
Clinical examinations and treatments
The evaluation of driver gene mutation and the tumor PD-L1 expression was commissioned to commercial laboratories, and the information were retrieved from medical charts. The absence or existence of driver gene mutation was evaluated by PCR, immunohistostaining, or next-generation sequencing, and the PD-L1 tumor proportion score (TPS) was assessed using the 22C3 antibody. Clinical information, including age, performance status (PS), disease stage, and the neutrophil–lymphocyte ratio (NLR) at the initiation of the treatment with ICIs, were assessed. The disease stage was re-staged based on the most recent imaging examination before the treatment. Therapeutic regimens, withdrawal, and discontinuation of the treatment were determined by clinical judgment. Disease progression was defined as either tumor growth or newly emerging lesions according to the Response Evaluation Criteria outlined in Solid Tumors version 1.1 or based on clinical judgment of exacerbation.
Flow cytometry
Peripheral blood was collected at the initiation of ICI therapy. The antibodies used in this study were anti-CD3-Fluorescein isothiocyanate (clone HIT3a), anti-CD4-allophycocyanin/Cy7 (clone A161A1), anti-PD1 (CD279)-phycoerythrin/Cy7 (clone EH12.2H7), anti-CCR7-PE (clone G043H7), and anti-CD45RA-APC (clone HI100) (BioLegend, San Diego, CA, USA). Flow cytometry was contracted to SRL Inc (Tokyo, Japan), performed using whole blood.
Statistical analysis
The endpoints of this study were PFS and overall survival (OS), after the initiation of ICI therapy. PFS events were defined as progression or death and were censored at the date of the last visit or the start of the next treatment without any events. The OS event was death and was censored at the date of the last visit without death. Survival analysis was performed after a 3-month observation period from the last patient enrollment.
Patients were subdivided according to the median of the proportion of each subset against CD3 + CD4 + T cells, including CCR7 + CD45RA + CD4 + T cells (naive T cells), CD45RA-CD4 + T cells (memory T cells), CCR7 + CD45RA-CD4 + T cells (central memory T cells), CCR7-CD45RA-CD4 + T cells (effector memory T cells), and CCR7-CD45RA + CD4 + T cells (effector T cells). The cutoff value of the NLR was set at 5, based on previous reports17.
Survival among the subdivided patient groups was analyzed by univariate analysis using the log-rank test and multivariate analysis using the Cox proportional hazard model, adjusting for PS, PD-L1 expression level, epidermal growth factor receptor (EGFR) mutation status, and combined therapy with cytotoxic agents. Fisher's exact test was used to test the nominal scale. A p-value of less than 0.05 was considered significant. Statistical analysis was performed using JMP version 15.0.0 (SAS, Cary, USA).
Ethical approval
This study was conducted in compliance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects (Ministry of Health, Labour and Welfare, Japan), with the approval of the Ethics Committee, University of Toyama (approval number: R2020042).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Results
Patient characteristics
A total of the 40 patients were enrolled. PD-L1 TPS was confirmed as < 1%, 1–49%, and ≥ 50% in 11 (27.5%), 18 (45.0%), and 10 (25.0%) patients, respectively. The EGFR mutation was detected in 6 patients, and 3 of them were treated with EGFR-TKIs before the treatment with ICIs. The KRAS mutation was detected in 5 patients, who were treated with ICIs as a first-line treatment (Table 1).
Survival
The median (95% confidence interval, CI) of PFS after the initiation of ICI therapy in 40 patients was 6.3 months (2.3–12.2 months), and the median (95% CI) of OS was 19.0 months (7.7–not estimated). PFS and OS events were observed in 25 and 14 patients, respectively (Fig. 1).
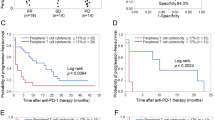
Representative flow cytometry plots of T cells according to CD3-CD4, PD-1, and CD45RA-CCR7 expression profiles are shown in Fig. 2. No significant association was found among the proportion of PD-1, CCR7, or CD45RA expression in peripheral blood CD4 + T cells and survival (Table 2 and Table 3). Then, a subset analysis was performed according to the tumor PD-L1 expression level. Only the proportion of CD45RA-CD4 + T cells was associated with PFS in each group classified according to tumor PD-L1 expression level. Patients with a higher proportion of CD45RA-CD4 + T cells (≥ 30%) showed longer PFS times in the subsets with tumor PD-L1 TPS of ≥ 50% (median, not reached vs. 15.8 months, p = 0.167, log-rank test) and < 50% (median, 6.2 months vs. 1.5 months, p = 0.001, log-rank test), respectively (Fig. 3). Therefore, we analyzed the association of the proportion of CD45RA-CD4 + T cells with survival by multivariate analysis using the Cox proportional hazard model. Cox proportional hazard model for PFS adjusting for PS, PD-L1 TPS, EGFR mutation status and combined therapy with cytotoxic agents showed that the proportion of CD45RA-CD4 + T cells was significantly associated with a reduced risk of progression (Table 4, hazard ratio: 0.18, 95% CI: 0.04–0.78).
Figure 4 shows Kaplan–Meier curves for PFS and OS after the initiation of ICI therapy in patient groups classified according to the tumor PD-L1 expression level and proportion of the CD45RA-CD4 + T cells. Those with a higher proportion of CD45RA-CD4 + T cells (≥ 30%) showed longer PFS and OS times than those with a lower proportion, in each group classified according to tumor PD-L1 expression level.
Association with clinical parameters
Table 5 shows a comparison of patient characteristics and the proportion of CD45RA-CD4 + T cells. The proportion of CD45RA-CD4 + T cells was significantly higher (≥ 30%) in the patients who received ICI therapy as a first-line treatment.
Discussion
The present study showed that the proportion of CD45RA-CD4 + T cells was associated with PFS after the start of ICI therapy, independent of several clinical background factors, indicating that peripheral CD4 memory T cells are associated with the efficacy of ICIs for treating NSCLC patients.
In the tumor microenvironment, CD8 + T cells are associated with the elimination of cancer cells, and it has been reported that tumor-infiltrating CD8 + T cells are associated with the efficacy of ICI therapy18,19. On the other hand, from the studies investigating peripheral immune cells, several authors have reported the association between CD4 + T cells and the efficacy of ICI therapy8,9,10,11, while the association with CD8 + T cells was also reported20,21. Furthermore, it was recently reported that CD4 + T cells in the tumor microenvironment are also associated with longer survival after the initiation of ICIs22. Given that CD4 + T cells play an important role in the differentiation and activation of CD8 + T cells under the support of dendritic cells23, they might be involved in the efficacy of ICIs.
The findings of the present study suggested the contribution of memory CD4 + T cells to the efficacy of ICI therapy. Similar results have been previously reported. Kagamu H et al. reported that CD62Llow T cells were related to the response to ICI therapy. Low expression of CD62L, a homing receptor, indicates the presence of antigen-primed T cells. The percentage of CD62LlowCD4 + T cells was also significantly correlated with the percentage of effector memory T lymphocytes that are identified as CCR7-CD45RA-8. Zuazo M et al.9 reported that highly differentiated CD4 + T cells, defined as CD27-CD28- in peripheral blood, were associated with PFS after the initiation of ICIs and that the majority of these T cells were central memory (CD45RA-CD62L +) or effector memory T cells (CD45RA-CD62L-). Iwahori et al. reported that peripheral blood T-cell cytotoxicity is an independent prognostic factor for PFS and that peripheral T-cell toxicity is correlated with the ratio of the effector memory population in CD4 + or CD8 + T cells24. Miao et al.10 reported that CD45RA-CD4 + T cells were associated with PFS in patients with NSCLC who received ICI therapy. Notably, memory T cells are thought to be necessary for long-term immunological memory and possibly for lasting response25. These reports on the association between CD4 memory T cells and the efficacy of ICI therapy suggest that the existence of antigen-primed CD4 T cells is related to the efficacy of ICIs. However, Zuazo M reported that the proportions of CD4 T cells that were reactive to A549 cell antigens were not significantly different between differentiated and non-differentiated T-cell groups9.
We previously reported that the proportion of PD-1 + CD4 + T cells evaluated within 1 week after initiation of ICIs was associated with the efficacy of ICIs. These findings were similar to those reported by Waki K et al.15 and Santegoets et al.26; however, no such relationship was observed in the present study. In the previous study, we obtained peripheral blood after ICI administration in 17 (89.5%) patients, but herein, it was obtained before the treatment in 37 (92.5%) patients. Du W et al. reported that responders to ICIs showed an increase in PD-1 + CD4 + T cells after one cycle of ICI therapy27. These findings suggest that an increase of PD-1 + CD4 + T cells after the initiation of ICI administration, but not at baseline, might be associated with the response to ICI therapy.
There are several limitations in the present study, and the findings should be interpreted with caution. First, the sample size was small, which may raise the issue of generalizability. Second, even if the peripheral memory CD4 + or differentiated CD4 + T cells are important for the efficacy of ICIs, it remains unclear whether CD45RA is the optimal marker for its evaluation. Furthermore, the optimal cutoff value for CD45RA-CD4 + T cells cannot be determined in the present study. Finally, although some clinical factors were adjusted by multivariate analysis, the patient backgrounds and treatments were not well balanced among the groups.
In summary, the present study suggested that peripheral CD4 + memory T cells, defined as CD45RA-CD4 + , are independently associated with PFS after the initiation of treatment with ICIs.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Scagliotti, G. V. et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J. Clin. Oncol. 26, 3543–3551 (2008).
Rodriguez-Abreu, D. et al. Pemetrexed plus platinum with or without pembrolizumab in patients with previously untreated metastatic nonsquamous NSCLC: Protocol-specified final analysis from KEYNOTE-189. Ann. Oncol. 32, 881–895 (2021).
Reck, M. et al. Five-year outcomes with pembrolizumab versus chemotherapy for metastatic non-small-cell lung cancer with PD-L1 tumor proportion score ≥ 50. J. Clin. Oncol. 39, 2339–2349 (2021).
Herbst, R. S. et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): A randomised controlled trial. Lancet 387, 1540–1550 (2016).
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373, 1627–1639 (2015).
Prelaj, A. et al. Predictive biomarkers of response for immune checkpoint inhibitors in non-small-cell lung cancer. Eur. J. Cancer 106, 144–159 (2019).
Manjarrez-Orduño, N. et al. Circulating T Cell subpopulations correlate with immune responses at the tumor site and clinical response to PD1 inhibition in non-small cell lung cancer. Front. Immunol. 9, 1613 (2018).
Kagamu, H. et al. CD4(+) T-cell immunity in the peripheral blood correlates with response to anti-PD-1 therapy. Cancer Immunol. Res. 8, 334–344 (2020).
Zuazo, M. et al. Functional systemic CD4 immunity is required for clinical responses to PD-L1/PD-1 blockade therapy. EMBO Mol. Med. 11, e10293 (2019).
Miao, K. et al. Peripheral blood lymphocyte subsets predict the efficacy of immune checkpoint inhibitors in non-small cell lung cancer. Front Immunol. 13, 912180 (2022).
Yamaguchi, O. et al. Establishing a whole blood CD4(+) T cell immunity measurement to predict response to anti-PD-1. BMC Cancer 22, 1325 (2022).
Ando, K. et al. A high number of PD-L1(+) CD14(+) monocytes in peripheral blood is correlated with shorter survival in patients receiving immune checkpoint inhibitors. Cancer Immunol. Immunother. 70, 337–348 (2021).
Osawa, H. et al. Absolute increase in the number and proportion of peripheral eosinophils associated with immune checkpoint inhibitor treatment in non-small cell lung cancer patients. Cancer Diagn. Progn. 1, 485–490 (2021).
Inomata, M. et al. Peripheral PD1-positive CD4 T-lymphocyte count can predict progression-free survival in patients with non-small cell lung cancer receiving immune checkpoint inhibitor. Anticancer Res. 39, 6887–6893 (2019).
Waki, K. et al. PD-1 expression on peripheral blood T-cell subsets correlates with prognosis in non-small cell lung cancer. Cancer Sci. 105, 1229–1235 (2014).
Duraiswamy, J. et al. Phenotype, function, and gene expression profiles of programmed death-1(hi) CD8 T cells in healthy human adults. J Immunol. 186, 4200–4212 (2011).
Jin, J., Yang, L., Liu, D. & Li, W. Association of the neutrophil to lymphocyte ratio and clinical outcomes in patients with lung cancer receiving immunotherapy: a meta-analysis. BMJ Open 10, e035031 (2020).
Spassova, I. et al. Clinical and molecular characteristics associated with response to therapeutic PD-1/PD-L1 inhibition in advanced Merkel cell carcinoma. J. Immunother. Cancer 10, e003198 (2022).
Lopez de Rodas, M. et al. Role of tumor infiltrating lymphocytes and spatial immune heterogeneity in sensitivity to PD-1 axis blockers in non-small cell lung cancer. J. Immunother. Cancer 10, e004440 (2022).
Dronca, R. S. et al. T cell Bim levels reflect responses to anti-PD-1 cancer therapy. JCI Insight https://doi.org/10.1172/jci.insight.86014 (2016).
Wistuba-Hamprecht, K. et al. Peripheral CD8 effector-memory type 1 T-cells correlate with outcome in ipilimumab-treated stage IV melanoma patients. Eur. J. Cancer 73, 61–70 (2017).
Kaira, K. et al. Prognostic significance of tumor infiltrating lymphocytes on first-line pembrolizumab efficacy in advanced non-small cell lung cancer. Discov. Oncol. 14, 6 (2023).
Burbage, M. & Amigorena, S. A dendritic cell multitasks to tackle cancer. Nature 584, 533–534 (2020).
Iwahori, K. et al. Peripheral T cell cytotoxicity predicts the efficacy of anti-PD-1 therapy for advanced non-small cell lung cancer patients. Sci. Rep. 12, 17461 (2022).
Jenkins, R. W., Barbie, D. A. & Flaherty, K. T. Mechanisms of resistance to immune checkpoint inhibitors. Br. J. Cancer 118, 9–16 (2018).
Santegoets, S. J. et al. T cell profiling reveals high CD4+CTLA-4 + T cell frequency as dominant predictor for survival after prostate GVAX/ipilimumab treatment. Cancer Immunol. Immunother. 62, 245–256 (2013).
Du, W. et al. Dynamic testing of stimulative and suppressive biomarkers on peripheral blood cells at early stages of immunotherapy predicts response in advanced cancer patients. Discov. Med. 25, 277–290 (2018).
Funding
This work was supported by grants from Nippon Boehringer Ingelheim Co.
Author information
Authors and Affiliations
Contributions
MI designed the study and wrote the main manuscript. MM, NT, KH, ZS, TH, KT (Kotaro Tokui), CT, SO, KK, SI, TM, RH, and SM contributed to the data collection and investigation. KT (Kazuyuki Tobe) supervised the study. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Inomata, M., Matsumoto, M., Takata, N. et al. Peripheral CD4 memory T cells predict the efficacy of immune checkpoint inhibitor therapy in patients with non-small cell lung cancer. Sci Rep 13, 10807 (2023). https://doi.org/10.1038/s41598-023-37736-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-37736-3
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.