Abstract
Assessing gastrointestinal motility lacks simultaneous evaluation of intraluminal pressure (ILP), circular muscle (CM) and longitudinal muscle (LM) contraction, and lumen emptying. In this study, a sophisticated machine was developed that synchronized real-time recordings to quantify the intricate interplay between CM and LM contractions, and their timings for volume changes using high-resolution cameras with machine learning capability, the ILP using pressure transducers and droplet discharge (DD) using droplet counters. Results revealed four distinct phases, BPhase, NPhase, DPhase, and APhase, distinguished by pressure wave amplitudes. Fluid filling impacted LM strength and contraction frequency initially, followed by CM contraction affecting ILP, volume, and the extent of anterograde, retrograde, and segmental contractions during these phases that result in short or long duration DD. This comprehensive analysis sheds light on peristalsis mechanisms, understand their sequence and how one parameter influenced the other, offering insights for managing peristalsis by regulating smooth muscle contractions.
Similar content being viewed by others
Introduction
The complex and intricate motility patterns of the gastrointestinal (GI) tract facilitate the proximal to distal movement of ingested food1,2. Peristalsis and segmentation are two distinct forms of motility that facilitate in thorough mixing, digesting, absorbing, and final excreting of foodstuffs3,4,5. Peristalsis involves involuntary contractions of both circular muscle (CM) and longitudinal muscle (LM) layers, propelling chyme from oral to aboral direction. In contrast, segmental contractions driven by CM facilitate food mixing3,5,6. The coordinated actions between CM and LM is key for proper food propulsion, and any disruption can lead to GI motility disorders7.
GI motility disorders refer to conditions that affect the normal movement of food or digesta through the digestive tract and can affect any part of the GI tract from the esophagus to the anus. The underlying cause may often be considered as unknown or multifactorial, involving a combination of genetic, environmental and lifestyle factors. Although the underlying mechanisms and complex interplay of factors involved in GI motility have been explained in previous studies7,8,9,10, the management of GI motility disorders is still complicated by an incomplete understanding of the precise mechanisms coordinating GI smooth muscle activity, which are necessary for proper bowel emptying.
Our collective understanding of mechanisms underlying gut motility has improved exponentially from new, innovative ex vivo and in vivo approaches to study GI motility, including: (1) high resolution manometry, which records pressure changes at various locations in the intestine; (2) spatiotemporal mapping, which allows analysis of CM and LM contractions; (3) fluoroscopy and MRI, which provide real-time imaging of gut contractions; and (4) in vivo quantification of electrolyte and fluid flux using a number of experimental techniques9,10,11,12,13,14. Due to technical limitations, however, all these parameters have not heretofore been studied simultaneously. Doing so would be a major scientific advance since it would allow comprehensive assessment of how CM and LM work together to appropriately modulate intraluminal pressure changes, anterograde, segmental and retrograde contractions to result in droplet discharge (DD).
The research described in this communication was designed to conceptualize and develop a sophisticated machine that integrates multiple components and subsystems to allow comprehensive analysis of gut motility. One major goal was to be able to accurately quantify the intricate interplay between CM and LM movements, as well as the precise timing of their contractions for resultant DD. In achieving this goal, we hoped to improve the understanding of how numerous physiological factors such as intraluminal pressure (ILP), peristalsis, segmental and longitudinal contractions, absorptive or secretory state of the intestine, and DD at the aboral end work in tandem to maintain GI motility. This knowledge could ultimately lead to the development of novel therapeutic approaches for GI motility disorders.
Results
Droplet discharge primarily occurred in D phase or A phase
In the “Short-D group” [SD; short duration droplet discharge occurring in the “During Phase” (phase during high amplitude pressure waves; DPhase)], the DDs occurred during the DPhase lasting 0.16 to 0.63 min (range) with an experimental DD duration divided by standard DD mean (D/Ds) of 0.85 ± 0.05. The “Long-A group” [LA; long duration droplet discharge occurring in “After Phase” (phase after high amplitude pressure waves; APhase)] exhibited significantly longer duration (range: 0.64–0.98 min), with a D/Ds of 1.09 ± 0.05 (range: 0.98–1.8). LA group exhibited longer durations compared to SD group. Similarly, the “Long-D group” (LD; long duration droplet discharge occurring in DPhase) group had all phases longer than SD (range: 0.68–0.81 min) and a significant D/Ds increase (1.24 ± 0.04, p < 0.001). LD’s DPhase was longer than LA (0.27 ± 0.02 min vs. 0.33 ± 0.05 min; p = NS). These three discharge groups represent distinct lumen filling stages.
Pressure contraction strength changes during four phases in SD, LA and LD groups
Comparing phases across discharge groups, LA showed a higher pressure contraction strength (Ps; amplitude of pressure contraction) in the “Before Phase” (BPhase; phase before the high amplitude pressure waves) compared to SD and LD with significant difference in SD (0.12 ± 0.01 cmH2O vs. 0.22 ± 0.02 cmH2O, p < 0.001; Table 1). Ps change between phases was smaller in LA compared to SD and LD. Results suggested substantial Ps increase coincided with both DPhase and APhase fluid discharges. LA group’s fluid discharge featured a relatively modest Ps increase. Nonetheless, whether Ps of DPhase alone accounted for DD duration remained unclear.
Gross pressure contraction changes during four phases in SD, LA and LD groups
Gross pressure contraction’s (Pg; mean pressure changes between two adjacent phases) influence on DD was examined by analyzing its changes between phases (Table 1). In SD group, Pg significantly increased from BPhase to “Near Phase” (NPhase; phase near high amplitude pressure waves, after BPhase), and from NPhase to DPhase followed by a decrease from DPhase to APhase. Maximum increase occurred from NPhase to DPhase (0.05 ± 0.01 cmH2O vs. 0.27 ± 0.06 cmH2O; p < 0.02, n = 18). The decrease in Pg from DPhase to APhase was significant compared to BPhase to NPhase and NPhase to DPhase (−0.28 ± 0.06 cmH2O; p < 0.001, n = 18). This study revealed an association between DD in DPhase and high Pg from NPhase to DPhase.
Comparing BPhase to NPhase and DPhase to APhase, SD (p < 0.04) and LD (p < 0.002) groups had significantly higher Pg than LA. Pg significantly decreased in all three DD groups in DPhase to APhase. Despite significant pressure changes between phases, LA’s Pg remained small, potentially contributing to longer durations between discharges. However, this observation did not fully explain LD discharges at relatively higher Pg than LA group. Consequently, Pg increase could only account for DPhase discharges and not discharge duration.
Gross longitudinal movement changes during four phases in SD, LA and LD groups
The magnitude by which LM moved from the oral end during BPhase to DPhase (0.20 + 0.14 mm) was ~ equal to the distance moved from DPhase to APhase (−0.33 ± 0.06 mm) toward the aboral end.
Although gross longitudinal movement changes (Lg; mean longitudinal movement between two adjacent phases) increased from NPhase to DPhase and rapidly decreased from DPhase to APhase, the LD showed no significant differences between BPhase to NPhase, NPhase to DPhase and DPhase to APhase (Table 1).
In LA group, Lg was lower in all three phases, with significant reduction in BPhase to NPhase and DPhase to APhase compared to SD group, suggesting reduced LM contraction. Similarly, LD group exhibited lower Lg in BPhase to NPhase and DPhase to APhase compared to SD group (Table 2). However, LD group showed no significant difference between phases and notably less aboral movement compared to SD group (−0.07 ± 0.06 mm vs. −0.33 ± 0.06 mm; p < 0.02). LD group also showed minor aboral movement in BPhase to NPhase compared to different phases (p = NS). Reduced LM movement toward both oral and /or aboral ends in LA and LD groups might contribute to the longer duration of these DDs.
Longitudinal contraction strength changes during four phases in SD, LA and LD groups
In the SD group, the longitudinal contraction strength (Ls; amplitude of longitudinal contractions) progressively increased from BPhase to DPhase, then declined in APhase. In SD group, Ls in DPhase was significantly higher compared to both BPhase and APhase. Conversely, LA group showed no significant differences in Ls between phases. In LA group, Ls in DPhase was significantly lower compared to SD group. LA group displayed small non-significant differences in Ls between phases. Conversely, in LD group, Ls in DPhase was significantly higher compared to SD group. Although LD generally had higher Ls, it lacked significant phase distinctions, potentially contributing to increased DD duration. Furthermore in LD group, Ls was significantly higher compared to LA group in all phases except BPhase (Table 1).
Gross volume and volume strength changes during four phases in SD, LA and LD groups
In the SD and LA groups, intestinal gross volume (Vg; mean volume changes between two adjacent phases) decreased marginally from BPhase to NPhase and NPhase to DPhase. SD group showed a significant volume drop from NPhase to DPhase, unlike LA group. SD group showed significantly increased volume in DPhase to APhase (Table 1). Conversely, LA group displayed minimal changes, with an increase from NPhase to DPhase followed by a slight decrease in DPhase to APhase. This suggests delayed fluid filling and emptying in LA compared to SD group. LD exhibited non-significant volume increments between phases unlike SD group. This explains the delayed lumen filling and prolonged duration of DD in LD group. Taking all phases together, SD (9.99 ± 0.96 mm3; p < 0.001, n = 72) and LD (14.84 ± 2.35 mm3; p < 0.006, n = 32) exhibited higher volume strength (Vs; amplitude of volume contraction) compared to LA (7.06 ± 0.73 mm3, n = 76). These studies showed that irrespective of contraction phase, LA consistently displayed lower Vs. Phase-related Vs changes for SD, LA and LD showed no significant difference (Table 1).
Gross movement of edge width tracker 1 and 4 changes during four phases in SD, LA and LD groups
Gross movement of edge width tracker 1 (EW1g; mean diameter changes between adjacent phases in edge width tracker 1; EW1) exhibited marginal decrease in BPhase to NPhase followed by a significant decrease in NPhase and DPhase in SD, signifying proximal CM contraction with DD. Conversely, LA and LD had minimal EW1g changes, suggesting DD without significant CM contractions, explaining delayed emptying.
Gross movement of edge width tracker 4 (EW4g; mean diameter changes between adjacent phases in edge width tracker 4; EW4) increased slightly from BPhase to NPhase and, decreased significantly from NPhase to DPhase in SD, implying open lumen becoming closed. A small non-significant increase followed from DPhase to APhase. LA showed smaller insignificant diameter changes. LD displayed a small but significant diameter decrease from BPhase to NPhase compared to NPhase to DPhase, suggesting closed to open lumen transition. The decreased BPhase to NPhase diameter could explain LD duration.
Comparing EW1g and EW4g contractions, a significant diameter decreases in EW1g during NPhase to DPhase suggested proximal contraction with distal CM relaxation. In SD, lumen filling primarily occurred in DPhase to APhase, where EW1g diameter increased compared to EW4g (Table 2). Similar changes were absent in the LA and LD groups, although EW1g showed greater diameter decrease than EW4g.
Changes in proximal and distal edge width contraction strength during four phases in SD, LA and LD groups
In SD, proximal edge width contraction strength (EW1s; amplitude of EW1 contraction) significantly decreased in DPhase compared to BPhase (Table 1). This suggests maximum CM contractions during NPhase to DPhase transition when EW1s was lowest. LA and LD showed stable EW1s with no significant phase differences. LD generally had higher EW1s compared to LA with significance in DPhase. DD in DPhase followed EW1s and EW1g decrease, suggesting a role for proximal CM contraction. Unlike EW1s, mean diameter for all phases was lower in EW4s for SD (0.21 ± 0.01 mm vs. 0.16 ± 0.01 mm; p < 0.002, n = 72) and LD (0.32 ± 0.04 mm vs. 0.23 ± 0.02 mm; p < 0.05, n = 32). In LA, there was no significant difference between EW1s and EW4s. In LA and LD, there was no significant phase differences. In SD, distal edge width contraction strength (EW4s; amplitude of EW4) increased from BPhase to NPhase, decreased in DPhase, and significantly increase in APhase (p < 0.03, n = 18) with maximum EW1s and EW4s decrease occurring in DPhase.
Frequency measurements during different contraction phases and droplet discharge intraluminal pressure wave frequency
Comparing ILP frequency across phases of DD groups showed no significant differences. However, distinct pattern emerged when comparing SD, LA and LD groups (Table 2). Frequency decrease was significant between SD and LA in BPhase (0.74 ± 0.01 Hz vs. 0.69 ± 0.01 Hz; p < 0.02), NPhase (0.73 ± 0.01 Hz vs. 0.66 ± 0.02 Hz; p < 0.001), DPhase (0.72 ± 0.01 Hz vs. 0.66 ± 0.01 Hz; p < 0.003) and APhase (0.76 ± 0.03 Hz vs. 0.67 ± 0.01 Hz; p < 0.001). This suggests that frequency decreases as contraction decreases, akin to LA. Intriguingly, LD exhibited significantly higher frequencies compared to LA in NPhase (0.71 ± 0.02 Hz vs. 0.66 ± 0.02 Hz; p < 0.05) and DPhase (0.70 ± 0.01 Hz vs. 0.66 ± 0.01 Hz; p < 0.04), and were not significantly different from SD group.
Longitudinal tracker frequency analysis
Comparing frequencies of LM contractions within SD, LA and LD phases showed no significant differences (Table 2), suggesting consistent pacemaker activity across discharge group phases. However, overall frequency and mean amplitude analysis using fast Fourier transform (FFT) revealed higher values in SD than LA (Fig. 1a, b). Frequencies between SD and LA phases displayed significantly lower values in LA group across all phases.
a Representative graph showing fast Fourier transform (FFT) of longitudinal trace. The sinusoidal oscillations of longitudinal contractions for a period were divided into distinct frequency components with their respective amplitude. A high-pass filter with a cut off frequency of 0.2 Hz and an amplitude threshold of 0.02 mm was used. Non-linear exponential curve fit using second order polynomial exponent (Exp3P2) was used to trace along the FFT. The graph shows a shift in the frequency to the left for LA (black tracings) compared to SD (gray tracings), suggesting a decrease in frequency in LA. The decrease in frequency was associated with a simultaneous decrease in the amplitude of the contraction. b Comparison of EW1, EW4 and longitudinal frequency within various discharge groups. EW1 and EW4 showed a significant difference in frequencies (Longi) in SD (p < 0.03, n = 18), LA (p < 0.03, n = 19) and LD (p < 0.03, n = 8) discharge groups. Comparing EW1, EW4 and Longi of SD with that of LA showed a significant difference. LA showed significant difference between EW1 and Longi. In LD discharge groups, there was no statistical significance between frequencies for EW and Longi. Significant differences were calculated using Kruskal–Wallis followed by Mann–Whitney test for individual comparison. c Overall frequency comparison between proximal (EW1) and distal edge trackers (EW4) irrespective of the discharge group. Proximal edge tracker have a higher frequency compared to the distal tracker (p < 0.001, n = 48). Significant differences were calculated using one-way ANOVA. d Comparison of net amplitude between EW1 and EW4 for the three discharge groups. Net amplitude was anterograde in BPhase and NPhase in SD, followed by retrograde net movement in DPhase and APhase with a significant difference between NPhase and APhase (p < 0.03, n = 18). In LA, the net amplitude was generally retrograde, with anterograde movement only in DPhase (n = 19). In LD, similar to SD, net amplitude was anterograde in BPhase and NPhase, retrograde movements were seen only in DPhase followed by a small anterograde movement in APhase (n = 8). In LA and LD, there are no significant differences between the phases. Significant differences were calculated using Kruskal–Wallis followed by Mann–Whitney test for individual comparison.
Similarly, LA exhibited significantly lower frequency in all phases compared to the LD group (Table 2). There was no significant difference in longitudinal frequencies between SD and LD phases. In summary, these findings suggest that when the intestinal lumen is mostly empty (LA), the contraction frequencies are lower across all four phases. Conversely, in SD and LD the frequencies are higher across all phases.
Proximal edge width tracker frequency analysis
Comparing frequencies within SD, LA and LD phases of EW1 showed no significant difference. However, significant distinctions emerged between discharge groups. SD exhibited higher frequency compared to LA across all phases (Table 2). Comparing LA and LD, LA displayed significantly lower frequencies in DPhase and APhase. While BPhase and NPhase in LA displayed lower frequencies compared to LD but was not significant. These studies showed that lower frequencies in the LA group aligned with minimal diameter changes between phases (Table 2), suggesting CM contraction frequency has a potential role in fluid discharge dynamics.
Distal edge width tracker frequency analysis
Frequency analyses of SD, LA and LD revealed no significant difference between phases (Table 2). Comparing SD and LA, LA showed significantly lower frequencies in NPhase, DPhase and APhase. Similarly, LA exhibited lower frequencies compared to LD in all phases, with a significant difference in DPhase. However, there were no significant differences in frequency between SD and LD in all four phases.
When comparing overall EW1 and EW4 frequencies, a significantly higher frequency was observed in EW1 (0.71 ± 0.01 Hz vs. 0.67 ± 0.00 Hz; p < 0.001, n = 180; Fig. 1c). This frequency difference was consistent across various phases of the contractions for SD, LA and LD but decreased significantly in LA which prolonged the time for discharge, particularly in EW1, highlighting the significance of proximal contractions in fluid propulsion dynamics.
Additionally, the frequency pattern indicated stronger proximal contractions, favouring anterograde propulsion. Reduced EW4 frequency relative to EW1 could be influenced by the steady oral fluid flow from the peristaltic pump, contrasting with variable fluid flow in aboral end because of pooling and emptying. This differential exposure to fluid flow could affect contraction frequency and strength.
Comparing LM and EW1 frequencies, SD and LD showed no significant difference across phases. In LA, LM frequency significantly decreased compared to EW1 in Nphase (0.65 ± 0.01 Hz vs. 0.69 ± 0.01 Hz; p < 0.04, n = 19) and Aphase (0.62 ± 0.02 Hz vs. 0.67 ± 0.01 Hz; p < 0.04, n = 19).
Anterograde, retrograde, and segmental contractions
SD group
The “net amplitude” increased from BPhase to NPhase (0.05 ± 0.04 mm vs. 0.12 ± 0.02 mm), and declined during DPhase (−0.01 ± 0.05 mm) and APhase (−0.05 ± 0.04 mm) with a significant difference between NPhase and APhase (p < 0.03) (Fig. 1d). This indicates that strong proximal contractions facilitate DD, with anterograde contractions during BPhase to NPhase, while retrograde contractions appeared in DPhase and APhase.
LA group
“Net amplitude” was relatively lower compared to SD. Retrograde contractions were noted in NPhase (−0.03 ± 0.05 mm) and APhase (−0.01 ± 0.02 mm). Low amplitude anterograde movements occurred in BPhase (0.01 ± 0.03 mm) and DPhase (0.07 ± 0.05 mm), without significant differences between the four phases (Fig. 1d).
LD group
LD had larger amplitude contractions than LA. LD exhibited anterograde contractions in all phases except DPhase, marked by retrograde contractions (Fig. 1d), without any significant differences between phases.
Comparing SD, LA, and LD
LA had lower contraction amplitude with a significant difference only in NPhase (0.12 ± 0.02 mm vs. −0.03 ± 0.05 mm; p < 0.004, n = 18 and n = 19, respectively; Fig. 1d) when compared to SD. No significant differences within phases of SD and LD groups were observed.
These findings suggest anterograde contractions precede DD. Variable “net amplitude” between phases in LA and LD discharge groups highlights the complexity of intestinal motility. Strong proximal CM and LM contractions and volume decrease in BPhase to NPhase and NPhase to DPhase are responsible for shorter DD duration, anterograde contraction in SD, while lower amplitude and predominantly retrograde contractions in LA might contribute to longer DD durations.
Discussion
Functional imbalance in GI motility is closely linked to numerous human ailments such as achalasia, dyspepsia, gastroparesis, constipation, IBS, chronic intestinal pseudo-obstruction15. The current understanding of intestinal peristalsis relies on in vitro and in vivo techniques including manometry and spatiotemporal mapping, but each technique has its own limitations9,10. Technical limitations have hindered quantitative analysis of smooth muscle layer movements affecting ILP and DD. In this study, a multi-spectrum image capture system, ILP transducers, Vernier Drop counters and associated proprietary software programs enabled real time acquisition of quantitative data on intestinal motility and DD. Specifically, the technology achieved: (1) Quantification of frequency and amplitude for both, high and low amplitude pressure waves; (2) Continuous monitoring of diameter and volume changes for luminal content accumulation and propulsion; (3) Characterizing intestinal contractions as anterograde, retrograde or segmentation; (4) Establishing “net amplitude” to assess overall contraction strength and direction; (5) Relationship to DD using various motility parameters; and (6) Establishing absorptive or secretory state of the intestine but is not part of this study, as intestinal segments were perfused with ringer solution and exhibited net absorption. Future comparisons between formulations will consider net fluid output, impacting both, motility and, absorption or secretion. Overall, this is an approach that simultaneously uses all these parameters to study the mechanisms of gut motility.
Interstitial cells of Cajal (ICCs) are specialized pacemaker cells that initiate and propagate slow electrical waves regulating smooth muscle contraction frequency in response to force16,17,18. Various ICC types are classified by their GI tract location19. They can be interconnected multipolar cells (myenteric region) or bipolar without interconnections within CM and LM layers17,18,20. ICC communicate directly via gap junctions and chemical signaling18. ICC initiate oscillations, initially synchronized proximally, but increasingly desynchronized aborally17. ICC form networks such as the Myenteric plexus situated between the CM and LM layers, coordinating peristalsis and food propulsion, or the Meissner’s plexus in the submucosa, coordinating local reflexes in response to various GI stimuli, and modulating peristalsis, vasomotor activity, absorption and secretion19.
In this study, CM and LM contractions were referenced to four phases of pressure tracing (BPhase, NPhase, DPhase and APhase) to clarify LM’s role in initiating CM contractions, and the resulting volume and pressure changes leading to DD. In SD group, increased Lg occurs through BPhase, NPhase and DPhase, followed by CM contraction. This could be explained by CM fiber gathering and associated ICC proximity, facilitating signal transmission and contraction. In dog ileum, LM played a crucial role in transmitting electrical signals to CM upon distention21,22. Similarly, findings in human esophagus revealed that LM contractions precede CM contractions, and last longer23,24. EW1 began to contract in BPhase to NPhase, while EW4 continued diameter increase suggesting relative aboral CM relaxation while LM contraction peaked ahead of CM contraction. Maximum increase in ILP followed EW contraction and decreased volume in NPhase to DPhase, rather than LM tracker movement, suggesting ILP changes as a reflection of CM contraction. Similar observations in other studies on intestine and esophagus have shown concurrent contraction and relaxation of CM and LM layers25,26.
In this study, EW4 was associated with a more relaxed state compared to EW1, and this combined with a relatively higher contraction frequency in the proximal regions, favored more anterograde contraction, irrespective of the DD type. Similar observations were made in animal and human showing that GI tract’s distal regions progressively exhibit reduced frequency and contractions27,28,29,30,31. Increased frequency and contraction in proximal segments may be necessary for mixing and propelling digested material in the upper GI tract. The frequency of contractions between LM and EW1 did not significantly differ in SD and LD but showed a significantly lower frequency in LA groups. Similar findings were observed in studies done in human ileal tissue32. This explains the decreased frequency, and LM and CM contractions when the lumen is mostly empty, as fewer stretch reflexes are initiated to stimulate the myenteric plexus (Fig. 2a).
a The illustration shows the entry of artery, veins and nerves from the mesentery through the serosa and the distribution of the myenteric plexus between the longitudinal and circular layers of smooth muscle. The orientation of the myenteric plexus is such that the ganglia (collection of nerve cell bodies) are stretched circumferentially and inter-ganglionic fibers run longitudinally, parallel to the longitudinal muscle fibers to allow transmission of signals and coordination of muscle contractions without exerting excessive traction or tension on the nerve fibers. Meissner’s plexus or submucosal plexus is a network of nerve fibers and ganglia located in the loose connective tissue of the submucosal layer of the GI tract. Receptive nerve endings from Meissner’s plexus projects into the mucosa as intrinsic primary afferent neurons and transmit the signals to submucosal neurons or Myenteric plexus. b Figure showing longitudinal muscle contraction with gathering of circular muscle rings (muscle fibers) toward the distal end that results in contraction with narrowing of the lumen at the aboral end, favouring fluid-filling. Fluid filling leads to ballooning proximal to the contracted region (bold arrows). Intestinal flow is reduced during the filling stage (thin arrow). Arrows within the lumen depicts more retrograde movement. c Figure showing longitudinal muscle contraction (parallel lines) with gathering of circular muscle rings (muscle fibers) and narrowing of the lumen at the proximal end that favors droplet discharge (bold arrows). Arrows within the lumen suggest more anterograde movement. a was created using Sketchbook® App in iPad (7th generation) and imported to Adobe Illustrator version 27.1 (2023) for final adjustments and labeling, while (b, c) were drawn using Adobe Illustrator version 27.1 (2023).
The “net amplitude” displayed more anterograde contractions and fluid emptying when distal tracker contractions lagged the proximal tracker contraction. Segmental contractions with no fluid emptying occurred in the absence of a lag between the two trackers. This is evident in SD group, where BPhase, NPhase and DPhase were anterograde with a significant difference between BPhase and APhase. Fluid accumulated toward the aboral end, leading to droplet formation. Although, DD happened in DPhase or APhase, the fluid accumulation commenced as early as BPhase continuing through NPhase and the early part of DPhase. Eventually, the droplet’s weight overcame cohesive forces, causing DD. Thus, anterograde movements occur during fluid emptying phases and shifted to net retrograde movement during fluid filling phases.
Studies suggest that ICCs decide frequency and character of propagative muscle contractions33. The proximal edge trackers recorded a diameter reduction from BPhase to the end of DPhase, after which the diameter began to increase progressively and peaking in DPhase to APhase. EW4 showed a relatively smaller reduction, indicating less gross contraction. Studies using rat small intestine, showed that proximal CMs were more sensitive to cholinergic drugs and active stress when compared to distal CM contraction34.
The decrease in Pg and Ps during APhase correlated with decreased Lg, signifying LM movement toward the distal end, accompanied by increased Vg and Vs. Following the peak contraction of EW1, LM contracted aborally in DPhase to APhase and APhase, associated with increased EW1, while EW4 showed only a minor increase. During this phase, the intestinal segment volume increased substantially, indicating fluid filling as LM contracts at the aboral end initiating contraction of EW4. Subsequently, LM moved toward the oral end as the volume continued to fill, and CM relaxed. This suggests that LM contraction is vital for initiation of contraction at both, oral and aboral ends. However, to sustain the CM contraction at either end, LM contraction may not be necessary (Fig. 2b, c).
In LD group, proximal LM movement was reduced in NPhase to DPhase compared to SD group but was not significant. EW1 did not show a significant difference between various phases, but was significantly lower compared to SD. These contraction parameters explained the relative retrograde movement observed in DPhase of LD group, and the relatively longer time for DD. Both, LA and LD groups had preceding short duration discharges. LA group had a longer DD duration compared to LD group. Consequently, the LA group had less time to fill the lumen before the next discharge, explaining why LD group had a higher intestinal volume, significantly in DPhase to APhase. In SD, intestinal volume increased, likely activating the stretch reflex for strong contractions. In LA, delayed filling resulted in less stretch reflex activation, manifesting as lower muscular contractions. LD was intermediate with some intestinal volume increase and potentially stronger stretch reflex and muscle contractions than LA, but less than SD.
Current management of GI motility disorders, including IBS aims to alleviate symptoms rather than addressing the root cause35,36. Most constipation drugs work by modifying fluid balance i.e., by decreasing absorption and increasing secretion, thereby increasing the fluid volume in the gut lumen37,38, but they do not address the primary alterations in GI motility. The limited effectiveness in altering the disease’s natural course can be attributed to technical limitations in understanding the complex and simultaneous interactions between ILP, CM and LM contractions and intestinal evacuation. The multi-parameter tracking setup developed in this study overcomes these limitations and gives a quantitative analysis of the complex muscular events governing GI motility and thereby facilitating the development and evaluation of drugs targeting intestine’s natural smooth muscle rhythm to achieve proper bowel evacuation.
Methods
Experimental mouse model
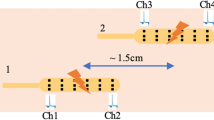
Intestinal peristalsis and DD were studied using jejunal segments from 9–12 week old Swiss Albino male mice. The GI electrophysiology of mice and humans is largely similar and therefore justified their use to study GI motility18. GI motility relies on intricate interactions between extrinsic and intrinsic neural networks, including the pivotal role of ICC and smooth muscle cells39. Intrinsic neuronal plexuses provide autonomous control over GI function, allowing the intestine to operate independently from extrinsic neuronal inputs40,41. This supported the use of isolated intestinal segments in the tissue bath in the present study. All experiments were approved by the University of Florida Institutional Animal Care and Use Committee (IACUC#: 202300000119). Mice were humanely sacrificed by CO2 narcosis followed by cervical dislocation (per American Veterinary Medical Association’s Guidelines for the Euthanasia of Animals). Thereafter, a ~4.5 cm jejunal segment located 12 cm proximal to the cecum was identified, dissected and then mounted in a Mayflower tissue bath (Type 813/6), which is a horizontal water-jacketed chamber (Hugo Sachs Elektronik, Harvard Apparatus, USA), held at 37 °C (Fig. 3a–e). Precise length of the intestinal segments was measured after mounting using a Vernier Calliper, and this information was used by the computer program to accurately calculate the edge width and quantify longitudinal movements. Intraluminal perfusion was achieved using a multi-channel roller pump calibrated to deliver Ringer’s solution at a steady state rate of ~0.065 ml/min (Figs. 3a and 4). Ringer was maintained at 37 °C in a water-jacketed glass buffer reservoir (73-3440; Hugo Sachs Elektronik/Harvard Apparatus, Germany) by passing the solution through a heat exchanger42. The perfusate was passed through a Windkessel (Figs. 3b and 4) to dissipate any pulsatility coming from the roller pumps. A separate multi-channel roller pump was used to superfuse the intestinal segment at a rate of 0.2 ml/min also at 37 °C. The Ringer solution for both perfusion and superfusion was continuously bubbled with 95% O2 and 5% CO2 (carbogen) and maintained at pH 7.4 (Fig. 4). Using this setup, the intestinal segments studied stayed viable for ~ 45 min. During this period, the ILP and volume changes were maintained grossly at a steady level. As the tissue deteriorated in the chamber, there were gross reduction in ILP and increase in volume with time. Therefore, most of the studies were limited to the first 30 min. In this setup, the lumen was filled using a peristaltic pump and an afterload was applied to generate an ILP ranging from 0 to 5 cmH2O column by increasing the height of the luminal efflux tubing (Figs. 3d and 4), as performed in previous studies43,44,45. Each perfusion pressure was maintained for 10 min and the ILP of 1.5 cmH2O was found to have the maximum amplitude pressure waves maintained for the longest period of time. The afterload help exert the mechanical stretch reflex via the enteric nervous system (ENS) that resides within the wall of the GI tract, including intrinsic primary afferent neurons (IPANs), interneurons, and motor neurons to achieve smooth muscle contraction45,46. IPANs are sensory neurons that detect the mechanical, hormonal, or chemical changes in the gut and the interneurons transmit the information to the enteric neural network, while the motor neurons provide the desired muscular activity41. This triggers mechanically a cascade of alterations in the CM and LM frequency, and contraction patterns, ultimately resulting in DD at the aboral end with different duration.
The experimental setup for studying peristalsis: a Lateral view, b Front view. PLUGSYS Transducer Amplifier Modules-A (TAM-A, Harvard apparatus, USA), CVX400 series vision system with multi-spectrum LumiTrax light (Keyence, USA) and infrared-LED sensor drop counters with LabQuest Mini interface (Vernier instruments, USA) are used to measure intraluminal pressure, diameter changes, longitudinal movements, and fluid output in intestinal segments. c Representative image showing jejunal segment mounted in tissue perfusion bath. Jejunal segment with 4 digital edge width (EW) trackers and one PatternTrax placed along the length of the intestine. EW trackers track the diameter change with time. PatternTrax measures the longitudinal movement with time using surface characteristics on the intestine such as blood vessels. d The luminal perfusate passing through the intestinal segments were made to fall through a specified area of the drop-counter so that the LED light falling on the detector is blocked, resulting in the generation of a digital signal that is then captured by a data collection interface. The data are converted into volume and expressed in ml/min by the data acquisition program. e Intestinal segments were perfused in water-jacketed tissue bath (Mayflower, USA). The oral and aboral end of the tissues are connected to the pressure transducers and the pressure recordings obtained were amplified using TAM-A.
The setup involves tissue bath, with units for pressure transducer-amplifier, camera control and droplet discharge sensor-meter. The setup allows for a comprehensive study of intestinal motility capturing movements of the intestinal segment mounted in a perfusion bath using a Keyence camera, multi-spectrum LumiTrax light (MSL) and CV-X400 series controller system. Changes in intraluminal pressure were measured using a pressure transducer and transducer amplifier module (TAM-A) connected to the ports on the tissue bath. A droplet discharge occurring at the aboral end was detected using the infrared-LED sensor drop counter (Vernier Instruments, USA) and metered using LabQuest Mini Interface. Together this setup allows for a comprehensive study of intestinal motility and enhances the understanding of complex biological processes responsible for droplet discharge. The figure was created using Corel Draw, version 21.3.0.755 (2019).
Intraluminal pressure measurements
ILP plays an important role in the movement of luminal content through the intestine, and was recorded in the past using high resolution manometry and pressure transducers connected to the oral and aboral ends. In the current study, the oral and aboral ends of the tissues were connected to two individual pressure ports at the top of the perfusion bath by using Tygon tubing with an inner diameter of 0.79 mm attached to a differential pressure transducer MPX (type 399/2) that uses a monolithic silicon piezoresistor (Hugo Sachs Elektronik/Harvard Apparatus, Germany). The pressure was calibrated after adjusting the water column using the afterload control (Fig. 4). This setup therefore accurately delivers pressure changes occurring in the intestinal segment (PBTO)42. Such a setup does not impede or alter the natural movement of the intestine. The pressure signal from the transducers were amplified using a universal DC bridge amplifier (Transducer Amplifier module (TAM-A) type 705/1 (Hugo Sachs Elektronik/Harvard Apparatus, Germany; Figs. 3b and 4). Four such TAM-A modules were housed within an HSE Plugsys measuring system. The Plugsys apparatus captured signals originating from the isolated intestinal segments mounted in PBTOs, and amplified and continuously recorded every 2 msec, using a Data Acquisition Hardware and Basic data acquisition software (HSE-BDAS; Hugo Sachs Elektronik/Harvard Apparatus, Germany) running on a Windows 10 operating system. A low-pressure afterload of 1.5 cmH2O was applied using a raised water column to simulate intestinal distention during the passage of the food (Figs. 3e and 4). The pressure waves acquired by the BDAS software were too enormous to manually quantify the number of high amplitude waves and their duration. Therefore, a proprietary program, peristalsis.exe47 was used to accurately quantify changes in pressure, frequency, amplitude, strength, and duration of contractions. These pressure parameters were later correlated with peristaltic events such as changes in outer diameter, longitudinal movements of the intestine and DD at the aboral end. Predetermined thresholds were set in the program to differentiate low and high amplitude pressure changes, facilitating analysis of large data sets. Our plan going forward was to use this experimental setup to assess segmental differences in ILP, and CM and LM contractions and their corresponding frequency (Fig. 5a–i), with and without various pharmacological interventions intended to mimic GI motility dysfunction in human disease states.
a The intraluminal pressure (ILP) tracings showing separation into four phases based on Ps, Ls and/or Lg. Lg trace (blue) is obtained by selecting the mean of each Ls. “Before-phase” (BPhase) started with low Lg and Ls, and both progressively increased by the end of the phase. During BPhase, low amplitude pressure waves were observed, and this phase was followed by a phase with increased Ps, called the “near-phase” or NPhase. The NPhase started with a rapid increase in Ps, and during this period Ls progressively increased and reached a peak or plateau marking the end of the NPhase. The NPhase displayed slightly higher Ps when compared to BPhase. The NPhase preceded the high amplitude Ps in “during-phase” (DPhase). Both, Ls and Lg progressively increased and reached a peak from the beginning of the NPhase. The DPhase is the region of the pressure tracing where the highest amplitude contraction waves were observed and was significantly higher when compared to BPhase and NPhase. The DPhase had the longest duration and was followed by “after-phase” (APhase). At the end of the DPhase, Ps, Pg and Lg returned to the base levels and marked the beginning for the APhase. Duration and amplitude (Ps) for Aphase was significantly lower when compared to DPhase but was comparable to that of BPhase. b Representative tracings for SD. The figure shows a significant increase in longitudinal movements (Lg and Ls) from BPhase to Dphase, during which Ps showed a significant increase. DD occurred in DPhase (blue dot). In APhase, Lg and Ls decreased together with a decrease in Ps and Pg. c Representative tracings for LA. The amplitude of Ps, Pg, Ls and Lg were relatively smaller when compared to SD and LD. Lg and Ls increased from BPhase to DPhase and decreased from DPhase to APhase. DD occurred in APhase (blue dots). d Representative tracings for LD. An increase in Lg was observed from NPhase to DPhase but was significantly lower than SD drops. Duration for LA and LD were significantly higher when compared to SD. The decrease in Lg during the Aphase in LD was significantly lower than that observed in SD drops. DD occurred in DPhase. At the end of APhase Lg decreased to the levels observed in Bphase. DD occurred in DPhase (blue dot). Decrease in Lg in Aphase was observed in all DD groups. e Representative pressure trace showing trend over time. ILP maintained steady levels for up to 40 min and thereafter, ILP decreased significantly. Therefore, all subsequent studies were performed within the first 30 min. f Zoomed view from (e) (20–22 min) showing low and high amplitude pressure waves (Ps) with gross pressure changes (Pg). Pressure tracings show high amplitude waves flanked by small rise and fall in pressure strength. g Zoomed view from (f) (21.02–21.1 min) showing crest, trough, amplitude, and wavelength. h Representative traces showing the diameter changes in proximal (EW1) and distal (EW4) tracker with time. Lower values represent decrease in diameter or circular muscle contraction. i Representative trace showing low and high amplitude oscillations (Ls) along the gross longitudinal muscle contraction (Lg). The Lg tracings recorded using PatternTrax are read from left to right, thereby increased values suggest contraction of longitudinal muscles at the proximal end while decreased values suggest contraction at the distal end.
Graphical data obtained using BDAS displayed both low and high amplitude pressure changes (Fig. 5e–g). The frequency of high amplitude contractions in jejunal segments were determined using “Peristalsis.exe”47 while low amplitude contractions were assessed manually. The frequencies of both low and high amplitude contractions were similar and not statistically different within each corresponding intestinal segment (0.69 ± 0.01 Hz vs. 0.69 ± 0.01 Hz; p > 0.05, n = 192). However, there was a significant difference in frequency between the jejunal and ileal segments (0.76 ± 0.01 Hz vs. 0.55 ± 0.01 Hz; p < 0.001, n = 22). This aligns with prior research indicating that the frequency progressively decreases in the distal regions of the GI tract compared to the jejunum30,48. Given the distinct frequency differences in the jejunum and ileum, indicating the involvement of separate pacemaker groups, these segments were individually analyzed to uncover variations in muscular activities responsible for fluid discharge. The present study specifically concentrates on the jejunal gut segment.
ILP recordings between tissues were compared between experiments using “gross pressure” (Pg) and “pressure strength” (Ps). In the detailed pressure recording window of BDAS, we observed multiple high-amplitude pressure waves occurring at irregular intervals (Fig. 5e–g). However, it was unclear how these waves affected Pg. Ps of these waves was calculated as the algebraic sum of individual pressure waves amplitudes (measured from crest to trough) divided by the number of waves. While Pg in the intestinal segments studied were calculated from the measured ILP recordings (Fig. 5e), and mathematically represented as Pg = the sum of pressure recordings taken over the study period divided by the number of recordings taken over the study period. Changes in Pg between phases measured the magnitude of pressure changes without considering the oscillations associated with ILP waves.
Analysis of edge width, volume, longitudinal movement and contraction type
Spatiotemporal mapping has been the most widely used technique to track CM and LM contractions. In this study, to monitor and quantify two-dimensional edge movements for CM and LM contractions in intestinal segments in real-time, we employed an innovative approach utilizing a CV-X400 series vision system. This setup comprised an ultra-high-speed camera (LumiTrax™), multi-spectrum lighting with eight color LEDs, and a dedicated control circuit (Keyence, USA) (Figs. 3a, b and 4). LumiTrax™ employs a novel imaging technique in which the lighting direction and color were automatically synchronized with the camera through machine learning to collect data and quantify real-time changes in both LM (length) and CM contraction (diameter) amplitudes. Multiple images with 24 image enhancement filters and lighting from various directions are taken and analyzed to detect patterns, such as blood vessels or mesentery, on the intestinal surface to optimize real-time visualization and tracking during intestinal movements, even when their orientation changes (Fig. 3c). Build-in “Auto-Teach Inspection Tools” allows the camera to “learn” and identify variations and differences in the pattern that may occur with intestinal contraction in real-time, ensuring stable tracking to obtain quantifiable data acquisition of diameter and longitudinal movements. This capability enables real-time tracking with less noise during data capture. The camera operates with preset configurations, reducing setup time, thus enhancing tissue viability. Both longitudinal and circular movements are captured every 50 msec.
Longitudinal movements are tracked and recorded from the aboral end. The gross longitudinal movements (Lg) tracked using “PatternTrax” helped determine whether LM contractions were oriented toward the oral or aboral end of the intestine. These movements were recorded as a gross shift along the Y-axis (Lg) over time (Figs. 5i and 6a–c) and are calculated by subtracting the mean longitudinal position of each phase from the previous phase. Increased Lg values indicate LM contractions toward the oral end, while decreased values suggest gross LM movement toward the aboral end. Due to slight differences in the length of the intestinal segment studied and the position of the PatternTrax on the intestine, the baseline Lg levels were never exactly the same. Therefore, we normalized the values by subtracting the smallest value from all longitudinal recordings to obtain the absolute distance moved, facilitating comparisons between experiments or different phases of DD. These values reflect the strength of the LM contractions. By comprehensively studying the coordinated roles of LM movements, CM movements, and their influence on ILP changes, we can bridge the existing knowledge gap and gain a deeper understanding of how these factors collectively contribute to the propulsion of luminal contents. LM tracings exhibited both low and high amplitude oscillations with amplitude representing the strength of LM contraction, denoted as Ls, calculated as the algebraic sum of the amplitudes of individual longitudinal waves divided by the number of waves. To understand the role of Ls in determining the duration of DD and how it interacts with Lg, Ls was compared across different phases and DD groups (Fig. 5b–d).
Panel graphs showing traces of factors responsible for droplet discharge duration and segmentation: a SD discharge: in BPhase to NPhase, longitudinal muscles showed maximum values, EW1 and EW4 begins to contract with maximum reduction occurring in the DPhase. Longitudinal muscle contraction at proximal end occurred before circular muscle began to contract. EW1g showed greater contraction when compared to EW4g. Correspondingly, maximum increase in volume was seen in BPhase and thereafter, the volume began to decrease with maximum reduction in the middle of DPhase. Lg, EWg and Vg showed reduction in the DPhase, where Ps was increased. Lg increased from the middle of DPhase and reached a maximum toward the early part of APhase while, EWg and Vg continued to increase through the APhase. Ps decreased during the APhase. b LA discharge: longitudinal muscles showed an increase from BPhase to DPhase and thereafter decreased from the beginning of DPhase and continued into the APhase. EW1 started to contract in BPhase, NPhase and early DPhase, while longitudinal muscle remained in the contracted state at the proximal end. EW1g showed a marginal increase in DPhase and APhase. Unlike EW1g, EW4g contractions were minimal. Volume changes are minimal compared to SD. An increase in volume was observed from NPhase to DPhase, followed by a decrease in APhase. c LD discharge: longitudinal muscle contraction showed a decrease in BPhase to NPhase, unlike SD and LA. EW1g values increased from BPhase to DPhase, suggesting continued filling through BPhase and NPhase, and began to empty only in the DPhase. Unlike SD and LA, in LD, the lumen continued to fill through BPhase and NPhase. EW4g continued to decrease from BPhase to APhase with maximum decrease occurring in BPhase to NPhase. Volume decreased in DPhase and did not return to base levels suggesting incomplete emptying. d Diameter changes between EW1 and EW4 depicting anterograde and retrograde contraction analyzed using “GutCode”. EW1 contraction with EW4 relaxation causes anterograde movement (upward arrow), and EW1 contraction with EW4 relaxation causes retrograde contraction (downward arrow). e Diameter changes between EW1 and EW4 depicting segmental contractions analysed by “GutCode”. Simultaneous contraction or relaxation of EW1 and EW4 causes pure segmental contraction. A small increase in diameter of EW4 compared to EW1 causes segmental forward, and a small decrease in diameter of EW4 compared to EW1 causes segmental backward contractions.
For diameter tracking, we selected opposite edges of the intestine at four regions along its length as edge width (EW) trackers using the CV-X400 series machine vision system. These EW trackers measured changes in the distance between opposite edges during contraction generating a graphical representation of diameter changes. All four pairs of EW trackers were used continuously along the sides of intestinal segment, with adjacent trackers spaced apart by approximately the length of one edge tracker. Contraction was indicated by a decrease in EW (diameter), while relaxation was indicated by an increase. The diameter measurement from the four EW trackers changed with changes in fluid volume in the intestine. The analysis of the gross movement of EW trackers (EWg) depicts the overall diameter change, which is calculated by subtracting the mean diameter in one phase from that of the previous phase. The amplitude of EW contractions at any given time represents the strength of EW contractions (EWs). To ensure that the changes recorded by “GutCode” accurately represented the actual variations in diameter in each of the EW trackers, the magnitude of contraction in each phase was manually measured. The data obtained through “GutCode”49 aligned well with the gross movement of the proximal edge width tracker (EW1g). The gross movement of edge width tracker contraction waves was calculated by dividing the sum of all the crests by the duration of the time period studied, and this measured the magnitude of the contraction. EW1g traces showed low and high amplitude oscillations, and the amplitude of the oscillation was considered as the strength of the contractions, and is denoted as EW1s. To determine the role of EW1s in the duration of DD, EW1s was compared between different DD groups.
The propagation of waves along the intestinal wall was captured using four pairs of EW trackers. The propagation of contraction waves along the intestinal wall and the development of anterograde, retrograde, and segmental contractions play a crucial role in intestinal motility and the dynamics of DD (Fig. 6a–e). The proximal tracker contraction with a distal tracker relaxation resulted in anterograde propulsion while a distal tracker contraction with a proximal tracker relaxation generated retrograde propulsion. When both proximal and distal trackers contracted or relaxed simultaneously, the contraction waves neither proceeded orally nor aborally, triggering segmental contraction (Fig. 6d, e).
The changes in EW trackers were used to calculate real time changes in intestinal volume (V) using the formula V = \(\pi \mathop{\sum }\nolimits_{i=1}^{4}{hi}\frac{{d}_{i}^{2}}{4}\), where d1, d2, d3, and d4 represent the diameters recorded by corresponding EW trackers, and h1, h2, h3, and h4 represent the length of the intestine measured by the trackers, including half the gap between trackers on each side of the gut segment. The formula for volume calculation was integrated into the proprietary program “GutCode”49 which automated and expedited the computation of diameter and volume changes from EW tracings. However, it’s important to note that this volume calculation represents volume changes and could be influenced by the longitudinal and circular muscle contractions, as it was not possible to separate the contributions of circular and longitudinal muscle contractions in our method. The volume calculation helps us understand how luminal filling or emptying influenced DD and ILP changes, or CM and LM movements. Volume tracings showed low and high amplitude contraction waves, and the amplitude of these waves was described as volume strength (Vs) and the gross volume movement was described as Vg.
Quantification of anterograde, retrograde and segmental contractions
We utilized “GutCode”49 for the analysis of diameter data obtained from four EW trackers positioned along the oral-to-aboral axis of intestinal segments. Contractions were categorized into anterograde, retrograde, and segmental based on relative movements of adjacent trackers. Anterograde was noted when the proximal tracker detected contraction followed by relaxation detected by the distal tracker. Retrograde was identified when the proximal tracker noted relaxation followed by contraction detected by the distal tracker.
Segmental contractions were recognized when both proximal and distal trackers detected contractions simultaneously. To quantify contraction strength, we divided the sum of the amplitudes by time, assigning positive values to anterograde, negative values to retrograde, and segmental values based on their overall inclination toward anterograde or retrograde with a positive or a negative sign.
Since “GutCode”49 processed data obtained at a 50 msec intervals, and contraction-relaxation cycle occur at 0.7 Hz, where each wave takes ~1.4 s to complete, only minor shifts were analyzed in anterograde, retrograde, or segmental contractions between EW trackers for each data point. In addition, the slow waves generating propulsive movements can instantaneously change direction and speed of propagation50. Therefore, to determine the overall contraction direction, we introduced “net amplitude”, accounting for small amplitude shifts among all four trackers. A “net amplitude” > 0 indicated anterograde, while <0 indicated retrograde contractions. “Net amplitude” allowed for comparisons between different discharge groups and contraction phases. These recordings provided insights into various contractions, tabulating their frequency, strength, duration, amplitude, retrograde, segmental, and anterograde characteristics, and their impact on intestinal DD. This tabulation facilitated easy comparisons between studied tissue segments (Figs. 1a–d, 5a–i, 6a–e and Tables 1 and 2).
Experimental analysis of droplet discharge
The outflow from the luminal perfusate that constituted a DD was directed to pass through a 1.3 × 3.7 cm opening of Vernier Drop Counter, equipped with an infrared (890 nm) LED emitter at one end, and a detector at the opposite end. When a drop of perfusate obstructed the infrared beam between the emitter and detector, a digital signal was transmitted to the LabQuest®3 system. These drops were then converted into microliters (μl) using a calibration chart within the LabQuest®3 program (Figs. 3d and 4). This method allowed for precise and automated measurement of the time and volume of each DD event occurring at the aboral end in the studied intestinal segments. Thus, DD duration was assessed as the interval between two DD.
Rate of fluid flow through the tubing and/or intestinal segment was represented as “Flow rate”. The flow rate was calculated by dividing the volume of a drop obtained at the aboral end by the time elapsed between DD events, and was represented as ml/min. The flow rate exhibited slight variations between experiments due to minor differences in flow arising from the peristaltic pump and tubing employed. The average flow rate was 0.065 ml/min. The flow rate through the intestine was therefore determined by running the perfusate through a Tygon tubing in lieu of the intestinal segment, both before and after the experiment, and the mean was represented as the average flow rate. The flow through the intestinal segment or the Tygon tubing was achieved using a peristaltic pump (Figs. 3a and 4). Accurate determination of DD event duration is crucial for precise muscular event evaluation. To account for slight variations in flow duration, we normalized the experimental duration (D) for each DD event while the intestine was positioned in the Mayflower bath by dividing D by the standard duration (Ds) when the perfusate passed through a Tygon tubing. Consequently, we utilized the normalization method D/Ds to mitigate potential variations in the flow rate introduced by the pump and tubing during the experiment. When the D/Ds ratio approached one, it indicated minimal variations.
The total inflow and outflow volume over a 15-min period was calculated, and their difference determined the secretory or absorptive nature of the studied intestinal segment. An increase in outflow volume indicated secretion, whereas a decrease suggested absorption. The variations in D/Ds were compared to other muscular events such as changes in ILP, longitudinal movements, diameter (i.e., EW contractions). This analysis provided insights into the mechanisms governing fluid flow and discharge at the aboral end of the gastrointestinal tract.
Since pressure waves were a reflection of CM and /or LM contractions, they were effectively employed as a reference to deduce DD, and assess all muscular activities. When categorizing DD duration, it was observed that DDs could be either short or long in duration. These distinctive durations were closely associated with various muscular parameters and amplitudes of the pressure waves. Therefore, when DDs were sorted by duration, discharges were found to occur either in DPhase or APhase (Fig. 5a). Among the 48 DDs studied, the shortest duration DDs primarily occurred in DPhase, making up 37.5% of total discharges and constituting the SD group (Fig. 5b). Majority of DDs (39.6%) with longer durations occurred in APhase, and were represented as the LA group (Fig. 5c). Additionally, 16.7% of DDs occurring in DPhase had longer durations, classified as the LD group (Fig. 5d). Three DDs, which occurred in APhase but had shorter durations compared to LA, and one discharge occurring in both DPhase and APhase with a long duration, were excluded from further analysis. Thus, based on duration and D/Ds, we identified three discharge groups: SD, LA, and LD.
To gain further insights, we divided the pressure contractions during each DD into four distinct phases (Fig. 5a) based on the Ps. Pressure levels ranging from 0.03 to 0.2 cmH2O were considered low amplitude pressure waves, while pressures exceeding 0.2 cmH2O indicated high amplitude contractions. These high amplitude pressure waves were further categorized based on Ps, Ls, and/or Lg. These parameters exhibited significant changes during these high amplitude pressure waves:
-
The BPhase featured low Ls and Lg, both of which gradually increased throughout this phase. During the BPhase, low amplitude pressure waves were observed.
-
The NPhase began with a rapid Ps increase following BPhase. During this phase, Ls progressively increased and reached a peak or plateau which marked the end of the NPhase. Lg did not increase as much as in BPhase or in some instances it showed a small decrease. The increase in Lg from BPhase to NPhase and NPhase to DPhase suggests LM movement and contraction at the oral end. Conversely, the decrease in Lg in APhase suggests LM movement and contraction at the aboral end.
-
The DPhase followed the NPhase and was characterized by progressively increasing Ls and Lg, both reaching a peak. This phase exhibited the highest amplitude pressure contractions. DPhase showed pressure tracings with the highest amplitude contraction waves and was significantly higher when compared NPhase (p < 0.001, n = 48). DPhase had the following characteristics: (1) Increase in Ps and reaching a plateau that marks the end of DPhase; (2) Increase in Ls and Lg followed by a decrease, which paralleled changes in Ps. Thus, at the end of the DPhase, Ps, Pg and Lg return to baseline levels, which marked the beginning of the APhase (Fig. 5a).
-
The APhase succeeded the DPhase. It was shorter in duration and featured lower amplitude pressure contractions compared to DPhase, resembling BPhase in characteristics. The total duration (20.1 ± 0.1% vs. 45.7 ± 0.8%) and amplitude (0.23 ± 0.02 cmH2O vs. 0.66 ± 0.07 cmH2O; p < 0.001, n = 48) for APhase was significantly lower than DPhase. APhase was comparable to BPhase (Fig. 5a).
These phases provided valuable information about the relative movement and contraction of LM and CM, as well as their timing. This enhanced our understanding of the muscular activity that initiates or precedes each contraction.
Statistics
Statistical analysis was conducted using OriginPro 9.9 (2022), and the different phases were compared within each discharge group. The data were presented as mean ± SEM, and the range of the data sets for DD was shown. Normality of the data sets was evaluated with Shapiro–Wilk test. One-way ANOVA was employed, followed by post hoc Bonferroni test to determine significant differences of data between the four phases. Kruskal–Wallis test was used for overall comparison of the discharge groups, and post hoc Mann–Whitney test was utilized to compare discharge groups between experiments. A significance level (p) was set as <0.05.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All raw data that support this study are available as Supplementary Data and software files in https://zenodo.org/51.
Code availability
The software applications used to extract and calculate the data points are available as Supplementary Data and software files in https://zenodo.org/47,49.
References
Greenwood-Van Meerveld, B., Johnson, A. C. & Grundy, D. Gastrointestinal physiology and function. Handb. Exp. Pharm. 239, 1–16 (2017).
PM, H. Gastrointestinal motility: regulation and impact on matbolism. J. Intern. Med. 237, 389 (1995).
Ailiani, A. C. et al. Quantitative analysis of peristaltic and segmental motion in vivo in the rat small intestine using dynamic MRI. Magn. Reson. Med. 62, 116–126 (2009).
Huizinga, J. D. et al. The origin of segmentation motor activity in the intestine. Nat. Commun. 5, 3326 (2014).
Patel, K. S. & Thavamani, A. StatPearls https://www.ncbi.nlm.nih.gov/books/NBK556137/ (2023).
Avvari, R. K. Role of segmental contraction in the small intestinal digestion: a computational approach to study the physics behind the luminal mixing and transport. J. Theor. Biol. 561, 111418 (2023).
Lujan, H. L. & DiCarlo, S. E. A simple, inexpensive model to demonstrate how contraction of GI longitudinal smooth muscle promotes propulsion. Adv. Physiol. Educ. 39, 131–132 (2015).
Lentle, R. G. & Hulls, C. M. Quantifying patterns of smooth muscle motility in the gut and other organs with new techniques of video spatiotemporal mapping. Front. Physiol. 9, 338 (2018).
Costa, M. et al. Analysis of intestinal movements with spatiotemporal maps: beyond anatomy and physiology. Adv. Exp. Med. Biol. 1383, 271–294 (2022).
Kendig, D. M., Hurst, N. R. & Grider, J. R. Spatiotemporal mapping of motility in ex vivo preparations of the intestines. J. Vis. Exp. 27, e53263 (2016).
Wang, D. et al. Trans-illumination intestine projection imaging of intestinal motility in mice. Nat. Commun. 12, 1682 (2021).
Boquet-Pujadas, A. et al. 4D live imaging and computational modeling of a functional gut-on-a-chip evaluate how peristalsis facilitates enteric pathogen invasion. Sci. Adv. 8, eabo5767 (2022).
Zhao, Q. et al. Action mode of gut motility, fluid and electrolyte transport in chronic constipation. Front. Pharm. 12, 630249 (2021).
Sinha, R. Recent advances in intestinal imaging. Indian J. Radio. Imaging 21, 170–175 (2011).
Lacy, B. E. & Weiser, K. Gastrointestinal motility disorders: an update. Dig. Dis. 24, 228–242 (2006).
Zheng, H. et al. Na(+)/Ca(2 +) exchange and pacemaker activity of interstitial cells of Cajal. Front. Physiol. 11, 230 (2020).
Aliev, R. R., Richards, W. & Wikswo, J. P. A simple nonlinear model of electrical activity in the intestine. J. Theor. Biol. 204, 21–28 (2000).
Sanders, K. M., Ward, S. M. & Koh, S. D. Interstitial cells: regulators of smooth muscle function. Physiol. Rev. 94, 859–907 (2014).
Iino, S. & Horiguchi, K. Interstitial cells of cajal are involved in neurotransmission in the gastrointestinal tract. Acta Histochem. Cytochem. 39, 145–153 (2006).
Al-Ahmadi, A., Mohammed, R. A., Atteya, M., Al-Matrafi, T. A. & Alfayez, M. A. Anoctamin 1 and c-Kit immunohistochemical study of interstitial cells of Cajal in the muscularis externa of human gastrointestinal tract. Folia Morphol. 82, 147–157 (2023).
Azuma, Y. T., Samezawa, N., Nishiyama, K., Nakajima, H. & Takeuchi, T. Differences in time to peak carbachol-induced contractions between circular and longitudinal smooth muscles of mouse ileum. Naunyn Schmiedebergs Arch. Pharmacol. 389, 63–72 (2016).
Shafik, A., Shafik, A. A. & Ahmed, I. Role of the longitudinal smooth muscle coat in the ileal motile activity: evidence of ileo-ileal inhibitory reflex. J. Gastroenterol. Hepatol. 17, 1267–1271 (2002).
Nicosia, M. A., Brasseur, J. G., Liu, J.-B. & Miller, L. S. Local longitudinal muscle shortening of the human esophagus from high-frequency ultrasonography. Am. J. Physiol. Gastrointest. Liver Physiol. 281, G1022–G1033 (2001).
Sugarbaker, D. J., Rattan, S. & Goyal, R. K. Mechanical and electrical activity of esophageal smooth muscle during peristalsis. Am. J. Physiol. 246, G145–150, (1984).
Mittal, R. K. Regulation and dysregulation of esophageal peristalsis by the integrated function of circular and longitudinal muscle layers in health and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 311, G431–G443 (2016).
Smith, T. K. & Robertson, W. J. Synchronous movements of the longitudinal and circular muscle during peristalsis in the isolated guinea-pig distal colon. J. Physiol. 506, 563–577 (1998).
Parsons, S. P. & Huizinga, J. D. Slow wave contraction frequency plateaux in the small intestine are composed of discrete waves of interval increase associated with dislocations. Exp. Physiol. 103, 1087–1100 (2018).
Parsons, S. P. & Huizinga, J. D. Spatial noise in coupling strength and natural frequency within a pacemaker network; consequences for development of intestinal motor patterns according to a weakly coupled phase oscillator model. Front. Neurosci. 10, 19 (2016).
Erickson, J. C., Obioha, C., Goodale, A., Bradshaw, L. A. & Richards, W. O. Detection of small bowel slow-wave frequencies from noninvasive biomagnetic measurements. IEEE Trans. Biomed. Eng. 56, 2181–2189 (2009).
Siegle, M. L., Buhner, S., Schemann, M., Schmid, H. R. & Ehrlein, H. J. Propagation velocities and frequencies of contractions along canine small intestine. Am. J. Physiol. 258, G738–G744 (1990).
Fleckenstein, P. Migrating electrical spike activity in the fasting human small intestine. Am. J. Dig. Dis. 23, 769–775 (1978).
Ryoo, S. B. et al. Electrophysiological and mechanical characteristics in human ileal motility: recordings of slow waves conductions and contractions, in vitro. Korean J. Physiol. Pharm. 19, 533–542 (2015).
Der-Silaphet, T., Malysz, J., Hagel, S., Larry Arsenault, A. & Huizinga, J. D. Interstitial cells of Cajal direct normal propulsive contractile activity in the mouse small intestine. Gastroenterology 114, 724–736 (1998).
Nowak, T. V. & Harrington, B. Effect of cholinergic agonists on muscle from rodent proximal and distal small intestine. Gastroenterology 88, 1118–1125 (1985).
Emmanuel, A., Johnson, M., McSkimming, P. & Dickerson, S. Laxatives do not improve symptoms of opioid-induced constipation: results of a patient survey. Pain Med. 18, 1932–1940 (2017).
Ford, A. C. & Suares, N. C. Effect of laxatives and pharmacological therapies in chronic idiopathic constipation: systematic review and meta-analysis. Gut 60, 209–218 (2011).
Eguchi, T. et al. Risk factors for adverse events in patients with chronic constipation following lubiprostone administration. Dig. Dis. 39, 10–15 (2021).
Linz, D. et al. Antihypertensive and laxative effects by pharmacological inhibition of sodium-proton-exchanger subtype 3-mediated sodium absorption in the gut. Hypertension 60, 1560–1567 (2012).
Al-Shboul, O. A. The importance of interstitial cells of cajal in the gastrointestinal tract. Saudi J. Gastroenterol. 19, 3–15 (2013).
Browning, K. N. & Travagli, R. A. Central nervous system control of gastrointestinal motility and secretion and modulation of gastrointestinal functions. Compr. Physiol. 4, 1339–1368 (2014).
Fung, C. & Vanden Berghe, P. Functional circuits and signal processing in the enteric nervous system. Cell Mol. Life Sci. 77, 4505–4522 (2020).
Bertoni, S. et al. Accommodation and peristalsis are functional responses to obstruction in rat hypertrophic ileum. World J. Gastroenterol. 19, 846–854 (2013).
Kubota, K. et al. Hydroxy-α sanshool induces colonic motor activity in rat proximal colon: a possible involvement of KCNK9. Am. J. Physiol. Gastrointest. Liver Physiol. 308, G579–G590 (2015).
Robinson, A. M. et al. Alterations of colonic function in the Winnie mouse model of spontaneous chronic colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 312, G85–G102 (2017).
Schreiber, D. et al. Motility patterns of ex vivo intestine segments depend on perfusion mode. World J. Gastroenterol. 20, 18216–18227 (2014).
Furness, J. B. The enteric nervous system and neurogastroenterology. Nat. Rev. Gastroenterol. Hepatol. 9, 286–294 (2012).
Sasidharan, A. et al. Peristalsis analysis. Zenodo https://doi.org/10.5281/zenodo.10138991 (2023).
Hasselbrack, R. & Thomas, J. E. Control of intestinal rhythmic contractions by a duodenal pacemaker. Am. J. Physiol. 201, 955–960 (1961).
Sasidharan, A. et al. GutCode. Zenodo https://doi.org/10.5281/zenodo.10145390 (2023).
Quan, X., Yang, Z., Xue, M., Chen, J. H. & Huizinga, J. D. Relationships between motor patterns and intraluminal pressure in the 3-taeniated proximal colon of the rabbit. Sci. Rep. 7, 42293 (2017).
Sasidharan, A. et al. Supplementary Data—Peristalsis. Zenodo https://doi.org/10.5281/zenodo.10145348 (2023).
Acknowledgements
This investigation was funded by R01 grants # DK074867 and # DK109717 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and the Entrinsic Bioscience Research Fund (# P0196836). We would also like to acknowledge Sheldon Xu, Damiano Angoli and Ahrad Nathan for assistance with instrumentation.
Author information
Authors and Affiliations
Contributions
S.V. conceived the project and methodology, and S.V. and J.F.C. contributed to the funding. A.G. conceived the project, and S.V., A.G. and A.S. developed the setup and performed the experiments. A.V.K. and A.H. developed the software applications. A.S., B.A.P. and K.S.K. performed the computational analyses. S.V., A.S. and B.A.P. wrote the manuscript. B.A.P. created Fig. 2a, while S.V. created Fig. 2b, c, and A.G. created Fig. 4. S.V., A.G., N.F. and J.F.C. performed data interpretation and edited the manuscript. All authors have given their approval to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The research was partially funded by Entrinsic Bioscience. S.V. is the Chief Science Officer of and has shares in Entrinsic Bioscience. K.S.K., A.H. and N.F. are consultants for Entrinsic Bioscience. PCT/US2023/017225: Peristaltic Propulsion Device and System and Methods of Use Thereof: Inventors: S.V., A.S., B.A.P., K.S.K., A.G., A.V.K. and A.H. US No. 18/194,632: Peristaltic Propulsion Device and System and Methods of Use Thereof: Inventors: S.V., A.S., B.A.P., K.S.K., A.G., A.V.K. and A.H. US Provisional: No. 63/493,748: Systems and Methods for Analyzing Intestinal Peristalsis. US Provisional: No. 63/599,812: Methods for Use of Peristaltic Propulsion System. J.F.C. does not have competing interests.
Peer review
Peer review information
Communications Biology thanks Ravi Kant Avvari and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Luke R. Grinham. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sasidharan, A., Peethambar, B.A., Kumar, K.S. et al. Advancing peristalsis deciphering in mouse small intestine by multi-parameter tracking. Commun Biol 6, 1237 (2023). https://doi.org/10.1038/s42003-023-05631-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-023-05631-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.