Abstract
Conversational artificial intelligence (AI), particularly AI-based conversational agents (CAs), is gaining traction in mental health care. Despite their growing usage, there is a scarcity of comprehensive evaluations of their impact on mental health and well-being. This systematic review and meta-analysis aims to fill this gap by synthesizing evidence on the effectiveness of AI-based CAs in improving mental health and factors influencing their effectiveness and user experience. Twelve databases were searched for experimental studies of AI-based CAs’ effects on mental illnesses and psychological well-being published before May 26, 2023. Out of 7834 records, 35 eligible studies were identified for systematic review, out of which 15 randomized controlled trials were included for meta-analysis. The meta-analysis revealed that AI-based CAs significantly reduce symptoms of depression (Hedge’s g 0.64 [95% CI 0.17–1.12]) and distress (Hedge’s g 0.7 [95% CI 0.18–1.22]). These effects were more pronounced in CAs that are multimodal, generative AI-based, integrated with mobile/instant messaging apps, and targeting clinical/subclinical and elderly populations. However, CA-based interventions showed no significant improvement in overall psychological well-being (Hedge’s g 0.32 [95% CI –0.13 to 0.78]). User experience with AI-based CAs was largely shaped by the quality of human-AI therapeutic relationships, content engagement, and effective communication. These findings underscore the potential of AI-based CAs in addressing mental health issues. Future research should investigate the underlying mechanisms of their effectiveness, assess long-term effects across various mental health outcomes, and evaluate the safe integration of large language models (LLMs) in mental health care.
Similar content being viewed by others
Introduction
Conversational agents (CAs), or chatbots, have shown substantial promise in the realm of mental health care. These agents can assist with diagnosis, facilitate consultations, provide psychoeducation, and deliver treatment options1,2,3, while also playing a role in offering social support and boosting mental resilience4,5,6. Yet, a majority of these CAs currently operate on rule-based systems, which rely on predefined scripts or decision trees to interact with users7. While effective to a certain degree, these rule-based CAs are somewhat constrained, primarily due to their limited capability to understand user context and intention. Recent advancements in artificial intelligence (AI), such as natural language processing (NLP) and generative AI, have opened up a new frontier--AI-based CAs. Powered by NLP, machine learning and deep learning, these AI-based CAs possess expanding capabilities to process more complex information and thus allow for more personalized, adaptive, and sophisticated responses to mental health needs8,9.
Despite their advantages, AI-based CAs carry risks, such as privacy infringement, biases, and safety issues10. Their unpredictable nature may generate flawed, potentially harmful outcomes leading to unexpected negative consequences11. To ensure the safe and effective integration of AI-based CAs into mental health care, it is imperative to comprehensively review the current research landscape on the use of AI-based CAs in mental health support and treatment. This will inform healthcare practitioners, technology designers, policymakers, and the general public about the evidence-based effectiveness of these technologies, while identifying challenges and gaps for further exploration.
A plethora of research has examined the effectiveness of CAs in influencing mental health, indicating that CAs can effectively mitigate symptoms of depression, anxiety, and distress, while also fostering well-being and quality of life3,12,13,14,15. However, these reviews have largely focused on specific types of CA12 or particular types of mental disorders13,14. Two comprehensive systematic reviews and meta-analyses3,15 provide evidence that supports the effectiveness of various types of CAs across a range of mental health outcomes. However, the over-representation of studies utilizing rule-based CAs in these reviews leaves the effectiveness of AI-based CAs in improving mental health remains underexplored. Moreover, the rapid progress in generative AI, such as Large Language Models (LLMs), necessitates an exploration of this technology’s potential and pitfalls, amidst uncertainties associated with its deployment in mental health care16. Yet, the latest studies on these advanced technologies have not been incorporated into review papers, and thus little is known about their effectiveness compared to other types of AI-based CAs for mental health support. Beyond clinical effectiveness, user experience is vital in impacting clinical outcomes. Nonetheless, prior reviews have not conclusively addressed user experience with AI-based CAs in mental health care or elucidated the factors driving the success of AI-based CA interventions.
This systematic review and meta-analysis aims to evaluate the effects of AI-based CAs on psychological distress and well-being, and to pinpoint factors influencing the effectiveness of AI-based CAs in improving mental health. Specifically, we focus on experimental studies where an AI-based CA is a primary intervention affecting mental health outcomes. Additionally, we conduct narrative synthesis to delve into factors shaping user experiences with these AI-based CAs. To the best of our knowledge, this review is the most up-to-date synthesis of evidence regarding the effectiveness of AI-based CAs on mental health. Our findings provide valuable insights into the effectiveness of AI-based CAs across various mental health outcomes, populations, and CA types, guiding their safe, effective, and user-centered integration into mental health care.
Results
Results of systematic review
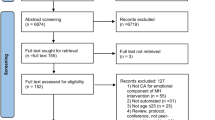
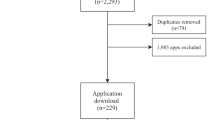
Searches of twelve databases identified 7834 unique citations (Fig. 1). We excluded 7301 records based on titles and abstracts, resulting in 533 records for full-text review. A total of 35 studies from 34 full-text articles met the inclusion criteria and were included in the systematic review for narrative synthesis. Among the 35 studies, one randomized trial17 did not report sufficient data for calculating pooled effect size and 19 studies were not randomized trials, leaving 15 randomized trials eligible for meta-analysis to estimate the effectiveness of AI-based CAs on psychological outcomes. Table 1 presents selected major characteristics of studies included in the systematic review (additional details are presented in Supplementary Table 1 and Supplementary Table 2).
Of the 35 studies included in our systematic review, 19 employed a quasi-experimental design, and 16 were randomized trials. The studies involved 17,123 participants from 15 countries and regions. Most were single-site studies, with 14 conducted in the United States and only one multi-site study conducted in the UK and Japan18. Studies were published between 2017 and 2023, with 27 published since 2020. The majority of studies (n = 28) had sample sizes under 200. Participants’ ages ranged from 10.7 to 92 years. Five studies19,20,21,22,23 focused on adolescents or children, while the rest included adult populations. In terms of gender, one study exclusively evaluated female populations24, and the rest included both genders. Half of the studies (n = 18) involved non-clinical populations, while 10 studies25,26,27,28,29,30,31,32,33,34 included participants with self-report or screened symptoms of mental illnesses, and another seven studies19,24,35,36,37,38,39 involved patients with diagnosed mental or physical issues. Study duration varied considerably, from several minutes to 6 months.
We extracted data on both the characteristics of the CA intervention and the technical design features of the CAs (see Table 2 for a summary). In total, 23 distinct CAs were evaluated across the 35 studies. Most commonly, CAs were used for the delivery of psychotherapy and/or psychoeducational content (n = 22). The integrative approach and CBT emerged as the most prevalent therapeutic approaches, represented in 11 and 6 studies respectively. Additionally, several CAs were designed to offer social assistance, companionship, or act as a source of emotional support for users18,22,30,38,40,41,42,43. There were also instances where CAs were employed for specific purposes such as coaching37,44, counseling45, remote monitoring42, teleconsultation35 or to coordinate within a larger system32. A significant majority of the studies (n = 32) featured CAs as independent, stand-alone systems.
Regarding the design characteristics of CAs, smartphone and tablet applications emerged as the most popular platforms for delivering CA interventions, featured in 16 studies. This was followed by widely used instant messenger platforms like Facebook messenger (n = 9), robots (n = 5), web-based platforms (n = 3), and two studies used VR and EMDR, respectively. The majority of the studies (n = 30) employed retrieval-based CAs to direct conversations through a set of established responses. In all of these retrieval-based CAs, NLP was leveraged to analyze the intent and context of user inputs and to select the appropriate responses. In some instances, this NLP capability was enhanced with machine learning (n = 7), emotion algorithm (n = 6), reinforcement learning (n = 2), natural language understanding (n = 2), or neural network techniques (n = 2) to improve learning and contextual understanding. Conversely, a smaller set of studies (n = 5) implemented generative CAs for mental health interventions, which can generate wholly original dialogs. Of these, one employed both GPT-2 and BERT27, the other four utilized GPT41, BERT45, LSTM40 and DP28, respectively. Regarding interaction mode, most studies used text-based CAs (n = 24). In eight studies22,29,38,42,43,45,46, CAs incorporated emotion AI, such as sentiment analysis, to understand users’ emotional states and address their in-situ needs. Other notable design features included personalization and customization (n = 20), regular check-ins (n = 10), mood tracking (n = 8), empathic responses (n = 7), multimedia (n = 5), and human-like character and personality (n = 2). Despite the growing significance of safety concerns regarding CAs in mental health, only 15 studies incorporated safety assessment or protection measures in CAs, such as access to human experts20,23,39, onboarding processes19,20,25,26,31, assessment of adverse events25,29,31,34 and automatic crises or harm identification17,19,25,31,34,36,41,42,46,47.
The studies evaluated a diverse range of mental health outcomes, with depression (n = 19) and anxiety (n = 18) being the most frequently assessed (see Fig. 2 for a summary). In addition to the psychotherapeutic approaches, three studies incorporated social psychological theories including empathy theory45, cultural competency theory18 and goal attainment theory44 to guide the CA intervention design. We did not identify any eligible studies that examined potential mediators accounting for changes in mental health outcomes, highlighting a critical gap that warrants further exploration. As for moderators, three studies probed the moderating role of user engagement. Notably, increased interactions were tied to enhanced effectiveness in reducing depression47 and anxiety symptoms36,47. However, another study20 observed divergent effects of interaction duration and amount on well-being, suggesting the need for more nuanced user engagement measurements to better understand the relationship between user engagement with CAs and the mental health outcomes. Of the four studies examining participant-related moderators, those with severe baseline mental health symptoms reported greater reductions in psychological distress34,48. Participants’ concurrent therapies or treatments, however, showed inconsistent results. Specifically, two studies noted smaller reductions in anxiety25,34 and depression34 among those engaging concurrent treatments, while another study documented larger reductions in depression in a similar cohort31. One study34 also revealed that unmarried participants experienced greater reductions in depression and anxiety than self-identified sexual minorities.
Narrative synthesis of user engagement and experience
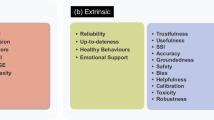
Of the 35 studies, 19 detailed various measures of CA engagement, including metrics such as the amount and length of conversations/messages (n = 13), frequency and duration of CA usage (n = 11), as well as the usage of specific modules or features (n = 5). User experiences with AI-based CAs were reported in 16 studies, primarily focusing on satisfaction (n = 8), acceptability (n = 7), and usability (n = 5), followed by working alliance (n = 4), helpfulness (n = 3), feasibility (n = 3), and likeability (n = 1). A total of 10 studies17,21,26,28,29,33,37,41,46,49 documented open-ended user feedback on their experiences interacting with AI-based CAs. Through inductive thematic analysis, these user feedbacks were classified into positive and negative experiences and further categorized into sub-themes (see Table 3). Notably, process factors fostering the formation of therapeutic relationships were frequently identified as positive experiences in eight studies, with empathic communication being the most commonly cited aspect (n = 5). Participants from six studies emphasized the value of specific therapeutic approaches or techniques (n = 3) and the richness of content (n = 3). Moreover, participants from three studies appraised the learning process facilitated by the CAs, and two favored accessibility. Text-based communication was regarded as a positive aspect in one study. Negative experiences predominantly revolved around communication breakdowns–when the CA failed to effectively understand, process, and respond to user input (n = 8). Content-related factors, both in terms of topics and formats, were indicated as unsatisfactory elements during interactions (n = 4). The impersonal nature of CAs was highlighted in two studies as a contributing factor to negative user experience while technical issues were reported in one study. Furthermore, in one study, participants voiced dissatisfaction regarding the CA’s lack of initiative and its interaction mode. Interestingly, one study found that participants suffering from more severe symptoms expressed a preference for human support over CAs.
Results of meta-analysis
A total of 15 studies, involving 1744 participants, were eligible for inclusion in our meta-analysis. Among these, 13 trials examined indicators of psychological distress (Fig. 3), and eight trials assessed psychological well-being (Fig. 4). Compared to various control conditions, participants interacting with AI-based CAs exhibited a significantly greater reduction in psychological distress, with an effect size of g = 0.7 (95% CI 0.18–1.22). The “leave-one-out” sensitivity analyses demonstrated the robustness of this result, with estimated effect sizes ranging from 0.529 to 0.787. However, when we excluded two influential studies24,27, the overall effect sizes modestly decreased to 0.529 and 0.564, respectively but maintained the same direction and significance (refer to Supplementary Table 3). Interestingly, both of these two studies employed generative CAs, suggesting that the response generation approach of CAs could potentially influence their effectiveness. Although participants interacting with AI-based CA showed improvements in psychological well-being, this enhancement was not statistically significant (g = 0.32; 95% CI –0.13 to 0.78), perhaps because of insufficient power. Only eight trials investigated psychological well-being compared to 13 examining psychological distress. Additional meta-analyses on specific mental health outcomes, detailed in Supplementary Figs. 1–4, indicated that CA interventions significantly outperformed control conditions in ameliorating depression (g = 0.644, 95% CI 0.17–1.12). However, they did not significantly impact anxiety (g = 0.65, 95% CI –0.46 to 1.77), positive affect (g = 0.07, 95% CI –0.43 to 0.57) or negative affect (g = 0.52, 95% CI -0.67 to 1.71).
Note: the pooled effect sizes (Hedges’g) on psychological distress were reverse coded from their original values to align with the directionality of the pooled effect sizes on psychological well-being, i.e., positive effect sizes indicate a more favorable outcome for the CA intervention compared to control conditions.
Analyses revealed significant heterogeneity for both psychological distress (Q = 267.98, p < 0.001, I2 = 95.3%) and psychological well-being (Q = 85.7, p < 0.001, I2 = 91.3%). Egger’s regression test suggested no clear publication bias (Supplementary Table 4). While AI-based CAs demonstrated high effectiveness in addressing psychological distress, we graded the quality of evidence as moderate. This decision was driven by the substantial heterogeneity observed across the studies and the wide confidence interval of the effect estimate, which cast doubts on the consistency and precision of the results. The grade of recommendation for AI-based CAs in enhancing psychological well-being was rated as low (see Supplementary Table 5 for the Summary of Findings). The overall risk of bias was low for two studies, high for five studies, and the remaining eight studies had unclear risk of bias. The most notable source of bias arose from performance bias, largely due to the lack of blinding of participants and personnel, which aligns with findings from a previous study50. Furthermore, the presence of attribution bias in five studies, influenced by either improper methods of addressing missing data or a significant dropout rate, might have caused deviations in the intended interventions (for a visual representation of risk of bias, see Supplementary Fig. 5).
To explore the potential sources of heterogeneity, we performed subgroup analyses focusing on various participant-, study- and CA- related moderators. Regarding psychological distress, the results showed that the ameliorative impact of CAs was more pronounced for generative CAs (g = 1.244) in contrast to retrieval-based ones (g = 0.523, F(2, 19) = 4.883, p = 0.019), and stronger for multimodal/voice-based agents (g = 0.828) compared to text-based ones (g = 0.665, F (2, 19) = 3.655, p = 0.045). Additionally, the effect was stronger when the intervention was delivered through smartphone or tablet apps (g = 0.963) and instant messengers (g = 0.751), than that observed for web-based platforms (g = –0.075, F (3,18) = 3.261, p = 0.046). As for participants’ characteristics, a larger effect size was observed in middle-aged/older adults (g = 0.846) in comparison with adolescents/young adults (g = 0.64, F (2, 19) = 3.691, p = 0.044). Moreover, the reduction in psychological distress was more pronounced in the clinical/subclinical population (g = 1.069) compared to non-clinical population (g = 0.107, F (2,19) = 7.152, p = 0.005). Female percentage in the sample did not moderate the effects of CA on psychological distress (g = –0.47, F (1, 19) = 0.105, p = 0.749). Similarly, CA intervention effects on psychological distress did not differ by the type of control groups (F (5, 20) = 2.598, p = 0.06). Yet, the effects of AI-based CA on psychological well-being did not exhibit significant variations associated with participants’ age (F(2,12) = 1.444, p = 0.274), gender (F(1, 12) = 0.462, p = 0.51), health status (F(2, 12) = 1.624, p = 0.238), the response generation approach (F(2, 12) = 1.253, p = 0.32), interaction mode (F(2, 12) = 1.338, p = 0.299) and delivery platform (F(3, 11) = 1.677, p = 0.23) of the CAs, or the type of control groups (F(4,14) = 0.175, p = 0.948). The detailed results of subgroup analysis are presented in Supplementary Table 6.
Discussion
In this systematic review and meta-analysis, we synthesized evidence on the effectiveness and user evaluation of AI-based CAs in mental health care. Our findings suggest that these CAs can effectively alleviate psychological distress, with the most pronounced effects seen in studies employing generative AI, using multimodal or voice-based CAs, or delivering interventions via mobile applications and instant messaging platforms. CA-based interventions are also more effective among clinical and subclinical groups, and elderly adults. Furthermore, AI-based CAs were generally well-received by the users; key determinants shaping user experiences included the therapeutic relationship with the CA, the quality of content delivered, and the prevention of communication breakdowns.
Notably, we observed a significant and large effect size of AI-based CAs in mitigating psychological distress (g = 0.7) compared to small-to-moderate effects (g ranging from 0.24 to 0.47) reported in a recent review that primarily included rule-based CAs15. This suggests that conversational agents enhanced by advanced AI and machine learning technologies outperform their rule-based counterparts in managing psychological distress. Furthermore, the notably larger effect size of generative CAs (g = 1.244) relative to retrieval-based ones (g = 0.523) suggests that the effectiveness of CA interventions may be influenced by the response generation approach employed, which determines how well these agents are capable of simulating human conversations. Given the rapid advancements in AI technologies, further investigations are warranted to explore the potential benefits and risks of generative CAs. Identifying conditions for optimal effectiveness of different response generation approaches is vital to developing evidence-based guidelines for the implementation of various conversational agents across diverse clinical contexts.
While AI-based CAs consistently reduced psychological distress, their impact on psychological well-being was less consistent, which aligns with a previous review51. There are two possible explanations for this result. First, fewer studies investigated psychological well-being (n = 8) compared to psychological distress (n = 13), which could potentially curtail the statistical power necessary to detect a significant pooled effect on well-being52. Second, measures of psychological distress tend to be more sensitive to recent experience-induced changes, while measures of psychological well-being are typically more stable over time, requiring sustained and long-term engagement. As such, future research should explore the long-term effects of AI-based CAs to evaluate their effectiveness in promoting psychological well-being and to better understand CA effectiveness across diverse mental health outcomes.
Multimodal or voice-based CAs were slightly more effective than text-based ones in mitigating psychological distress. Their integration of multiple communication modalities may enhance social presence53 and deepen personalization, thus fostering a more human-like experience54,55 and boost the therapeutic effects56. In addition, a CA including text and voice functionalities might support individuals with cognitive, linguistic, literacy, or motor impairments. However, a recent study found text-based chatbots were better at promoting fruits and vegetable consumption57. This suggests that the effectiveness of chatbot modality may vary based on context and desired outcomes, underscoring the importance of adaptable, tailored CA designs. Moreover, a significant subgroup difference in psychological distress was noted regarding CA’s delivery platform. Mobile applications and instant messaging platforms may offer advantages in terms of reach, ease of use, and convenience when juxtaposed with web-based platforms, potentially leading to enhanced outcomes.
Our analysis also revealed that AI-based CAs were more effective in clinical and subclinical populations. This result echoes previous studies suggesting that psychological interventions are more effective for people with mental or physical health conditions compared to the general population51 and such effect is larger when mental health symptoms are more severe58. However, prior research also shows that people with more severe symptoms showed a preference for human support37. This underscores the need for research to untangle the complex interplay between symptom severity, CA intervention, human support, and clinical outcomes, and to pinpoint the conditions under which CAs are most effective and when human support is indispensable. Another interesting finding was that middle-aged and older adults seemed to benefit more from AI-based CAs than younger populations. One possible explanation might be the variations in engagement levels, but due to the high heterogeneity across studies, we were unable to validate these assumptions. Future research is warranted, as a prior review suggests a curvilinear relationship between age and treatment effects59. Notably, we did not find a significant moderating effect of gender, consistent with earlier findings demonstrating that digital mental health interventions are similarly effective across genders60.
In terms of user evaluation, most studies included in our review reported positive feedback for AI-based CAs, suggesting their feasibility across diverse demographic groups. Our analysis of open-ended user feedback revealed that factors such as the therapeutic relationship, content quality, and communication breakdowns were key determinants of user experience, which corresponds to previous psychotherapy research that identifies these common elements (e.g., therapeutic alliance, empathy, and therapist effect) as active ingredients contributing to therapeutic changes across various therapeutic frameworks61. Communication breakdowns with CAs can lead to negative user experiences, making the intervention less likely to succeed. Although retrieval-based CAs understand user context better than rule-based CAs, their limitations in generating responses can cause unnatural or repetitive interactions, potentially reducing clinical effectiveness. Despite these factors being identified as important based on qualitative user feedback, none of the included studies empirically examined their mediating or moderating effects. Future research should delve into these elements to understand the mechanisms of change and key components for successful CA interventions.
This review has its limitations. First, our broad search strategy, while exhaustive, led to considerable heterogeneity in outcome measures and results, making definitive conclusions and direct comparisons challenging. Standardized evaluation methods for clinical and non-clinical outcomes in future studies would help address this issue. Second, due to a limited number of studies reporting follow-up effects (n = 6) and the substantial variation in follow-up durations, we were unable to conduct a meta-analysis of the long-term effects of CA interventions on psychological outcomes. Therefore, the lasting effects of CA interventions remain unclear. Third, by only including English-language publications, we may have overlooked relevant studies in other languages, potentially limiting the generalizability of our findings. Fourth, the narrative synthesis of user experiences heavily depends on the interpretative reliability of the original studies, which may have methodological issues influencing their results. Lastly, the realm of generative AI and LLMs is evolving at an unprecedented pace. While we identified five studies using generative CAs powered by various generative AI models and frameworks, we were unable to examine the effect of specific AI models on outcomes due to the limited sample size. As the adoption of generative AI for mental health care expands, future research may benefit from differentiating the impacts of various generative AI forms.
AI-based CAs are surfacing as an impactful component in mental health care. This review provides preliminary and most up-to-date evidence supporting their effectiveness in alleviating psychological distress, while also highlighting key factors influencing effectiveness and user experience. While AI-based CAs are not designed to replace professional mental health services, our review suggests their potential to serve as a readily accessible and effective solution to address the expanding treatment gap. Future research endeavors need to delve deeper into the mechanisms and empirically evaluate the key determinants of successful AI-based CA interventions, spanning diverse mental health outcomes and populations.
Methods
Search strategy and selection criteria
We conducted a systematic search across twelve datasets, using a wide array of search terms. The search covered all data from the inception of each database up until Aug 16, 2022 and was later updated to include new entries up to May 26, 2023. We fine-tuned our search strategy based on previous systematic reviews3,51,62 to locate sources related to AI-based CAs for addressing mental health problems or promoting mental well-being. The search was limited to English-language publications. Complete lists of datasets and search strategies are detailed in Supplementary Table 7.
After removing duplicates, we screened all retrieved citations and abstracts in two stages: title/abstract screening and full-text review. Two reviewers independently reviewed all titles and abstracts for eligibility, followed by a full-text review. At each screening stage, a 10% subset of records was jointly reviewed to evaluate inter-rater reliability; disagreements were resolved through discussion, with the involvement of a third reviewer if needed. Inter-rater reliability, assessed using Cohen’s Kappa63, indicated near-perfect agreement for title/abstract screening (0.9) and full-text review (0.83).
The full description and examples of eligibility criteria are outlined in Supplementary Table 8. Briefly, we developed our eligibility criteria based on PICOS framework: (1) Population: all demographics or groups were eligible; (2) Intervention: we included studies that used an AI-based CA as the primary intervention, which entails a two-way interaction between a user and the CA. These AI-based CAs are defined as software agents or bots that leverage NLP, machine learning or other AI models and techniques to simulate human-like conversations. Unlike rule-based systems that depend on predefined rules or decision trees to formulate responses7, these agents possess the capability to understand user intent, analyze contexts, and retrieve or generate appropriate response based on the users’ input and the context of the conversation; (3) Comparator: we included studies with any comparison, ranging from active CA or human control groups to usual care, or those without a direct comparator, such as single group pre-post studies; (4) Outcome: we considered any outcomes related to psychological distress or well-being as eligible. These could be measured through self-reported questionnaires, objective metrics (e.g., audio or visual signals from passive sensing systems) or third-party evaluations; (5) Study: we included any experimental study design.
Data management and extraction
We developed a comprehensive data extraction form and pilot-tested it on a subset of included studies to ensure reliability and reproducibility. The following data were then extracted from all included studies: publication details (author, title, journal, year), study details (region, duration, method), participant characteristics (population type, sample size, demographics), CA intervention characteristics (deployment, session, role, target condition, safety measures), CA design features (name, delivery platform, AI model/framework/technique, interaction mode, and other reported design features), therapeutic orientation (e.g., cognitive behavioral therapy; CBT), user evaluation approach (user engagement, user experience, and other reported user feedback), psychological outcomes and measures, and mechanisms (theory, moderator, mediator).
We also extracted and narratively synthesized data related to engagement and user experience of AI-based CAs from studies reporting relevant information, encompassing users’ involvement, interactions with CA interventions, and their affective and cognitive evaluations64. Moreover, we observed that some studies reported open-ended user feedback on their experiences with CAs, potentially providing insights into factors affecting the success of CA interventions. To analyze user feedback, two coders performed an inductive thematic analysis to identify prevalent themes in user feedback and summarized these themes narratively.
Meta-analysis methods
To assess the effectiveness of AI-based CA interventions, we conducted a meta-analysis on randomized trials wherein participants were randomly assigned to an experimental group receiving a target CA intervention or to control groups receiving alternative treatments, information, or being placed on a waitlist. Since all of the included randomized controlled trials (RCTs) reported at least one indicator of psychological distress (i.e., distress, depression, anxiety and stress)65 and/or psychological well-being (i.e., psychological well-being, positive and negative affect, mental resilience, mental health self-efficacy), we performed two separate meta-analyses to estimate pooled effect sizes for these two overall psychological outcomes. Furthermore, we conducted meta-analyses for specific psychological outcomes reported by at least three trials, including depressive symptom, generalized anxiety symptom, and positive affect and negative affect.
The meta-analyses were conducted using R software (version 3.6.2) and the metafor package. Data were extracted from RCTs to calculate pooled effect sizes of Hedges’ g, with corresponding 95% confidence intervals and P-values. Hedges’ g of 0.2 indicated a small effect, 0.5 a moderate effect and 0.8 a large effect66. Since we expected considerable heterogeneity among RCTs, random-effects models were used for all meta-analyses a priori. Heterogeneity among trials was assessed using Cochran’s Q test and I2. Egger’s regression test was used to evaluate publication bias. As most trials contributed more than one observed effect size in assessing the two overall psychological outcomes, we fit two three-level random-effects meta-analytical models to account for dependencies between effect sizes, which allow effect sizes to vary between participants, outcomes, and studies67. We calculated Hedges’g using post-intervention outcome data that provided means and standard deviations (SDs). When SDs were not reported, they were obtained by mathematical transformation68. When both intention-to-treat and completer analyses were reported, we extracted and analyzed the former. For studies with multi-arm designs that included multiple experimental or control groups, we combined the means and SDs from the different arms to create a single pair-wise comparison, as suggested by the Cochrane guidelines for integrating multiple groups from a single study69. If a study did not report sufficient data (mean, SD, SE, 95% CI) to calculate Hedges’g, we contacted corresponding authors for missing data; studies lacking necessary data were excluded from the meta-analysis. For sensitivity analysis, we employed a “leave-one-out” method70 to identify influential studies and assess the robustness of estimates.
To investigate potential sources of heterogeneity, we conducted a series of subgroup analyses on the two primary psychological outcomes. In accordance with previous research, we examined participant-specific characteristics (i.e., gender, age, and health status) as well as the type of control groups60. Additionally, we considered three CA technical features (i.e., response generation approach, interaction mode and delivery platform) as potential moderators. We defined response generation approach as the technique a CA employs to formulate responses to user inputs. For building AI-based CAs, there are two major response generation approaches: the retrieval-based approach and the generative approach. The key distinction between the two approaches stems from their underlying mechanisms in response generation. Retrieval-based CAs, like Woebot and Wysa, rely on dialog management frameworks to track the flow of conversation and select appropriate responses from a pre-established repository of conversational utterances. In contrast, generative CAs, such as ChatGPT and Replika, leverage machine learning algorithms to learn and auto-generate responses based on a large amount of training data71. In terms of the interaction mode, we categorized the CAs into text-based, where users communicate with the CA via textual messages, and multimodal/voice-based, allowing users to engage with the CA using either text or vocal inputs. Furthermore, based on the medium through which the CA interacts with the users, the CAs were grouped into smartphone/tablet app, instant messaging platform, web-based platform, or robot.For categorical variables such as response generation approach, we used mixed-effects models for the subgroup analyses, while a meta-regression approach was employed for the continuous variable (i.e., gender). A detailed description of the moderators is outlined in Table 4.
We employed the Cochrane risk of bias assessment72 to assess the risk of bias in the included RCTs. This assessment tool evaluates seven domains of potential bias: selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias. For each domain, a trial can be categorized as having a low, high or unclear risk of bias. For the overall risk-of-bias judgment, we adopted the approach from He et al.15 Specifically, a trial was deemed to have a low risk of bias only if all domains were rated as low-risk. Conversely, any trial was judged to have a high risk of bias if it scored high in any domain, with the exception of performance bias. We excluded performance bias from this criterion due to the practical challenges associated with blinding participants and personnel in CA-based interventions50. Trials with at least one domain rated as unclear, but no domains rated as high risk were classified as having “some concerns”. For visualization, the risk of bias was represented using Review Manager (version 5.4).
To evaluate the quality of evidence presented in the two primary meta-analyses of RCTs, we used the GRADE approach73, which provides a holistic assessment of the combined evidence from meta-analyses. It incorporates five key considerations, and the quality of evidence may be downgraded if any of these are not adequately met. Specifically, the five considerations focus on study limitations (i.e., concerns about the risk of bias), inconsistency of the effects (i.e., variability in the effect estimates, often indicated by heterogeneity), indirectness (i.e., differences in the population, intervention, or outcome from what was intended), imprecision (i.e., uncertainty in the effect estimate, e.g., wide confidence interval), and publication bias (potential underreporting of studies with negative or null results). Conversely, factors like a large magnitude of effect or evidence of a dose-response gradient can lead to upgrades. The overall quality of evidence can be classified as high, moderate, low, or very low. The GRADE assessment is presented in the Summary of Findings table.
The study protocol was registered in PROSPERO, CRD 42023392187, and adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analyses74 (Supplementary Table 9).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data collected and used in this meta-analysis can be requested from the corresponding author.
References
Dingler, T., Kwasnicka, D., Wei, J., Gong, E. & Oldenburg, B. The use and promise of conversational agents in digital health. Yearb. Med. Inf. 30, 191–199 (2021).
Jabir, A. I. et al. Evaluating conversational agents for mental health: Scoping review of outcomes and outcome measurement instruments. J. Med. Internet Res. 25, e44548 (2023).
Abd-Alrazaq, A. A., Rababeh, A., Alajlani, M., Bewick, B. M. & Househ, M. Effectiveness and safety of using chatbots to improve mental health: Systematic review and meta-analysis. J. Med. Internet Res. 22, e16021 (2020).
Loveys, K., Fricchione, G., Kolappa, K., Sagar, M. & Broadbent, E. Reducing patient loneliness with artificial agents: Design insights from evolutionary neuropsychiatry. J. Med. Internet Res. 21, e13664 (2019).
Inkster, B., Sarda, S. & Subramanian, V. An empathy-driven, conversational artificial intelligence agent (Wysa) for digital mental well-being: Real-world data evaluation mixed-methods study. JMIR Mhealth Uhealth 6, e12106 (2018).
Torous, J. et al. The growing field of digital psychiatry: current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 20, 318–335 (2021).
Abd-Alrazaq, A. A. et al. An overview of the features of chatbots in mental health: A scoping review. Int. J. Med. Inf. 132, 103978 (2019).
Koutsouleris, N., Hauser, T. U., Skvortsova, V. & De Choudhury, M. From promise to practice: Towards the realisation of AI-informed mental health care. Lancet Digit Health 4, e829–e840 (2022).
Adamopoulou, E. & Moussiades, L. An overview of chatbot technology. In Artificial Intelligence Applications and Innovations 373–383 (Springer International Publishing, 2020).
May, R. & Denecke, K. Security, privacy, and healthcare-related conversational agents: A scoping review. Inform. Health Soc. Care 47, 194–210 (2022).
Luxton, D. D. Ethical implications of conversational agents in global public health. Bull. World Health Organ 98, 285–287 (2020).
Scoglio, A. A., Reilly, E. D., Gorman, J. A. & Drebing, C. E. Use of social robots in mental health and well-being research: Systematic review. J. Med. Internet Res. 21, e13322 (2019).
Lim, S. M., Shiau, C. W. C., Cheng, L. J. & Lau, Y. Chatbot-delivered psychotherapy for adults with depressive and anxiety symptoms: A systematic review and meta-regression. Behav. Ther. 53, 334–347 (2022).
Vaidyam, A. N., Linggonegoro, D. & Torous, J. Changes to the psychiatric chatbot landscape: A systematic review of conversational agents in serious mental illness. Can. J. Psychiatry 66, 339–348 (2021).
He, Y. et al. Conversational agent interventions for mental health problems: Systematic review and meta-analysis of randomized controlled trials. J. Med. Internet Res. 25, e43862 (2023).
Arora, A. & Arora, A. The promise of large language models in health care. Lancet 401, 641 (2023).
Fulmer, R., Joerin, A., Gentile, B., Lakerink, L. & Rauws, M. Using psychological Artificial Intelligence (Tess) to relieve symptoms of depression and anxiety: Randomized controlled trial. JMIR Ment. Health 5, e64 (2018).
Papadopoulos, C. et al. The CARESSES randomised controlled trial: Exploring the health-related impact of culturally competent Artificial Intelligence embedded into socially assistive robots and tested in older adult care homes. Adv. Robot. 14, 245–256 (2022).
Nicol, G., Wang, R., Graham, S., Dodd, S. & Garbutt, J. Chatbot-delivered cognitive behavioral therapy in adolescents with depression and anxiety during the COVID-19 pandemic: Feasibility and acceptability study. JMIR Form. Res. 6, e40242 (2022).
Vertsberger, D., Winsberg, M. & Naor, N. Adolescents’ wellbeing while using a mobile Artificial Intelligence-powered acceptance commitment therapy tool: Evidence from a longitudinal study. JMIR AI 1, e38171 (2022).
De Nieva, J. O., Joaquin, J. A., Tan, C. B., Marc Te, R. K. & Ong, E. Investigating students’ use of a mental health chatbot to alleviate academic stress. In 6th International ACM In-Cooperation HCI and UX Conference (ACM, 2020).
Gamborino, E., Yueh, H.-P., Lin, W., Yeh, S.-L. & Fu, L.-C. Mood estimation as a social profile predictor in an autonomous, multi-session, emotional support robot for children. In 2019 28th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN) 1–6 (2019).
Legaspi, C. M., Jr, Pacana, T. R., Loja, K., Sing, C. & Ong, E. User perception of Wysa as a mental well-being support tool during the COVID-19 pandemic. In Asian HCI Symposium’22 52–57 (Association for Computing Machinery, 2023).
Tawfik, E., Ghallab, E. & Moustafa, A. A nurse versus a chatbot ‒ the effect of an empowerment program on chemotherapy-related side effects and the self-care behaviors of women living with breast Cancer: a randomized controlled trial. BMC Nurs. 22, 102 (2023).
Prochaska, J. J. et al. A randomized controlled trial of a therapeutic relational agent for reducing substance misuse during the COVID-19 pandemic. Drug Alcohol Depend. 227, 108986 (2021).
Fitzpatrick, K. K., Darcy, A. & Vierhile, M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): A randomized controlled trial. JMIR Ment. Health 4, e19 (2017).
Romanovskyi, O., Pidbutska, N. & Knysh, A. Elomia Chatbot: The effectiveness of Artificial Intelligence in the fight for mental health. In COLINs 5th International Conference on Computational Linguistics and Intelligent Systems, 1215–1224 (2021).
He, Y. et al. Mental health chatbot for young adults with depressive symptoms during the COVID-19 pandemic: Single-blind, three-arm randomized controlled trial. J. Med. Internet Res. 24, e40719 (2022).
Liu, H. et al. chatbots to provide self-help depression interventions for university students: A randomized trial of effectiveness. Internet Inter. 27, 100495 (2022).
Abdollahi, H., Mollahosseini, A., Lane, J. T. & Mahoor, M. H. A pilot study on using an intelligent life-like robot as a companion for elderly individuals with dementia and depression. In 2017 IEEE-RAS 17th International Conference on Humanoid Robotics (Humanoids) 541–546 (2017).
Prochaska, J. J. et al. A therapeutic relational agent for reducing problematic substance use (Woebot): Development and usability study. J. Med. Internet Res. 23, e24850 (2021).
Goga, N. et al. An efficient system for Eye Movement Desensitization and Reprocessing (EMDR) therapy: A pilot study. Healthcare (Basel) 10, (2022).
Wrightson-Hester, A.-R. et al. An artificial therapist (Manage Your Life Online) to support the mental health of youth: Co-design and case series. JMIR Hum. Factors 10, e46849 (2023).
Chiauzzi, E. et al. Demographic and clinical characteristics associated with anxiety and depressive symptom outcomes in users of a digital mental health intervention incorporating a relational agent. Preprint at https://doi.org/10.21203/rs.3.rs-2488688/v1 (2023).
Ogawa, M. et al. Can AI make people happy? The effect of AI-based chatbot on smile and speech in Parkinson’s disease. Parkinsonism Relat. Disord. 99, 43–46 (2022).
Leo, A. J. et al. A digital mental health intervention in an orthopedic setting for patients with symptoms of depression and/or anxiety: Feasibility prospective cohort study. JMIR Form. Res. 6, e34889 (2022).
Bassi, G. et al. A virtual coach (Motibot) for supporting healthy coping strategies among adults with diabetes: Proof-of-Concept study. JMIR Hum. Factors 9, e32211 (2022).
Tulsulkar, G. et al. Can a humanoid social robot stimulate the interactivity of cognitively impaired elderly? A thorough study based on computer vision methods. Vis. Comput. 37, 3019–3038 (2021).
Leo, A. J. et al. Digital mental health intervention plus usual care compared with usual care only and usual care plus in-person psychological counseling for orthopedic patients with symptoms of depression or anxiety: Cohort study. JMIR Form. Res. 6, e36203 (2022).
Drouin, M., Sprecher, S., Nicola, R. & Perkins, T. Is chatting with a sophisticated chatbot as good as chatting online or FTF with a stranger? Comput. Hum. Behav. 128, 107100 (2022).
Sabour, S. et al. A chatbot for mental health support: Exploring the impact of Emohaa on reducing mental distress in China. Front. Digit. Health 5, 1133987 (2023).
Rathnayaka, P. et al. A mental health chatbot with cognitive skills for personalised behavioural activation and remote health monitoring. Sensors 22, (2022).
Pham, M., Do, H. M., Su, Z., Bishop, A. & Sheng, W. Negative emotion management using a smart shirt and a robot assistant. IEEE Robot. Autom. Lett. 6, 4040–4047 (2021).
Terblanche, N., Molyn, J., De Haan, E. & Nilsson, V. O. Coaching at scale: Investigating the efficacy of Artificial Intelligence coaching. Int. J. Evid. Based Coach. Mentor 20, 20–36 (2022).
Trappey, A. J. C., Lin, A. P. C., Hsu, K. Y. K., Trappey, C. V. & Tu, K. L. K. Development of an empathy-centric counseling chatbot system capable of sentimental dialogue analysis. Processes 10, 930 (2022).
Klos, M. C. et al. Artificial Intelligence–based chatbot for anxiety and depression in university students: Pilot randomized controlled trial. JMIR Formative Res. 5, e20678 (2021).
Daley, K. et al. Preliminary evaluation of the engagement and effectiveness of a mental health chatbot. Front Digit Health 2, 576361 (2020).
Bird, T., Mansell, W., Wright, J., Gaffney, H. & Tai, S. Manage your life online: A web-based randomized controlled trial evaluating the effectiveness of a problem-solving intervention in a student sample. Behav. Cogn. Psychother. 46, 570–582 (2018).
Demirci, H. M. User experience over time with conversational agents: Case study of Woebot on supporting subjective well-being. (Middle East Technical University, 2018).
Linardon, J., Cuijpers, P., Carlbring, P., Messer, M. & Fuller-Tyszkiewicz, M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry 18, 325–336 (2019).
van Agteren, J. et al. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 5, 631–652 (2021).
Hak, T., van Rhee, H. & Suurmond, R. How to interpret results of meta-analysis. (Rotterdam, The Netherlands: Erasmus Rotterdam Institute of Management, 2016).
Cho, E. Hey Google, Can I ask you something in private? in Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems 1–9 (Association for Computing Machinery, 2019).
Druga, S., Williams, R., Breazeal, C. & Resnick, M. Hey Google is it OK if I eat you? in Proceedings of the 2017 Conference on Interaction Design and Children (Association for Computing Machinery, 2017).
Loveys, K., Hiko, C., Sagar, M., Zhang, X. & Broadbent, E. ‘I felt her company’: A qualitative study on factors affecting closeness and emotional support seeking with an embodied conversational agent. Int. J. Hum. Comput. Stud. 160, 102771 (2022).
Sezgin, E. et al. Readiness for voice assistants to support healthcare delivery during a health crisis and pandemic. npj Digit. Med. 3, 122 (2020).
Singh, B. et al. Systematic review and meta-analysis of the effectiveness of chatbots on lifestyle behaviours. npj Digit. Med. 6, 118 (2023).
Driessen, E., Cuijpers, P., Hollon, S. D. & Dekker, J. J. M. Does pretreatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J. Consult. Clin. Psychol. 78, 668–680 (2010).
Cuijpers, P. et al. Psychotherapy for depression across different age groups: A systematic review and meta-analysis. JAMA Psychiatry 77, 694–702 (2020).
Firth, J. et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry 16, 287–298 (2017).
Wampold, B. E. How important are the common factors in psychotherapy? An update. World Psychiatry 14, 270–277 (2015).
Charlson, F. et al. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet 394, 240–248 (2019).
McHugh, M. L. Interrater reliability: the kappa statistic. Biochem. Med. 22, 276–282 (2012).
O’Brien, H. L. & Toms, E. G. What is user engagement? A conceptual framework for defining user engagement with technology. J. Am. Soc. Inf. Sci. Technol. 59, 938–955 (2008).
Viertiö, S. et al. Factors contributing to psychological distress in the working population, with a special reference to gender difference. BMC Public Health 21, 611 (2021).
Cohen, J. A power primer. Psychol. Bull. 112, 155–159 (1992).
Assink, M. & Wibbelink, C. J. M. Fitting three-level meta-analytic models in R: A step-by-step tutorial. Quant. Methods Psychol. 12, 154–174 (2016).
Higgins J. P. T., Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. https://handbook-51.cochrane.org/chapter_7/7_7_3_2_obtaining_standard_deviations_from_standard_errors_and.htm (accessed Nov 10, 2022).
Higgins J. P. T., Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. https://handbook-5-1.cochrane.org/chapter_16/16_5_4_how_to_include_multiple_groups_from_one_study.htm (accessed Nov 10, 2022).
Higgins, J. P. T. et al. Cochrane Handbook for Systematic Reviews of Interventions. (John Wiley & Sons, 2019).
Wang, L., Mujib, M. I., Williams, J., Demiris, G. & Huh-Yoo, J. An evaluation of generative pre-training model-based therapy chatbot for caregivers. Preprint at https://doi.org/10.48550/arXiv.2107.13115 (2021).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926 (2008).
Moher, D. et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J. Surg. 8, 336–341 (2010).
Bennion, M. R., Hardy, G. E., Moore, R. K., Kellett, S. & Millings, A. Usability, acceptability, and effectiveness of web-based conversational agents to facilitate problem solving in older adults: Controlled study. J. Med. Internet Res. 22, e16794 (2020).
Massetti, G. M., Thomas, C. C., King, J., Ragan, K. & Buchanan Lunsford, N. Mental health problems and cancer risk factors among young adults. Am. J. Prev. Med. 53, S30–S39 (2017).
Acknowledgements
The present study is supported by the Singapore Ministry of Education Academic Research Fund Tier 1 A-8000877-00-00, National University of Singapore Start-up Grant A-8000936-01-00, and NIMH grant P50 MH119029. The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
H.L. and R.Z. have contributed equally to this manuscript. H.L. and R.Z. developed the protocol. H.L. searched the electronic databases. The study selection process, data extraction, and risk of bias assessment were carried out by H.L. and R.Z. Data synthesis was conducted by H.L. and R.Z. H.L. did the statistical analysis and visualization. H.L., R.Z., Y.C.L., R.E.K. and D.C.M. contributed to data interpretation. H.L. and R.Z. prepared the original manuscript draft. The article was revised critically for important intellectual content by all authors. All authors approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, H., Zhang, R., Lee, YC. et al. Systematic review and meta-analysis of AI-based conversational agents for promoting mental health and well-being. npj Digit. Med. 6, 236 (2023). https://doi.org/10.1038/s41746-023-00979-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-023-00979-5