Abstract
Many areas of medicine would benefit from deeper, more accurate phenotyping, but there are limited approaches for phenotyping using clinical notes without substantial annotated data. Large language models (LLMs) have demonstrated immense potential to adapt to novel tasks with no additional training by specifying task-specific instructions. Here we report the performance of a publicly available LLM, Flan-T5, in phenotyping patients with postpartum hemorrhage (PPH) using discharge notes from electronic health records (n = 271,081). The language model achieves strong performance in extracting 24 granular concepts associated with PPH. Identifying these granular concepts accurately allows the development of interpretable, complex phenotypes and subtypes. The Flan-T5 model achieves high fidelity in phenotyping PPH (positive predictive value of 0.95), identifying 47% more patients with this complication compared to the current standard of using claims codes. This LLM pipeline can be used reliably for subtyping PPH and outperforms a claims-based approach on the three most common PPH subtypes associated with uterine atony, abnormal placentation, and obstetric trauma. The advantage of this approach to subtyping is its interpretability, as each concept contributing to the subtype determination can be evaluated. Moreover, as definitions may change over time due to new guidelines, using granular concepts to create complex phenotypes enables prompt and efficient updating of the algorithm. Using this language modelling approach enables rapid phenotyping without the need for any manually annotated training data across multiple clinical use cases.
Similar content being viewed by others
Introduction
Robust phenotyping is essential to multiple clinical and research workflows, such as clinical diagnosis1, novel phenotype discovery2, clinical trial screening3, comparative effectiveness research4, quality improvement5, and genome-wide and phenome-wide association studies6. The wide adoption of electronic health records (EHR) has enabled the development of digital phenotyping approaches, which seek to leverage the large amounts of electronic patient data, stored as structured data (e.g. diagnosis codes, medications, and laboratory results) and unstructured clinical notes, to characterize a patient’s clinical presentation. Currently, many phenotyping approaches utilize diagnosis codes such as the International Classification of Diseases (ICD)7 or a combination of rules based on structured data8,9. While structured data is readily available and easily computable, structured data often reflect billing processes rather than disease course and do not capture the nuanced clinical narrative found in the EHR notes10,11.
Natural language processing (NLP) methods have increasingly been used to enable more precise, multi-modal phenotyping by automating data extraction from unstructured clinical notes. Most approaches are rule-based, relying on keywords12, regular expressions13, and/or existing NLP tools that extract medical ontology concepts14,15 to identify relevant information from notes. These approaches produce interpretable phenotypes, but often have low recall due to the use of hand-crafted features. In contrast, supervised machine learning based phenotyping approaches allow for learning useful features and may produce less brittle models11,16,17. However, supervised machine learning models have been difficult to implement because they require substantial clinician-annotated data for training robust models.
Recent advances in training large language models (LLMs) offer an opportunity to develop generalizable phenotypes without substantial annotated data. A common paradigm in NLP has been to first pretrain a model via a self-supervised learning objective on large amounts of unlabeled text and then fine-tune the model on a specific downstream task of interest using labeled training data. However, more recent work has demonstrated the ability of LLMs to adapt to new tasks without any gradient updates or fine-tuning, simply by specifying task instructions via text interaction with the model18,19,20,21,22. For example, Agrawal et al. found that GPT-3 can perform few-shot information extraction on several clinical tasks, including acronym disambiguation, co-reference resolution, and medication extraction23. Contemporaneous to this work, McInerney et al. show that Flan-T5 can perform feature extraction from clinical notes to enable training of risk prediction models24. The zero- and few-shot capabilities of these models (i.e., their ability to generalize to novel tasks with zero or limited examples) can enable rapid development of models for diverse clinical applications where labeled data is sparse or expensive to acquire. The zero shot capabilities of LLMs provide an opportunity to perform phenotyping of complex clinical conditions, such as postpartum hemorrhage (PPH), using clinical notes. PPH is the leading cause of severe maternal morbidity and mortality. Globally, PPH complicates 2-3% of all pregnancies and accounts for 140,000 maternal deaths annually25. The current PPH definition is based on the documentation of estimated blood loss of at least 1000 mL following delivery26. PPH is typically identified in large epidemiological studies using diagnosis codes7,27; however, such codes have limited accuracy7. More comprehensive PPH phenotype definitions have been developed8, but there is limited work in incorporating clinical notes into PPH phenotype definitions28. Furthermore, several subtypes of PPH exist, each of which is associated with different etiologies, management, and outcomes. Clinical guidelines recommend prompt identification of the PPH subtype in order to initiate appropriate interventions26. However, to the best of our knowledge, there are no digital phenotyping algorithms for PPH subtypes.
The goal of this study is to develop a robust and interpretable approach for rapid phenotyping and subtyping of postpartum hemorrhage (PPH) patients. We leverage Flan-T5, an open-source LLM, to perform zero-shot extraction of PPH-related concepts from obstetric discharge summaries, and we use the extracted concepts to perform interpretable PPH phenotyping and subtyping. We validate the extracted concepts using manual expert chart review and find that Flan-T5 can extract PPH-related concepts with strong performance and can identify PPH patients and subtypes of PPH that are missed by common structured data approaches. This two-step extract-then-phenotype approach allows for greater interpretability compared to end-to-end supervised machine learning models and better recall compared to more brittle keyword or regex rules-based models. Furthermore, the open-source Flan-T5 LLMs can be run locally behind a hospital firewall, limiting concerns regarding the security, privacy, and run-time costs of the models. Our findings highlight the potential for LLMs to annotate clinical notes and facilitate rapid and accurate phenotyping for diverse clinical outcomes.
Results
Study cohort
We identified 138,648 unique individuals with an obstetric encounter resulting in birth after 20 gestational weeks at the Mass General Brigham (MGB) hospitals in Boston, MA, from 1998–2015. There were a total of 503,991 discharge summaries for patients in this initial cohort. We leveraged discharge summaries for NLP-based phenotyping, as postpartum hemorrhage (PPH) typically develops within 24 hours after delivery, and patients are not discharged until at least 24 hours post-delivery. As not every discharge note described a delivery encounter, we developed a combination of terms to identify delivery-related discharge notes with high recall (See Methods). After filtering discharge summaries that did not describe a delivery encounter, our final study cohort was comprised of 131,284 unique patients with 271,081 discharge summaries (Fig. 1a). Each patient had an average of 2.1 obstetric discharge summary notes (SD = 1.4), consisting of 807.6 words on average (SD = 923.1). The cohort characteristics are summarized in Fig. 1b–e.
a Inclusion criteria for identifying delivery-related discharge summaries. The final cohort consists of 271,081 discharge notes for 131,284 women with an obstetric encounter at Mass General Brigham hospitals from 1998–2015. b–e Characteristics of the cohort based on (b) delivery hospital and (c) patient age at delivery, (d) patient race, and (e) patient ethnicity. ER emergency room, MGH Massachusetts General Hospital, BWH Brigham and Women’s Hospital, NSM North Shore Medical Center, NWH Newton Wellesley Hospital.
Zero-shot extraction of PPH-related concepts with NLP
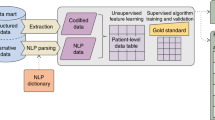
We developed a list of 24 PPH-related concepts based on an extensive literature review and discussion with expert physicians (V.K. and K.G.; full list and definitions in Supplementary Table 1). We identified the PPH-related concepts in all discharge summaries by prompting the 11 billion parameter Flan-T5 model (Flan-T5-XXL), to either answer a yes/no question regarding the presence of a condition, medication, or procedure (e.g., uterine atony) or to extract a specific measurement (e.g., estimated blood loss; Fig. 2a). We used a set of 50 annotated notes to develop the LLM prompts. This approach allows for extraction of concepts from unstructured text without requiring data to further train the model. Only a small number of annotated notes are needed for prompt development.
a Zero-shot extraction of PPH concepts using Flan-T5. We constructed either yes/no or extraction prompts for each PPH concept, concatenated the discharge summary of interest, and fed the combined input into Flan-T5. This process enabled the rapid extraction of PPH-related information from notes with no training data. b We leveraged the extracted concepts to perform interpretable phenotyping of PPH defined as cesarean deliveries with at least 1L or vaginal deliveries with at least 500mL of estimated blood loss. c We used the extracted concepts to perform interpretable subtyping of PPH based on the underlying etiology. We assigned a delivery note to the “tone", “tissue", “trauma", or “thrombin" subtype if any of the concepts associated with the subtype are present. PPH postpartum hemorrhage, EBL estimated blood loss, image: Flaticon.com.
We evaluated the Flan-T5 model performance on a random sample of 1175 manually annotated discharge summaries with PPH ICD diagnosis codes. Discharge summaries with PPH diagnosis codes were used to enrich for obstetric discharge summaries more likely to contain PPH-related concepts. The Flan-T5 performance is summarized in Table 1.
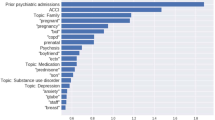
We compared the Flan-T5 NLP models to regular expressions constructed for each PPH-related concept (Fig. 3; Supplementary Table 2). Regular expressions were selected as the baseline approach because they can similarly be constructed with minimal “training" data. Our primary evaluation metric for the classification tasks was binary F1 score, which is useful for imbalanced datasets with rare labels where performance on the positive class is most important. The Flan-T5 model achieved a binary F1 score of 0.75 or higher on 21 of 23 binary concepts, exceeding a 0.9 binary F1 score on 12 of the PPH concepts. Flan-T5 significantly outperformed the corresponding regular expression for nine binary PPH-related concepts (all p-values < 0.05, McNemar test). Furthermore, the model extracted estimated blood loss values with a recall of 0.745, precision of 0.905, and note level accuracy of 95.1%. While regular expressions achieved similar performance on simpler extraction tasks, such as identification of medication use, the Flan-T5 model outperformed regular expressions on concepts that are expressed in clinical notes in variable formats, such as coagulation disorders. Flan-T5’s false positives were largely in notes with polysemy or semantically related concepts.
For example, the notes that contained postpartum ‘dilation and curettage’ were also often predicted to be positive for ‘manual removal of placenta’; the latter procedure commonly precedes curettage. The majority of false positives for the concept ’uterine rupture’ were in notes in which there was a mention of ’rupture’. However, in those cases, the annotators inferred that ’rupture’ was related to the artificial or spontaneous rupture of membranes, which is part of normal labor, rather than ’uterine rupture’. The false negatives were commonly due to unusual abbreviations or concepts with multiple misspellings. For example, in one of the notes containing the following text ‘500ccf/b d&c for retained POC’, the model correctly identified the concept ‘retained products of conception’ but was unable to extract the blood loss, in this case ‘500’ or identify ‘dilation and curettage’.
While prompts were developed solely on notes from a single hospital site, we found that the model generalized well to notes from other MGB hospitals. There was no substantial difference in performance across hospital sites (Supplementary Table 3). We further evaluated Flan-T5 on a sample of 100 notes from 2015–2022 to assess generalizability over time and across electronic health records. The Flan-T5 model achieved a binary F1 score of 0.75 or higher on 14 of the 20 binary concepts with annotated examples (Supplementary Table 4). The model performed comparably in both settings for most concepts, but there were six concepts with fewer positive examples that had larger differences in binary F1 score over time.
NLP-based identification of PPH cases
We leveraged the extracted concepts to identify deliveries with postpartum hemorrhage (Fig. 2b). The Flan-T5 model extracted the estimated blood loss values and delivery type (cesarean or vaginal) from all notes in the cohort (n = 271,081). Subsequently, we classified notes as describing PPH if patients had blood loss greater than 500 mL for vaginal deliveries or greater than 1000 mL for cesarean deliveries. This matched the PPH definition used in the hospitals during the study period (See Methods). There were 2598 discharge summary notes for 2270 deliveries in our study cohort with PPH, according to the model. The prevalence of each PPH-related concept in the deliveries with PPH identified based on model-extracted blood loss can be found in Table 2.
We evaluated the PPH phenotyping algorithm by comparing the model performance on a random sample of 300 expert-annotated discharge summary notes predicted by Flan-T5 to describe deliveries with PPH. The gold-standard discharge summaries were annotated via manual medical record review. The positive predictive value of the NLP-based PPH phenotyping algorithm is 0.95. The NLP-based approach allows identification of PPH cases that lack any PPH International Classification of Diseases (ICD) diagnosis codes associated with the delivery. Of the 285 discharge summaries with confirmed PPH, 148 and 136 did not have an associated PPH ICD code according to the definitions in Butwick et al.7 and Zheutlin et al.8, respectively. Over 47% of the discharge summaries with PPH would not have been identified using PPH ICD codes alone.
We further examined the relationship between model-extracted estimated blood loss and presence of PPH ICD codes on the entire notes cohort (n = 271,081). As the blood loss amount increases, there is more likely to be a PPH ICD code associated with the admission, as expected (Fig. 4, Supplementary Fig. 2). When no estimated blood loss is extracted, the prevalence of PPH ICD codes is less than 5%. When the extracted blood loss values are between 1000 and 1500 mL, criteria which meet both historical and current definitions of PPH, less than 50% of notes have an associated PPH ICD code.
The y-axis depicts the range of estimated blood loss (EBL) values extracted from the delivery note by Flan-T5 (if any), and the x-axis denotes the proportion of notes in each EBL category with a postpartum hemorrhage ICD diagnostic code. PPH ICD codes are defined according to the definition in Zheutlin et al.8. Refer to Supplementary Fig. 2 for a similar plot using the PPH ICD definition from Butwick et al.7. PPH postpartum hemorrhage, ICD international classification of diseases, EBL estimated blood loss.
NLP-based classification of PPH subtypes
Finally, we leverage the extracted PPH concepts to classify deliveries with PPH into four subtypes corresponding to distinct causes of PPH: uterine atony ("tone"), retained products of conception and placenta accreta spectrum ("tissue”), birth or surgical trauma, (‘trauma’) and coagulation abnormalities ("thrombin”; Fig. 2c). We constructed composite phenotypes for each subtype based on the presence of one or more NLP-extracted PPH terms (See Methods). Using these NLP-based subtyping algorithms, we estimate that 29.9% of predicted PPH deliveries in our study cohort are due to uterine atony, 26.8% are due to retained products of conception, 24.0% are due to trauma, and 5.7% are due to coagulation abnormalities.
We validated the subtyping algorithm via an expert manual medical record review of the 285 confirmed PPH deliveries. The PPH subtype could be determined via manual review of the discharge summary in 73% of notes. We found that the NLP-based approach can achieve strong performance in subtype classification of those notes across three of the four subtypes, significantly outperforming an ICD-based approach to PPH subtyping for the “tone”, “tissue”, and “trauma” subtypes with binary F1 score by 50.6%, 66.5%, and 17.8%, respectively (p-value < 0.01, McNemar test; Table 3).
Discussion
Large language models (LLMs) hold immense potential to improve the administration and practice of medicine. In this study, we report the evaluation of a large language model for zero-shot phenotyping using clinical notes. As a proof-of-concept, we focused on postpartum hemorrhage, the leading cause of maternal morbidity and mortality. We developed a set of 24 postpartum-hemorrhage-related concepts, which included binary identification of a concept or value extraction of a specific measurement. We found that the Flan-T5 model extracted most concepts with high precision and recall, enabling the creation of an interpretable postpartum hemorrhage phenotype that identified significantly more deliveries with postpartum hemorrhage than would be identified by using diagnosis codes alone.
Furthermore, these granular concepts can be used for the precise and interpretable identification of the subtypes of postpartum hemorrhage based on the underlying etiology.
Interestingly, we found that the Flan-T5 model can achieve strong performance despite not being specifically trained on specialized EHR data or medical information. This is consistent with prior work that has investigated the utility of GPT-3 in performing few-shot extraction from clinical text23. The Flan-T5 performance was best for concrete concepts where the prompt could sufficiently describe how the concept might be described in a clinical note. The model was resilient to misspellings and medical abbreviations. Flan-T5 provided the greatest benefit over regular expressions on more complex concepts, such as coagulation disorders and retained products of conception, which vary in how they are documented. However, the model had lower performance when differentiating closely related concepts, such as manual extraction of the placenta and dilation and curettage, suggesting that clinical instruction-tuning or the use of few-shot exemplars may be beneficial to improve performance. The model demonstrated temporal generalizability across EHR systems for most concepts, and additional prompt-tuning on more recent notes may further improve performance.
Our proposed approach demonstrates how complex large language models can be leveraged to create downstream interpretable models. The “extract-then-phenotype” approach enables easy validation of extracted concepts and rapid updating of phenotype definitions. In this work, we chose a postpartum hemorrhage definition that was valid at the time of clinical care29. Since 2018, the definition of PPH has changed to include only those cases with blood loss of more than 1000 ml, regardless of the type of delivery26. The advantage of our approach is that in such cases, the algorithm can quickly be adapted to remain relevant.
The challenges in identifying patients with PPH are well recognized. Currently, most epidemiological studies rely on ICD diagnostic codes to develop the PPH phenotype. While ICD codes are available as structured data in EHR and many large datasets, the studies using ICD codes demonstrate an underestimation of the incidence of PPH compared to EBL7 or manual chart review30. In addition, studies have demonstrated positive predictive power of 74.5% and only 9% overall prevalence of PPH ICD codes in all patients resenting for cesarean delivery7. Zero-shot phenotyping with LLMs enabled us to rapidly identify delivery encounters with postpartum hemorrhage using clinical notes, enabling identification of PPH cases that would have been missed by PPH ICD codes. Our analysis of PPH ICD code prevalence by extracted estimated blood loss (EBL) revealed that there are many clinical notes with EBL values that meet our PPH definition, yet do not have associated PPH ICD codes. There are several possible explanations for this, including preemption of additional blood loss with appropriate medication, inaccurate EBL measurements that do not clinically correlate with the severity of the patient’s presentation, and incorrect extraction of EBL. Nevertheless, these findings underscore the limitations of traditional PPH phenotyping approaches based on claims data alone.
We also created interpretable algorithms to classify different etiology-based subtypes of PPH. This type of analysis is rarely done in other studies as all subtypes are rarely documented28. Most studies have focused on atonic PPH, which is identified based on the use of uterotonic medications, sometimes available as structured data31. In this work, drug administration was not part of the historical medical record and could not be easily retrieved. Our approach using granular concepts from clinical notes allowed for improved classification based on the presence of inadequate uterine tone even when specific medications were not mentioned. Furthermore, this approach is easily portable across institutions as evidenced by the stable performance across two different hospitals in our cohort.
The NLP model outperformed an ICD-based approach for three of the four subtypes, only underperforming on the “thrombin" subtype, which had a substantially lower prevalence of 6.3% compared to the other subtypes in our evaluation cohort. These approaches for subtyping PPH create new opportunities for the investigation of different PPH etiologies and allow for the creation of better gold-standard phenotype labels, which can be used to train models to predict future occurrence of PPH subtypes. Future work is needed to investigate the utility and feasibility of models for PPH subtype prediction.
Our work has some limitations. By focusing on discharge notes during the delivery admission, we may have missed cases of delayed or recurrent postpartum hemorrhage, which may have happened later in the postpartum period. Future work could modify the pipeline to analyze later postpartum events. The discharge notes may also reflect institution-specific clinical practices, e.g., the notes may not include some relevant elements such as estimated blood loss and the clinician’s subjective decision to administer medication or perform a procedure. To mitigate this, we selected a long study period and analyzed notes from several hospitals.
Another limitation of using Flan-T5 for phenotyping is the size of the model, which, while significantly smaller than many other LLMs, still incurs substantial computational cost. While Flan-T5 can run on a CPU, graphic processing unit (GPU) resources are needed for efficient inference. The Flan-T5-XXL model is approximately 20 gigabytes in size. In contrast, a regular expression requires trivial computational resources. A hybrid approach that leverages regular expressions and LLMs may offer the benefits of both methods. Future work could also train a clinical instruction-tuned model, which we expect can achieve comparable performance with fewer parameters32. We also did not train Flan-T5 on our phenotyping task or consider recent LLMs such as ChatGPT and GPT-4 in this work. While these models have demonstrated outstanding performance, they are closed models that can require substantial costs when run over lengthy clinical notes. We opt for evaluation of an open-sourced language model which limits security, privacy, and cost concerns. Additional studies are needed to assess whether other LLMs can further improve phenotyping performance.
Furthermore, LLMs have limitations such as hallucinations and bias. Our “extract-then-phenotype” approach allows for better interpretability, but careful attention is needed to evaluate and mitigate these limitations. Finally, we performed an initial assessment of the model’s temporal generalizability, but further validation is needed to assess performance over time and across other medical conditions.
We investigated the utility of an open-source large language model in performing interpretable, zero-shot clinical phenotyping and subtyping. This approach offers a major advantage compared to existing methods for phenotyping from clinical notes, which rely on manually annotated training data. Zero-shot phenotyping approaches have the potential to accelerate research and improve clinical operations and medicine by enabling the rapid identification of patient cohorts. These capabilities are critical for precise disease investigations and, in the future, could lead to the development of personalized medicine tools.
Methods
Cohort construction
Mass General Brigham (MGB) is an integrated healthcare system of tertiary and community hospitals and associated outpatient practices across New England. We leveraged MGB’s Research Patient Data Repository (RPDR)33 to retrieve the data for all MGB patients with a pregnancy related ICD (International Classification of Diseases) or DRG (Diagnoses Related Groups) code according to the enhanced delivery identification method34. The available data includes self-reported race and ethnicity, date of birth, insurance information, ICD and DRG codes, and EHR notes. We restricted the cohort to patients with delivery prior to 5/1/2015, when MGB transitioned to using EPIC’s electronic health record system, to enrich for delivery notes with longer narrative sections and less structured data collection.
The discharge summaries were filtered to remove duplicates, draft notes, and any notes from the emergency department. The patient’s race, ethnicity, delivery hospital, and age at delivery were extracted from Mass General Brigham’s RPDR. This study was approved by the Mass General Brigham Institutional Review Board, protocol #2020P002859, with a waiver of patient consent.
Annotation method
We extended PRAnCER (Platform Enabling Rapid Annotation for Clinical Entity Recognition)35, an annotation tool for clinical text, to collect annotations for the PPH-related concepts. During the annotation process, the annotator highlights a span of text in the note and assigns it to the corresponding label. Regular expressions are used initially to highlight potential annotations, and the annotator can confirm or reject the regex “pre-annotation". We found that this pre-annotation process can accelerate the annotation workflow and improve annotator recall. However, it does have the potential to induce over-reliance on the pre-annotations. An image of the modified annotation tool is found in Supplementary Fig. 1.
Identification of delivery discharge summaries
The discharge summaries retrieved from RPDR could pertain to any hospital admission during the time window. We compared three approaches for identifying the subset of discharge summaries that described an obstetric encounter: a regex approach, an ICD code approach, and a language modelling approach.
The first approach involved the development of a regular expression algorithm. We selected all discharge summaries containing any of the following terms: “labor “, “delivery”, “l&d”, “cesarean section”, “c-section”, “estimated edc”, or “pregnancy”. This approach was designed to optimize for recall, but it may produce false positive examples when there are discharge notes for admissions in the weeks prior and following a delivery. In the second approach, we retrieved all discharge summaries that had a pregnancy-related ICD or DRG code (and do not have an excluded code) within x days of the date of the discharge summary, where x may be 0, 2, 7, or 14 days. This time-based linking is necessary because there is no encounter linking between billing data and clinical notes in our data repository. In the final approach, we split each note into chunks containing 512 tokens and prompted Flan-T5 with the following question: “Answer the following yes/no question. Does this discharge summary note mention a woman’s delivery? note: <note>”, where <note> corresponds to the text of each chunk. If the model responded “yes” for any of the discharge summary sections, we labeled the discharge summary as related to a delivery encounter. See below methods for additional details about the Flan-T5 model.
We evaluated each of the approaches on 100 randomly sampled discharge summaries. We found that the language modelling approach yielded the highest overall performance with a macro F1 of 0.936 (Supplementary Table 4) but opted to use the regex approach for creation of the final cohort given its 100% recall.
Zero-shot natural language processing to extract PPH concepts
We utilized Flan-T5, an instruction-tuned LLM that can be applied to unseen tasks without any additional model training20, to extract PPH-related concepts from obstetric discharge summaries. Flan-T5 takes as input a prompt describing the task and generates a text output. We leverage Flan-T5 for two broad classes of tasks: binary classification and text extraction. Identification of estimated blood loss is framed as a text extraction task, and all other PPH-related concepts are framed as binary classification tasks.
We developed and evaluated the Flan-T5 models on a set of 1225 manually labelled discharge summaries with ICD codes related to PPH, as defined in Zheutlin et al.8. We performed stratified sampling to set aside 50 discharge summaries for a small development cohort to conduct minimal prompt engineering for each PPH-related concept, and the remaining 1175 discharge summaries served as our test set. Importantly, there was no overlap in patients between the development and test sets. Furthermore, we only included discharge summaries from a single MGB hospital (Brigham and Women’s Hospital) in the development set in order to evaluate the generalizability of the models to notes from other hospitals in the MGB system. We also measure the temporal generalizability of the model by evaluating on a separate sample of 100 manually labelled discharge summaries with PPH ICD codes from 2015–2022.
We performed minimal prompt engineering, constructing one to five prompts for each PPH-related concept. We selected the optimal prompt via binary F1 performance on the development set. Example prompts for PPH-related concepts are in Table 4. For the most complex concepts, such as “placenta accreta spectrum”, “PPH due to surgical causes”, “coagulation disorders with increased risk of bleeding”, and “misoprostol (used as uterotonic)”, we chained together several separate prompts to generate more nuanced predictions. If any of the prompts labeled a concept as present, we considered the concept present.
The length of discharge summaries often exceeded the max length of the input for Flan-T5 models. To address this, we split each discharge summary into text chunks of 512 tokens with a stride of 128, generated a prediction for each text chunk, and aggregated the resulting predictions. For binary classification tasks, we considered the label as positive if any of the text chunks have a positive label. For the text extraction tasks, we took the union of all segments extracted from each text chunk. We also performed post-processing to extract numbers from the generated text. This post-processing was necessary for text extraction tasks because the model can extract random text from the text chunk if a particular text chunk does not contain the information to extract (e.g., a measurement for estimated blood loss).
We experimented with Flan-T5 models of varying sizes on our development set and found that the 11 billion parameter Flan-T5-XXL model performed substantially better than the smaller models (Supplementary Table 5). All analyses in this paper use the Flan-T5-XXL model downloaded from the HuggingFace model hub at https://huggingface.co/google/flan-t5-xxl. Text was generated using greedy decoding with max new tokens set to 5 and temperature of 1.0. We performed inference using a single 16 GB RTX A4000. The Hugging Face accelerate library with DeepSpeed integration was used to speed up inference by enabling a batch size of 48 on a single GPU36.
We performed inference using Flan-T5 on all delivery-related discharge summaries for each PPH-related concept. We compared the Flan-T5 model to regular expressions constructed for each concept. Regular expressions are the most pertinent baseline because they similarly do not require model training. We compared model performance on the distinct test set of 1175 manually annotated discharge summaries.
Creation of an NLP-based PPH phenotyping algorithm
During the study period, the hospitals used a PPH definition based on the estimated blood loss (EBL) > 500 mL during a vaginal delivery or >1000 mL during a cesarean delivery29, and we leveraged the extracted PPH-related concepts to identify PPH deliveries. We focused on the phenotyping of primary PPH, as patients with secondary PPH may develop PPH after discharge29. Concretely, we identify a PPH delivery if the sum of all extracted EBL values is > 500 and the model predicts a vaginal delivery or if the model sum of all extracted EBL values is > 1000 and the model predicts a cesarean delivery.
In cases where multiple EBL were extracted with the same value, we assumed that these were multiple mentions of the same EBL in the note and did not sum the values. In cases where the extracted EBL was a single digit, we assumed the EBL was reported in liters and converted the extracted values to milliliters.
We identified PPH deliveries from our entire cohort of delivery discharge summaries and report characteristics of the identified PPH deliveries. We evaluated the positive predictive value of our approach by manually annotating the EBL and cesarean status of a random sample of 300 discharge summaries that the model predicts as describing a PPH delivery. We measured the ability of the NLP-approach to identify PPH cases missed by ICD-based definitions of PPH7,8,37 by calculating the fraction of confirmed PPH cases that have PPH-related ICD codes.
Creation of an NLP-based PPH subtyping algorithm
We used the extracted PPH-related concepts to develop four composite PPH subtyping algorithms corresponding to distinct causes of PPH: uterine atony (“tone”), retained products of conception (“tissue”), trauma (“trauma”), and coagulation abnormalities (“thrombin”)38 (Table 5). We labeled a PPH delivery with the “tone” subtype if the discharge summary contained any of the following: mention of uterine atony, administration of methylergonovine, administration of carboprost or administration of misoprostol as a uterotonic. We labeled a PPH delivery with the “tissue” subtype if the discharge summary contained any of the following: placenta accreta spectrum, retained products of conception, dilatation and curettage, or manual extraction of the placenta. We labeled a PPH delivery with the “trauma” subtype if the discharge summary contained documentation of any of the following: uterine rupture, O’Leary stitches, PPH due to surgical causes (e.g. damage to the uterine artery), or laceration with no other PPH subtype mentioned. We labeled a PPH delivery with the “thrombin” subtype if the discharge summary contained any of the following: mention of disseminated intravascular coagulation, transfusion of platelets, transfusion of cryoprecipitate, or transfusion of frozen fresh plasma in ratio with red blood cells higher than 1:1:1.
We performed subtyping on all deliveries that the NLP-based model predicted as describing postpartum hemorrhage. We validated the performance of the classification algorithms via manual chart review of the confirmed PPH deliveries identified above (See “Identification of deliveries with PPH”). We compared the NLP-based approach to a subtyping approach that leveraged ICD codes. The ICD definitions for each subtype based on conversion from ICD10 codes28 are in Table 5.
Validation of model performance
We performed manual annotation of discharge summaries to assess the performance of our models for extracting PPH-related concepts, identifying patients with PPH, and classifying subtypes of PPH. In each use case, one of four annotators with experience in reading obstetrics notes (M.R., R.F., A.G., and V.K.) first annotated the notes with the relevant PPH-related concepts or subtypes, and a clinician (V.K. and K.G.) subsequently reviewed all annotations.
Statistical analyses
We performed a McNemar test to assess whether there is a significant difference in performance between our NLP-based approach and a regular expression approach for extracting PPH-related concepts. We similarly used a McNemar test to compare the NLP-based and ICD-based approaches for subtyping PPH deliveries.
Data availability
The MGB data used in this study contains identifiable protected health information and therefore cannot be shared publicly. MGB investigators with an appropriate IRB approval can contact the authors directly regarding data access.
Code availability
The code used to run Flan-T5 and reproduce results can be found at https://github.com/EmilyAlsentzer/PPH-Extract.
References
Yu, S. et al. Toward high-throughput phenotyping: unbiased automated feature extraction and selection from knowledge sources. J. Am. Med. Inform. Assoc.: JAMIA 22, 993–1000 (2015).
Nakamaru, R. et al. Phenotyping of elderly patients with heart failure focused on noncardiac conditions: a latent class analysis from a multicenter registry of patients hospitalized with heart failure. J. Am. Heart Assoc. 12, e027689 (2023).
Bennett, W. L. et al. Patient recruitment into a multicenter clinical cohort linking electronic health records from 5 health systems: cross-sectional analysis. J. Med. Internet Res. 23, e24003 (2021).
Richesson, R. L. et al. Electronic health records based phenotyping in next-generation clinical trials: a perspective from the NIH Health Care Systems Collaboratory. J. Am. Med. Inform. Assoc.: JAMIA 20, e226–e231 (2013).
Post, A. R. et al. Temporal abstraction-based clinical phenotyping with Eureka! AMIA Ann. Symposium Proc. 2013, 1160–1169 (2013).
Denny, J. C. et al. Systematic comparison of phenome-wide association study of electronic medical record data and genome-wide association study data. Nat. Biotechnol. 31, 1102–1110 (2013).
Butwick, A. J., Walsh, E. M., Kuzniewicz, M., Li, S. X. & Escobar, G. J. Accuracy of international classification of diseases, ninth revision, codes for postpartum hemorrhage among women undergoing cesarean delivery. Transfusion 58, 998–1005 (2018).
Zheutlin, A. B. et al. A comprehensive digital phenotype for postpartum hemorrhage. J. Am. Med. Inform. Assoc.: JAMIA 29, 321–328 (2022).
Kirby, J. C. et al. PheKB: a catalog and workflow for creating electronic phenotype algorithms for transportability. J. Am. Med. Inform. Assoc.: JAMIA 23, 1046–1052 (2016).
Liao, K. P. et al. Development of phenotype algorithms using electronic medical records and incorporating natural language processing. BMJ 350, h1885 (2015).
Zeng, Z., Deng, Y., Li, X., Naumann, T. & Luo, Y. Natural language processing for EHR-based computational phenotyping. IEEE/ACM Trans. Comput. Biol. Bioinform. 16, 139–153 (2019).
Aramaki, E., Imai, T., Miyo, K. & Ohe, K. Patient status classification by using rule based sentence extraction and bm25 knn-based classifier. In i2b2 Workshop on Challenges in Natural Language Processing for Clinical Data (2006).
Sharma, H. et al. Developing a portable natural language processing based phenotyping system. BMC Med. Inform. Decis. Making 19, 78 (2019).
Chase, H. S., Mitrani, L. R., Lu, G. G. & Fulgieri, D. J. Early recognition of multiple sclerosis using natural language processing of the electronic health record. BMC Med. Inform. Decis. Making 17, 24 (2017).
Chapman, W. W., Fizman, M., Chapman, B. E. & Haug, P. J. A comparison of classification algorithms to automatically identify chest x-ray reports that support pneumonia. J. Biomed. Inform. 34, 4–14 (2001).
Yang, S., Varghese, P., Stephenson, E., Tu, K. & Gronsbell, J. Machine learning approaches for electronic health records phenotyping: a methodical review. J. Am. Med. Inform. Assoc. 30, 367–381 (2023).
Gehrmann, S. et al. Comparing deep learning and concept extraction based methods for patient phenotyping from clinical narratives. PloS One 13, e0192360 (2018).
Brown, T. B. et al. Language models are few-shot learners. In Proceedings of the 34th Annual Conference on Neural Information Processing Systems. 1877–1901 (Curran Associates, Inc, 2020).
Ouyang, L. et al. Training language models to follow instructions with human feedback. In: Advances in Neural Information Processing Systems. 27730–27744 (Curran Associates, Inc, 2022).
Chung, H. W. et al. Scaling Instruction-Finetuned Language Models. Preprint at: http://arxiv.org/abs/2210.11416 (2022).
Sivarajkumar, S. & Wang, Y. HealthPrompt: a zero-shot learning paradigm for clinical natural language processing. AMIA Ann. Symposium Proc. 2022, 972–981 (2022).
Yao, Z., Cao, Y., Yang, Z., Deshpande, V. & Yu, H. Extracting biomedical factual knowledge using pretrained language model and electronic health record context. In AMIA Annual Symposium Proceedings, vol. 2022, 1188 (American Medical Informatics Association, 2022).
Agrawal, M., Hegselmann, S., Lang, H., Kim, Y. & Sontag, D. Large Language Models are Few-Shot Clinical Information Extractors. In: Proceedings of the 2022 Conference on Empirical Methods in Natural Language Processing. 1998–2022 (Abu Dhabi, United Arab Emirates. Association for Computational Linguistics, 2022).
McInerney, D. J., Young, G., van de Meent, J.-W. & Wallace, B. C. CHiLL: Zero-shot Custom Interpretable Feature Extraction from Clinical Notes with Large Language Models. Preprint at: http://arxiv.org/abs/2302.12343 (2023).
Global Burden of Disease Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study. Lancet 388, 1775–1812 (2016).
American College of Obstetricians and Gynecologists. Practice Bulletin No. 183: Postpartum Hemorrhage. Obstetrics and Gynecology 130, e168–e186 (2017).
Corbetta-Rastelli, C. M. et al. Postpartum hemorrhage trends and outcomes in the United States, 2000–2019. Obstet. Gynecol. 141, 152–161 (2023).
Walther, D. et al. Hospital discharge data is not accurate enough to monitor the incidence of postpartum hemorrhage. PloS One 16, e0246119 (2021).
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: postpartum hemorrhage. Obstetrics and Gynecology 108, 1039–1047 (2006).
He, M. et al. Validation of algorithms to identify adverse perinatal outcomes in the Medicaid Analytic Extract database. Pharmacoepidemiol. Drug Safety 29, 419–426 (2020).
Ende, H. B. et al. Development of clinical risk-prediction models for uterine atony following vaginal and cesarean delivery. Int. J. Obstet. Anesth. 51, 103550 (2022).
Lehman, E. et al. Do we still need clinical language models? In: Proceedings of the Conference on Health, Inference, and Learning, PMLR 209, 578–597, (2023).
Nalichowski, R., Keogh, D., Chueh, H. C. & Murphy, S. N. Calculating the benefits of a research patient data repository. AMIA Ann. Symposium Proc. 2006, 1044 (2006).
Kuklina, E. V. et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Maternal Child Health J. 12, 469–477 (2008).
Levy, A. & Agrawal, M. PRAnCER, Platform enabling Rapid Annotation for Clinical Entity Recognition. Original-date: 2020-10-25. https://github.com/clinicalml/prancer (2023).
Sylvain Gugger, T. W. P. S. Z. M. S. M., Lysandre Debut. Accelerate: training and inference at scale made simple, efficient and adaptable. https://github.com/huggingface/accelerate (2022).
Goffman, D. et al. A framework for improving characterization of obstetric hemorrhage using informatics data. Obstet. Gynecol. 134, 1317–1325 (2019).
Evensen, A., Anderson, J. M. & Fontaine, P. Postpartum hemorrhage: prevention and treatment. Am. Fam. Physician 95, 442–449 (2017).
Acknowledgements
K.J.G. reports funding from NIH/NHLBI grants K08 HL146963-02, K08 HL146963-02S1, and R03 HL162756. V.P.K. reports funding from the NIH/NHLBI grants 1K08HL161326-01A1, Anesthesia Patient Safety Foundation (APSF), and BWH IGNITE Award. The funders played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
E.A. and V.K. conceptualized and designed the study. M.R., R.F., A.C., K.G., and V.K. read and annotated all clinical notes. E.A. conducted all analyses, V.K. performed validation. E.A. and V.K. drafted the manuscript, which was edited and critically reviewed by M.R., R.F., A.C., B.B., K.G., and D.B. Mass General Brigham was the source of data and location for all analyses. All authors read and approved the final manuscript and had final responsibility for the decision to submit it for publication.
Corresponding author
Ethics declarations
Competing interests
K.J.G. has served as a consultant to Illumina Inc., Aetion, Roche, and BillionToOne outside the scope of the submitted work. D.W.B. reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from Valera Health, equity from CLEW, equity from MDClone, personal fees and equity from AESOP Technology, personal fees and equity from FeelBetter, and grants from IBM Watson Health, outside the submitted work. V.P.K. reports consulting fees from Avania CRO unrelated to the current work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alsentzer, E., Rasmussen, M.J., Fontoura, R. et al. Zero-shot interpretable phenotyping of postpartum hemorrhage using large language models. npj Digit. Med. 6, 212 (2023). https://doi.org/10.1038/s41746-023-00957-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-023-00957-x
This article is cited by
-
Disease progression strikingly differs in research and real-world Parkinson’s populations
npj Parkinson's Disease (2024)