Abstract
Technological advancements facilitate feedback adaptation in rehabilitation through virtual reality (VR) exergaming, serious gaming, wearables, and telerehabilitation for older adults fall prevention. Although studies have evaluated these technologies, no comparisons of their effectiveness have been conducted to date. Thus, this study aims to assess the differences in effectiveness of these interventions on balance and functional mobility in the older adults. A systematic review and network meta-analysis (NMA) were conducted to identify the most effective interventions for improving balance and functional mobility in adults aged 60 and over. The search was conducted in five databases (PubMed, Embase, Cochrane Central Register of Controlled Trials, Scopus, and Web of Science) up to June 10, 2023. The eligibility criteria were: (1) older adults, (2) functional mobility, balance, or gait as the primary outcome, (3) new technology intervention, and (4) randomized study design. New technology interventions were classified into five categories: exergaming with balance platforms or motion capture technologies, other serious gaming, interventions with wearables, and telerehabilitation. Additionally, two categories of control interventions (conventional exercises and no treatment) were extracted. The NMA was performed for the aggregated results of all outcomes, and separately for clinical functional scales, functional mobility, and gait speed results. Fifty-two RCTs with 3081 participants were included. Exergaming with motion capture was found to be statistically significant in producing a better effect than no treatment in the analysis of the functional mobility with an SMD of −0.70 (P < 0.01). The network meta-analysis revealed that exergaming with motion capture offers greater therapeutic benefits for functional mobility and balance compared to no treatment control. The effectiveness of this approach is similar to that of conventional exercises. Further RCTs are needed to provide a more definitive conclusion, particularly with respect to the effectiveness of serious games, telerehabilitation, and interventions with wearables.
Similar content being viewed by others
Introduction
According to the projections of the United Nations World Population Prospects, by 2050, one in four people living in Europe and Northern America will be 65 years or older1. Among the numerous challenges associated with an aging population are those related to falls and the resultant consequences. The World Health Organization reports that every year, between 28 and 35% of seniors aged 65 and above fall, and this rate increases to between 32 and 42% for individuals over 70 years old2. Data indicate that falls are the leading cause of both fatal and non-fatal unintentional injuries for this group of people3.
Accordingly, extensive studies have been conducted to discover effective forms of balance enhancement, thereby reducing the risk of falls. Approaches such as exercise, assistive technology, examination and adjustments to the environment, and the implementation of quality improvement strategies, have all been demonstrated to be valuable components of fall prevention programs4. A supplementary mechanism that could be utilized in balance training is feedback. It is a form of sensory augmentation in which information regarding the output or result of a system is utilized to modify or regulate the input or future behavior of that same system. In medical research, augmented feedback is used to induce enduring changes in motor learning and attain superior performance5. For balance training, augmented feedback is most commonly provided in the form of visual displays, tactile and kinesthetic perception stimuli, or a combination of these modalities6,7.
Technological advancements in wearables and virtual reality (VR) have facilitated the integration of feedback in rehabilitation medicine. Multiple studies have been conducted to investigate the efficacy of combining various forms of VR with feedback to enhance postural stability and balance8. For instance, visual feedback has been utilized in various force plates used in exergaming. These devices transfer the center of pressure (COP) record to the screen in real-time, allowing the patient to control and adjust the COP’s displacement9. Another mechanism frequently utilized in exergaming is motion capture. It is a method used to capture the movements of the participant and convert them into a digital (on screen) representation of the motion, thus providing visual feedback and enabling real-time correction of the exercises performed10. The advantage of exergaming is the accessibility of equipment and commercially available game software; however, its effectiveness may be limited as it is not specifically designed for rehabilitation purposes. Hence, researchers are developing specialized software called ‘serious games’ that target special interest groups by combining the desired and measurable outcomes (serious aspect), in-game functional messaging, skills learning and entertainment (game aspect) simultaneously11. Telerehabilitation, which has recently gained wider recognition, can also provide visual feedback, particularly through the use of inertial sensors12. These sensors, when employed as wearable technology, can also provide haptic feedback that can be used for posture adjustments13.
The efficacy of the previously mentioned mechanisms for balance training has been separately evaluated in numerous systematic reviews and meta-analyses; however, no study has directly compared their effectiveness to each other14,15,16,17,18,19. Therefore, the main aim of this study was to quantitatively evaluate the differences in the effectiveness of virtual reality exergaming, serious gaming, interventions with wearables, and telerehabilitation compared to conventional treatments or no treatment on balance and functional mobility in the older adults. Additionally, this study aimed to assess the acceptability of interventions based on new technologies for functional rehabilitation.
Our study’s key findings reveal that VR exergaming incorporating motion capture technology yields substantial improvements in functional mobility and balance among older adults, similar to conventional exercises. This intervention proves more effective than exergaming with balance boards, serious games, wearables, and telerehabilitation. When assessing dropout rates, new technologies demonstrated comparable patient acceptability to the control group, although the pooled results indicated control interventions exhibited a statistically significant 2-percentage-point lower rate.
Results
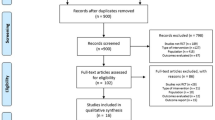
The flow of the study’s identification and selection process is shown in Fig. 1. The systematic search yielded 1619 records, of which 779 remained after removing duplicates and screening titles and abstracts. Following the initial screening procedure, 92 articles were considered for the full-text review. After a full-text assessment, 55 RCTs involving 3273 enrolled participants were included in the NMA (Fig. 1).
Characteristics of the included studies
Among the included studies, exergaming with balance platforms20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41 (n = 22, total participants: 1084) and motion capture42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58 (n = 17, total participants: 912) were the most frequently investigated interventions. Seven studies (total participants: 452) examined the use of other serious games59,60,61,62,63,64,65, four studies (total participants: 98) examined interventions with wearables66,67,68,69, and three studies (participants: 619) investigated telerehabilitation70,71,72. Two studies could not be classified into either group as it involved an intervention with the Nintendo Switch console73,74.
The sample size of the individual trials ranged from 12 to 503 participants, with a mean sample size of 58. All studies reported the mean ages of participants, which ranged from 63.3 to 86.2 (mean age: 73.7 years old). The total amount of therapy varied among the studies, ranging from 6 to 52 sessions (mean 23.6) of practice spread over a mean training period of 8.1 weeks (range 2–104 weeks), with a mean session duration of 48.9 min (range 15–60 min). The average sample size for exergaming with a balance board was 48.9 participants with a mean age of 74.8 years. Participants attended an average of 18.9 sessions, spread over 7.9 weeks, each lasting 39.6 min on average. For exergaming with motion capture, the mean sample size was 54 participants (mean age: 71.2), the mean number of sessions was 23.8, the mean number of weeks was 7.6, and the mean session length was 43 min. The mean sample size for other serious games interventions was 65 participants (mean age: 75.5) with an average of 20.9 sessions conducted over 8.1 weeks and lasted 41 min each. For interventions with wearables, the average sample size was 24 participants with a mean age of 77.4, who participated in 26 sessions over 7.6 weeks with an average session length of 43 min. For telerehabilitation, the mean sample size was 206 participants (mean age: 70.7), the mean number of sessions was 34.5, the mean number of weeks was 42.3 and the mean session length was 40 min. The study characteristics are summarized in Supplementary Table 1.
Assumption assessment results
The studies included in Network 1 (All Outcomes) showed considerable heterogeneity, with a value of I2 = 49.6% (CI 33.6%; 60.8%). The heterogeneity test conducted for Network 2 (Functional Scales) and Network 3 (TUG) in the NMA resulted in I2 values of 56.6% (CI 26.5%; 74.4%) and 68.9% (CI 53.1%; 79.4%), respectively. However, for Network 4 (Gait Speed), the results did not support consistency, as indicated by a high heterogeneity of I2 = 97.7% (CI 96.5%; 98.5%). Since the results did not meet the NMA assumptions, they were not presented here. Nevertheless, they are included as Supplementary Information, along with a detailed description of the assumptions assessment results (Supplementary Figs. 2, 3).
NMA results and ranking of the treatments
Figure 2 illustrates the network plot for each of the selected network analyses. The main result of the NMA was that exergaming with motion capture was found to be on the verge of statistical significance in producing a better effect than no treatment in Network 1 (All Outcomes), with a SMD of −0.16 (CI −0.33; 0.01, P = 0.06), and statistically significant in Network 3 (TUG), with a SMD of −0.70 (CI −1.16; −0.23, P < 0.01) (Table 1). However, the interventions did not yield significantly better response rates than conventional exercises in each of the selected networks, with 95% confidence intervals not crossing the null (Fig. 3). Supplementary Table 2 contains total direct and indirect effect estimates.
In terms of ranking, Network 1 (All Outcomes) found that exergaming with motion capture (P-score of 72%) had a similar probability to produce therapeutic benefits as conventional exercises (71%) (Table 1). Other serious games (55%), exergaming with a balance platform (48%), interventions with wearables (45%), and telerehabilitation (43%) were found to be better treatments in the network than no treatment (16%). In Network 2 (functional scales), the P-score obtained by each intervention was similar to no treatment (43%), and below conventional exercises (75%). In Network 3 (TUG), exergaming with motion capture (89%) and balance platform (58%) had P-scores above conventional exercises (55%). On the other hand, other serious games, telerehabilitation, and interventions with wearables had P-scores similar or lower than no treatment (42%, 37%, and 18%, respectively).
Acceptability: drop-out analysis
A total of 51 trials, derived from 45 studies, were included in the proportional drop-out meta-analysis. When considering all pooled treatments among 2613 participants, 324 dropouts were reported, resulting in a prevalence of 12.4% (CI 8.4%; 13.4%). The dropout rate for technology-based interventions was 13.5% (CI 11.1%; 15.8%), compared to 11.3% (CI 9.1%; 14.1%) for the CE control group. The main findings indicated a significant difference, resulting in slightly higher probability of drop-out in technology-based interventions than in the CE group (OR = 1.22; CI 1.03; 1.45; P = 0.03) (Supplementary Fig. 4). No significant heterogeneity was found between the studies (I2 = 0.0%; CI 0.0%; 79.2%; P = 0.90). There were no statistically significant differences when comparing drop-out rate within technology-based interventions.
Risk of bias assessment
Figure 4 illustrates the results of the risk of bias assessment. Thirty-two percent (18 out of 55), 24% (13 out of 55), and 44% (24 out of 55) of the studies had a low, some concerns, and high overall risk of bias, respectively. One in three studies had some concerns about the risk of bias for allocation concealment (i.e., concealment method not described or insufficient detail to allow judgment). Furthermore, 21 studies (38%) had some concerns or a high risk of bias for selective outcome reporting, mainly due to incomplete or missing data necessary to conduct the NMA. Considering the analysis of the interventions, the level of risk of bias was found to be similar across them. In the studies included, exergaming with a balance platform had a high risk of bias of 45%, motion capture had 47%, other serious games had 42%, interventions with wearables had 25%, and telerehabilitation had 33%.
Discussion
The primary objective of this study was to conduct a quantitative evaluation of the disparities in effectiveness between new technology interventions and conventional treatments, or no treatment at all, with regard to balance and functional mobility in the older adults. The main finding of this study was that exergaming with motion capture was found to be significantly more effective than no treatment in improving balance and functional mobility in the older adults. Additionally, in terms of ranking, exergaming with motion capture was comparable to conventional exercises, particularly in the context of Network 1 (All Outcomes), and superior to conventional exercise in Network 3 (TUG). However, no statistically significant differences were observed between the other interventions and either conventional exercise or no treatment.
The superiority of exergaming with motion capture over other new technology interventions can be attributed to its ability to provide comprehensive feedback to the patient. This intervention entails a visual representation of the patient’s entire body on the screen, thereby facilitating greater mobility that more closely reflects activities performed during balance functional scales and functional mobility tests. Conversely, exergaming with a balance platform relies on feedback using the COP, which restricts mobility to the patient’s stability limits. As a consequence, this approach may hinder the transfer of motor skills acquired during training to functional test results. Given that augmented feedback is a crucial element of motor learning, a more comprehensive feedback mechanism has the potential to enhance the translation of these skills into clinical functioning5. A meta-analysis from 2020 produced comparable outcomes to no treatment, however, the analysis was conducted on exergaming as a collective whole and did not specify the effectiveness of individual technologies75. In 2016, Donath and colleagues conducted a study comparing exergaming to conventional balance training, and obtained outcomes similar to ours, ultimately concluding that traditional exercise is marginally superior76. A recent meta-analysis examining both conventional exercises and no-exercise as a control interventions concluded that exergaming has the potential to improve specific physical function domains in older adults77. However, none of the previously mentioned meta-analyses differentiated motion capture and balance platform as separate forms of exergaming.
It is noteworthy that serious games, which are software programs explicitly designed for rehabilitation purposes, exhibit lower effectiveness than anticipated. Considering their purposeful design and intended functions, it would be reasonable to expect a higher degree of efficacy. Although meta-analyses have investigated the effectiveness of serious games in enhancing cognitive functions among older adults, no such analysis has assessed their efficacy in improving balance and functional mobility in the older adults78. This research gap could potentially be attributed to the primary application of serious games in treating neurological diseases79,80,81. Similarly, in our study, interventions involving wearables did not demonstrate significantly higher effectiveness in augmenting balance. This outcome may be related to the fact that such devices often employ custom-made software, which exhibit considerable diversity in their approaches, consequently leading to inconsistent results. In a recent systematic review on the application of eHealth interventions in balance treatment, Gaspar and Lapão (2020) reported that the employed methodologies did not allow for a definitive comparison of the results, and they recommended more rigorous investigations16. The aforementioned findings regarding serious games and wearable interventions should be interpreted within the context of their costs. A recent study examining the costs of an off-the-shelf exergame intervention in patients with heart failure demonstrated relatively low costs, and it was observed that patients were willing to cover more than half of the intervention expenses82. In contrast, the development and ongoing software updates of a serious game program can be financially demanding and resource-intensive, involving multiple stakeholders such as experts, game developers, and software engineers83,84.
Furthermore, when comparing the drop-out rate within new technologies, we provided evidence that each of them is equally acceptable to patients as the control group. However, considering the pooled acceptability results, the control interventions exhibited a statistically significant 2-percentage-point lower drop-out rate than the new technology interventions. This difference can be attributed to the fact that advanced age can influence the acceptability of using new technologies85. Additionally, Chen et al. (2018) demonstrated that perceived playfulness and perceived usefulness are two primary factors influencing seniors’ willingness to engage in exergames86. In light of the obtained results, the latter factor appears to be particularly significant because, compared to conventional professional-guided exercises, commercial games may not be perceived as equally useful as standard exercises. These results differ slightly from a 2018 systematic review that concluded that technology-based exercise interventions have similar adherence to traditional exercise programs87. However, it is worth noting that the review employed a qualitative analysis method and included less than half the number of articles compared to this NMA.
Exergaming, particularly the type that incorporates motion capture technology, can offer patients an accessible way to engage in feedback-based exercises without requiring professional supervision. The benefits of accessibility render exergaming a viable intervention for enhancing balance and functional mobility among older adults. Therefore, it is reasonable to consider the deployment of this type of intervention as either a standalone treatment or as a complementary measure alongside traditional rehabilitation programs. In addition to its clinical effectiveness, exergaming has been found to be a safe form of exercise, exhibiting minimal to no adverse effects88. The confluence of this study results, coupled with its safety and potential efficacy in enhancing the cognitive capabilities of older adults, positions exergaming with motion capture technology as a compelling therapeutic tool that may prove valuable in nursing home settings or for individual use by older persons in their homes. Serious games offer a primary advantage of greater individualization, making them particularly suitable for personalized medicine. Similarly, interventions involving wearables provide the same advantage, along with enhanced convenience and accessibility. Conversely, telerehabilitation holds a distinct advantage in its ability to deliver services remotely. This characteristic allows for increased access to specialized rehabilitation expertise and ensures continuity of care, particularly for individuals residing in remote or underserved areas.
A crucial factor in evaluating the effectiveness of an intervention is its dose, which includes elements such as frequency, intensity, duration, and timing89. However, the number of intervention sessions conducted varied significantly among the articles analyzed in this study. This difference is important since the number of interventions can impact the therapy’s effectiveness and, consequently, the results of the meta-analysis. To enhance the comparability of studies, future research should focus on identifying the appropriate number of sessions, their duration, and the weeks of intervention. This is particularly important for interventions that are self-directed and conducted by the patient at home without therapist supervision. Given the substantial variability and customization of software utilized in serious games, wearables interventions, and telerehabilitation, it is imperative to evaluate the cost-effectiveness of these interventions, especially when compared to commercially available exergames. However, more studies evaluating the efficacy of these interventions are needed as the current body of research is limited. Furthermore, most of the studies conducted so far have employed clinical functional scales, and it would be valuable to enhance future research efforts by incorporating measurements of COP and conducting 3D gait analyses. Another area worth exploring is the comprehensive implementation of the gamification process, which involves incorporating competitive elements like points or leaderboards. Senior users, particularly in the health domain, could potentially benefit from gamification, and a full adoption of this approach may lead to increased engagement in interventions and a reduction in the dropout rate90. Finally, the use of the Nintendo Switch in the field of exergaming is worth exploring. Although there has been little research done on this topic so far, the device offers additional accessories that enable feedback during resistance, aerobic, and balance exercises91.
There are several limitations to consider when interpreting the obtained results. One major limitation is the small number of studies included in some interventions, such as wearables (4 studies) and telerehabilitation (3 studies), as well as the presence of small sample sizes in some studies, which may have resulted in less robust quantitative findings. Additionally, the RCTs had varying intervention durations, ranging from 6 to 52 sessions, and the studies in the current NMA had relatively short follow-up durations, with an average follow-up of 8 weeks (excluding telerehabilitation). Moreover, except for telerehabilitation, the average number of participants per study was low, ranging from 24 to 65. The interpretation of the results is significantly constrained due to the presence of risk of bias. Only 32% of the included studies received a low risk-of-bias assessment. Specifically, when considering exergaming with motion capture, the proportion of studies categorized as low risk was 29%, while a considerable 47% were classified as high risk. Another limitation is the combining of all types of control exercises into a single category of “conventional exercises” and interventions without exercises into a single category of “no treatment”, which prevented quantification of the comparative effectiveness of specific interventions within the same category. In Network 4 (Gait Speed) analysis, the data failed to meet the assumptions of statistical analysis due to a high degree of heterogeneity among the included studies, rendering the results inconclusive. Lastly, a significant number of studies reported results as median and IQR, which had to be transformed into mean and SD for use in NMA. Although this transformation is commonly used, it can potentially distort the results obtained.
Based on the results of this network meta-analysis, exergaming incorporating motion capture technology may provide therapeutic benefits for functional mobility and balance compared to no treatment control, exhibiting comparable effectiveness to conventional exercises. However, the interpretation of the results is significantly constrained by the presence of risk of bias, with only 32% of the included studies receiving a low risk-of-bias assessment. Additional high quality RCTs are required to draw a more definitive conclusion, particularly concerning the effectiveness of other serious games, telerehabilitation, and interventions involving wearables. This could lead to the identification of quantitative and objective tools to aid balance treatment in fall prevention programs. It is also crucial in terms of supplementing these programs with interventions that patients can perform at home without therapist supervision, potentially improving functional mobility and reducing the risk of falls.
Methods
Design
In order to jointly estimate the relative effectiveness of different treatments provided to patient, this study was designed as a systematic review with network meta-analysis (NMA). We combined direct evidence, i.e., that directly observable from the selected studies, and indirect evidence, i.e., that obtained through one or more common comparators92. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses 2020 and AMSTAR2 guidelines93,94. The review protocol was registered a priori in the PROSPERO database (CRD42022376092).
Literature search and study selection
MEDLINE (via PubMed), Embase, Cochrane Central Register of Controlled Trials, Scopus, and Web of Science databases were searched up to June 10, 2023. Please see the Supplementary Information for full search strategy used in the databases.
Studies identified from search databases were assessed by two independent authors (JM and AW) according to the following eligibility criteria: (1) targeted participants were limited to healthy older adults (aged 60 years or older); (2) functional mobility, balance, or gait specified as the primary outcome measure; (3) intervention defined as virtual reality exergaming, other serious gaming, interventions with wearables, or telerehabilitation, with at least one control group in the trial (eligible comparators included no treatment, usual care, conventional rehabilitation, exercises, or unrelated interventions); and (4) studies with a randomized design. Studies were excluded if the targeted participants were restricted to specialized populations (with neurodegenerative diseases, neurological, orthopedic, or pulmonary disorders, and cancers). Studies were also excluded if the intervention included robotic or exoskeleton devices.
The primary outcomes were changes for functional mobility, balance in the scores of the rating scales and for gait in gait speed after the interventions. Outcomes were measured using the Timed Up and Go test (TUG), Center of Pressure (COP), Berg Balance Scale (BBS), Short Physical Performance Battery (SPPB), Five-Time Sit to Stand Test (5XSST), Functional Reach Test (FRT), Single Leg Stance (SLS), Fullerton Advanced Balance Scale (FAB), Overall Stability Index (OSI), Tinetti Performance Oriented Mobility Assessment (POMA), and Mini-Balance Evaluation Systems Test (Mini-BESTest). The secondary outcome was acceptability, measured as the dropout rate (defined as leaving the study before its end for any reason).
The studies retrieved by the search strategy, along with study information and abstract text, were imported into the Systematic Review Assistant-Deduplication Module for de-duplication95. Articles were divided between two reviewers (JM and AW), with each title and abstract independently screened using Rayyan AI software96. After the initial literature search was conducted, BC and PK retrieved and independently screened the full-text articles. Conflicts over inclusion were resolved through discussions. Data were extracted by a single reviewer (BC) and checked by JSzG.
Data extraction
From each study, we extracted the following information: the number of participants included (along with the average age), the number of sessions of the intervention received and the length of a single session, the outcome measures used, the number of dropouts in the groups, and the study conclusion.
New technology interventions were classified into 5 categories: (1) exergaming with balance platform, including all kinds of devices which could provide feedback though stepping on it; (2) virtual reality exergaming with motion capture, defined as a device which could provide feedback via recording the movement; (3) other serious gaming, including all kinds of devices and software’s created for rehabilitation purposes; (4) interventions with wearables, including mobile phones and wearables; (5) telerehabilitation (including all forms of remote support aimed at balance and functional mobility training). Additionally, we extracted two categories of control interventions: (6) conventional rehabilitation, including all forms of traditional rehabilitation, physical exercises, and treatment as usual; and (7) no treatment (defined as no intervention or interventions without physical exercises, such as education and cognitive training).
Quality assessment
Two authors (JM and AW) independently assessed the quality of the included studies using version 2 of the Cochrane risk of bias tool for randomized trials (RoB2), with any disagreements resolved by a third researcher (BC)97. The bias risk assessment included seven criteria: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases.
Data analysis
The analyses were carried out with R Studio v4.2.2 software with the netmeta package for frequentist analysis. For each study that presented pre- and post-treatment mean and standard deviation values, the Standardized Mean Difference (SMD) and Standard Error (SE) were calculated both within and between treatment groups. When the studies provided median values and quartiles of the distribution, the SMD and SE values were calculated, first calculating the pre- and post-treatment mean and standard deviation values for each group. The frequentist weighted least squares approach was applied to the network meta-analysis with random model. For each treatment comparison, the direct and indirect effect, associated with the 95% confidence interval (95% CI), were estimated. The data analysis was performed for four outcome sets. Network 1 (All Outcomes) represents the aggregated results of all balance related outcomes (COP, BBS, SPPB, FAB, POMA, Mini-BESTest, 5xSST, FRT, SLS, and TUG), Network 2 (Functional Scales) comprises the clinical functional scales, including BBS, SPPB, FAB, POMA, and Mini-BESTest. Network 3 (TUG) encompasses the functional mobility results based on the TUG test, while Network 4 (Gait Speed) includes the results of quantitative gait speed analysis. Heterogeneity between studies was assessed using generalized Cochran’s Q statistic (Supplementary Fig. 2). In addition, the I-square inconsistency index (I2) was used to quantify the percentage of variability among studies due to heterogeneity rather than chance. Heterogeneity was calculated both within (Qw) and between (Qb) studies. A significant Q value (PQ < 0.05) indicates a lack of homogeneity of results among studies. The hypothesis of consistency between designs was tested by performing a generalized between-designs Cochran’s Q statistic. The significance of the difference between effect estimates based on direct and indirect evidence (P < 0.05) was an indication of significant disagreement (inconsistency). The change of the inconsistency contribution of single designs has been investigated in more detail by the Net Heat plot and Net splitting method. Finally, the comparative advantages of the treatments were investigated, calculating P-score values, i.e., the cumulative probability that treatments with the highest priority and those with the lowest priority are selected. To test whether the probability of dropout was higher in the treatment or control group, a binary meta-analysis based on odds ratios (OR) was conducted. The statistical significance was set at α < 0.05.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The search strategy is available in the Supplementary Information, and any additional data are available on reasonable request to the corresponding author.
References
Population Division of the United Nations Department of Economic and Social Affairs. World Population Prospects 2019: Highlights. https://www.ined.fr/fichier/s_rubrique/29368/wpp2019_10.key.findings_embargoed.version.en.pdf (2019).
World Health Organization. WHO global report on falls prevention in older age. Ageing Life Course Fam. Community Health WHO Glob. Rep. Falls Prev. Older Age (2008).
Hu, G. & Baker, S. P. Recent increases in fatal and non-fatal injury among people aged 65 years and over in the USA. Inj. Prev. 16, 26–30 (2010).
Dautzenberg, L. et al. Interventions for preventing falls and fall-related fractures in community-dwelling older adults: a systematic review and network meta-analysis. J. Am. Geriatr. Soc. 69, 2973–2984 (2021).
Moinuddin, A., Goel, A. & Sethi, Y. The role of augmented feedback on motor learning: a systematic review. Cureus 13, e19695 (2021).
Williams, A. D. & Vette, A. H. A vibrotactile feedback device for seated balance assessment and training. J. Vis. Exp. JoVE https://doi.org/10.3791/58611 (2019).
Oungphalachai, T. & Siriphorn, A. Effects of training with a custom-made visual feedback device on balance and functional lower-extremity strength in older adults: a randomized controlled trial. J. Bodyw. Mov. Ther. 24, 199–205 (2020).
Baragash, R. S., Aldowah, H. & Ghazal, S. Virtual and augmented reality applications to improve older adults’ quality of life: a systematic mapping review and future directions. Digit. Health 8, 20552076221132100 (2022).
Takeda, K. et al. Adaptation effects in static postural control by providing simultaneous visual feedback of center of pressure and center of gravity. J. Physiol. Anthropol. 36, 31 (2017).
Scott, B., Seyres, M., Philp, F., Chadwick, E. K. & Blana, D. Healthcare applications of single camera markerless motion capture: a scoping review. PeerJ 10, e13517 (2022).
Caserman, P. et al. Quality criteria for serious games: serious part, game part, and balance. JMIR Serious Games 8, e19037 (2020).
Picerno, P. et al. Wearable inertial sensors for human movement analysis: a five-year update. Expert Rev. Med. Devices 18, 79–94 (2021).
Lind, C. M., Diaz-Olivares, J. A., Lindecrantz, K. & Eklund, J. A wearable sensor system for physical ergonomics interventions using haptic feedback. Sensors 20, 6010 (2020).
Alhasan, H., Alshehri, M. A., Wheeler, P. C. & Fong, D. T. P. Effects of interactive videogames on postural control and risk of fall outcomes in frail and pre-frail older adults: a systematic review and meta-analysis. Games Health J. 10, 83–94 (2021).
Chen, Y., Zhang, Y., Guo, Z., Bao, D. & Zhou, J. Comparison between the effects of exergame intervention and traditional physical training on improving balance and fall prevention in healthy older adults: a systematic review and meta-analysis. J. Neuroeng. Rehabil. 18, 164 (2021).
Gaspar, A. G. M. & Lapão, L. V. eHealth for addressing balance disorders in the elderly: systematic review. J. Med. Internet Res. 23, e22215 (2021).
Truijen, S. et al. Effect of home-based virtual reality training and telerehabilitation on balance in individuals with Parkinson disease, multiple sclerosis, and stroke: a systematic review and meta-analysis. Neurol. Sci. J. Ital. Neurol. Soc. Ital. Soc. Clin. Neurophysiol. 43, 2995–3006 (2022).
Ren, Y. et al. Effectiveness of virtual reality games in improving physical function, balance and reducing falls in balance-impaired older adults: a systematic review and meta-analysis. Arch. Gerontol. Geriatr. 108, 104924 (2023).
Chen, P.-J., Hsu, H.-F., Chen, K.-M. & Belcastro, F. VR exergame interventions among older adults living in long-term care facilities: a systematic review with Meta-analysis. Ann. Phys. Rehabil. Med. 66, 101702 (2023).
Benitez-Lugo, M.-L., Suárez-Serrano, C., Galvao-Carmona, A., Vazquez-Marrufo, M. & Chamorro-Moriana, G. Effectiveness of feedback-based technology on physical and cognitive abilities in the elderly. Front. Aging Neurosci. 14, (2022).
Hou, H.-Y. & Li, H.-J. Effects of exergame and video game training on cognitive and physical function in older adults: a randomized controlled trial. Appl. Ergon. 101, 103690 (2022).
Kim, S.-H. & Cho, S.-H. Benefits of virtual reality program and motor imagery training on balance and fall efficacy in isolated older adults: a randomized controlled trial. Med. Kaunas. Lith. 58, 1545 (2022).
Khanmohammadi, R. et al. The effect of video game-based training on postural control during gait initiation in community-dwelling older adults: a randomized controlled trial. Disabil. Rehabil. 44, 5109–5116 (2022).
Sonthikul, C., Hadhoh, N., Madeeyoh, N., Ponlakarn, A. & Dolthamsiri, N. Comparative effect of core stabilization exercise and active video gaming on dynamic balance in elderly female people: a single-blind randomized controlled clinical trial. J. Health Sci. Med. Res. 40, 53–65 (2022).
Gallardo-Meza, C. et al. Effects of 4 weeks of active exergames training on muscular fitness in elderly women. J. Strength Cond. Res. 36, 427–432 (2022).
Fakhro, M. A., Hadchiti, R. & Awad, B. Effects of Nintendo Wii fit game training on balance among Lebanese older adults. Aging Clin. Exp. Res. 32, 2271–2278 (2020).
Morat, M. et al. Effects of stepping exergames under stable versus unstable conditions on balance and strength in healthy community-dwelling older adults: a three-armed randomized controlled trial. Exp. Gerontol. 127, 110719 (2019).
Lim, J., Cho, J.-J., Kim, J., Kim, Y. & Yoon, B. Design of virtual reality training program for prevention of falling in the elderly: a pilot study on complex versus balance exercises. Eur. J. Integr. Med. 15, 64–67 (2017).
Padala, K. P. et al. Efficacy of Wii-Fit on static and dynamic balance in community dwelling older veterans: a randomized controlled pilot trial. J. Aging Res. 2017, (2017).
Kwok, B. C. & Pua, Y. H. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: a randomised control trial. Age Ageing 45, 621–628 (2016).
Schattin, A., Arner, R., Gennaro, F. & de Bruin, E. D. Adaptations of prefrontal brain activity, executive functions, and gait in healthy elderly following exergame and balance training: a randomized-controlled study. Front. Aging Neurosci. 8, 278 (2016).
Eggenberger, P., Schumacher, V., Angst, M., Theill, N. & de Bruin, E. D. Does multicomponent physical exercise with simultaneous cognitive training boost cognitive performance in older adults? A 6-month randomized controlled trial with a 1-year follow-up. Clin. Interv. Aging 10, 1335–1349 (2015).
Whyatt, C., Merriman, N. A., Young, W. R., Newell, F. N. & Craig, C. A Wii bit of fun: a novel platform to deliver effective balance training to older adults. Games Health J. 4, 423–433 (2015).
Bieryla, K. A. & Dold, N. M. Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin. Interv. Aging 8, 775–781 (2013).
Jorgensen, M. G., Laessoe, U., Hendriksen, C., Nielsen, O. B. F. & Aagaard, P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: a randomized controlled trial. J. Gerontol. Ser. -Biol. Sci. Med. Sci. 68, 845–852 (2013).
Singh, D. K. A. et al. Effects of balance-focused interactive games compared to therapeutic balance classes for older women. Climacteric 16, 141–146 (2013).
Franco, J. R., Jacobs, K., Inzerillo, C. & Kluzik, J. The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol. Health Care 20, 95–115 (2012).
Pichierri, G., Murer, K. & de Bruin, E. D. A cognitive-motor intervention using a dance video game to enhance foot placement accuracy and gait under dual task conditions in older adults: a randomized controlled trial. Bmc Geriatr. 12, 74 (2012).
Pluchino, A., Lee, S. Y., Asfour, S., Roos, B. A. & Signorile, J. F. Pilot study comparing changes in postural control after training using a video game balance board program and 2 standard activity-based balance intervention programs. Arch. Phys. Med. Rehabil. 93, 1138–1146 (2012).
Rendon, A. A. et al. The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 41, 549–552 (2012).
Toulotte, C., Toursel, C. & Olivier, N. Wii Fit (R) training vs. adapted physical activities: which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin. Rehabil. 26, 827–835 (2012).
Alemrany, A. M., Badr, N. M., Farghaly, A. A., & Abed El Ghaffar, H. A. Effect of virtual reality training on risk of falls and quality of life among elderly. Fizjoterapia Pol. 21, 138–143 (2021).
Babadi, S. Y. & Daneshmandi, H. Effects of virtual reality versus conventional balance training on balance of the elderly. Exp. Gerontol. 153, 111498 (2021).
de Lima, B. E., Passos, G. S., Youngstedt, S. D., Bandeira Santos Junior, L. C. & Santana, M. G. Effects of Xbox Kinect exercise training on sleep quality, anxiety and functional capacity in older adults. J. Bodyw. Mov. Ther. 28, 271–275 (2021).
Moreira, N. B., Rodacki, A. L. F., Costa, S. N., Pitta, A. & Bento, P. C. B. Perceptive-cognitive and physical function in prefrail older adults: exergaming versus traditional multicomponent training. Rejuvenation Res. 24, 28–36 (2021).
Sadeghi, H. et al. Effects of 8 weeks of balance training, virtual reality training, and combined exercise on lower limb muscle strength, balance, and functional mobility among older men: a randomized controlled. Trial Sports Health- Multidiscip. Approach 13, 606–612 (2021).
Chen, P.-J., Penn, I.-W., Wei, S.-H., Chuang, L.-R. & Sung, W.-H. Augmented reality-assisted training with selected Tai-Chi movements improves balance control and increases lower limb muscle strength in older adults: a prospective randomized trial. J. Exerc. Sci. Fit. 18, 142–147 (2020).
Yang, C.-M., Chen Hsieh, J., Chen, Y.-C., Yang, S.-Y. & Lin, H.-C. K. Effects of Kinect exergames on balance training among community older adults a randomized controlled trial. Med. (Baltim.) 99, e21228 (2020).
Phirom, K., Kamnardsiri, T. & Sungkarat, S. Beneficial effects of interactive physical-cognitive game-based training on fall risk and cognitive performance of older adults. Int. J. Environ. Res. Public. Health 17, 6079 (2020).
Bacha, J. M. R. et al. Effects of kinect adventures games versus conventional physical therapy on postural control in elderly people: a randomized controlled trial. Games Health J. 7, 24–36 (2018).
Htut, T. Z. C., Hiengkaew, V., Jalayondeja, C. & Vongsirinavarat, M. Effects of physical, virtual reality-based, and brain exercise on physical, cognition, and preference in older persons: a randomized controlled trial. Eur. Rev. Aging Phys. Act. 15, 10 (2018).
Ordnung, M., Hoff, M., Kaminski, E., Villringer, A. & Ragert, P. No overt effects of a 6-week exergame training on sensorimotor and cognitive function in older adults. A preliminary investigation. Front. Hum. Neurosci. 11, 160 (2017).
Bieryla, K. A. Xbox Kinect training to improve clinical measures of balance in older adults: a pilot study. Aging Clin. Exp. Res. 28, 451–457 (2016).
Chow, D. H. K. & Mann, S. K. F. Effect of cyber-golfing on balance amongst the elderly in Hong Kong: a pilot randomised trial. Hong. Kong J. Occup. Ther. 26, 9–13 (2015).
Gschwind, Y. J. et al. The effect of sensor-based exercise at home on functional performance associated with fall risk in older people - a comparison of two exergame interventions. Eur. Rev. Aging Phys. Act. 12, 11 (2015).
Karahan, A. Y. et al. Effects of exergames on balance, functional mobility, and quality of life of geriatrics versus home exercise programme: randomized controlled study. Cent. Eur. J. Public Health 23, S14–S18 (2015).
Lee, M., Son, J., Kim, J. & Yoon, B. Individualized feedback-based virtual reality exercise improves older women’s self-perceived health: a randomized controlled trial. Arch. Gerontol. Geriatr. 61, 154–160 (2015).
Sato, K., Kuroki, K., Saiki, S. & Nagatomi, R. Improving walking, muscle strength, and balance in the elderly with an exergame using kinect: a randomized controlled trial. Games Health J. 4, 161–167 (2015).
Liepa, A., Tang, J., Jaundaldere, I., Dubinina, E. & Larins, V. Feasibility randomized controlled trial of a virtual reality exergame to improve physical and cognitive functioning in older people. Acta Gymnica 52, e2022.007 (2022).
Gonçalves, A. et al. The benefits of custom exergames for fitness, balance, and health-related quality of life: a randomized controlled trial with community-dwelling older adults. Games Health J. 10, 245–253 (2021).
Lee, K. Virtual reality gait training to promote balance and gait among older people: a randomized clinical trial. Geriatrics 6, 1 (2021).
Li, X. et al. The impact of a multitasking-based virtual reality motion video game on the cognitive and physical abilities of older adults. Sustainability 12, 9106 (2020).
Park, J. & Yim, J. A new approach to improve cognition, muscle strength, and postural balance in community-dwelling elderly with a 3-d virtual reality kayak program. Tohoku J. Exp. Med. 238, 1–8 (2016).
Gschwind, Y. J. et al. ICT-based system to predict and prevent falls (iStoppFalls): results from an international multicenter randomized controlled trial. Eur. Rev. Aging Phys. Act. 12, 10 (2015).
Duque, G. et al. Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 8, 257–263 (2013).
Bao, T. et al. Retention effects of long-term balance training with vibrotactile sensory augmentation in healthy older adults. Sensors 22, 3014 (2022).
Adcock, M. et al. Effects of an in-home multicomponent exergame training on physical functions, cognition, and brain volume of older adults: a randomized controlled trial. Front. Med. 6, 321 (2020).
Bao, T. et al. Effects of long-term balance training with vibrotactile sensory augmentation among community-dwelling healthy older adults: a randomized preliminary study. J. Neuroeng. Rehabil. 15, 5 (2018).
Schwenk, M. et al. Interactive balance training integrating sensor-based visual feedback of movement performance: a pilot study in older adults. J. Neuroeng. Rehabil. 11, 164 (2014).
Delbaere, K. et al. E-health StandingTall balance exercise for fall prevention in older people: results of a two year randomised controlled trial. BMJ 373, n740 (2021).
Yerlikaya, T., Oniz, A. & Ozgoren, M. The effect of an interactive tele rehabilitation program on balance in older individuals. Neurol. Sci. Neurophysiol. 38, 180–186 (2021).
Wu, G., Keyes, L., Callas, P., Ren, X. & Bookchin, B. Comparison of telecommunication, community, and home-based Tai Chi exercise programs on compliance and effectiveness in elders at risk for falls. Arch. Phys. Med. Rehabil. 91, 849–856 (2010).
Lee, K. Home-based exergame program to improve physical function, fall efficacy, depression and quality of life in community-dwelling older adults: a randomized controlled trial. Healthc. Basel Switz. 11, 1109 (2023).
Zhao, C. et al. The effects of active video game exercise based on self-determination theory on physical fitness and cognitive function in older adults. J. Clin. Med. 11, 3984 (2022).
Pacheco, T. B. F., de Medeiros, C. S. P., de Oliveira, V. H. B., Vieira, E. R. & de Cavalcanti, F. A. C. Effectiveness of exergames for improving mobility and balance in older adults: a systematic review and meta-analysis. Syst. Rev. 9, 163 (2020).
Donath, L., Rössler, R. & Faude, O. Effects of virtual reality training (Exergaming) compared to alternative exercise training and passive control on standing balance and functional mobility in healthy community-dwelling seniors: a meta-analytical review. Sports Med. Auckl. NZ 46, 1293–1309 (2016).
Hai, L., Hou, H.-Y., Zhou, C. & Li, H.-J. The effect of exergame training on physical functioning of healthy older adults: a meta-analysis. Games Health J. 11, 207–224 (2022).
Abd-Alrazaq, A., Alhuwail, D., Ahmed, A. & Househ, M. Effectiveness of serious games for improving executive functions among older adults with cognitive impairment: systematic review and meta-analysis. JMIR Serious Games 10, e36123 (2022).
Vinolo Gil, M. J. et al. Augmented reality in physical therapy: systematic review and meta-analysis. JMIR Serious Games 9, e30985 (2021).
Ernst, M. et al. Physical exercise for people with Parkinson’s disease: a systematic review and network meta-analysis. Cochrane Database Syst. Rev. 1, CD013856 (2023).
Crebbin, K., Grisbrook, T., Elliott, C. & Thornton, A. The use of serious gaming to improve sensorimotor function and motivation in people with cerebral palsy: a systematic review. Games Health J. https://doi.org/10.1089/g4h.2022.0112 (2022).
Klompstra, L., Mourad, G., Jaarsma, T., Strömberg, A. & Alwin, J. Costs of an off-the-shelf exergame intervention in patients with heart failure. Games Health J. 12, 242–248 (2023).
Carlier, S., Naessens, V., De Backere, F. & De Turck, F. A Software Engineering framework for reusable design of personalized serious games for health: development study. JMIR Serious Games 11, e40054 (2023).
Arpaia, P., Cimmino, P., De Matteis, E. & D’Addio, G. A low-cost force sensor-based posturographic plate for home care telerehabilitation exergaming. Measurement 51, 400–410 (2014).
Chimento-Díaz, S. et al. Factors associated with the acceptance of new technologies for ageing in place by people over 64 years of age. Int. J. Environ. Res. Public. Health 19, 2947 (2022).
Chen, C.-K. et al. Acceptance of different design exergames in elders. PLoS ONE 13, e0200185 (2018).
Valenzuela, T., Okubo, Y., Woodbury, A., Lord, S. R. & Delbaere, K. Adherence to technology-based exercise programs in older adults: a systematic review. J. Geriatr. Phys. Ther. 41, 49 (2018).
Skjæret, N. et al. Exercise and rehabilitation delivered through exergames in older adults: an integrative review of technologies, safety and efficacy. Int. J. Med. Inf. 85, 1–16 (2016).
Jette, A. M. The importance of dose of a rehabilitation intervention. Phys. Ther. 97, 1043 (2017).
Koivisto, J. & Malik, A. Gamification for older adults: a systematic literature review. Gerontologist 61, e360–e372 (2021).
Tuan, S.-H., Chang, L.-H., Sun, S.-F., Lin, K.-L. & Tsai, Y.-J. Using exergame-based exercise to prevent and postpone the loss of muscle mass, muscle strength, cognition, and functional performance among elders in rural long-term care facilities: a protocol for a randomized controlled trial. Front. Med. 9, 1071409 (2022).
Li, T. et al. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 9, 79 (2011).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71 (2021).
Shea, B. J. et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358, j4008 (2017).
Rathbone, J., Carter, M., Hoffmann, T. & Glasziou, P. Better duplicate detection for systematic reviewers: evaluation of Systematic Review Assistant-Deduplication Module. Syst. Rev. 4, 6 (2015).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
Sterne, J. A. C. et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898 (2019).
Acknowledgements
This work was supported by the Italian Ministry of Health (Ricerca Corrente).
Author information
Authors and Affiliations
Contributions
B.C.: conceptualization, formal analysis, data curation, investigation, methodology, project administration, visualization, writing - original draft; J.M.: investigation, validation, writing - review & editing; A.W.: investigation, validation, writing - review & editing; L.M.: formal analysis, methodology; data curation, visualization, writing - original draft; J.Sz-G.: supervision, validation, writing - review & editing; P.C.: supervision, writing - review & editing; P.K.: conceptualization, supervision, writing - review & editing. All authors read, edited, and approved the final manuscript. All authors had full access to the data in the study, and the data analysis group (B.C., P.K.) verified the underlying data in the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cieślik, B., Mazurek, J., Wrzeciono, A. et al. Examining technology-assisted rehabilitation for older adults’ functional mobility: a network meta-analysis on efficacy and acceptability. npj Digit. Med. 6, 159 (2023). https://doi.org/10.1038/s41746-023-00907-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-023-00907-7
This article is cited by
-
Factors associated with the effectiveness of immersive virtual therapy in alleviating depressive symptoms during sub-acute post-stroke rehabilitation: a gender comparison
BMC Sports Science, Medicine and Rehabilitation (2023)